Aktiferrin
Children have a high risk of intoxication with iron preparations; life-threatening conditions can occur when taking 1 g of iron sulfate. Therefore, iron supplements should be stored out of the reach of children.
Symptoms
: with accidental ingestion of very large doses of the drug, the following symptoms may be observed: weakness, fatigue, paresthesia, pale skin, cold clammy sweat, decreased blood pressure, palpitations, acrocyanosis, abdominal pain, bloody diarrhea, cyanosis, confusion, weak pulse, hyperthermia, lethargy, seizures, symptoms of hyperventilation, coma.
Signs of peripheral circular collapse appear within 30 minutes after administration; metabolic acidosis, convulsions, fever, leukocytosis, coma - within 12-24 hours; acute renal and hepatic necrosis - after 2-4 days.
Treatment
: before carrying out specific therapy, measures are taken to remove the drug that has not yet been absorbed from the stomach (gastric lavage), milk and raw eggs are given. Specific therapy is carried out by prescribing deferoxamine (desferal) orally and parenterally. In case of acute poisoning, to bind iron that has not yet been absorbed from the gastrointestinal tract, give 5-10 g of the drug by dissolving the contents of 10-20 ampoules in drinking water.
In case of advanced poisoning, deferoxamine is administered slowly intramuscularly, for children - 15 mg/hour, for adults - 5 mg/kg/hour (up to 80 mg/kg/day); for mild poisoning - children 1 g intramuscularly every 4-6 hours; adults - 50 mg/kg (up to 4 g/day).
In severe cases, accompanied by the development of shock in patients, 1 g of the drug is administered intravenously and symptomatic therapy is carried out. Death mainly occurs when patients are not treated in a timely manner due to shock. Hemodialysis is ineffective for removing iron, but can be used to accelerate the removal of the iron-deferoxamine complex, and can also be prescribed for oligo- and anuria. Peritoneal dialysis is also possible.
During a course of treatment with iron supplements, systematic monitoring of serum iron levels and other blood serum parameters is necessary.
Special measures: for severe intoxication - Unitaol (sodium dimercaptopropanesulfonate) parenterally.
Due to the possibility of the formation of neurotoxic complexes, Unitaol should be used with caution.
Selection of iron preparations for ferrotherapy of iron deficiency anemia in children
AND
Iron deficiency anemia (IDA) accounts for more than 80% of all anemias in children [2,1]. Young children and adolescents are most predisposed to developing IDA. It has now been shown that long-term iron deficiency in young children can contribute to impaired myelination of nerve fibers and the formation of brain structures, which is accompanied by delayed mental and motor development. Often the symptoms of sideropenia at an early age, especially in the second half of life, are hardly noticeable [9]. In adolescents, the symptoms of iron deficiency state (IDS) can have a peculiar character - there is increased fatigue, muscle weakness, decreased memory, decreased emotional tone, etc. This asthenic syndrome is often associated with overwork, characteristics of adolescence and other reasons, which can lead to late diagnosis ZhDS [5,4]. IDA and latent iron deficiency (LDI) significantly worsen the quality of life of patients, leading to decreased academic performance, neurotic reactions, and conflicts at school and at home. The reasons for the development of sideropenic conditions in children are very diverse and are largely determined by the characteristics of iron metabolism during certain age periods.
Often, with timely diagnosis of IDA in children, its irrational therapy is carried out (for example, the use of only diet therapy, parenteral administration of iron supplements, treatment with “large” doses of iron supplements, etc.) [1,7]. The duration of ferrotherapy at various stages of VHD (IDA, LDJ) remains a subject of discussion. All this dictates the need to clarify the optimal doses and timing of therapy with iron preparations of different groups at different stages of VSD.
Today, the country's pharmaceutical market has a large selection of iron preparations, represented by monocomponent and combined compounds of iron salts and preparations based on the hydroxide-polymaltose complex. A pediatrician is faced with the difficult task of differentiated selection of an iron supplement for a child, taking into account not only the effectiveness, but also their tolerability.
Therapy for iron deficiency conditions should be aimed at eliminating the cause and simultaneously replenishing iron deficiency with iron-containing drugs. The principles of treatment of IDA were formulated by L.I. Idelson in 1981 [6] and have not lost their relevance to the present day.
The main postulates of L.I. Idelson about the treatment of IDA:
- It is impossible to compensate for iron deficiency only with the help of diet therapy without iron supplements;
- IDA therapy should be carried out primarily with oral iron supplements;
- IDA therapy should not be stopped after normalization of hemoglobin levels;
- Blood transfusions for IDA should be carried out only for health reasons.
The choice of drug for the correction of sideropenia is given particular importance, since the duration of treatment is several months. In this case, not only the high effectiveness of treatment is important, but also the absence of side effects, as well as adherence to the therapy, especially in pediatric practice [8].
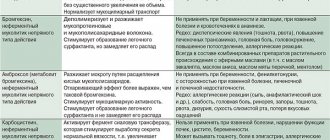
Currently, all iron preparations can be divided into two groups: ionic iron-containing preparations
(salt, polysaccharide compounds of iron) and
nonionic compounds
, which include preparations of the hydroxide-polymaltose complex of ferric iron. This classification is based on the difference in the mechanisms of iron absorption from ionic and nonionic compounds. Absorption of iron from ionic compounds occurs predominantly in divalent form, while the activity of utilization of iron from preparations containing ferric iron salts is strictly limited by a certain pH level of gastric juice (at high acidity of gastric juice, sparingly soluble iron hydroxides are formed). As a result, divalent iron salt preparations, which have good solubility and high dissociation ability, are most often used. Once in the gastrointestinal tract, ferrous iron compounds penetrate the mucosal cells of the intestinal mucosa (pass the “mucosal barrier”), and then into the bloodstream through the mechanism of passive diffusion. In the bloodstream, the process of restoring divalent iron to its trivalent form occurs with the participation of ferroxidase-I and combines with transferrin and ferritin, forming a pool of deposited iron, which, if necessary, is used in the synthesis of hemoglobin, myoglobin, and other iron-containing compounds. As numerous studies have shown, the frequency of side effects depends on the dose of elemental iron. Most often, undesirable symptoms are observed from the gastrointestinal tract (GIT) in the form of diarrhea or constipation. Symptoms of upper gastrointestinal dysfunction usually appear within an hour after taking the medication and can be mild (nausea, epigastric discomfort) or severe (with abdominal pain or vomiting). In addition, therapy with iron salt preparations is accompanied by harmless but rather unpleasant side effects, such as the appearance of a metallic taste in the mouth during the first days of treatment, darkening of tooth enamel and gums. It is known that children receiving ferrous sulfate often develop dark spots on their teeth (up to 30% of cases). At the same time, according to M.K. Soboleva [9], the frequency of adverse events when using actiferrin drops in young children was only about 4%. In only 3% of patients, the start of ferrotherapy was accompanied by increased regurgitation, restlessness, thinning and frequent stools, and in 1% of patients, staining of tooth enamel was noted.
It is well known that iron salt preparations in the intestinal lumen interact with food components and medications, which complicates the absorption of iron. In this regard, iron salt preparations are recommended to be prescribed 1 hour before meals, however, this may enhance the damaging effect of ferrous iron compounds on the intestinal mucosa. Taking into account the high risk of developing undesirable effects when treating IDA with iron salt preparations, the staff of our department proposed a method of “gradually increasing” the dose to a therapeutic dose, taking into account the severity of iron deficiency in the body and the child’s individual tolerance to the drug, which, if they develop, makes it possible to timely identify the initial manifestations. Initial treatment for IDA begins with a dose equal to 1/2–1/3 of the therapeutic dose (1–1.5 mg/kg/day of elemental iron for young children), followed by gradual achievement of the full dose over 7–14 days [7 ].
An important aspect of ferrotherapy, especially in pediatric practice, is the therapeutic safety of the iron preparations used. The high risk of side effects and iron intoxication during therapy with iron salt preparations is due to the mechanism of absorption of divalent iron - through passive diffusion. Salt preparations contain iron in divalent form. In order to be absorbed, Fe2+ undergoes oxidation, which promotes the formation of free radicals.
Thus, ID replacement therapy with iron salt preparations is quite effective, but the high risk of side effects reduces the patient’s adherence to treatment in some cases.
New highly effective and safe iron preparations include preparations that are nonionic iron compounds based on the hydroxide–polymaltose complex (HPC) of ferric iron. The structure of the complex consists of polynuclear Fe(III) hydroxide centers surrounded by non-covalently bound polymaltose molecules. The complex has a high molecular weight, which makes it difficult to diffuse through the intestinal mucosal membrane. The chemical structure of the complex is as close as possible to the structure of natural compounds of iron and ferritin. The absorption of iron in the form of HPA has a fundamentally different pattern compared to its ionic compounds and is ensured by the entry of Fe (III) from the intestine into the blood through active absorption. From the drug, iron is transferred through the brush border of the membrane on a carrier protein and is released to bind with transferrin and ferritin, in a block with which it is deposited and used by the body as needed. Physiological processes of self-regulation completely exclude the possibility of overdose and poisoning. There is evidence that when the body is saturated with iron, its resorption stops according to the feedback principle. Based on the physicochemical characteristics of the complex, in particular, on the fact that active transport of iron is carried out according to the principle of competitive exchange of ligands (their level determines the rate of iron absorption), its absence of toxicity has been proven. The non-ionic structure of the complex ensures its stability and the transfer of iron using a transport protein, which prevents the free diffusion of iron ions in the body, i.e. pro-oxidant reactions.
Safety data obtained during clinical trials of an iron preparation based on Fe(III) hydroxide with polymaltose indicate a lower incidence of side effects compared to iron salt preparations. In rare cases, there is a feeling of stomach fullness, pressure in the epigastrium, nausea, diarrhea or constipation. Thus, in numerous randomized studies it was shown that treatment with Fe (III)-GPA preparations was tolerated significantly better than with iron salt preparations (ferrous sulfate, ferrous fumarate), which was confirmed by a lower incidence of side effects from the gastrointestinal tract.
After choosing an iron-containing drug and the method of its use, it is necessary to determine the daily daily dose of the drug and the frequency of administration. Daily therapeutic doses of oral iron salt preparations for the treatment of IDA in children were proposed by WHO experts (WHO, 1989): for children under 3 years of age – 3 mg/kg/day of elemental iron; for children over 3 years old – 45–60 mg/day of elemental iron; for adolescents – up to 120 mg/day of elemental iron. When using Fe (III)–HPA preparations, the daily dose for young children is 3–5 mg/kg body weight. Recommended doses of ferrous iron are calculated taking into account the fact that only 10-15% of the iron entering the body is absorbed.
The therapeutic effect of oral iron supplementation appears gradually. Initially, clinical improvement is noted, and only after some time does hemoglobin normalize. The first positive clinical symptom that appears during treatment with iron supplements is a decrease in muscle weakness. The latter is due to the fact that iron is part of the enzymes involved in the contraction of myofibrils. On days 10–12 from the start of treatment, the content of reticulocytes in the peripheral blood increases. The increase in hemoglobin can be gradual or abrupt; most often, the onset of an increase in hemoglobin levels occurs 3–4 weeks from the start of therapy. Elimination of clinical manifestations of the disease is observed after 1–2–3 months of therapy, and overcoming tissue sideropenia after 3–6 months of treatment [1]. The daily dose of elemental iron after normalization of hemoglobin levels should correspond to 1/2 of the therapeutic dose. Some authors [3] recommend that in premature infants, in order to completely replenish iron reserves in their body, continue ferrotherapy in maintenance doses until the end of the 2nd year of life. Early cessation of iron treatment usually leads to relapses of IDA [6].
Thus, given the duration of ferrotherapy, the choice of drug for the correction of sideropenia in young children requires special attention. The main requirements for oral iron preparations used in pediatric practice are: sufficient bioavailability, high safety, good organoleptic properties, the presence of various dosage forms convenient for patients of all ages, and compliance [7]. These criteria are best met by iron preparations based on CGP.
- Ferrum Lek, Maltofer.
We have studied the effectiveness and tolerability of the drug Ferrum Lek
at various stages of VDS in 43 children aged from 4 months to 5 years. The vast majority of patients (81%) were 1–3 years of age, with a mean age of 1 year 8 months. The observation was carried out at the Moscow orphanage.
Patients received hydroxide - polymaltose complex of iron (III) - the drug Ferrum Lek in the form of syrup, which was used according to the following scheme:
- for iron deficiency anemia (IDA) - at the rate of 5 mg/kg/day;
- for latent iron deficiency (LID) - at the rate of 2.5 mg/kg/day.
The drug was given 2 times a day before meals, washed down with juice.
Examination of children to confirm the diagnosis of IDA and LVAD included:
- determination of hemoglobin (Hb) level (in case of anemia, its level is less than 110 g/l in children under 5 years of age);
- determination of serum ferritin (FS) content in the blood (for anemia less than 30 μg/l).
Among 43 examined children with sideropenia, 24 were diagnosed with IDA (56%). Of these, mild anemia was observed in 15 (63%), moderate anemia in 8 (33%), and severe anemia in 1 (4%) child. Latent iron deficiency was found in 19 children (44%).
All children with sideropenia received therapy with Ferrum Lek at a dose of 5 mg/kg/day for IDA and 2.5 mg/kg/day for LAD.
The duration of the main course of treatment with Ferrum Lek (in full dose) was:
- for mild anemia – 8 weeks
- for moderate anemia – 10 weeks
- for severe anemia 12 weeks.
The duration of prophylactic administration of Ferrum Lek - syrup at a dose of 2.5 mg/kg/day (in order to create an iron depot in the body) was:
- for mild anemia – 4–6 weeks
- for moderate anemia – 6 weeks
- for severe anemia – 8 weeks.
Thus, the total duration of ferrotherapy for IDA ranged from 12 to 20 weeks. Our observations have shown the high effectiveness of the drug Ferrum Lek in the treatment of VSD in children. On average, within 8–12 weeks, all children had normalized hemoglobin and serum ferritin levels, which indicates not only the elimination of IDA, but also the replenishment of iron depots in the body (Table 1). The dynamics of hemoglobin and serum ferritin levels in a child with severe IDA is shown in Fig. 1.
Rice. 1. Dynamics of hemoglobin (Hb), serum iron (SI), total iron-binding capacity (TIBC) and ferritin (SF) levels in a child with severe IDA during treatment with Ferrum Lek.
The duration of therapy with Ferrum Lek in children with LID ranged from 4 to 8 weeks.
The criterion for determining the optimal duration of ferrotherapy for LID is the restoration of serum ferritin levels. The dynamics of ferritin content in the blood serum of children with LID before and after ferrotherapy are presented in Table. 2.
During the study, we did not identify any adverse reactions. Only 12% of children with functional disorders of the gastrointestinal tract showed a tendency to constipation during treatment with Ferrum Lek. 41 out of 43 children completed the course of treatment, thus, adherence to treatment was 95.3%. In 100% of cases, children took Ferrum Lek in syrup form with pleasure.
Treatment with Ferrum Lek for 8–12 weeks led to normalization of hemograms, hemoglobin levels, and improvement of iron levels in all examined children with IDA. The total duration of ferrotherapy in this group of patients was 12–20 weeks. The duration of treatment for LID was 4–8 weeks.
The absence of complications and adverse events indicates the safety of using the drug Ferrum Lek.
An important advantage of the drug Ferrum Lek is not only its high efficiency, but also good tolerability, as well as a convenient form of release in the form of syrup, good organoleptic qualities, which allows us to consider Ferrum Lek the optimal drug for the treatment and prevention of IDA in young children.
Literature:
1. Anemia in children: diagnosis and treatment / Practical manual for doctors edited by Rumyantsev A.G., Tokarev Yu.N.. - M.: MAKS Press, 2000 - 9–17 p.
2. Beloshevsky V.A. Iron deficiency. – Voronezh, 2000.
3. Bisyarina V.P., Kazakova L.M. Iron deficiency anemia in young children. – M.: Medicine, 1976. – 176 p.
4. Vorobyov P.A. Anemic syndrome in clinical practice. M. – 2001, p. 36–94.
5. Dvoretsky L.I. Iron deficiency anemia. – M., 1998.
6. Idelson L.I. Hypochromic anemia. – M.: Medicine, 1981. – 192 p.
7. Korovina N.A., Zaplatnikov A.L., Zakharova I.N. Iron deficiency anemia in children. – M., 1999.
8. Kazyukova T.V., Samsygina G.A., Kalashnikova G.V., Rumyantsev A.G., Fallukh A., Motina A.G., Levina A.A. New possibilities of ferrotherapy for iron deficiency anemia. /Clinical pharmacology and therapy/M., 2000, volume 9, No. 2, pp. 88–91.
9. Soboleva M.K. Iron deficiency anemia in young children and nursing mothers and its treatment and prevention with Maltofer and Maltofer-Fol. /Pediatrics/, M., No. 6, 2001, 27–32.
ACTIFERRIN (drops)
...in kindergarten, hemoglobin returned to normal!
Hurray!!)) Now about “Actiferrin”. My son is still breastfed. He also eats other foods, but in small portions and not varied enough (we also have allergies, so I can’t give him everything). One of the consequences is iron deficiency. There was low hemoglobin a year ago, but then it was higher, and I hoped for the best and did not treat the child with anything. That's what I've been waiting for! During the next test, the iron level dropped to 80. The doctor prescribed “Actiferrin” drops. I bought it. The bottle, 30 ml (which is very convenient - you will have time to understand whether it is effective, and you do not have to overpay for the extra volume if suddenly the drug does not suit you), is equipped with a dispenser to make it more convenient to drip. We started treatment, and then... Usually there is constipation, but my son has diarrhea! Well, I guess it's a coincidence. After the next use - the same thing, we ran to the potty several times in a row. I decided to stop using this drug. We didn’t use it for several days, and during this time the readings dropped to 76! I'm starting to panic! It's good that I thought of re-reading the instructions again. It says that it is better to start administering the medicine in small doses to avoid side effects. Considering our weight, it was necessary to give 25 drops 3 times a day. I started with 5 drops, increasing the amount by 1-2 drops every day. After just 2 weeks, hemoglobin rose to 102!! She continued to give “Actiferrin” until the bottle ran out. I hope that now all my son’s indicators will be normal.
The most important advantage is obvious - the drug works, and quickly, which is important. One caveat - do not give iron supplements at the same time as dairy products, because calcium interferes with the absorption of iron. Now about the so-called disadvantages (but personally I don’t consider these to be disadvantages, I just read other reviews - most are unhappy): - teeth darken. My opinion is that it’s better to have stained teeth than health problems. And the teeth darken in those places where the enamel is problematic, and this is certainly not Aktiferrin’s fault. Personal advice: give the drug with food, then the remaining medication will be swallowed with food and will not remain in the mouth. Here are our teeth BEFORE this is AFTER In my opinion, there is nothing wrong. - stains on clothes from spilled medicine. Also a dubious “minus”. People, are you really giving the drug to a child in formal clothes??? Well, put on a homemade T-shirt for him and always give your baby something to drink only in it, so as not to dirty anything else! And the spots can’t be called spots either. Do you see anything above the letter “a”? This is the so-called stain)) - the next point that others write about: bad taste, children categorically refuse to drink. Nothing like this. How did I do it? We take a spoon, a cup of water (so that we have it at hand), fill the spoon with water, add 5 (or as many as is convenient for you) drops of medicine, and give it to the baby. You can immediately give it a spoonful of plain water to wash it down. And so several times in a row. We needed to drink 25 drops, so we drank them with 5 tablespoons of water. Everything is simple, as you can see) Well, don’t forget to chew on food (see the previous point) - the only adequate minus is the possibility of side effects. But I have already written how to cope with such a risk.
We're done with the negatives. The advantages were higher) Draw your own conclusions, I hope my review will help you with this. All the best, don't get sick)