History of the creation of streptocide
How it all began
Sulfanilamide, an intermediate in the production of dyes, has been used in the textile and leather industries since 1908. But until some time no one thought to study its antimicrobial properties. One of the greatest discoveries in medicine was made in a roundabout way.
At the beginning of the twentieth century, some aniline dyes were already used as antiseptics - methylene blue, brilliant green. Scientific developments in this direction continued - scientists were actively looking for new means to combat infections among dyes.
One of these scientists was the German bacteriologist Gerhard Domagk. He faced many trials. During the First World War, after being wounded, he had to work as a military orderly at the front, where he saw dozens and hundreds of deaths and injuries. Very young people died in hospitals from infected wounds, sepsis, lost limbs due to amputations and became disabled, and died from epidemics. Streptococcal infection was especially rampant. Even then, Gerhard Domagk promised himself that he would find a way to fight this evil.
From experiments on mice to an experiment of despair
Returning from the war, Domagk continued his interrupted medical studies and then began scientific work. At the end of the 20s, he investigated the properties of a red dye called “prontosil rubrum,” a substance patented by the IG Farbenindustrie concern, in whose laboratory he worked. The scientist infected laboratory animals (mice, rabbits) with staphylococcal and streptococcal infections, and then gave some of them a solution of prontosil. The results obtained in 1932 were stunning - animals treated with Prontosil survived and recovered, while others died from infection.
However, the scientist was in no hurry to transfer his research to people - years of painstaking work still lay ahead to decide on this important step. However, life itself made its own adjustments. A misfortune occurred in the Domagk family - his daughter Hildegard pricked herself with a sewing needle, as a result of which she quickly developed a severe streptococcal infection. When the question arose about amputating the arm to save the girl’s life, the desperate father risked using a drug that had not yet been fully studied. After taking several doses of Prontosil, the girl began to recover. This was followed by thorough clinical trials, the results of which were published only by 1935. Other countries also tried to create analogues of Prontosil. In the USA, in 1936, President Roosevelt’s son was cured of septic sore throat with a similar drug (called “Printilin”).
Well-deserved recognition
In 1939, Gerhard Domagk was awarded the Nobel Prize in Physiology or Medicine for the discovery of the antibacterial effect of Prontosil, but he was unable to receive it. The Third Reich had tense relations with the Nobel Committee in connection with the award of the Peace Prize to the anti-fascist imprisoned in a concentration camp - Karl von Ossietzky. For this and some other reasons, in Hitler's Germany, writers, scientists, and public figures were strictly forbidden to receive Nobel awards. Domagk even had a chance to visit the dungeons of the Gestapo, although not for long, where he was strongly advised to refuse the bonus. Only in 1947 was the scientist finally awarded a gold medal and a diploma, but the deadline for paying the monetary reward had already been missed at that time.
Old friend - sulfanilamide
It was not entirely clear why the drug Prontosil, which is so active in animals and humans, does not give any effect “in vitro” (in a test tube). The answer in 1935 was given by French scientists who determined that in a living organism prontosil is split into two components: the long-known sulfonamide (which, in fact, has an antibacterial effect), and the rather toxic 1,2,4-triaminobenzene.
Streptocide – red or white?
Subsequently, sulfonamide without triaminobenzene was continued to be used in medicine, calling the drug “white streptocide.” “Red streptocide” (formerly Prontosil), due to its toxicity, was phased out, although it was still used for some time, for example, for hair dyeing.
The word “streptocide” translated means “killing streptococci,” but the medicine had a much wider spectrum of action: it was used in the treatment of plague, cholera, diphtheria, anthrax, gas gangrene and other diseases. At the time of the discovery of streptocide, most bacteria did not have resistance to this drug, so the effect of the treatment was truly miraculous. The use of streptocide saved the lives of tens and hundreds of thousands of people.
“White streptocide” preparations serve humanity to this day. By the way, its name turned out to be not entirely accurate. The fact is that, in fact, streptocide does not kill bacteria, but blocks their reproduction, that is, it has not a bactericidal, but a bacteriostatic effect, which, however, does not have much significance for the final result.
The most important medical and social problem is the treatment of long-term non-healing wounds of various etiologies. Trophic ulcers and deep skin cracks in the lower extremities, as well as chronic ulcerative pyoderma, sharply reduce the quality of life and limit the activity of patients for a long time. Local therapy occupies a special place in the treatment and prevention of these diseases, preventing the development of an infectious process in the wound and being a barrier to the spread of infection.
Modern highly effective agents for local treatment of long-term non-healing wounds have a number of medicinal qualities that allow their use taking into account the phases of the wound process. They must have anti-inflammatory and proteolytic effects, have a wide antibacterial spectrum of action, remain active in an acidic environment, not cause hypergranulation and pigmentation, have hypoallergenic qualities, be non-toxic and easy to use.
There are many combination drugs for local treatment containing antibiotics or sulfonamides in combination with each other and/or various antiseptics. Such drugs are characterized by a slower development of microbial resistance and a wider coverage of bacterial agents that cause infections.
Argosulfan cream
2% (“Elfa Farmzavod A.O.”) is a combined topical antibacterial drug that promotes healing and effective protection of wounds (trophic, purulent, burns, etc.) from infection.
silver sulfathiazole
included in its composition has a wide spectrum of antibacterial and bacteriostatic effects against gram-positive, gram-negative microflora and pathogenic anaerobes, and is also effective against fungal superinfection. The mechanism of the antimicrobial action of sulfathiazole - inhibition of the growth and reproduction of microbes - is associated with competitive antagonism with para-aminobenzoic acid and inhibition of dihydropteroate synthetase, which leads to disruption of the synthesis of dihydrofolic acid and its active metabolite - tetrahydrofolic acid, necessary for the synthesis of purines and pyrimidines of the microbial cell [1].
The silver ions present in the cream enhance the antibacterial effect of sulfonamide - they inhibit the growth and division of bacteria by binding to the deoxyribonucleic acid of the microbial cell [1]. The gradual release of silver ions suppresses the growth of pathogenic microflora over a long period of the dressing being on the wound, which is important when there is a high risk of reinfection with hospital strains and is a permanent barrier to the spread of infection.
In addition, silver ions weaken the sensitizing properties of sulfonamide. There is an opinion according to which the application of sulfonamides to the skin and mucous membranes is undesirable due to their low activity and the risk of an allergic reaction. When applying such an ointment to a burn or infected surface, burning and pain may occur [1]. Hydrophilic cream base Argosulfan
, which has an optimal pH and contains a large amount of water, provides its moisturizing and analgesic effect and leads to a decrease in wound healing time.
Due to minimal resorption Argosulfan
-cream applied even to large wound surfaces does not have a toxic effect, since silver sulfathiazole has low solubility, due to which the concentration of the drug in the wound is maintained at the same level for a long time.
A small amount of silver sulfathiazole that appears in the bloodstream undergoes acetylation in the liver and is found in the urine in the form of inactive metabolites and partially unchanged [1]. Due to the lack of systemic absorption of the drug, Argosulfan
in combination with other drugs.
Dressings with Argosulfan
containing silver ions are painless when applied to the wound surface, do not dry to the wound and are easily removed from its surface, have a mild drying effect, and penetrate well into necrotic tissue and exudate. Tissue detritus impregnated with the drug forms a “protective cushion”, under which accelerated formation of granulations and epithelization occurs.
We used Argosulfan
for long-term non-healing wounds in patients with trophic ulcers of various etiologies, necrobiosis lipoidica, chronic ulcerative and ulcerative-vegetative pyoderma, deep fissures complicating the course of tylotic eczema.
The appearance of trophic ulcers
can complicate the course of many diseases - from diseases of the circulatory system to metabolic disorders, and the development of a peptic ulcer is accompanied by both a violation of normal blood circulation and a change in innervation. That is why the recovery process may require the use of complex effects and fairly long-term treatment.
There are varicose, ischemic and neurotrophic ulcers [2-5]. The largest group (1-2% of the adult population) consists of patients with chronic venous insufficiency (CVI) of the lower extremities, which develops when venous outflow is impaired and pressure inside the capillaries increases. The main causes of CVI are varicose veins and postthrombophlebitic syndrome. When the valves of the deep veins of the leg are damaged, the function of the muscular-venous pump is disrupted and retrograde blood flow occurs. Damage to the perforating veins, which connect the superficial veins to the deep veins, aggravates venous insufficiency. Due to fibrin deposition in the perivascular space and inhibition of tissue fibrinolysis, sclerosis and obliteration of lymphatic and small blood vessels develop. Perivascular fibrosis disrupts the delivery of nutrients to the epidermis, which leads to the formation of varicose trophic ulcers [2-5].
Ischemic ulcers form in diseases of the peripheral arteries, in particular in obliterating atherosclerosis (OA). OSA is always accompanied by skin damage - from gradually increasing ischemia to infarction, i.e. necrosis, which develops when there is a sudden disruption of blood supply as a result of atheroembolism - blockage of small arteries with fragments of atherosclerotic plaques. Ischemic ulcers are localized in frequently injured areas and areas of compression, and are accompanied by severe pain. Mixed ulcers develop in patients suffering from both CVI and OSA, who clinically have features of both diseases [4, 5].
The cause of neurotrophic ulcers is damage to sensory and motor nerves, circulatory disorders and atherosclerosis in diabetes mellitus and its complications, secondary hyperparathyroidism, granulomatous inflammation in response to collagen degeneration in necrobiosis lipoidica [6, 7].
Necrobiosis lipoidica
- a rare chronic dermatosis of a vascular-metabolic nature, which is usually classified as a group of localized lipoidoses of the skin. The provoking factors in necrobiosis lipoidica in 1/3 of cases are diabetes mellitus, and in another 1/3 - impaired glucose tolerance, therefore, family history and research are necessary to identify hidden forms of diabetes mellitus. The onset of the disease is often preceded by trauma. Collagen degeneration leads to increased platelet aggregation, microangiopathies, damage to arterioles, sclerosis and obliteration of blood vessels in foci of necrobiosis. Vascular disorders lead to trophic disturbances and necrobiotic changes in the dermis with subsequent deposition of lipids in it. The disease often has a long, relapsing course, its severity does not depend on the severity of diabetes mellitus; the developing trophic ulcers are accompanied by severe pain and heal, as a rule, with the formation of a rough scar [6, 7].
Without special treatment, trophic ulcers are characterized by a low tendency to heal and a long, relapsing course [8, 9]. It is generally accepted that surgical treatment of CVI and OSA is best performed after healing of the trophic ulcer or thorough sanitation of its surface. However, conservative treatment using outdated, ineffective local medications is often complicated by dermatitis, eczema, and erysipelas, which delays the timing of vascular surgery. The choice of drug is influenced by the phase of the disease and the severity of the inflammatory reaction (phase I - pre-ulcerative state; phase II - dystrophic changes, necrosis, inflammation of the skin and adjacent tissues; phase III - ulcer cleansing and regeneration; phase IV - epithelization and scarring), complications (mycoses, eczema, pyoderma, erysipelas, recurrent thrombophlebitis, malignancy, etc.), species composition of the ulcer microflora. Numerous bacteriological studies of the qualitative composition of the microflora of the surface of trophic ulcers have revealed multidrug-resistant gram-positive and gram-negative microflora. The content of microorganisms in induratively changed tissues surrounding the ulcer sometimes reaches 107-109 microbial bodies per 1 g of wound tissue, which indicates a high risk of generalization of the infectious process [10]. As a rule, the isolated microorganisms are highly resistant not only to traditional antibacterial drugs, but also to the local agents most often used in such cases - solutions of furatsilin, chlorhexidine, syntomycin emulsion, ointments with antibiotics (tetracycline, gentamicin), etc. At the stages of granulation and epithelialization, to speed them up, as well as when wounds are complicated by dermatitis, eczema or other manifestations of allergies to traditional drugs, silver salts may become the drug of choice, given their high efficiency in suppressing both gram-positive and gram-negative microflora, better tolerability and the rarity of allergic reactions even in patients with a burdened history of allergies.
Pyoderma
(pustular skin diseases) are a group of dermatoses based on purulent inflammation of the skin and its appendages, as well as subcutaneous fat. Pyoderma accounts for 1/3 of all cases of skin diseases [4, 5]. The development of pyoderma is promoted by microtrauma, maceration and contamination of the epidermis, increased sweating, hypothermia, overheating, endocrinopathies (diabetes mellitus), hypogammaglobulinemia, insufficient protein intake, hypovitaminosis, immunity disorders and severe somatic diseases, fatigue, chronic intoxication, persistent foci of staphylococcal infection. The most common causative agents of pyoderma are Staphylococcus aureus and Staphylococcus epidermidis (80-90% of patients); in 10-15% of cases a mixed infection is detected (staphylococcus in combination with streptococcus, Pseudomonas aeruginosa, Proteus, Escherichia coli, etc.) [1, 4, 10 ].
Chronic ulcerative and ulcerative-vegetative pyoderma belong to deep streptostaphylococcal pyoderma, characterized by the formation of poorly healing ulcerative purulent lesions of the skin and underlying tissues. Often the disease is accompanied by a deterioration in general condition, increased body temperature, weakness, symptoms of intoxication, lymphangitis and lymphadenitis. Ulcerative pyoderma
(streptostaphylococcal impetigo) manifests itself as phlyctenae, ecthyma, located against the background of erythema.
The rashes, usually disseminated, cover large areas of the skin. Under the crusts, the formation of deep ulcers with flaccid granulations at the bottom and inflamed soft edges is characteristic. Streptostaphylococcal impetigo is often a complication of itchy dermatoses (eczema, scabies, atopic dermatitis, etc.). Chronic ulcerative-vegetative pyoderma
is characterized by ulcerative formations of irregular shape with pronounced vegetations in the area of the edges and bottom. Often there is a stagnant pink halo of hyperemia around the ulcer. Characterized by a chronic course with periodic exacerbations with the appearance of new ulcers or serpigenization of the main ulcer formation.
Therapy for pyoderma should be etiopathogenetic. In the treatment of chronic, recurrent and deep forms of pyoderma, antibiotics (locally and systemically), antiseptic solutions, glucocorticosteroids, immunomodulators, vitamins are used, pustules and abscesses are opened, and if necessary, vegetations and necrotic tissue are removed and scraped out.
Tylotic (horny) eczema
- a chronic persistently recurrent allergic skin disease, a type of true eczema. Tilotic eczema is manifested by hyperkeratosis of the palms and soles with the formation of rough horny and cortical layers, dry skin, as well as deep, painful, long-term non-healing, often bleeding cracks. This disease is characterized by polyvalent sensitization and autosensitization, occurs against the background of neuroendocrine changes, and is accompanied by changes in the central and autonomic nervous system, disorders of metabolic processes and tissue trophism [4, 5]. Damage to the soles and palms is usually symmetrical; cracks form against the background of erythema and peeling, especially in areas of greatest pressure and load, including on the lateral surfaces of the fingers. Inflammation can be expressed in a limited area or occupy the entire sole and/or palm; pain in the area of the cracks can be more intense than itching. The tendency for cracks to deepen is associated with the patient’s age, duration of the disease, cold season and the presence of underlying diseases.
Pyogenic infection can easily penetrate into cracks on the soles, and erysipelas or pyoderma can develop. Tilotic eczema is resistant to treatment, prone to recurrence, improvement of the condition is achieved by frequent and strong moisturizing of the skin and immediate cessation of wearing wet shoes [11].
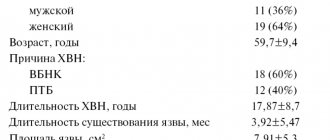
We observed 47 patients (13 men, 34 women) aged 44-75 years with trophic ulcers that developed against the background of CVI and obliterating endarteritis, circulatory and trophic disorders in necrobiosis lipoidica, as well as with pyoderma and tylotic eczema. The duration of the disease ranged from 2 months to 4 years. Argosulfan cream externally as part of complex therapy.
.
11 (23.4%) patients had varicose ulcers, 5 (10.6%) had mixed trophic ulcers, 8 (17%) had trophic ulcers due to necrobiosis lipoidica; 8 (17%) had chronic ulcerative and chronic ulcerative-vegetative pyoderma, 15 (32%) had tylotic eczema with deep cracks on the palms and soles.
In 22 (46.8%) patients, dermatoses occurred against the background of endocrine diseases: in 4 (8.4%) - diabetes mellitus, in 2 (4.2%) - impaired glucose tolerance, in 5 (10.6%) - nodular goiter, 1 (2.1%) - hypothyroidism, 1 (2.1%) - adrenal pathology. Chronic bronchitis was detected in 2 (4.2%) patients, chronic gastritis in 3 (6.3%), chronic pancreatitis in 5 (10.6%), and viral hepatitis C in 2 (4.2%) , 10 (21.3%) had hypertension, 9 (1%) had coronary heart disease, 2 (4.2%) had uterine fibroids.
Bacteriological studies of the qualitative composition of microflora from the surface of lesions (ulcers, cracks) revealed Staphylococcus aureus and Staphylococcus epidermidis in 29 (61.7%) patients, mixed infection (staphylococci in combination with streptococcus, Escherichia coli, bacteroides, Proteus, yeast fungi) in the amount of 104-105 microbial bodies per 1 g of wound tissue.
All patients were prescribed a protective regimen. It was proposed to limit stay in an upright position in order to reduce the static load, and to place the affected limb in an elevated position. It was recommended to reduce dietary intake of salt and extractive products; patients with tylotic eczema were prescribed a hypoallergenic diet; patients with necrobiosis lipoidica were prescribed a diet with a limited carbohydrate-fat load.
As part of complex therapy, all patients received vascular drugs and venoprotectors (pentoxifylline, detralex, aescusan), antiplatelet agents (curantil), desensitizing agents (calcium gluconate, sodium thiosulfate), trophic improvers (solcoseryl, actovegin) and antihistamines (suprastin, tavegil, loratadine) drugs. Patients with trophic ulcers, necrobiosis lipoidica, pyoderma were treated with cephalosporin antibiotics, immunomodulators (methyluracil, viferon, cycloferon), vitamins (milgamma), with tylotic eczema - vitamin A preparations (Aevit, retinol palmitate), with necrobiosis lipoidica - lipoic acid preparations (berlition).
Argosulfan cream as an external remedy.
.
After cleansing with a 0.1% aqueous solution of chlorhexidine and/or surgical treatment of the wound surfaces, the drug was applied in a layer of 2-3 mm daily, 2 times a day, to the lesions on cracks or ulcers from the middle to the edges until completely absorbed. For larger lesions, Argosulfan
was applied daily under an occlusive dressing at night. During treatment, the wound was completely covered with the drug; if part of it was opened, additional cream was applied. The course of complex treatment was 25-30 days.
Pain, as well as local and general allergic reactions when using Argosulfan
was not observed.
Argosulfan cream
in the local treatment of long-term non-healing wounds, it allowed to achieve improvement in all patients.
As a result of complex therapy, complete epithelization of trophic ulcers in patients with CVI, OSA and necrobiosis lipoidica occurred in 10 (41.7%) cases, partial regression (reduction in size, inflammatory and dystrophic changes in the skin, the appearance of mature granulations and marginal epithelialization with minimally pronounced pigmentation ) - in 14 (58.3%). The symptoms of pyoderma resolved in 7 (87.5%) patients and decreased significantly (with a sharp slowdown in microflora growth to 102 microbial bodies per 1 g of wound tissue) in 1 (12.5%). Argosulfan
cream contributed to the formation of soft, mobile, weakly pigmented scars. Cracks in the area of the palms and soles against the background of resolution of tilotic eczema were epithelialized in all 15 (100%) patients.
Because Argosulfan
- a drug for long-term use, which is due to the slow restoration of physiological processes in the epidermis and dermis; for patients with trophic ulcers and pyoderma, we recommended using it according to the previously used scheme on an outpatient basis for 1-2 months after the end of the course of treatment in the hospital (until complete healing or skin transplantation ).
Thus, 2% cream Argosulfan
in the complex therapy of patients with long-term non-healing wounds, it turned out to be highly effective both at the stage of formation of trophic ulcers and during the period of filling deep wounds with granulation tissue, which in many cases led to their independent healing under a bandage. The drug was well tolerated, easy to use, and made it possible to significantly reduce the cost of treating a patient in a hospital and successfully continue treatment on an outpatient basis.