This disease can be divided into several forms:
- congenital anemia - characterized by the breakdown of red blood cells as a result of genetic defects: erythrocyte membranopathy - the membrane of red blood cells is disrupted at the genetic level, which leads to their rapid decay;
- enzymopathies (enzymopathies) – rapid decay is caused by a deficiency in the activity of erythrocyte enzymes (most often glucose-6-phosphate dehydrogenase);
- hemoglobinopathies are a type of anemia that is associated with disturbances in the structure of the hemoglobin protein at the genetic level;
- a defect in the red blood cell membrane is a disease that is extremely rare. It is characterized by the breakdown of red blood cells during sleep;
- toxic substances on red blood cells (for example, poisoning with poisons, heavy metals, lead);
Causes
The following causes may influence the appearance of hemolytic anemia:
Congenital anemias:
- hereditary hemolytic anemia, in which the defective gene is passed on to the child from one or both parents;
- a spontaneous mutation at the genetic level during the period of intrauterine development of the fetus leads to the development of hemolytic anemia in children.
In the case of the presence of a defective gene that causes this disease in both fragments of the chromosome, we are talking about a homozygous form. The chances of surviving to adulthood for patients with this diagnosis are almost zero.
Acquired hemolytic anemia:
- arise as a result of prolonged exposure to chemicals or medications on the body;
- anemia resulting from the effects on the body of infections caused by bacteria or parasites (for example, malaria);
- anemia can be caused by an extensive burn, due to which the body is poisoned with poisons;
- reasons related to the immune system, for example, blood type incompatibility during transfusion, the production of antibodies in the body against its own red blood cells, mechanical damage to red blood cells, lack of vitamin E in the body.
Autoimmune hemolytic anemia
With the acute onset of autoimmune hemolytic anemia, patients experience rapidly increasing weakness, shortness of breath and palpitations, pain in the heart, sometimes in the lower back, fever and vomiting, intense jaundice. In the chronic course of the process, a relatively satisfactory state of health of patients is noted even with deep anemia, often pronounced jaundice, in most cases an enlargement of the spleen, sometimes the liver, alternating periods of exacerbation and remission. Anemia is normochromic, sometimes hyperchromic; during hemolytic crises, severe or moderate reticulocytosis is usually observed. Macrocytosis and microspherocytosis of erythrocytes are detected in the peripheral blood, and normoblasts may appear. ESR is increased in most cases. The content of leukocytes in the chronic form is normal; in the acute form, leukocytosis occurs, sometimes reaching high numbers with a significant shift in the leukocyte formula to the left. The platelet count is usually normal. In Fisher-Evens syndrome, autoimmune hemolytic anemia is combined with autoimmune thrombocytopenia. In the bone marrow, erythroposis is enhanced, and megaloblasts are rarely detected. In most patients, the osmotic resistance of erythrocytes is reduced, which is due to a significant number of microspherocytes in the peripheral blood. The bilirubin content is increased due to the free fraction, and the content of stercobilin in the feces is also increased.
Incomplete heat agglutinins are detected using a direct Coombs test with polyvalent antiglobulin serum. With a positive test, using antisera to IgG, IgM, etc., it is clarified which class of immunoglobulins the detected antibodies belong to. If there are less than 500 fixed IgG molecules on the surface of red blood cells, the Coombs test is negative. A similar phenomenon is usually observed in patients with a chronic form of autoimmune hemolytic anemia or those who have suffered acute hemolysis. Cases when antibodies belonging to IgA or IgM (against which polyvalent antiglobulin serum is less active) are fixed on red blood cells are also Coombs-negative. In approximately 50% of cases of idiopathic autoimmune hemolytic anemia, antibodies to one’s own lymphocytes are detected simultaneously with the appearance of immunoglobulins fixed on the surface of red blood cells.
Hemolytic anemia due to warm hemolysins is rare. It is characterized by hemoglobinuria with black urine, alternating periods of acute hemolytic crisis and remissions. Hemolytic crisis is accompanied by the development of anemia, reticulocytosis (in some cases thrombocytosis) and an enlarged spleen. There is an increase in the level of free bilirubin fraction and hemosiderinuria. When treating donor red blood cells with papain, it is possible to detect monophasic hemolysins in patients. Some patients have a positive Coombs test.
Hemolytic anemia caused by cold agglutinins (cold hemagglutinin disease) has a chronic course. It develops with a sharp increase in the titer of Cold hemagglutinins. There are idiopathic and symptomatic forms of the disease. The leading symptom of the disease is excessive sensitivity to cold, which manifests itself in the form of blueness and whiteness of the fingers and toes, ears, and tip of the nose. Peripheral circulatory disorders lead to the development of Raynaud's syndrome, thrombophlebitis, thrombosis and trophic changes up to acrogangrene, sometimes cold urticaria. The occurrence of vasomotor disorders is associated with the formation of large intravascular conglomerates of agglutinated erythrocytes during cooling, followed by spasm of the vascular wall. These changes are combined with increased predominantly intracellular hemolysis. In some patients, enlargement of the liver and spleen occurs. Moderately expressed normochromic or hyperchromic anemia, reticulocytosis, a normal number of leukocytes and platelets, an increase in ESR, a slight increase in the level of the free fraction of bilirubin, a high titer of complete cold agglutinins (detected by agglutination in a saline medium), and sometimes signs of hemoglobinuria are observed. Characteristic is the agglutination of erythrocytes in vitro, which occurs at room temperature and disappears when heated. If it is impossible to perform immunological tests, a provocative test with cooling takes on diagnostic significance (in the blood serum obtained from a finger tied with a tourniquet after lowering it into ice water, an increased content of free hemoglobin is determined).
With cold hemagglutinin disease, in contrast to paroxysmal cold hemoglobinuria, hemolytic crisis and vasomotor disturbances arise only from hypothermia of the body and hemoglobinuria, which began in cold conditions, ceases when the patient moves to a warm room.
The symptom complex characteristic of cold hemagglutinin disease can occur against the background of various acute infections and some forms of hemoblastosis. In idiopathic forms of the disease, complete recovery is not observed; in symptomatic forms, the prognosis depends mainly on the severity of the underlying process.
Paroxysmal cold hemoglobinuria is one of the rare forms of hemolytic anemia. It affects people of both sexes, most often children.
Patients with paroxysmal cold hemoglobinuria may experience general malaise, headache, body aches and other unpleasant sensations after exposure to cold. Following this, chills begin, the temperature rises, nausea and vomiting are noted. Urine turns black. At the same time, jaundice, enlarged spleen and vasomotor disturbances are sometimes detected. Against the background of a hemolytic crisis, patients exhibit moderate anemia, reticulocytosis, increased content of the free fraction of bilirubin, hemosiderinuria and proteinuria.
The final diagnosis of paroxysmal cold hemoglobinuria is established on the basis of the detected biphasic hemolysins using the Donath-Landsteiner method. It is not characterized by autoagglutination of erythrocytes, which is constantly observed in cold hemagglutination disease.
Hemolytic anemia caused by erythropsonins. The existence of autoopsonins to blood cells is generally accepted. In acquired idiopathic hemolytic anemia, liver cirrhosis, hypoplastic anemia with a hemolytic component and leukemia, the phenomenon of autoerythrophagocytosis was discovered.
Acquired idiopathic hemolytic anemia, accompanied by the positive phenomenon of autoerythrophagocytosis, has a chronic course. Periods of remission, sometimes lasting a considerable time, are replaced by a hemolytic crisis, characterized by icterus of the visible mucous membranes, darkening of the urine, anemia, reticulocytosis and an increase in the indirect fraction of bilirubin, sometimes an enlargement of the spleen and liver.
In idiopathic and symptomatic hemolytic anemia, the detection of autoerythrophagocytosis in the absence of data indicating the presence of other forms of autoimmune hemolytic anemia gives grounds to classify them as hemolytic anemia caused by erythropsonins. The diagnostic test of autoerythrophagocytosis is carried out in direct and indirect versions.
Immunohemolytic anemia caused by drug use. Various medicinal drugs (quinine, dopegit, sulfonamides, tetracycline, ceporin, etc.), capable of causing hemolysis, form complexes with specific heteroantibodies, then settle on erythrocytes and add complement, which leads to disruption of the erythrocyte membrane. This mechanism of drug-induced hemolytic anemia is confirmed by the detection of complement on the erythrocytes of patients in the absence of immunoglobulins on them. Anemia is characterized by an acute onset with signs of intravascular hemolysis (hemoglobinuria, reticulocytosis, increased content of the free bilirubin fraction, increased erythropoiesis). Acute renal failure sometimes develops against the background of a hemolytic crisis.
Hemolytic anemias that develop when penicillin and methyldopa are prescribed proceed somewhat differently. Administration of 15,000 or more units of penicillin per day can lead to the development of hemolytic anemia, characterized by intracellular hyperhemolysis. Along with the general clinical and laboratory signs of hemolytic syndrome, a positive direct Coombs test is also detected (the detected antibodies are classified as IgG). Penicillin, by binding to the red blood cell membrane antigen, forms a complex against which antibodies are produced in the body.
With long-term use of methyldopa, some patients develop hemolytic syndrome, which has features of the idiopathic form of autoimmune hemolytic anemia. The detected antibodies are identical to warm agglutinins and belong to IgG.
Hemolytic anemia caused by mechanical factors is associated with the destruction of red blood cells as they pass through altered vessels or through artificial valves. The vascular endothelium changes in vasculitis, malignant arterial hypertension; At the same time, platelet adhesion and aggregation are activated, as is the blood coagulation system and thrombin formation. Widespread blood stasis and thrombosis of small blood vessels (DIC syndrome) develop with traumatization of red blood cells, as a result of which they fragment; Numerous fragments of red blood cells (schistocytes) are found in the blood smear. Red blood cells are also destroyed when they pass through artificial valves (more often during multivalve correction); Hemolytic anemia has been described in the setting of a senile calcified aortic valve. The diagnosis is based on signs of anemia, an increase in the concentration of free bilirubin in the blood serum, the presence of schistocytes in a peripheral blood smear and symptoms of the underlying disease that caused mechanical hemolysis.
Less common in clinical practice is hemolytic anemia caused by exposure to lead, poisoning with acids, snake venoms or vitamin E deficiency, as well as intracellular parasites. Hemolytic anemia develops, for example, after a snake bite, accidental or intentional (suicide) ingestion of acetic acid, upon contact with lead vapor, against the background of malaria. Anemia is normocytic, normochromic, regenerative in nature; in the blood serum the content of the free fraction of bilirubin and iron is increased.
Hemolytic-uremic syndrome (Moschkovich's disease, Gasser's syndrome) can complicate the course of autoimmune hemolytic anemia. A disease of an autoimmune nature is characterized by hemolytic anemia, thrombocytopenia, and kidney damage. Disseminated damage to blood vessels and capillaries is noted, involving almost all organs and systems, and pronounced changes in the coagulogram characteristic of DIC syndrome.
Symptoms
With hemolytic anemia, the symptoms are pronounced and look like this:
- the skin and mucous membranes of the mouth and eyes become pale or jaundiced (as a result of the presence of breakdown products of blood cells in the body);
- heart rate increases;
- there is general weakness in the body, fatigue, shortness of breath;
- the liver and spleen enlarge;
- The level of bilirubin increases and jaundice develops (the skin, whites of the eyes, saliva and tear fluid become lemon-colored);
- body temperature rises, attacks of dizziness appear;
- sometimes there is a disorder of consciousness and muscle cramps;
- a characteristic symptom is an increase in blood density, as a result of which there is poor blood circulation, oxygen saturation is poor, blood clots form, and the blood supply to internal organs is disrupted.
3. Symptoms and diagnosis
Autoimmune lysis of red blood cells can begin suddenly and end just as suddenly, without any intervention. In other cases, the disease develops gradually and remains asymptomatic for a long time.
There is also a steadily progressive course, for example, with the patient’s increased sensitivity to cold.
The most typical symptoms of autoimmune hemolytic anemia are “unreasonable” (actually caused by tissue hypoxia) fatigue, weakness, palpitations, shortness of breath, an uncomfortable feeling of heaviness in the left hypochondrium (splenomegaly occurs, the predominant destruction of red blood cells occurs in the spleen).
Sometimes there is pain in the heart and/or lower back, nausea and frequent vomiting. With more severe pathology, jaundice is observed. Some pathogenetically different types of the disease lead to “black urine syndrome”; in the clinic of others, an angiospastic response to cold is formed and secondary Raynaud’s syndrome, cold urticaria or, in the most severe disorders of tissue trophism in the extremities, acrogangrene develops.
Suspicion of hemolytic anemia arises, as a rule, in the presence of an appropriate clinical picture and complaints, as well as a characteristic medical history (risk factors, see above). However, the final diagnosis is established and confirmed by a thorough, most often multiple laboratory blood test (direct and indirect Coombs tests, general clinical, biochemical analysis, etc.).
About our clinic Chistye Prudy metro station Medintercom page!
Diagnostics
To determine hemolytic anemia, diagnosis is carried out as follows:
- an analysis of complaints is carried out: how long have symptoms such as weakness, general malaise of the body been observed. What color is the skin (yellowness indicates anemia)? What color is the mucous membrane of the eye whites, is there any darkening of the urine;
- an analysis of the disease history is carried out: whether this disease has been observed in one of the relatives, whether the body has been exposed to the influence of chemicals, whether there are any diseases of the blood or immune system;
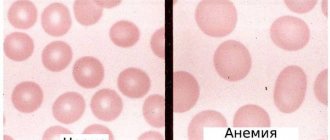
- clinical blood test - to determine the level of hemoglobin and red blood cells in the blood;
Anemia - symptoms and treatment
Treatment should first of all be aimed at identifying and eliminating the root cause, so therapy for anemia lasts a long time, often accompanied by several medical specialists.
Indication for treatment
The indication for drug treatment is a decrease in hemoglobin levels to less than 120 g/l in women and below 130 g/l in men.
Basically, treatment involves restoring hemoglobin reserves, increasing the number of red blood cells, and normalizing hematocrit. The main effective method of treating iron deficiency anemia is the use of iron supplements orally or parenterally (intravenously or intramuscularly)
To restore the hemoglobin level in a patient with iron deficiency anemia, the dose of ferrous iron per day (only it is effectively absorbed) must be 100-300 mg, taking into account depleted iron reserves (about 1.5 g).
| Drug name | Components included in the drug | Fe dosage, mg | Dosage form of release | Daily dose, g |
| Conferon | succinic acid | 50 | Pills | 3-4 |
| Heferol | Fumaric acid | 100 | Capsules | 1-2 |
| Hemophere prolongatum | Ferrous sulfate | 105 | Dragee | 1-2 |
| Ferrogradumet | Plastic matrix - gradation | 105 | Pills | 1-2 |
| Aktiferrin | D, L-serine | 113,8 34,8 | Capsules Syrup | 1-2 1 teaspoon per 12 kg body weight |
| Ferroplex | Ascorbic acid | 10 | Dragee | 8-10 |
| Sorbifer Durules | Ferrous sulfate + Ascorbic acid | 100 | Pills | 1-2 |
| Tardiferon | Ferrous sulfate + mucoprotease | 80 | Pills | 1-2 |
| Fenyuls | Ascorbic acid, nicotinamide, B vitamins | 50 | Capsules | |
| Irovit | The same + ascorbic acid, cyanocobalamin, L-lysine | 100 | Capsules | 1-2 |
| Irradian | Ascorbic acid, folic acid, cyanocobalamin, L-cysteine, D-fructose, yeast | 100 | Dragee | 1-2 |
It is more effective to prescribe drugs with a higher content of ferrous iron; they should be taken orally (by mouth) 1-2 times a day. This is the most convenient approach for patients, and therefore their adherence to therapy increases. Many dosage forms of iron include ascorbic and succinic acids, fructose, cysteine, etc., they help the best absorption of iron in the gastrointestinal tract. Iron supplements are best tolerated if taken with food.
Treatment of iron deficiency anemia with parenteral forms of iron supplements
There are clear indications for such therapy:
- with impaired absorption from the intestine (absorption deficiency syndrome, resection of the small intestine, enteritis, etc.);
- exacerbation of chronic diseases of the gastrointestinal tract, such as peptic ulcer of the stomach or duodenum, Crohn's disease, ulcerative colitis;
- poor tolerance to iron-containing drugs when taken orally;
- if you need to quickly replenish iron reserves in the body.
For parenteral administration, iron preparations are used, such as Ferinject (intravenous), Ektofer (intramuscular), Ferbitol (intramuscular), Ferrum Lek (intramuscular, intravenous), Ferkoven (intravenous) [2].
Regarding the treatment of postpartum anemia, there are no clear conclusions about methods. Studies have shown that oral iron does not have a significant benefit over intravenous iron or placebo. However, oral iron does not cause life-threatening allergic reactions like intravenous iron. The clinical value of blood transfusion remains uncertain, in part because of the risks involved. This method can be used to treat postpartum anemia in cases of acute or severe bleeding during childbirth. However, it is not recommended after minor to moderate bleeding in stable patients with mild or asymptomatic anemia. In any case, it is necessary to assess the severity of anemia and consider the use of an iron-rich diet as a method of prevention and adjunct to treatment [7].
Iron deficiency anemia is the most common type of anemia. However, treatment for other types of anemia differs from treatment for IDA. With other types of anemia, to normalize blood counts, it is necessary, for example, to replenish vitamin B12, folic acid, control concomitant chronic diseases and other factors that were the root cause of anemia. To do this, you need a timely visit to a doctor who will diagnose and determine management tactics.
How to improve treatment. Diet
For all types of anemia, the diet should include foods high in iron: pork and beef liver, veal, beef, buckwheat, green apples, pomegranates, mushrooms, cabbage, beans and other legumes, dark chocolate, etc.
You need to eat 4-6 times a day. For normal digestion, food should be at room temperature; too cold or too hot food irritates the gastric mucosa, which prevents the absorption of beneficial elements. The amount of water you drink per day is 30 ml per 1 kg of weight, including tea, juice, soup, etc. Drinking alcohol and smoking are strictly prohibited. Alcohol not only negatively affects the health of the gastrointestinal tract, but also washes out beneficial components in the urine, which is harmful even for healthy people. Smoking increases stomach acidity, which can cause gastritis or ulcers. In this case, the absorption of beneficial microelements will be impaired.
For iron deficiency anemia, it is necessary to include fermented foods (kefir, kvass, sauerkraut, etc.). The acid contained in such products easily comes into contact with iron and prevents the formation of poorly absorbed iron phytates, resulting in improved penetration of iron into enterocytes (cells lining the inner surface of the intestine). The formation of iron phytates is also reduced if plant products are crushed or cooked [10].
Daily iron supplementation in menstruating women is an effective clinical public health strategy for alleviating anemia and iron deficiency, as well as increasing hemoglobin and iron stores. Daily iron supplementation also improves physical performance in women. In addition, there is evidence that iron supplementation reduces fatigue [8].
Daily oral iron and folic acid supplementation of 30–60 mg elemental iron and 400 μg (0.4 mg) folic acid is recommended for pregnant women to prevent anemia, puerperal sepsis, preterm birth, and low birth weight [9].
Contraindications for anemia
For anemia, strict diets are contraindicated; the diet should include foods high in iron, vitamin B12 and folic acid. The development of anemia is also possible while taking certain medications (antitumor drugs, a number of antibacterial, antiprotozoal, antiviral, anti-inflammatory, antirheumatic, antiepileptic and antipsychotic drugs). Therefore, taking this group of drugs for anemia should be under the supervision of a specialist.
Is it possible to treat anemia with folk remedies?
To date, there are no effective folk remedies for treating anemia, because correction of iron deficiency cannot be achieved only by changing diet or using any herbs, decoctions and juices. The reason for this is that the absorption of iron from food is limited (no more than 3-5% from plant foods), and in medications it is contained in higher concentrations.
Treatment
For hemolytic anemia, treatment is carried out using the following methods:
- medications are prescribed, such as glucocorticosteroids, which relieve inflammation and immunosuppressants (prescribed in case of a malfunction in the immune system, to suppress autoimmune reactions);
- if the disease is based on a lack of enzymes in red blood cells, then the missing enzymes are prescribed to be taken with medication;
- if the disease occurs due to the destruction of red blood cells in the spleen, then surgical removal of the spleen is prescribed - splenectomy;
- plasmapheresis is a procedure based on the removal of plasma from the blood, which contains toxic substances and metabolic breakdown products;
- transfusion of purified donor red blood cells. Purification involves removing foreign protein from the surface of red blood cells;
- bone marrow transplantation.
Hereditary hemolytic anemia caused by impaired activity of erythrocyte enzymes
Differential diagnosis of enzyme deficiency hemolytic anemia with various diseases depends on the clinical signs of the disease. The first stage of diagnosis is to clarify the nature of hyperbilirubinemia associated with an increase in free, indirect bilirubin; Enzyme deficiency anemia must be differentiated from Gilbert's disease and mild forms of chronic hepatitis.
Hemolytic anemia is characterized by an enlarged spleen, irritation of the red sprout of the bone marrow, reticulocytosis, changes in the morphology of erythrocytes, sometimes a decrease in hemoglobin levels, and a shortening of the lifespan of erythrocytes. In Gilbert's disease there are no signs of increased destruction of red blood cells and impaired liver function.
Comparative diagnosis of hereditary hemolytic anemia and chronic hepatitis causes significant difficulties. Although in hepatitis both direct and indirect bilirubin are often increased, in some cases of chronic or incompletely resolved acute hepatitis, bilirubin is increased mainly due to indirect bilirubin. Differential diagnostic difficulties increase when the spleen is enlarged due to hepatitis, especially if chronic hepatitis is accompanied by autoimmune hemolytic anemia.
A study of the functional state of the liver, and, if necessary, a liver examination helps to establish an accurate diagnosis.
It is necessary to distinguish between hereditary dyserythropoietic and hemological anemia. Dyserythropoietic anemia is accompanied by hyperbilirubinemia due to an increase in the indirect fraction, an enlarged spleen, and, unlike hemolytic anemia, a normal level of reticulocytes. In the bone marrow, a sharp predominance of red cells and a large number of binucleate erythrokaryocytes are found.
The second stage of diagnosis is the differentiation of various types of hemolytic anemia. To exclude hemolytic anemia caused by a membrane defect of erythrocytes (microspherocytosis, elliptocytosis, stomatocytosis, acanthocytosis), it is necessary to study the morphology of erythrocytes.
To make a correct diagnosis, the doctor is most helped by studying the type of inheritance of the disease. It should be noted that forms of hemolytic anemia caused by a defect in membrane proteins, for example microspherocytosis, stomatocytosis, are transmitted in a dominant manner, and most enzyme-deficiency hemolytic anemias are recessive.
Inheritance of deficiency of the enzyme glucose-6-phosphate dehydrogenase is linked to the X chromosome, so mainly men suffer from this form of hereditary pathology. When differential diagnosis with hemoglobinopathies, it should be borne in mind that these forms of anemia are inherited codominantly and in hemoglobinopathies associated with the carriage of unstable hemoglobins, the disease is clinically manifested in heterozygous carriers and, therefore, is transmitted from generation to generation.
It is quite difficult for a doctor to establish an accurate diagnosis for hereditary hemolytic anemia, characterized by a deficiency of enzyme activity, and autoimmune hemolytic anemia. With enzyme deficiency hemolytic anemia, it is not always possible to identify another family member suffering from this hereditary disease.
The most important criterion for the disease is laboratory detection of an enzyme defect in red blood cells. There are rapid methods for identifying deficiency of glucose-6-phosphate dehydrogenase activity. When a deficiency is detected using the rapid method, a quantitative test of activity is necessary to confirm the diagnosis.
Prevention
In case of hereditary predisposition, it is necessary to consult a geneticist at the pregnancy planning stage and determine the Rh factor of the blood in advance. It is recommended to take measures to strengthen the immune system, namely:
- proper fractional nutrition;
- rejection of bad habits;
- maintaining a sleep schedule;
- staying in the fresh air;
- consumption of vitamins in the autumn-winter period.
If any of these symptoms are detected, you should consult a hematologist. He will help you choose a treatment regimen based on the characteristics of your body. A wide selection of drugs is also available on our portal. You can quickly find the drug you need in the “Pharmacy” section.