09/15/2021 Non-steroidal anti-inflammatory drugs (NSAIDs or NSAIDs) are widely used against inflammatory processes in the body. Medicines are sold in tablet form, capsules, and dosage forms for external use. They not only have an anti-inflammatory effect, but also reduce temperature and also relieve pain.
The drugs have contraindications and side effects, so the doctor must select them, taking into account the individual characteristics and condition of the patient.
Introduction
Nonsteroidal anti-inflammatory drugs (NSAIDs) are among the most commonly used medications, both among prescription drugs and among over-the-counter drugs, i.e., used by patients themselves for self-medication without prescription. The frequency of use of NSAIDs in clinical practice is due to the spectrum of their pharmacological effects: analgesic, anti-inflammatory, antipyretic, antiaggregation (acetylsalicylic acid). However, a wide range of therapeutic effects and high clinical effectiveness also have a downside: NSAIDs are among the group of drugs that most often cause adverse drug reactions (ADRs) associated with toxic effects, hypersensitivity, drug and food interactions. Therefore, the clinician faces a difficult task: selecting NSAIDs for a specific patient.
The choice of drug is carried out according to a certain algorithm.
- Determination of indications for use of a medicinal product , which is determined by the clinical diagnosis of the patient: the underlying disease, the presence of comorbid pathology, complications, concomitant diseases. Of great importance is the assessment of risk factors for the development of complications of drug therapy: allergy history; previously identified symptoms of drug intolerance; concomitant therapy, including the use of herbal remedies, vitamin preparations, over-the-counter medications, dietary supplements; the patient's dietary preferences, alcohol abuse, smoking.
- Having determined the indication (“problem” of the patient), the doctor selects a group of drugs and a specific drug within this group, based on the criteria of effectiveness, safety, cost and ease of use.
- Having decided on the choice of a specific drug, the doctor chooses the mode of use of the drug: dose, frequency of use, duration of therapy.
- The doctor explains to the patient in an accessible form what is wrong with him and why the symptoms that bother him appeared, provides information about possible non-drug methods for correcting the pathological condition, explains to the patient why this drug was chosen and what the patient should pay attention to when using this drug, if any symptoms, he should immediately consult a doctor and even stop taking the drug. Almost 50% of cases of ineffective pharmacotherapy are due to low patient compliance, which is why it is so important to achieve cooperation with the patient and his compliance with the drug therapy regulations.
- During the treatment process, the doctor himself evaluates the effectiveness and safety of the pharmacotherapy being carried out, decides on the indications for prescribing protective therapy, stopping/prolonging treatment when the goal is achieved, or changing the drug if it is ineffective.
The implementation of this algorithm is possible only if the doctor is well aware of the indications for use and the clinical and pharmacological properties of the selected drug.
A few words about the disease
Osteochondrosis is a disease of the spine, which is a disorder of the structure of joints, bones or intervertebral discs. This disease is one of the most common problems among people of all ages. In half of the cases, the age of people who were diagnosed with osteochondrosis is more than forty-five years.
There are four types of osteochondrosis:
- cervical osteochondrosis;
- thoracic osteochondrosis;
- osteochondrosis of the lumbosacral region;
- common osteochondrosis
The latter type of disease is characterized by the fact that it affects not one, but several parts of the spine at once. Treatment of this type of disease is more complex and requires comprehensive measures to treat all affected areas. Fortunately, this type of osteochondrosis is the least common.
Osteochondrosis is a dangerous disease that greatly affects human health.
Most often, osteochondrosis appears in the cervical region (since this region is the most mobile), a little less often - in the lumbar region (this region is subjected to frequent physical activity). The least common, but also the most dangerous, is osteochondrosis of the thoracic region, since the symptoms of the disease are initially absent and are more difficult to notice.
Osteochondrosis, like any disease, has several stages of development.
Table No. 1. Stages of osteochondrosis.
Features of the use of NSAIDs in clinical practice
As mentioned above, the main pharmacodynamic effects of NSAIDs are: analgesic, anti-inflammatory, antipyretic. Thus, drugs in this group are used for diseases of the musculoskeletal system, joints, postoperative pain, tension headaches, migraines, dysmenorrhea, renal and hepatic colic, chronic pain syndrome, colds, and fever.
The effectiveness of a drug is determined by a number of factors: the mechanism of action, bioavailability (the percentage of the dose taken that enters the systemic circulation), metabolic characteristics, concentration in the blood and tissues of the body, the rate of development of the therapeutic effect and the duration of its retention. The safety of using a drug depends on the mechanism of action and characteristics of metabolism, excretion of the drug, and its ability to enter into drug interactions.
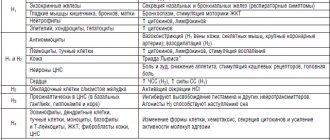
The mechanism of action of NSAIDs is due to their ability to inhibit the enzyme cyclooxygenase-2 (COX-2) at the site of inflammation (Fig. 1). It is COX-2 that takes part in the formation of pro-inflammatory prostaglandins, which potentiate the activity of inflammatory mediators (histamine, serotonin, bradykinin) that activate pain receptors; participate in controlling the activity of the thermal regulation center, promote cell proliferation, mutagenesis and destruction [1, 2]. At the same time, NSAIDs also block cyclooxygenase-1 (COX-1), which is present in all organs and ensures normal physiological processes (synthesis of protective stomach mucus, some stages of hematopoiesis, filtration and reabsorption in the kidneys). There is also “constitutive” COX-2, which is found in high concentrations in the brain, bones, organs of the female reproductive system, and kidneys, ensuring their normal functioning.
Additional mechanisms of anti-inflammatory action of NSAIDs are:
- inhibition of interleukin-1 synthesis activity;
- suppression of neutrophil function and interaction of leukocytes with the vascular endothelium;
- inhibition of activation of NF-kB (transcription factor), which regulates the synthesis of “pro-inflammatory” mediators;
- activation of PPARs (peroxisoma proliferator activated receptors).
- A decrease in the synthesis of “beneficial” prostanoids underlies the mechanisms of development of ADRs when using NSAIDs.
NSAIDs can be divided into two groups: non-selective COX inhibitors (ibuprofen, diclofenac, naproxen, etc.) and selective, predominantly inhibiting COX-2 (meloxicam, nimesulide, coxibs). When using drugs of the second group, NSAID gastropathy and NSAID enteropathy, gastrointestinal bleeding develop much less frequently, but the risk of complications from the cardiovascular system increases [1]. The effect of NSAIDs increases with increasing dose of the drug, while at maximum doses the selectivity of the action of selective NSAIDs decreases (Fig. 2) [3].
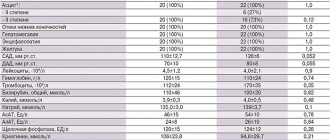
It should also be noted that when using medium and high doses of various NSAIDs, their effectiveness is comparable, which follows from the results of multicenter clinical studies that compared the analgesic and anti-inflammatory effects of NSAIDs in injuries, operations and diseases of the musculoskeletal system. Thus, a meta-analysis of data from 29 randomized clinical trials (n=18,000) assessed the effectiveness of various NSAIDs in osteoarthritis. The differences in pain reduction (in visual analogue scale millimeters) between NSAIDs and placebo were:
- for naproxen 1000 mg/day - 12.9 (95% confidence interval (CI) - 8.2–17.7),
- ibuprofen 2400 mg/day - 9.0 (95% CI 5.0–13.1),
- diclofenac - 16.2 (95% CI 11.7–20.6),
- celecoxib 200 mg – 14.7 (95% CI 12.1–17.3),
- etoricoxib 30 mg – 14.2 (95% CI 12.6–16.8),
- etoricoxib 60 mg – 16.2 (95% CI 12.7–19.8) [4].
There is an opinion that intravenous or intramuscular administration of the drug provides a faster and more pronounced therapeutic effect than taking the drug orally. However, this position is not confirmed by data from clinical studies [5]. A systematic review of 26 RCTs (n=2225) analyzed the effectiveness of NSAIDs administered parenterally, rectally, or orally. Indications for the prescription of NSAIDs were musculoskeletal diseases, postoperative pain, dysmenorrhea, and renal colic. There were no significant differences in the analgesic effect of various dosage forms of NSAIDs, with the exception of renal colic, in which a significant advantage of intravenous NSAIDs compared with oral administration was shown [6].
Thus, the following conclusions can be drawn [1].
- All NSAIDs in adequate anti-inflammatory (average and maximum) doses with long-term use have equal analgesic potential (evidence level 1a).
- The effectiveness of NSAIDs depends on the dose. The use of higher doses provides more pronounced analgesic and anti-inflammatory effects (evidence level 1b).
- There is no evidence that injectable or rapidly dissolving oral NSAIDs are superior to oral NSAIDs for longer than 1 day of treatment (LE: 1b).
Risk of adverse drug reactions when using NSAIDs
Since the effectiveness of NSAIDs in therapeutic doses is comparable, when choosing NSAIDs for a particular patient, we proceed from the possible risks of developing ADRs (Table 1) [1]. Risk factors for the development of ADRs when using NSAIDs are: age over 60 years, overweight, smoking, history of gastric and duodenal ulcers, history of venous thrombosis and thromboembolism, coronary artery disease, cerebrovascular disease, peripheral atherosclerosis, arterial hypertension, lipid metabolism disorders , diabetes mellitus, diseases of the intestines, liver, kidneys, blood, congestive heart failure, chronic alcohol intoxication, combined use of medications that interact with NSAIDs, lactation. For a more differentiated selection of NSAIDs, a special algorithm was proposed, which involves the prescription of selective NSAIDs to patients with risk factors for developing gastrointestinal complications and the use of NSAIDs with a less pronounced toxic effect on the cardiovascular system in patients with high cardiovascular risk, as well as the prescription protective therapy (Table 2) [1].
According to Russian recommendations for the rational use of NSAIDs:
- the main method of preventing the development of ADRs when using NSAIDs is taking into account risk factors, their correction (if possible) and prescribing NSAIDs with a more favorable gastrointestinal (recommendation grade A) and cardiovascular safety profile (recommendation grade B);
- an additional method of preventing complications from the upper gastrointestinal tract is the prescription of proton pump inhibitors (PPIs) (grade of recommendation A);
- an additional method for preventing complications from the upper gastrointestinal tract, small and large intestine can be the prescription of rebamipide (gradation of recommendation B);
- There are no effective drug methods of nephro- and hepatoprotection to reduce the risk of NSAID-associated complications.
Safety of using a combination of ibuprofen and paracetamol
It was already noted above that ibuprofen in moderate therapeutic doses (600–1200 mg/day) has low gastrotoxicity [17]. Paracetamol is a centrally acting analgesic and does not cause NSAID gastropathy. Table 4 presents a comparison of the activity of a number of NSAIDs in relation to the selectivity of COX-1/COX-2.
If we talk about the risk of developing cardiovascular complications when using a combination of paracetamol and ibuprofen, it is also low (Table 5) [18, 19]. However, it should be remembered that ibuprofen reduces the antiplatelet effect of acetylsalicylic acid and their combined use is not recommended [20].
The use of a combination of ibuprofen and paracetamol is contraindicated: with hypersensitivity to ibuprofen, paracetamol or other components of the drug, with simultaneous use of other drugs containing paracetamol, with complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses, with intolerance to acetylsalicylic acid or other NSAIDs, erosive - ulcerative diseases of the gastrointestinal tract, ulcerative bleeding (in the active phase or in history), perforation of a gastrointestinal ulcer provoked by taking NSAIDs, severe heart failure, severe liver failure or liver disease in the active phase. The combination of ibuprofen and paracetamol is not prescribed to patients with severe renal failure (creatinine clearance less than 30 ml/min), with confirmed hyperkalemia, decompensated heart failure and during coronary artery bypass surgery, with cerebrovascular or other bleeding, in the third trimester of pregnancy, with hemophilia and others bleeding disorders and hemorrhagic diathesis, as well as the genetic absence of glucose-6-phosphate dehydrogenase. The combination of ibuprofen and paracetamol is contraindicated in persons under 18 years of age [9].
In general, the combination of ibuprofen and paracetamol is well tolerated, ADRs are rare, usually mild and comparable in frequency to placebo (Fig. 5) [13].
![Table 1. Dynamics of publications on clinical trials of piracetam and piracetam-like drugs over four time periods [5, with additions]](https://laram-halal.ru/wp-content/uploads/tablica-1-dinamika-publikacij-posvyashchennyh-klinicheskim-ispytaniyam-piracetama-i-piracetamopodobnyh2-330x140.jpg)
![Table 1. Dynamics of publications on clinical trials of piracetam and piracetam-like drugs over four time periods [5, with additions]](https://laram-halal.ru/wp-content/uploads/tablica-1-dinamika-publikacij-posvyashchennyh-klinicheskim-ispytaniyam-piracetama-i-piracetamopodobnyh-330x140.jpg)