Composition and release form
Several companies are involved in the production of the drug. Regardless of the manufacturer, all drugs have the same active ingredient, the same indications, contraindications and adverse reactions.
Available in the following forms:
- pills;
- effervescent tablets;
- syrup.
The active ingredient is loratadine. 1 tablet (including effervescent) contains 10 mg of active ingredient, 5 ml of syrup - 5 mg.
In addition to the active component, the syrup contains other excipients: citric acid, ethanol, water, glycerin, flavoring.
Additional components in the tablets are: corn starch, microcrystalline cellulose, calcium stearate.
Effervescent tablets additionally contain: citric acid, lactose, sodium carbonate, silicon dioxide.
Popular questions about Loratadine
How to take Loratadine?
Adults and adolescents over 12 years of age are prescribed orally - one tablet once a day. Eating does not affect the therapeutic effect of the medication. The medicine is swallowed and washed down with water. The dose for children aged two to twelve years is calculated based on the child’s weight: Children whose weight exceeds 30 kg take one tablet once a day. Children with lower weights use Loratadine in syrup.
How long can you take Loratadine?
The medicine is taken in long-term yearly courses, if there are no contraindications to the patient’s administration and no side effects.
How long does it take for Loratadine to work?
one to three hours after administration by the patient and persists for 24 hours.
Where can you buy Loratadine?
The medication is sold in branches of the retail pharmaceutical network 9-1-1, which has 950 pharmacies in cities and regions of Ukraine, or the medicine can be booked on the 9-1-1 Pharmacy website and purchased at the pharmacy closest to your place of residence or convenient for you.
Effect of the drug
The allergy medicine blocks histamine-sensitive receptors, which prevents them from being released from mast cells. As a result, the allergic reaction recedes or the symptoms of its manifestation are alleviated. After taking Loratadine, swelling and itching decrease. In addition, the product allows you to relax spasmodic smooth muscles.
The first noticeable result can be seen 30-40 minutes after administration. The maximum effect is achieved after 8-10 hours and lasts for a day. The components do not depress the central nervous system and are not addictive.
Choosing an antihistamine: a pharmacologist's view
For citation. Kareva E.N. Choosing an antihistamine: a pharmacologist’s view // RMJ. 2016. No. 12. pp. 811–816.
Antihistamines (AGDs) are the first line of treatment for most allergic diseases.
They are predominantly over-the-counter products; they have long been firmly established in our practice and have been used for more than half a century. Often the choice of these drugs is carried out empirically or even left to the patients, but there are many nuances that determine how effective a particular drug will be for a particular patient, which means that the choice of these drugs must be approached no less responsibly than, for example, the choice antibiotics. Each specialist in his clinical practice has probably encountered situations when a particular drug did not have the desired clinical effect or caused hyperergic reactions. What does this depend on and how can you minimize the risks? Variability in response to a drug is most often associated with the activity of metabolic enzymes in the patient’s liver; the situation is aggravated in the case of polypharmacy (5 or more prescribed drugs at the same time). Therefore, one of the real ways to reduce the risk of an inadequate response of the body to a drug is to choose a drug that is not metabolized in the liver. In addition, when choosing an antihypertensive, it is important to evaluate the following parameters: the strength and speed of onset of the effect, the possibility of long-term use, the benefit/risk ratio (efficacy/safety), ease of use, the possibility of use for concomitant pathology in combination with other drugs in a given patient, the route of elimination , need for dose titration, price. To solve this problem, consider the current information on histamine and antihistamines. Histamine and its role in the body
Histamine in the human body performs a number of physiological functions, plays the role of a neurotransmitter and is involved in many pathobiological processes (Fig. 1).
The main depot of histamine in the body is mast cells and basophils, where it is found in the form of granules in a bound state. The largest number of mast cells are localized in the skin, mucous membranes of the bronchi and intestines. Histamine realizes its activity exclusively through its own receptors. Modern ideas about the functional load of histamine receptors, their localization and mechanisms of intracellular signaling are shown in Table 1.
In addition to physiological functions, histamine is involved in the development of an inflammatory process of any nature. Histamine causes itching, sneezing and stimulates secretion of the nasal mucosa (rhinorrhea), contraction of smooth muscles of the bronchi and intestines, tissue hyperemia, dilatation of small blood vessels, increased vascular permeability to water, proteins, neutrophils, and the formation of inflammatory edema (nasal congestion). Not only with allergic diseases, but also with any pathological processes with a pronounced inflammatory component, the level of histamine in the body is always increased. This is indicated for chronic infectious and inflammatory diseases of the respiratory and urogenital tracts, acute respiratory viral infections, and influenza [1–3]. Moreover, the daily amount of histamine in urine during influenza is approximately the same as during exacerbation of allergic diseases. Therefore, a pathogenetically justified and clinically useful step is to reduce the activity of the histamine system in conditions of its increased activity. In principle, the histaminergic activity of the body can be suppressed either through a decrease in the amount of free histamine (inhibition of synthesis, activation of metabolism, inhibition of release from the depot), or through blockade of histamine receptor signals. In clinical practice, drugs have been used that stabilize mast cell membranes, thereby preventing the release of histamine. However, when using them, you have to wait a long time for the desired effect to occur, and the therapeutic effectiveness of this group of drugs is very moderate, so they are used exclusively for prophylactic purposes. A quick and pronounced effect is achieved when using antihistamines.
Classification of antihistamines
According to the classification adopted by the European Academy of Allergists and Clinical Immunologists, all antihistamines are divided into 2 generations depending on their effect on the central nervous system.
First-generation antihistamines
H1-antagonists of the first generation penetrate the blood-brain barrier (BBB) and can both stimulate and suppress the functioning of the central nervous system (Fig. 2). As a rule, the latter happens in most patients. A sedative effect when taking first generation AGPs is subjectively noted by 40–80% of patients. The lack of sedative effect in individual patients does not exclude the objective negative impact of these drugs on cognitive functions, which patients may not pay attention to (ability to drive, learn, etc.). Dysfunction of the central nervous system is observed even when using minimal doses of these drugs. The effect of first-generation antihypertensive drugs on the central nervous system is the same as when using alcohol and sedatives. Stimulation has been observed in some patients receiving conventional doses of antihypertensives and is manifested by restlessness, nervousness and insomnia. Typically, central excitation is characteristic of an overdose of first generation AGPs; it can lead to convulsions, especially in children.
When taking AGP of the first generation, in addition to the sedative effect and effect on cognitive functions, the following are observed: • short-term effect (forced use 3-4 times a day); • rapid development of tachyphylaxis (it is necessary to change the drug every 7–10 days); • low selectivity of action: in addition to histamine H1 receptors, they block acetylcholine, adrenaline, serotonin, dopamine receptors and ion channels, causing many side effects: tachycardia, dry mucous membranes, increased sputum viscosity. They can increase intraocular pressure, interfere with urination, cause stomach pain, constipation, nausea, vomiting, and increase body weight [4, 5]. That is why these drugs have a number of serious restrictions for use among patients with glaucoma, benign prostatic hyperplasia, cardiovascular pathology, etc. In acute poisoning of first generation AGPs, their central effects pose the greatest danger: the patient experiences agitation, hallucinations, ataxia, incoordination, convulsions, etc. Fixed, dilated pupils on a flushed face, together with sinus tachycardia, urinary retention, dry mouth and fever are very similar to signs of atropine poisoning. In children with an overdose of first-generation antihypertensive drugs, agitation and convulsions may occur, so experts in many countries are calling for the refusal of this group of drugs in the treatment of children or their use under strict supervision. In addition, sedation can impair children's learning and performance at school.
II generation antihistamines
New AGPs (II generation) do not penetrate the BBB and do not have a sedative effect (Fig. 2). Note: III generation drugs have not yet been developed. Some pharmaceutical companies present new drugs that have appeared on the pharmaceutical market as AGP III - the newest generation. They tried to classify metabolites and stereoisomers of modern AGPs as the third generation. However, it is currently believed that these drugs belong to the second generation AGPs, since there is no significant difference between them. According to the Consensus on Antihistamines, it was decided to reserve the name “third generation” to designate antihistamines synthesized in the future, which will differ from known compounds in a number of basic characteristics. Unlike older drugs, II generation AGPs practically do not penetrate the BBB and do not cause a sedative effect, so they can be recommended to drivers, people whose work requires concentration, schoolchildren and students. The term “practically” is used here, because in very rare cases and when taking second-generation drugs, cases of sedation are possible, but this is rather an exception to the rule and depends on the individual characteristics of the patient. Second-generation antihypertensives are capable of selectively blocking H1 receptors, quickly providing a clinical effect with a long-lasting effect (for 24 hours), and, as a rule, are not addictive (no tachyphylaxis). Due to their higher safety profile, they are preferred for elderly patients (over 65 years of age).
Antihistamines of the 2nd generation
Pharmacokinetic features Metabolism of AGPs of the 2nd generation
All AGPs of the 2nd generation are divided into 2 large groups, depending on the need for metabolic activation in the liver (Fig. 3).
The need for metabolic activation in the liver is associated with a number of problems, the main of which are the danger of drug interactions and the late onset of the maximum therapeutic effect of the drug. Concomitant use of two or more drugs that are metabolized by the liver may result in changes in the concentration of each drug. In the case of parallel use of an inducer of drug metabolism enzymes (barbiturates, ethanol, St. John's wort, etc.), the rate of antihistamine metabolism increases, the concentration decreases and the effect is not achieved or is weakly expressed. With the simultaneous use of liver enzyme inhibitors (antifungal azoles, grapefruit juice, etc.), the metabolic rate of AGP slows down, which causes an increase in blood levels and an increase in the frequency and severity of side effects. The most successful option for antihypertensive drugs are drugs that are not metabolized in the liver, the effectiveness of which does not depend on concomitant therapy, and the maximum concentration is achieved in the shortest possible time, which ensures a rapid onset of action. An example of such a second-generation antihypertensive drug is cetirizine.
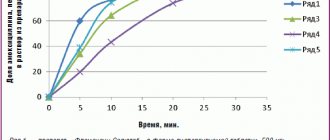
The speed of onset of the effect of AGP of the second generation
One of the most important aspects of the drug’s action is the speed of onset of the effect. Among the second generation AGPs, the shortest period of achieving Cmax was observed for cetirizine and levocetirizine. It should be noted that the antihistamine effect begins to develop much earlier and is minimal for drugs that do not require prior activation in the liver, for example, cetirizine - after 20 minutes (Table 2).
Distribution of II generation AGP
The next most important characteristic of a drug is the volume of distribution. This indicator indicates the predominant localization of the drug: in plasma, intercellular space or inside cells. The higher this indicator, the more the drug enters the tissues and inside the cells. The small volume of distribution indicates that the drug is predominantly located in the vascular bed (Fig. 4). For AGP, localization in the bloodstream is optimal because its main target cells (immunocompetent blood cells and vascular endothelium) are represented here.
The values of the volume of distribution (liter/kg) for II generation AGPs are as follows in increasing order: cetirizine (0.5) < fexofenadine (5.4–5.8) < desloratadine (49) < ebastine (100) < loratadine (119) (Fig. . 5). The small volume of distribution ensures: a) high concentrations of this AGP on the surface of target cells, therefore, precisely targeted action and high therapeutic efficacy; b) lack of accumulation in parenchymal organs and safety of use.
Features of pharmacodynamics
The pharmacological effects of antihypertensive drugs are mediated by histamine receptors, selectivity for different subtypes, the strength and duration of binding to which varies between drugs. A distinctive characteristic of the second generation AGP cetirizine is its high affinity - the ability to bind histamine H1 receptors for a long time: their occupancy 4 hours after taking the drug is 90%, after 24 hours - 57%, which exceeds similar indicators of other AGPs. The most important property of antihistamines is their ability to reduce the expression of histamine H1 receptors, thereby reducing the sensitivity of tissues to histamine [8, 9]. According to the strength of the antihistamine effect, second-generation antihistamines can be arranged in the following order: cetirizine >> ebastine > fexofenadine >> loratadine (Fig. 6) [10].
The antiallergic effect of individual antihypertensive drugs (cetirizine) includes the so-called additional, extra-H1-receptor effect, together with which the anti-inflammatory effect of the drug is realized. Side effects of AGP
Side effects of antihypertensive drugs include anticholinergic effects (dry mouth, sinus tachycardia, constipation, urinary retention, blurred vision), adrenolytic effects (hypotension, reflex tachycardia, anxiety), antiserotonin (increased appetite), central antihistamine effects (sedation, increased appetite), blockade potassium channels in the heart (ventricular arrhythmia, QT prolongation) [11]. The selectivity of the action of drugs on target receptors and the ability to penetrate or not penetrate the BBB determine their effectiveness and safety [12]. Among the second generation AGPs, the drugs cetirizine and levocetirizine have the lowest affinity for M-cholinergic receptors, and therefore an almost complete absence of anticholinergic action (Table 3) [13].
Some antihypertensive drugs that can cause AR are terfenadine and astemizole. Due to the ability to cause a potentially fatal arrhythmia - atrial fibrillation (metabolic disturbance due to liver disease or in the presence of CYP3A4 inhibitors), terfenadine and astemizole have been prohibited for use since 1998 and 1999. respectively. Among the currently available antihypertensive drugs, ebastine and rupatadine have cardiotoxicity and are not recommended for use in persons with a prolonged QT interval or hypokalemia. Cardiotoxicity increases when taken simultaneously with drugs that prolong the QT interval - macrolides, antifungals, calcium channel blockers, antidepressants, fluoroquinolones.
Cetirizine
Cetirizine occupies a special place among second generation drugs.
Along with all the advantages of non-sedating antihistamines, cetirizine demonstrates properties that distinguish it from a number of new generation drugs and ensure its high clinical efficacy and safety [5, 14]. In particular, it has additional antiallergic activity, a rapid onset of effect, and there is no risk of interaction with other drugs and food, which opens up the possibility of safely prescribing the drug to patients with concomitant diseases. The effect of cetirizine consists of its influence on both phases of allergic inflammation. The antiallergic effect includes the so-called extra-H1 receptor effect: inhibition of the release of leukotrienes, prostaglandins in the nasal mucosa, skin, bronchi, stabilization of mast cell membranes, inhibition of eosinophil migration and platelet aggregation, suppression of ICAM-1 expression by epithelial cells [7, 15] . Many authors, both foreign and domestic, consider cetirizine to be the standard of modern AGP. It is one of the most studied antihypertensive drugs, having proven its effectiveness and safety in many clinical studies. For patients who respond poorly to other antihypertensive drugs, cetirizine is recommended [16]. Cetirizine fully meets the requirements for modern antihypertensive drugs [17]. Cetirizine is characterized by a half-life of 7–11 hours, the duration of the effect is 24 hours, after a course of treatment the effect lasts up to 3 days, with long-term use – up to 110 weeks, no addiction is observed. The duration of the effect of cetirizine (24 hours) is explained by the fact that the effect of AGP is determined not only by the plasma concentration, but also by the degree of binding to plasma proteins and receptors. Cetirizine is practically not metabolized in the liver and is excreted primarily by the kidneys, so it can be used even in patients with impaired liver function. But for patients with renal failure, a dose adjustment of the drug is required. Cetrin is an effective, high-quality generic cetirizine at an affordable price.
Currently, cetirizine preparations, in addition to the original (Zyrtec), are registered with 13 generic drugs from different manufacturers [18]. The relevant issue is the interchangeability of generic cetirizine, their therapeutic equivalence to the original drug and the choice of the optimal drug for the treatment of allergic diseases. The stability of the therapeutic effect and the therapeutic activity of the reproduced drug are determined by the features of the technology, the quality of the active substances and the range of excipients. The quality of drug substances from different manufacturers may vary significantly. Any change in the composition of excipients may be accompanied by pharmacokinetic deviations (decreased bioavailability and the occurrence of side effects) [18]. The generic must be safe to use and equivalent to the original drug. Two drugs are considered bioequivalent (pharmacokinetically equivalent) if, after administration by the same route (for example, orally) in the same dose and schedule, they have the same bioavailability (the proportion of the drug that enters the bloodstream), the time to reach the maximum concentration and the level of this concentration in the blood, half-life and area under the time-concentration curve. The listed properties are necessary for the proper effectiveness and safety of the drug. According to the recommendations of the World Health Organization, the bioequivalence of a generic drug should be determined in relation to the officially registered original drug. Bioequivalence studies have become mandatory for drug registration since 2010. The FDA (Food and Drug Administration, USA) annually issues and publishes the “Orange Book” with a list of drugs (and their manufacturers) that are considered therapeutic. equivalent to the original ones. In addition, it is important to pay attention to compliance with international manufacturing standards (GMP) when manufacturing drugs. Unfortunately, not all manufacturers (especially domestic ones) have production facilities that meet GMP requirements, and this may affect the quality of drugs, and therefore the effectiveness and safety of generics. Thus, when choosing generics, there are a number of reliable guidelines: the authority of the manufacturer, compliance with GMP, inclusion in the FDA Orange Book [19]. All of the above criteria are fully met by the drug Cetrin from Dr. Reddy's Laboratories Ltd. Cetrin is produced by an international pharmaceutical company whose production sites are GMP certified. It is bioequivalent to the original drug [20] and is included in the FDA Orange Book as a drug with proven therapeutic equivalence. In addition, Cetrin has a long-term successful experience of use in Russia and a large own evidence base. A comparative study of the therapeutic efficacy and pharmacoeconomics of cetirizine preparations from different manufacturers in the treatment of chronic urticaria showed that the largest number of patients who achieved remission were in the groups receiving Zyrtec and Cetrin, while the best results in terms of cost-effectiveness were demonstrated by therapy with Cetrin [21, 22 ]. The long history of use of Cetrin in domestic clinical practice has proven its high therapeutic effectiveness and safety. Cetrin is a drug that meets the practical need of clinical medicine for an effective and safe antihistamine drug available to a wide range of patients.
Loratadine: how much to drink
To prevent overdose and side effects, it is worth knowing for how long you are allowed to take the medicine.
Adults and children over 12 years of age take 1 tablet once a day. If taken in syrup form, the daily dose is 10 mg.
Children from 3 to 12 years old take ½ tablet per day. The daily dose in syrup form is 5 mg.
The average duration of the treatment course is 1-2 weeks, in some cases the treatment can be extended to 30 days. A more precise duration of the treatment course can be determined by your doctor.
When are allergy pills Loratadine used?
The drug is used in the treatment and prevention of allergic diseases:
- rhinitis, which causes seasonal climate changes and plant flowering,
- itchy dermatoses, conjunctivitis and hay fever,
- with angioedema and urticaria.
Loratadine tablets are used for emergency treatment after human insect bites and pseudo-allergic reactions.
The drug Loratadine is prescribed orally for adults and adolescents from the age of twelve - one tablet once a day, regardless of meals.
The medication is swallowed and washed down with water. Relief of the patient's condition occurs in the first three hours after admission to the body. The course of treatment is agreed with the doctor and depends on the severity of the patient’s condition.
Loratadine is prescribed to children from the age of two. When calculating the dose, pediatricians use the weight of the small patient.
A child whose weight is more than 30 kg takes one tablet once a day.
A child with a lower weight drinks the medicine in syrup - one teaspoon (5 ml) once a day.
Children under 12 years of age whose weight exceeds 30 kg and adults are prescribed a dessert spoon (10 ml) once a day.
The medication is not used in the treatment of pregnant and breastfeeding women, since the instructions for the drug do not contain information about conducting research.
Is Loratadine safe for pregnant women?
The instructions for use in the “Contraindications” section do not say anything about taking Loratadine during pregnancy. The drug should not be given only during breastfeeding.
Taking medication during pregnancy is acceptable provided that the possible benefits outweigh the possible side effects and consequences. If possible, you should stop taking any medications in the 1st trimester of pregnancy, when the fetus is not yet strong enough.
During pregnancy, the following adverse reactions may occur: lack of appetite, nausea, dizziness, changes in heartbeat.
Note!
The description of the drug Loratadine on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use.
Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug). Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.
Contraindications and side effects
You should avoid taking Loratadine in the following cases:
- individual intolerance to the constituent components;
- breastfeeding period;
- 1st trimester of pregnancy;
- age up to 2 years.
If the child weighs less than 30 kg, then it is best to give him the drug in syrup form.
People with serious liver diseases and patients with diabetes mellitus should take it with caution.
If you do not follow the instructions, neglect contraindications and permissible doses, the following adverse reactions may occur:
- headache;
- weakness, lethargy, drowsiness;
- dizziness;
- tachycardia;
- feeling of dry mouth;
- alopecia;
- increased appetite;
- changes in kidney function.
Children from 2 to 12 years old may experience adverse reactions in the form of irritability, drowsiness and headache.
There may be cases of overdose, which is manifested by the side effects described above. In this case, you need to rinse the stomach, drink enterosorbent and take care of symptomatic treatment.
Hydroxychloroquine and mefloquine
Doctors have been using drugs based on chloroquine for more than 70 years to treat malaria and autoimmune diseases (for example, systemic lupus erythematosus). Scientists have found that the active substance is also effective against the SARS-CoV-2 virus. In March, the Chinese holding Shanghai Pharmaceuticals provided Russia with the drug hydroxychloroquine (a derivative of chloroquine) for the treatment of COVID-19. The Ministry of Health did not identify any contraindications and allowed its use, donating more than 68 thousand packages to hospitals, despite the fact that hydroxychloroquine is not registered in Russia.
Scientists are still arguing about the validity of using hydroxychloroquine. Research by French infectious disease specialist Didier Raoult showed positive results. But the Associated Press published data from American studies. An analysis of medical records of patients treated with the drug showed that hydroxychloroquine was less effective than standard treatments.
In April, the Federal Medical and Biological Agency of the Russian Federation conducted clinical trials of mefloquine (an analogue of hydroxychloroquine approved in Russia). Scientists found out how effective and safe this antimalarial drug is. According to preliminary data from a study involving 347 patients, after using mefloquine, positive dynamics were noted in 78% of cases. The FMBA will provide its final conclusions at the end of May.

![Table 1. Dynamics of publications on clinical trials of piracetam and piracetam-like drugs over four time periods [5, with additions]](https://laram-halal.ru/wp-content/uploads/tablica-1-dinamika-publikacij-posvyashchennyh-klinicheskim-ispytaniyam-piracetama-i-piracetamopodobnyh-330x140.jpg)
![Table 1. Dynamics of publications on clinical trials of piracetam and piracetam-like drugs over four time periods [5, with additions]](https://laram-halal.ru/wp-content/uploads/tablica-1-dinamika-publikacij-posvyashchennyh-klinicheskim-ispytaniyam-piracetama-i-piracetamopodobnyh2-330x140.jpg)