At the present stage of development and improvement of methods for treating endogenous depression, increasing attention is paid to the participation of monoamine neurotransmitters in the pathogenesis of the disease and the peculiarities of the impact of newly created psychotropic antidepressant drugs on these links [1, 2]. The pharmacological effect of different classes of antidepressant drugs introduced into psychiatric practice is due to different mechanisms of their interaction with certain brain receptors and participation in various metabolic processes. The search for thymoanaleptics that interact with both serotonergic and noradrenergic receptors, i.e., with a dual mechanism of action, led to the creation of a new class of antidepressants - selective serotonin and norepinephrine reuptake inhibitors (SNRIs). The emergence of antidepressants with a dual mechanism of action was accompanied by an increase in the effectiveness of treatment of depressive conditions and made it possible to achieve remission in 45% of patients [2, 3].
One of the SNRIs is venlafaxine, the first third-generation thymoanaleptic. In many studies [4–6], it is rated as a “reference” in the group of these compounds.
Venlafaxine and its main metabolite, O-desmethylvenlafaxine, are potent serotonin and norepinephrine reuptake inhibitors and weak dopamine reuptake inhibitors. Both the main drug and its indicated metabolite reduce β-adrenergic reactivity. Venlafaxine has no affinity for muscarinic, cholinergic, histamine, and α1-adrenergic, opioid, benzodiazepine, orencyclidine and N-methyl-α-aspartate receptors in the brain; while the ratio of monoamine transfer (serotonin/norepinephrine) with venlafaxine is 30 (compared to 9.4 for another SNRI - duloxetine). This indicates a significant predominance of the serotonergic effect in the action of venlafaxine, similar in strength to selective serotonin reuptake inhibitors (SSRIs). A group of authoritative experts in the field of psychopharmacotherapy showed [7] that venlafaxine, along with escitalopram and clomipramine, can be considered one of the most effective antidepressants.
Venlafaxine is a racemic mixture of two enantiomers: the S-enantiomer, which is a more potent serotonin reuptake inhibitor, and the R-enantiomer, a potent norepinephrine reuptake inhibitor. Thanks to this structure, the drug eliminates the deficiency of both serotonin and norepinephrine in neuronal synapses, which provides a more balanced effect on neurotransmission and synergism of psychopharmacological effects. The features of venlafaxine should also include the high selectivity of its pharmacological action, which determines its favorable tolerability and safety profile [8-10].
To date, data have been accumulated on the dose dependence of the therapeutic effect of venlafaxine. Possessing a wide range of therapeutic action, venlafaxine consistently includes serotonergic, noradrenergic and dopaminergic receptors in the spectrum of its neurochemical activity [11]. When comparing the effectiveness of venlafaxine with antidepressants from the SSRI group in a meta-analysis of 34 randomized, double-blind studies [12], which included 8,000 patients with depressive disorders of varying severity, statistically significant advantages of venlafaxine as a means of achieving remission were established.
The relatively short half-life necessitates strict adherence to the daily dosage regimen [13, 14]. Many years of successful global experience in the use of venlafaxine indicate a dose-dependent mechanism of its action, which makes it possible to use the drug as an alternative to SSRIs and tricyclic antidepressants in the treatment of both treatment-resistant depression and acutely developed primary depression both in inpatient and outpatient practice [7, 14— 19]. The favorable tolerability profile and low incidence of side effects during venlafaxine therapy are emphasized [14].
Venlafaxine has been noted to be highly effective in treating a wide range of depressive conditions within the framework of recurrent and bipolar affective disorders [14], as well as in generalized anxiety, somatogenic and post-stroke depression [4, 20].
A number of authors [5, 21, 22] note the early onset of the antidepressant effect of venlafaxine and its positive effect on the manifestations of the actual thymic component of depression, anxiety, agitation, motor retardation, and cognitive functions. However, the questions of the effect of venlafaxine on depressive states of various structures remain insufficiently developed [23].
The purpose of the study was to evaluate the clinical effect of venlafaxine during a course of treatment of patients with various depressive states of endogenous nature.
Material and methods
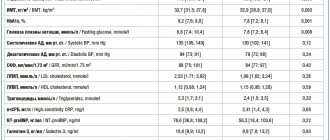
We examined 32 patients, 15 women and 17 men, aged from 18 to 57 years (average age 31.75 years) with endogenous depression, who were undergoing inpatient treatment in the clinical departments of the department for the study of endogenous mental disorders and affective states of the Federal State Budgetary Institution "Research Center for Mental Health" » RAS.
The design of the study was open naturalistic. The average duration of the disease from its first manifestation was 7.9 years, the average number of depressive episodes suffered before inclusion in the study was 3.3. The duration of the current depressive episode before starting Velaxin was on average 4.5 months.
According to nosological affiliation, the patients were distributed as follows: 22 (68.6%) patients were diagnosed with endogenous affective diseases - manic-depressive psychosis (MDP), cyclothymia; in 5 (15.6%) depression developed in the dynamics of low-progressive schizophrenia, and in 5 (15.6%) postpsychotic depression was noted in the context of paroxysmal schizophrenia. According to ICD-10, the depressive state of patients was diagnosed according to the following categories: F31.3—F31.4; F32.0—F32.2; F33.0—F33.2; F21; F20.4. Typologically, depressive states were defined as melancholy (3 patients, 9.4%), anxious (11 cases; 34.4%) and apatho-adynamic (18 patients; 56.2%). Thus, in accordance with the two-level psychopathological model of depression [24], its first 2 types were defined as typical, representing positive affectivity (sad and anxious depression), apatho-adynamic depression as atypical and related to negative affectivity.
According to the total scores on the Hamilton Depression Scale (HAM-D) before treatment: mild depressive disorders were registered in only 2 (6.25%) people, moderate in 13 (40.6%), severe depression in 17 (53.15%), i.e., the vast majority of patients had moderate to severe depression.
The study used venlafaxine, marketed as Velaxin 75 mg tablets (Hungary). The drug was prescribed orally, starting from 37.5-75 mg per day. Subsequently, based on the condition of the patients, over the next few days the daily dose was increased, reaching the maximum for a given patient, but not more than 300 mg. On average, the highest mean dose of Velaxin used was 182.1–198.2 mg per day. The drug was taken twice, morning and evening. According to the study protocol, the course of Velaxin therapy was 56 days (8 weeks).
To assess the severity of depressive symptoms and determine the therapeutic effect, in addition to the clinical observation method, the HAM-D-24 scale, containing 24 signs, was used. The severity of depressive symptoms was assessed before the start of the course of treatment (day 0), then on days 1, 3, 5 of therapy and then at the end of each of the 8 weeks of course treatment. The effectiveness of the antidepressant effect of velaxin was assessed by the degree of reduction in HAM-D scores in % relative to the score before treatment in the following gradations: reduction in scores up to 20% - as “insignificant”, by 21-50% - as “moderate”, by 51- 80% - as “good” and 81-100% - as a “significant” effect (including “practical recovery”). A decrease in the total HAM-D score to 6 or less meant complete “entry” into remission. Maintaining the HAM-D depression severity score at the same level or increasing the total score was regarded as no effect or “worsening” of the condition. To assess the spectrum of antidepressant action of Velaxin, the degree of reduction in the average total score of individual signs identified in the HAM-D was determined, conditionally characterizing melancholic or sad (items 1-3, 22-24), apatho-adynamic (items 7 and and anxious (items 9 and 10) manifestations in the structure of the depressive state.
The severity of depressive symptoms was assessed before the start of the course of treatment (day 0), then on days 1, 3, 5 of therapy and then at the end of each of the 8 weeks of course treatment. The effectiveness of the antidepressant effect of velaxin was assessed by the degree of reduction in HAM-D scores in % relative to the score before treatment in the following gradations: reduction in scores up to 20% - as “insignificant”, by 21-50% - as “moderate”, by 51- 80% - as “good” and 81-100% - as a “significant” effect (including “practical recovery”). A decrease in the total HAM-D score to 6 or less meant complete “entry” into remission. Maintaining the HAM-D depression severity score at the same level or increasing the total score was regarded as no effect or “worsening” of the condition. To assess the spectrum of antidepressant action of Velaxin, the degree of reduction in the average total score of individual signs identified in the HAM-D was determined, conditionally characterizing melancholic or sad (items 1-3, 22-24), apatho-adynamic (items 7 and and anxious (items 9 and 10) manifestations in the structure of the depressive state.
In addition, at the above periods, the severity of the depressive state and the degree of its improvement over time were assessed using the CGI Clinical Global Impression scale and its subscales CGI-S and CGI-I. To record side effects, the UKU interview scale was used, which consists of 4 subscales that allow us to distinguish mental, neurological, autonomic and so-called other side effects.
results
During the prescribed 56-day course of treatment with Velaxin, 31 (96.9%) people were recognized as responders, of which a “minor” effect of treatment was observed in 1 (3.1%) patient, a “moderate” effect in 3 (9.4 %), “good” - in 2 (6.25%), and 25 (78.1%) patients showed a “significant” therapeutic effect. Thus, a decrease in the intensity of depressive disorders by 50% or more during treatment with Velaxin was found in the vast majority of cases - in 27 (84.4%) patients, as shown in Fig. 1.
Rice. 1. The degree of severity of the therapeutic effect of Velaxin for endogenous depression. The x-axis is the degree of reduction according to HAM-D,%; The y-axis is % of patients.
In general, the effectiveness of Velaxin, assessed on the 56th day of therapy, was quite high: the average total score of depression severity according to HAM-D was reduced by 85.9%. By the end of the 1st week of treatment with Velaxin, a positive therapeutic response to the drug was observed: the reduction in depression was at the level of a “minor” effect, but was approaching a 20% reduction in disorders, bordering on a “moderate” improvement. A clear “moderate” improvement (reduction in HAM-D score by 33.2%) was observed by the 14th day of treatment; between the 21st and 28th days of treatment, the therapeutic effect reached the “good” range with a decrease in HAM-D scores by 50% or more, and by the 6th week the effect of Velaxin treatment was already approaching the “significant” border (up to 76.7% reduction in the severity of depressive symptoms). In the subsequent 7-8 weeks of therapy, an undeniable “significant” improvement in the patients’ condition was detected (reduction of disorders by more than 80%), up to “recovery” (Fig. 2). In 20 out of 31 patients (64.5% of cases) who completed the course of treatment with Velaxin, depression was completely reduced and “entry” into remission was observed (their total HAM-D score became 6 or lower).
Rice. 2. The spectrum of therapeutic action of velaxin for endogenous depression (HAM-D score). Here and in Figs 3, 4 and 5 (in the last one - the right axis): on the ordinate - the average score as a percentage of the score before the start of therapy, on the x-axis - the day of therapy.
The severity of the condition, assessed by the CGI-S subscale, on average decreased during treatment with Velaxin from 4.7 to 1.6 points at the end of the study (from “significantly expressed” to less than “mildly expressed”, i.e., to the virtual absence of distress ). Moreover, a noticeable decrease in the severity of symptoms was noted in the period between the 7th and 21st days of treatment, when the intensity of the manifestations of depression consistently decreased on average to “moderately” and “weakly” expressed. From the 5th week of therapy, the severity of depressive disorders became “very weak”, and at the 7-8th week of course therapy there was a practical “exit” from depression with the “absence” of depressive symptoms (their average level of severity was 1.6 points). During the 56-day course of therapy, assessment of the degree of improvement in the depressive state on the CGI-I subscale showed a “deterioration” of the mental state (5th assessment level) in only 1 (3.1%) person, remained “unchanged” (4th assessment level) also in 1 (3.1%) patient, “minor improvement” (3rd level) - also in 1 (3.1%), “pronounced” improvement (2nd level) was observed in 4 (12 .6%), the remaining 25 (78.1%) patients showed a “significant” improvement (grade 1).
It was found that in the spectrum of antidepressant action of Velaxin, all 3 components of its psychotropic activity, in accordance with the final results of treatment, are presented to almost the same extent with a slight advantage in terms of anti-depressive action (see Fig. 2). Thus, the degree of reduction in the average total score of disorders on items 1-3 and 22-24 of HAM-D (reflecting the actual thymoleptic effect of the drug) was 88.2%, on items 7 and 8 (stimulating effect) - 83.7%, and on points 9 and 10 (anti-anxiety effect) - 85.1%. However, the implementation of all 3 components of the action of Velaxin over time was different and had its own characteristics. Thus, thymoleptic and especially anxiolytic effects were detected most quickly during treatment. They developed almost in parallel, reaching a level of reduction in the severity of disorders according to HAM-D by 32.8 and 37.1%, respectively, by the 14th day of therapy (“moderate” effect). At the same time, the stimulating effect of Velaxin was somewhat “lagged” compared to the anti-anxiety and anti-sadness effects, reaching similar values (“moderate” effect - reduction of disorders by 36.9%) only by the 21st day of the study.
Subsequently, in the period from the 21st to the 28th days of treatment, the thymoleptic and anti-anxiety components of the action in the spectrum of antidepressant activity of Velaxin leveled off and increased in rate of development to the range of a clear “good” effect (score reduction by 60.2 and 59. 2%). But already from the 5th week of treatment, the thymoleptic effect itself began to surpass the anxiolytic one in terms of the depth of reduction of disorders according to the corresponding HAM-D items: the thymoleptic effect appeared at the “significant” level already at the 6th week, and the anti-anxiety effect only after the 7th week course therapy. The formation of the stimulating effect was “lagged” in the degree of manifestation compared to the other two components of the action of Velaxin at 1 week, and its “significant” severity was determined only at the 8th week of treatment. And only at this stage of treatment, as already mentioned, the depth of the stimulating effect of Velaxin approximately coincided with the severity of the thymoleptic and anxiolytic effects.
In accordance with established data on the peculiarities of the implementation of individual components of antidepressant action in the spectrum of psychotropic activity of velaxin, its therapeutic effectiveness was analyzed depending on the syndromic type of depression, i.e., on the dominant affect that determines the picture of the depressive state (Fig. 3). It was found that with leading anxious affect, the reduction in the average total score on HAM-D was 85.5% by the 56th day of treatment; with a predominance of apatho-adynamic affect, the effectiveness of Velaxin was similar - the average total score on HAM-D decreased by 85.9%. The highest effectiveness of Velaxin was observed in the treatment of patients with a leading sad affect in the picture of depression - the reduction in the average total score on HAM-D was 91.1%. But with a relatively similar degree of reduction in depressive symptoms, differences were also noted in the dynamics of the implementation of the antidepressant effect of the drug. Thus, with leading anxious and melancholy affects, i.e. in patients with positive affectivity and the most typical manifestations of depression, the reduction of depressive symptoms proceeded at an equal pace, reaching 21.1% (with anxious depression) and 22.5% (with melancholy depression) already by the 7th day of therapy. Subsequently, the decrease in the average total score on HAM-D occurred more intensively and reached more than 50% reduction in depressive symptoms by the 28th day of treatment. When treating patients with negative affectivity (atypical apatho-adynamic depression) with Velaxin, improvement occurred more slowly. A reduction in the average total HAM-D score by 20% or more (“moderate” effect) occurred only in the 2-3rd week of therapy; and only by the 4th week a “good” effect of Velaxin was recorded (reduction of disorders by 61.3%). By the 7-8th week of treatment, the improvement in the condition was already “significant” (more than 80% reduction in disorders), it coincided in severity with the therapeutic effect of Velaxin for anxious depression and was somewhat “lag behind” the effect for melancholy depression.
Rice. 3. Dynamics of the effectiveness of Velaxin for different types of endogenous depression (HAM-D score).
Analysis of the effectiveness of Velaxin depending on the nosological affiliation of depression also revealed some features (Fig. 4): the lowest rate of decrease in the average total score on HAM-D by the end of the course of treatment was in patients with low-progressive schizophrenia, it was equal to 82.3%. These same patients also had the slowest rate of reduction in depressive disorders - by the 7th day it was only 15.2%, and a reduction of 50% or more (the limit of a “good” effect) was achieved only by the 28th day; A “significant” effect was detected in patients with low-progressive schizophrenia only after the 7th week of treatment with Velaxin. In patients with affective illness (MDP, cyclothymia), the reduction in the average total score on HAM-D at the end of course therapy was close in value (86.6%), and the rate of reduction in depressive symptoms was similar: by the 7th day this figure reached 18 .2%, and by the 4th week of therapy it was already 59.4% (“good” effect). The best treatment result was achieved in patients with postpsychotic depression and paroxysmal schizophrenia - 90.4% reduction in disorders on the 56th day of treatment. Despite the fact that by the end of the 1st week of the study, the rate of reduction in depressive symptoms reached gradations of “insignificant” improvement (19.2%), subsequently the reduction in depressive symptoms occurred more intensively than with MDP, demonstrating a “good” effect already at 14 days. 1st day of treatment (symptom reduction rate -53.9%), and by the 28th day it was already 76.5%, i.e. it was almost on the border of “significant”. However, it should be noted that in these patients the initial severity of depressive disorders was significantly lower, at the level of “moderate” severity, than in other, more “severe” depressions (23 points on HAM-D versus 31.3 points for affective illness and 31.6 for low-progressive schizophrenia).
Rice. 4. Antidepressant effect of Velaxin in different nosological groups of patients (HAM-D score).
All of the indicated patterns of development of the therapeutic effect of Velaxin indicate the absence of a direct dependence on the size of its daily dose. As can be seen from Fig. 5, the therapeutic effect began to appear and increase from the 3-4th week of treatment (reduction of depressive symptoms by 50% or more according to HAM-D), with an increase in the average daily dose to the maximum (182.1-198.2 mg per day) . But subsequently, despite stabilization and even a slight decrease in the achieved maximum average daily dose of Velaxin (up to 190.3 mg per day), the response to therapy continued to increase at a faster pace, to the level of “significant” improvement,
Rice. 5. The relationship between the therapeutic effect (HAM-D score) and the daily dose of Velaxin. On the left ordinate is the average daily dose of the drug (mg).
During the course of Velaxin therapy, 45 adverse events of various types were registered in 21 (65.6%) patients; in 5 they were single, and in 16 they were combined. The most common were mental and autonomic adverse events noted on the UKU scale; they occurred in 40% of patients. One patient withdrew from the study early (after 2 weeks of treatment) due to the development of acute affective-delusional psychosis, requiring a change in therapy. Neurological and other side effects occurred in only 8.9 and 11.1% of patients. The most common individual side effects observed were “excitement/anxiety” (in 15.5% of patients), decreased sleep duration and nausea (in 11.1%), tachycardia and hyperhidrosis (in 6.6%), sedation and constipation (in 4.4%). All other side effects occurred in isolated cases. The incidence of side effects during a course of treatment with Velaxin was highest in the 2nd week of treatment, when the average daily dose of the drug was insignificant (157.7 mg per day). The most common adverse events during this period were psychiatric and autonomic adverse events. But subsequently, despite increasing the average daily dose, the incidence of side effects gradually decreased. The exception was “other” side effects, the frequency of which practically remained at the same level until the end of treatment. These were mainly sexual dysfunctions, which developed according to an increase in the daily dose of Velaxin.
It should be noted that, in general, all adverse events were mild or approaching moderate severity in the first 2 weeks of treatment, and then their average severity as assessed by UKU decreased to a “mild” level, despite a gradual increase in the average daily doses of Velaxin. At the same time, mental side effects were initially the most severe: the average UKU severity score at 1–2 weeks of treatment was 1.9–2.0. However, during the further course of treatment, the severity of adverse mental symptoms decreased from the 3rd week. The severity of some other adverse events increased slightly compared to the initial one: if on the 2nd week of treatment their severity on average corresponded to the UKU “mild” degree (1 point), then later they reached 1.5 points, and at the same time their degree severity increased according to an increase in the average dose of Velaxin.
Venlafaxine
Use during pregnancy and breastfeeding
Venlafaxine should not be prescribed to pregnant and breastfeeding women, because
The safety of the drug during pregnancy and lactation in women has not been sufficiently established, due to the fact that there are no adequately controlled clinical studies on a sufficiently large sample of such patients. This concerns the health of both the mother and, to a greater extent, the fetus/child. Women of childbearing age should be warned about this before starting treatment and should immediately consult a doctor if they become pregnant or plan to become pregnant during treatment with the drug. Venlafaxine and its metabolite (EFV) are excreted into breast milk. If it is necessary to take the drug during lactation, breastfeeding must be stopped.
In practice, there are cases of prescribing venlafaxine to mothers during pregnancy and shortly before childbirth, when in a particular situation the expected benefit to the mother outweighs the potential risk to the fetus. In these cases, newborns often experienced complications that required: increased hospitalization, maintenance of breathing and tube feeding. These complications can develop immediately after childbirth and are also typical when taking other antidepressants from the SNRI group or SSRIs (not containing venlafaxine). In such cases, the following clinical symptoms in newborns have been reported: respiratory disorders, cyanosis, apnea, convulsions, temperature instability, feeding difficulties, vomiting, hypoglycemia, muscle hypertension or hypotonia, hyperreflexia, tremor, trembling, irritability, lethargy, constant crying, drowsiness or insomnia. Such disturbances may indicate the serotonergic effects of the drug Venlafaxine.
If venlafaxine was used during pregnancy and maternal treatment was completed shortly before delivery, the newborn may experience withdrawal symptoms. In such a newborn, the presence of serotonin syndrome or neuroleptic malignant syndrome should be excluded. Epidemiological evidence suggests that use of SSRIs during pregnancy, especially late in pregnancy, may increase the risk of persistent neonatal pulmonary hypertension.
special instructions
Suicide and suicidal behavior
Depression is associated with an increased risk of suicidal ideation, self-harm, and suicide (suicidal behavior). This risk persists until significant remission occurs. Since improvement may not be observed during the first few weeks of therapy or even longer, patients should be closely monitored until such improvement occurs. Based on accumulated clinical experience, the risk of suicide may increase in the early stages of recovery.
Patients with a history of suicide attempts or high levels of suicidal ideation prior to treatment are at greater risk for suicidal ideation or suicide attempts and should be closely monitored. A meta-analysis of placebo-controlled clinical trials of antidepressants in adult patients with mental disorders found that antidepressants were at increased risk of suicidal behavior compared with placebo in patients under 25 years of age. Drug treatment of these patients, and in particular those at high risk of suicide, should be accompanied by careful monitoring, especially early in therapy and during dose adjustment. Patients (and caregivers of such patients) should be warned to monitor for any signs of clinical worsening, suicidal behavior or ideation, or unusual changes in behavior, and to seek immediate medical attention if these symptoms occur.
In a small number of patients taking antidepressants, incl. venlafaxine, aggression may occur during initiation of treatment, dose changes, or discontinuation of treatment.
Clinical studies conducted to date have not revealed tolerance or dependence to venlafaxine. Despite this, as with other drugs that act on the central nervous system, the physician should closely monitor patients for signs of drug abuse, as well as patients with a history of such symptoms.
Special patient groups
Venlafaxine is not approved for use in children.
In patients with a history of aggression, venlafaxine should be used with caution.
In patients with affective disorders, bipolar disorder when treated with antidepressants, incl. venlafaxine, hypomanic and manic states may occur. Like other antidepressants, venlafaxine should be used with caution in patients with a history of mania. Such patients require medical supervision.
Convulsive disorders may occur during therapy with venlafaxine. As with all antidepressants, venlafaxine should be used with caution in patients with a history of seizure disorders and such patients should be closely monitored. Treatment should be discontinued if seizures develop.
Akathisia
The use of venlafaxine has been associated with the development of akathisia, which is characterized by an unpleasant feeling of internal motor restlessness for the patient and manifested in the patient’s inability to sit quietly in one position for a long time or remain motionless for a long time. This condition may occur at the beginning of treatment and during the first weeks of treatment. In patients who develop such symptoms, increasing the dose is not recommended.
Bipolar disorder
Before starting treatment, it is necessary to identify those patients who are at risk for bipolar disorder. Such a check should include a detailed examination of the medical history, incl. family, to identify cases of suicide, bipolar disorder. It should be noted that venlafaxine is not recommended for use in the treatment of bipolar depression.
Use in patients with concomitant diseases
Clinical experience with the use of venlafaxine in patients with concomitant diseases is limited.
It should be used with caution in patients with diseases in which the effect of venlafaxine on hemodynamic parameters and/or metabolism may be significant.
Patients should be warned to immediately consult a doctor if a rash, urticaria or other allergic reactions occur.
Some patients while taking venlafaxine experienced a dose-dependent increase in blood pressure and/or an increase in heart rate, so regular monitoring of blood pressure and ECG is recommended, especially during the period of adjusting or increasing the dosage of venlafaxine. In post-marketing experience with venlafaxine (overdose), fatal cardiac arrhythmias have been reported. Before prescribing venlafaxine to patients at high risk of developing serious cardiac arrhythmias, the ratio of the likely benefit to the possible risk of use should be assessed.
Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance in order to prevent injury.
While taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone may occur.
Venlafaxine has not been studied in patients with recent myocardial infarction and decompensated heart failure. The drug should be prescribed to such patients with caution.
Taking SSRIs or venlafaxine in patients with diabetes may cause changes in plasma glucose levels. Dosage adjustments of insulin and/or antidiabetic medications may be required.
During treatment, it is recommended to refrain from drinking any alcohol-containing drinks.
The safety and effectiveness of venlafaxine in combination with weight loss medications (including phentermine) have not been established. The simultaneous use of venlafaxine and drugs that reduce body weight is not recommended.
Women of childbearing potential should use appropriate contraception while taking venlafaxine.
Explanations of special symptoms and conditions that may occur during treatment with the drug
Dry mouth occurs in 10% of patients receiving venlafaxine. This may increase your risk of developing tooth decay. Patients should practice good oral hygiene.
The use of venlafaxine may cause the development of akathisia, characterized by subjective discomfort or restlessness and the need to move frequently, often accompanied by an inability to sit or stand still. This mostly occurs during the first few weeks of treatment. Increasing the dose in patients who develop these symptoms may cause undesirable effects.
In placebo-controlled clinical trials, a clinically significant increase in serum cholesterol was reported in 5.3% of patients. Cholesterol level control is necessary during long-term treatment.
Withdrawal syndrome
When stopping treatment, withdrawal symptoms are common, especially if it is stopped abruptly. The risk of withdrawal syndrome may depend on several factors, including the duration of treatment, the size of therapeutic doses and the rate of dose reduction. These symptoms are very rarely reported in patients who accidentally missed taking the drug.
Withdrawal symptoms usually occur within the first few days after stopping treatment. These symptoms usually go away within 2 weeks, although in some people they may last 2-3 months or more. It is recommended to gradually reduce the dose of venlafaxine when stopping the drug - over several weeks or months, depending on the severity of the clinical symptoms of the disease.
Serotonin syndrome
Taking venlafaxine, like other serotonergic drugs, can cause serotonin syndrome, a potentially life-threatening condition, especially when used concomitantly with other drugs that can affect the serotonergic neurotransmitter systems such as MAO inhibitors.
Symptoms of serotonin syndrome may include mental status changes (agitation, hallucinations, coma), autonomic instability (tachycardia, blood pressure lability, hyperthermia), neuromuscular disorders (hyperreflexia, incoordination), and/or gastrointestinal symptoms (nausea, vomiting). , diarrhea).
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care should be taken when performing potentially hazardous types of work that require increased concentration and speed of psychomotor reaction (including driving a car and operating machinery).