Use of teriflunomide in patients with multiple sclerosis
N.Yu. LASCH
, Ph.D.,
A.N.
BOIKO , Doctor of Medical Sciences, Professor,
Department of Neurology, Neurosurgery and Medical Genetics, Russian National Research Medical University.
N.I. Pirogova, Moscow The article discusses the prospects for the use of a new drug for the treatment of patients with relapsing-remitting form of multiple sclerosis, teriflunomide. To date, phase II and III clinical studies have been completed, which have shown good tolerability, efficacy and relative safety of teriflunomide. In the TEMSO and TOWER studies, there was a reduction in the rate of relapses leading to hospitalization (59% and 37%, respectively), as well as the rate of exacerbations requiring corticosteroid therapy (34% and 36%, respectively).
Multiple sclerosis (MS) remains one of the pressing problems of modern neurology. The disease is quite common and occurs in most populations. Against the backdrop of a persistent global trend towards an increase in the number of cases, mainly young people of working age, the problem of MS treatment is acute. Modern advances in the diagnosis and treatment of MS [1] have made it possible to significantly extend the life of patients with MS and maintain activity for many years. Despite significant progress in understanding the mechanisms of MS development and the introduction into clinical practice of immunomodulatory drugs that modify the course of MS (IMDS), the search for new drugs continues.
Currently, all drugs for the treatment of MS are divided into three groups [2]. The first line of therapy is β-interferon (β-INF) preparations, low-dose and high-dose, for subcutaneous and intramuscular administration, glatiramer acetate (GA) for subcutaneous use. The second line is intravenous mitoxantrone, oral fingolimod, intravenous natalizumab. These drugs are prescribed in cases of proven ineffectiveness or intolerance to first-line drugs or in particularly malignant cases of MS. The third line is intravenous immunoglobulins (IVIG), immunosuppressants - cyclosporine, cyclophosphamide, etc., experimental treatment methods that are prescribed when the use of drugs of the first and second groups is ineffective or impossible. The list of medicines is constantly expanding. In recent years, new tablets have been approved in the European Union, America, and Russia for use in patients with relapsing-remitting MS, laquinimod and teriflunomide, which could potentially be classified in the first group of DMTs. Clinical studies of new original drugs and biosimilars used long-term in the treatment of MS are ongoing.
The procedure for prescribing, discontinuing, monitoring the effectiveness and safety of first-line DMTs is contained in the recommendations of the All-Russian Society of Neurologists and the technology for treating MS using DMTs adopted by Roszdravnadzor [2, 3].
Currently, there is no doubt about the need for early initiation of immunopathogenetic therapy after a reliable diagnosis of MS has been established (according to the latest criteria of Mac Donald, 2010). In this case, two main principles of therapy are used: escalation (starting treatment with a known, safer and milder drug) and induction (at the beginning of the disease, using drugs with a strong effect, short courses with a possible further transition to a milder treatment) [4, 5].
An important issue in the use of DMTs is patient adherence to the course of treatment - duration of treatment, method of administration, effectiveness, etc. In this regard, it can be assumed that the use of tablet forms is preferable for the patient, although comparative studies of adherence to injectable and tablet drugs in MS have so far was not carried out.
A new drug, teriflunomide (trade name Abagio®), has now been approved for the treatment of patients with relapsing-remitting MS (RRMS). The drug has been registered since 2012 in the USA, since 2013 - in the countries of the European Union, Australia, Argentina, Chile, Canada, Mexico, South Korea and Israel, and since July 2014 [6] - in the Russian Federation. The drug is approved as monotherapy for MS and as a first-line drug.
Teriflunomide (C₁₂H₉F₃N₂O₂) is the active metabolite of leflunomide (registered as Arava), a drug that has been used in the treatment of rheumatoid arthritis since 1998. After oral administration, leflunomide is rapidly and almost completely metabolized to teriflunomide (TF), which may have played a role in the choice drug for research in MS [7]. TF inhibits the enzyme dihydroorotate dehydrogenase (DHODH) and blocks pyrimidine synthesis in activated cells, therefore it has a cytostatic and anti-inflammatory effect [2]. TF affects only activated, rapidly dividing cells and does not affect slowly dividing cells of the hematopoietic system, so protective immunity does not suffer [8]. TF also suppresses the production of NO synthetase, Th1 cytokines, and tyrosine kinase activity, but stimulates the activity of Th2 cytokines. The bioavailability of TF is almost 100%, with the maximum plasma concentration achieved 1–2 hours after oral administration. It is known that the pharmacokinetic properties of the drug do not depend either on food intake or on the patient’s demographic parameters (gender and age) [9].
TF, as a rule, is completely (>99%) bound to plasma proteins (most of it with albumin), excreted unchanged through the gastrointestinal tract (37.5%) and urine (22.6%), practically does not penetrate through the blood-brain barrier [8]. The half-life of the drug is 10-12 days, but its elimination can be accelerated if necessary (for example, in the case of an unplanned pregnancy), which is an undoubted advantage of TF. In this case, cholestyramine is used in a dosage of 8 g 3 times a day or activated carbon 50 g 2 times a day.
To date, phase II and III studies have been conducted, which have shown good tolerability, efficacy and relative safety of the drug Abagio®. Since 2003, clinical multicenter international studies of TF have included approximately 4,000 patients with MS worldwide. These are patients with RRMS and secondary progressive MS (SPMS), with clinically isolated syndrome (CIS) (since 2007, phase III). In addition, comparative trials were conducted with high-dose interferon beta-1a [10]. In the Russian Federation, clinical studies of TF started in 2004. 14 clinical centers in Moscow, St. Petersburg, Kazan, Nizhny Novgorod, Novosibirsk, Rostov-on-Don (projects TEMSO and TOPIC) took part in them. The study included 152 patients, and 62 participants continue to be followed up to date. The TERACLES clinical trial was initiated, but was terminated early worldwide due to flaws in the study design; Russian clinics did not participate in the TENERE trial.
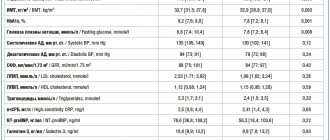
A total of 2,257 patients with RRMS and SPMS took part in international randomized placebo-controlled studies (TEMSO, TOWER), including Russian centers, as already noted, that took an active part in TEMSO. The use of TF in doses of 7 and 14 mg once led to a significant reduction in the frequency of exacerbations by more than 30% (p < 0.001), and a significant slowdown in progression was confirmed for a higher dose (14 mg, p = 0.03). The data are confirmed by clinical and MRI data.
Adverse events were assessed during Abagio® therapy. The most common disorders were the gastrointestinal tract (nausea, diarrhea, increased levels of liver enzymes). Elevations of alanine transferase (ALT) above the upper limit of normal were observed more often during treatment with TF (54% - 7 mg and 57.3% - 14 mg) compared with placebo (35.9%). However, the frequency of an increase in ALT three times the upper limit of normal did not differ significantly in the TF and placebo groups (6.3, 6.7 and 6.7%, respectively) [9]. In addition, the increase in ALT was not accompanied by a change in bilirubin levels above normal and often did not require additional therapy. Also, during TF therapy, nasopharyngitis, hair loss, arthralgia, and a slight increase in blood pressure (BP), on average systolic blood pressure by 2.8 mm Hg, were noted. Art. and diastolic blood pressure by 1.3 mm Hg. Art. and peripheral neuropathy. Complaints of thinning and hair loss were noted in clinical studies in the TF 7 mg group - 11.4%, in the TF 14 mg group - 15.2%, and to a lesser extent in the placebo group (4.3%). In patients who stopped therapy (less than 1%), hair growth was restored. The mechanism of hair loss is similar to that under stress, after childbirth and other transient conditions. At the same time, accelerated loss of mature hair in the resting phase (telogen effluvium), rather than young hair in the growth phase (anagen effluvium), as during chemotherapy, was noted [16]. In some patients who continued to participate in the projects, hair growth was restored independently after 3-6 months. [17].
There were no significantly significant differences between the placebo and TF-treated groups in the number of serious adverse events and the occurrence of malignant neoplasms.
Animal studies have shown a teratogenic and embryo-lethal effect, therefore, during the course of treatment with TF, pregnancy is prohibited and the mandatory use of a dual method of contraception is recommended. However, 70 cases of pregnancy were registered in those taking TF, 13 in patients who were prescribed placebo and interferon beta-1a. Twenty-six patients delivered healthy newborns without any structural or functional abnormalities; 29 and 13 patients had medical or spontaneous termination of pregnancy, respectively; one pregnancy is ongoing, the outcome of another is unknown [11, 13]. The percentage of patients who experienced spontaneous abortion (19%) does not exceed that in the general population of patients with MS [12]. In addition, 16 pregnancy outcomes are known in partners of patients receiving TF therapy: 12 healthy newborns, one case of spontaneous abortion and 2 pregnancies currently ongoing [11]. Animal models (in vitro and in vivo) have not provided data on the effect of TF on DNA in sperm [18]. In the event of pregnancy, active forced elimination of the drug using cholestyramine is recommended. It is not recommended to use TF by nursing women, since the penetration of TF into breast milk has been experimentally established. Monitoring of patients receiving TF continues to assess safety and refine the risk management plan; in total, clinical observations last more than 10 years.
The new oral drug Abagio® may increase adherence in some patients to long-term therapy due to the absence of injections, which quite often develop local adverse events (redness, swelling, itching, induration, atrophy of subcutaneous fat). Retaining chronic patients on long-term therapy is one of the most important factors in the effectiveness of therapy (reducing the number of exacerbations, reducing the severity of exacerbations, slowing the progression of neurological disease). Due to the fact that young, able-bodied people are most often affected, increasing adherence to treatment helps reduce the costs of outpatient and hospital care for patients with MS. In clinical trials of TF (TEMSO and TOWER), there was not only a reduction in the rate of relapses leading to hospitalization by 59 and 37%, respectively, but also a decrease in the rate of exacerbations requiring corticosteroid therapy by 34 and 36%, respectively [14, 15].
The introduction of new methods for treating chronic disabling neurological diseases makes it possible to improve the quality of life of patients and look into the future with optimism.
Literature
1. Multiple sclerosis. Clinical guidelines. Ed. E.I. Guseva, I.A. Zavalishina, A.N. Boyko. M.: Real Time, 2011. 2. Boyko A.N. Pathogenetic treatment of multiple sclerosis and other autoimmune diseases of the nervous system. In the book. "Autoimmune diseases in neurology." Clinical manual ed. I.A. Zavalishina, M.A. Piradova, A.N. Boyko, S.S. Nikitina, N.N. Spirin and A.V. Peresedova. ROOI "Human Health". M., 2014, 1: 285-344. 3. Recommendations of the All-Russian Society of Neurologists for conducting a course of treatment with drugs that change the course of multiple sclerosis. Journal neurol. and Psychiat., 2009, 109 (7), 2: 129-134. 4. Comi G. Induction vs. Escalating therapy in multiple sclerosis: practical implications. Neurol Sci, 2008, 29(2): 253-255. 5. Freedman MS. Induction vs. escalation of therapy for multiple sclerosis: evidence. Eurol Sci, 2008, 29(2): 250-252. 6. Instructions for medical use of the drug Abagio. 2014. 7. Osiri M, Shea B, Robinson V et al. Leflunomide for treating rheumatoid arthritis. Cochrane database of systematic reviews (Online) (1): CD002047. 8. Limsakin T, Menguy-Vacheron F. Pharmacokinetics of oral teriflunomide, a novel oral disease modifying agent under investigation for the treatment of MS. Presented at the Annual Meeting of the American Academy of Neurology (ANN) 2010. 9. O'Connor PW, Li D, Freedman MS et al. A Phase II study of the safety and efficacy of teriflunomide in multiple sclerosis with relapses. Neurology, 2006, 66(6): 894-900. 10. Boyko O.B., Stolyarov I.A., Petrov A.M., Boyko A.N. Teriflunomide is a new oral disease-modifying drug for multiple sclerosis (review). Journal neurol. and Psychiat., 2013, 10/2: 78-81. 11. Kieiseier B, Benamor M, Truffinet P. Pregnancy outcomes for female patients and partners of male patients in the teriflunomide clinical development program. 2014 Joint ACTRIMS - ECTRIMS Meeting, September 10–13, 2014, Boston, MA, USA. 12. Kieiseier B, Struve O, Benamor M et al. Upated pregnancy outcomes from teriflunomide clinical development program: retrospective analysis of the teriflunomide clinical trial database. Mult Scler, 2013, 19: 74. 13. Kieiseier B, Benamor M, Truffinet P. Pregnancy outcomes for female patients and partners of male patients in the teriflunomide clinical development program. 2014 Joint ACTRIMS - ECTRIMS Meeting, September 10–13, 2014, Boston, MA, USA. 14. O'Connor P, Wolinsky JS, Confavreux C et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N.Engl. J Med 2011, 365: 1293–303. 15. Confavreux C, O'Connor P, Comi G et al. Oral teriflunomide for patients with relapsing multiple sclerosis (TOWER): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. Mar 2014; 13(3): 247-56. 16. Harrison S, Bergfeld W. Diffuse hair loss: its triggers and management. Cleve Clin J Med. 2009, 76(6): 361-367. 17. Freedman M, Wolinsky J, Comi G et al. Safety and efficacy of teriflunomide in patients with relapsing multiple sclerosis treated with interferon beta. Presented at: 8th World Congress on Controversies in Neurology 2014. Berlin, Germany. 18. Davenport L, Czich A, Turpault S. Teriflunomide: no effects on sperm DNA. Mult Scler 2013, 19, 559: 1187.
Source:
Medical Council, No. 5, 2015
Teriflunomide
special instructions
Treatment should be carried out under the supervision of a physician experienced in treating patients with multiple sclerosis. Before starting treatment, the following studies should be carried out: measuring blood pressure, determining ALT activity, a complete blood count, including a leukocyte count and determining the number of platelets in the blood.
During treatment with teriflunomide, the following parameters should be regularly monitored: blood pressure, ALT activity.
If new symptoms and signs (for example, infection) appear during treatment, a complete blood count, including a leukocyte count, and a determination of the platelet count in the blood should be performed
Teriflunomide is slowly cleared from plasma: plasma concentrations reach values below 0.02 mg/l on average within 8 months, although due to individual deviations in the process of drug elimination it can last up to 2 years. The elimination of the drug can be accelerated through an accelerated elimination procedure. The accelerated elimination procedure may be used at any time after stopping teriflunomide.
An increase in liver enzyme activity was observed in patients taking teriflunomide. These adverse reactions occurred mainly in the first 6 months of treatment.
Patients with a history of liver disease are at risk of worsening liver function while taking teriflunomide. In this group of patients, symptoms of liver damage should be carefully monitored.
Teriflunomide should be prescribed with caution to patients who abuse alcohol.
Because teriflunomide is highly bound to plasma proteins, mainly albumin, plasma concentrations of unbound teriflunomide may be increased in patients with hypoproteinemia, such as those with nephrotic syndrome. Teriflunomide should not be prescribed to patients with severe hypoproteinemia.
If blood pressure increases, appropriate antihypertensive therapy should be administered before and during treatment with teriflunomide.
Initiation of treatment with teriflunomide should be delayed in patients with serious active infections until complete recovery.
Given the immunomodulatory effect of teriflunomide, if a patient develops a serious infection, the need to pause treatment with the drug should be considered and the possible benefits and risks assessed before restarting detoxification therapy. Due to the long T1/2, it is necessary to consider the need for accelerated elimination using cholestyramine or activated carbon.
Patients who test positive for tuberculosis at screening should receive appropriate treatment before starting teriflunomide.
During therapy, interstitial lung diseases can develop acutely.
Pulmonary symptoms, such as persistent cough and shortness of breath, may prompt discontinuation of therapy and further evaluation. In patients with existing anemia, leukopenia and/or thrombocytopenia, as well as in patients with impaired bone marrow function or at risk of suppression of bone marrow hematopoiesis, the risk of hematological diseases during teriflunomide therapy is increased. In the event of the development of these adverse reactions, it is necessary to consider the possibility of using an accelerated elimination procedure to reduce the concentration of teriflunomide in plasma. In cases of severe hematological reactions, including pancytopenia, teriflunomide and any other myelosuppressive drug should be discontinued. The feasibility of an accelerated elimination procedure should be considered.
If ulcerative stomatitis occurs, teriflunomide should be discontinued. If severe generalized skin reactions (Steven-Johnson syndrome or toxic epidermal necrolysis - Lyell's syndrome) are suspected when skin and/or mucocutaneous reactions occur, teriflunomide and any other drugs potentially causing such reactions should be stopped and should be started immediately. accelerated elimination procedure. In such cases, patients should not be reintroduced to teriflunomide. If peripheral neuropathy is diagnosed in a patient taking teriflunomide, discontinuation of teriflunomide and an accelerated elimination procedure should be considered. The use of live attenuated vaccines may pose a risk of infection and should therefore be avoided. Because leflunomide is the parent compound of teriflunomide, coadministration of teriflunomide with leflunomide is not recommended.
Switching to or from teriflunomide Based on clinical data relating to concomitant use of teriflunomide with interferon beta or glatiramer acetate, there is no need for a waiting period when initiating teriflunomide therapy after interferon beta or glatiramer acetate, or when initiating interferon beta therapy. or glatiramer acetate after teriflunomide.
Due to the long T1/2 of natalizumab, concurrent exposure and, therefore, concomitant effects on the immune system may occur if teriflunomide therapy is initiated within 2-3 months after discontinuation of natalizumab. Therefore, precautions should be taken when switching from natalizumab therapy to teriflunomide.
Taking into account the T1/2 of fingolimod, a 6-week interval without therapy is required to eliminate circulating substances from the body. It takes 1 to 2 months for the lymphocyte count to return to normal after stopping fingolimod. This may result in additive effects on the immune system. Therefore, precautions should be taken when switching from fingolimod therapy to teriflunomide.
In multiple sclerosis, the median T1/2 was approximately 19 days after repeated doses of 14 mg. If the decision is made to stop treatment with teriflunomide within 5 T1/2 (approximately 3.5 months, although may be longer in some patients), starting other therapy will result in concurrent exposure to teriflunomide. This may lead to additive effects on the immune system, which requires careful precautions.
Impact on the ability to drive vehicles and machinery
If undesirable effects from the nervous system occur, for example, dizziness, you should refrain from driving vehicles and engaging in other potentially hazardous activities.