Quetiapine
Children and adolescents (ages 10 to 17 years)
Quetiapine is not indicated for use in children and adolescents under 18 years of age due to insufficient data on use in this age group. According to the results of clinical studies of quetiapine, some side effects (increased appetite, increased serum prolactin concentrations, vomiting, runny nose and fainting) were observed with a higher frequency in children and adolescents than in adult patients. Some adverse events (AEs) may have different consequences in children and adolescents compared to adult patients. An increase in blood pressure was also noted, which was not observed in adult patients. Changes in thyroid function have also been observed in children and adolescents. The effects on growth, puberty, mental development and behavioral reactions with long-term use (more than 26 weeks) of quetiapine have not been studied.
In placebo-controlled studies in children and adolescents with schizophrenia and mania in bipolar disorder, the incidence of advanced EPS was higher with quetiapine compared with placebo.
Suicide/suicidal ideation or clinical worsening
Depression in bipolar disorder is associated with an increased risk of suicidal ideation, self-harm, and suicide (suicide-related events). This risk persists until significant remission occurs. Because it may take several weeks or more for the patient's condition to improve from the start of treatment, patients should be under close medical supervision until improvement occurs.
According to generally accepted clinical experience, the risk of suicide may increase in the early stages of remission. Patients (especially those at increased risk for suicide) and their caregivers should be warned to monitor for clinical worsening, suicidal behavior or thoughts, unusual changes in behavior, and to seek immediate medical attention if these occur.
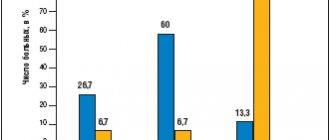
In clinical trials in depressed patients with bipolar disorder, the risk of suicide-related events was 3.0% (7/233) for quetiapine and 0% (0/120) for placebo in patients aged 18–24 years; 1.8% (19/1616) for quetiapine and 1.8% (11/622) for placebo in patients over 25 years of age.
Other mental disorders for which quetiapine is prescribed are also associated with an increased risk of suicide-related events. In addition, such conditions may be comorbid with a depressive episode. Thus, the precautions used when treating patients with a depressive episode should also be taken when treating patients with other mental disorders.
If quetiapine therapy is abruptly discontinued, the potential risk of suicide-related events should be taken into account.
Patients with a history of suicidal events, as well as patients who clearly express suicidal thoughts before starting therapy, are at increased risk of suicidal intent and suicide attempts and should be carefully monitored during treatment.
An FDA meta-analysis of placebo-controlled studies of antidepressants, summing up data from approximately 4,400 children and adolescents and 7,700 adult patients with mental disorders, found an increased risk of suicidal behavior with antidepressants compared with placebo in children. adolescents and adult patients under 25 years of age. This meta-analysis does not include studies that used quetiapine.
In short-term, placebo-controlled studies across all indications and all age groups, the incidence of suicide events was 0.8% for both quetiapine (76/9327) and placebo (37/4845).
In these studies in patients with schizophrenia, the risk of suicide-related events was 1.4% (3/212) for quetiapine and 1.6% (1/62) for placebo in patients aged 18–24 years; 0.8% (13/1663) for quetiapine and 1.1% (5/463) for placebo in patients over 25 years of age; 1.4% (2/147) for quetiapine and 1.3% (1/75) for placebo in patients under 18 years of age.
In patients with manic bipolar disorder, the risk of suicide-related events was 0% (0/60) for quetiapine and 0% (0/58) for placebo in patients aged 18–24 years; 1.2% (6/496) for quetiapine and 1.2% (6/503) for placebo in patients over 25 years of age; 1.0% (2/192) for quetiapine and 0% (0/90) for placebo in patients under 18 years of age.
Drowsiness
Drowsiness and associated symptoms such as sedation may occur during quetiapine therapy. In clinical studies involving patients with depression as part of bipolar disorder, somnolence usually developed during the first three days of therapy. The severity of this side effect was generally minor or moderate. If severe sleepiness develops, patients with depression as part of bipolar disorder may require more frequent visits to the doctor for 2 weeks after the onset of sleepiness or until symptoms improve. In some cases, discontinuation of quetiapine therapy may be necessary.
Patients with cardiovascular diseases
Caution should be exercised when prescribing quetiapine to patients with cardiovascular and cerebrovascular disease, and other conditions predisposing to hypotension.
Orthostatic hypotension may occur during quetiapine therapy, especially during dose titration at the beginning of therapy. Orthostatic hypotension and associated dizziness may increase the risk of accidental injury (fall), especially in older patients.
Patients should use caution until they adjust to these potential side effects. If orthostatic hypotension occurs, dose reduction or slower titration may be necessary.
Sleep apnea syndrome
Sleep apnea syndrome has been reported in patients taking quetiapine. Caution should be exercised when prescribing quetiapine to patients receiving drugs that have a depressant effect on the central nervous system, as well as patients with risk factors for sleep apnea (for example, overweight/obesity, male gender) or with a history of sleep apnea.
Seizures
There were no differences in the incidence of seizures in patients taking quetiapine or placebo. However, as with other antipsychotic drugs, caution is recommended when treating patients with a history of seizures with quetiapine.
Extrapyramidal symptoms
There was an increase in the incidence of EPS in adult patients with depression in the structure of bipolar disorder when taking quetiapine for depressive episodes compared to placebo.
While taking quetiapine, akathisia may occur, which is characterized by an unpleasant feeling of motor restlessness and the need to move, and is manifested by the patient's inability to sit or stand without moving. If such symptoms occur, the dose of quetiapine should not be increased.
Tardive dyskinesia
If symptoms of tardive dyskinesia develop, it is recommended to reduce the dose of the drug or gradually discontinue it. Symptoms of tardive dyskinesia may worsen or even occur after you stop taking the drug.
Neuroleptic malignant syndrome
While taking antipsychotic drugs, including quetiapine, neuroleptic malignant syndrome may develop. Clinical manifestations of the syndrome include hyperthermia, altered mental status, muscle rigidity, lability of the autonomic nervous system, and increased creatine phosphokinase activity. In such cases, it is necessary to discontinue quetiapine and carry out appropriate treatment.
Severe neutropenia and agranulocytosis
In short-term, placebo-controlled clinical trials of quetiapine monotherapy, cases of severe neutropenia (neutrophil count <0.5 x 109/L) without infection were reported infrequently. The development of agranulocytosis (severe neutropenia associated with infections) has been reported in patients receiving quetiapine in clinical trials (rare), as well as during post-marketing use (including death). Most of these cases of severe neutropenia occurred several months after initiation of quetiapine therapy. No dose-dependent effect was found.
Leukopenia and/or neutropenia resolved after discontinuation of quetiapine therapy.
A possible risk factor for the occurrence of neutropenia is a previous low white blood cell count and a history of drug-induced neutropenia. The development of agranulocytosis was also noted in patients without risk factors. The possibility of neutropenia should be considered in patients with infection, especially in the absence of obvious predisposing factors, or in patients with unexplained fever; these cases should be managed in accordance with clinical guidelines. In patients with a neutrophil count <1.0 x 109/L, quetiapine should be discontinued. The patient should be observed for possible symptoms of infection and the neutrophil level should be monitored (until the level exceeds 1.5 x 109/L).
Use of the drug Kvetiron
Adults take Kvetiron tablets orally 2 times a day during or between meals. The dose of the drug and the duration of treatment are determined by the doctor individually for each patient, depending on the indications and severity of the disease. Adults Course treatment of acute and chronic psychoses, including schizophrenic. In the first 4 days of therapy, the daily dose is: 1st day - 50 mg, 2nd - 100 mg, 3rd - 200 mg, 4th - 300 mg. Starting from the 4th day, the dose is increased until the required clinical effect is achieved (within 300–450 mg/day). Depending on the clinical effectiveness and tolerability of the drug, the daily dose of Kvetiron can be 150–750 mg. The maximum daily dose of Kvetiron for the treatment of schizophrenia is 750 mg. Course treatment of manic episodes associated with bipolar disorders. The daily dose in the first 4 days of treatment is: 1st day - 100 mg, 2nd - 200 mg, 3rd - 300 mg, 4th - 400 mg. Subsequently, the dose is increased (but not more than 200 mg daily) to 800 mg/day, starting from the 6th day of treatment. Depending on the clinical effectiveness and tolerability of the drug, the dose may be 200–800 mg/day. The maximum daily dose of Kvetiron for the treatment of manic episodes is 800 mg. Elderly people are prescribed Kvetiron with caution, especially at the beginning of the course of treatment. For patients in this age group, the initial dose should not exceed 25 mg/day. The dose should be increased by 25–50 mg daily until effective, which should not exceed the dose for young patients.
Interactions of the drug Kvetiron
Kvetiron should be used with caution in combination with drugs that act on the central nervous system. In this regard, alcohol consumption is strictly prohibited during treatment. The pharmacokinetics of lithium with simultaneous administration of quetiapine does not change. The pharmacokinetics of sodium valproate and quetiapine do not change when used simultaneously. The pharmacokinetics of quetiapine does not change significantly when administered concomitantly with risperidone or haloperidol. Concomitant use of quetiapine and thioridazine leads to increased clearance of quetiapine. The simultaneous administration of quetiapine and carbamazepine (an inducer of microsomal liver enzymes) leads to an increase in the clearance of quetiapine. When quetiapine is co-administered with phenytoin (or other hepatic enzyme inducers such as carbamazepine, barbiturates, rifampicin), the systemic effect of quetiapine may be significantly reduced, so it may be necessary to increase the dose of quetiapine to maintain control of psychotic symptoms. The dose of quetiapine may be reduced when phenytoin, carbamazepine or other liver enzyme inducers are discontinued or replaced with a drug that does not induce liver microsomal enzymes (for example, sodium valproate). CYP 3A4 is a key enzyme involved in the cytochrome P450-mediated metabolism of quetiapine. The pharmacokinetics of quetiapine does not change significantly when used simultaneously with cimetidine, which is a cytochrome P450 inhibitor. Co-administration of quetiapine and the antidepressant imipramine (CYP 2D6 inhibitor) or fluoxetine (CYP 3A4 and CYP 2D6 inhibitor) does not cause significant changes in pharmacokinetics. Co-administration of ketoconazole leads to an increase in the mean maximum concentration and AUC of quetiapine by 235 and 522%, respectively, and a decrease in clearance by 84%. The average half-life of quetiapine increases from 2.6 to 6.8 hours, but the average period to reach maximum concentration remains unchanged. Caution is recommended when using quetiapine concomitantly with potential CYP3A4 inhibitors (azole antifungals and macrolide antibiotics), and a dose reduction of quetiapine should be considered.
Overdose of the drug Kvetiron, symptoms and treatment
Cases of taking quetiapine at a dose of 20 g without fatal consequences and with complete clinical rehabilitation have been described. However, there are also reports of isolated cases of overdose that resulted in coma or death. Symptoms : drowsiness, sedation, tachycardia and hypotension as a consequence of enhancing the known pharmacological effects of the drug. Treatment : there is no specific antidote. In cases of severe intoxication, it is necessary to carry out intensive symptomatic drug therapy, as well as restore and control the patency of the airways, adequate ventilation and oxygenation, and the activity of the cardiovascular system. Careful medical monitoring of the patient's condition should continue until his complete recovery.