In the treatment of psychiatric diseases, it is often impossible to do without pharmacotherapy, and in some cases, drugs - antipsychotics - are the main way to cope with complications.
The line of such antipsychotics has recently been supplemented with a new generation of atypical antipsychotics. These drugs suppress the negative symptoms of mental disorders and show positive results on the patient. In addition, they do not cause at all or almost no extrapyramidal (motor function disorders), hyperprolactinemia (increased levels of the hormone prolactin in the blood), that is, unwanted side effects.
A prominent representative of modern atypical antipsychotics is a drug called Seroquel, which contains the active component quetiapine. The developers recommended this remedy for the treatment of schizophrenia. In the Russian Federation, its use has been approved for the treatment of psychosis and other mental disorders since 1999, and it is also widely used for the same purposes in another seventy countries around the world. The most detailed information about Seroquel and the experience of its use is discussed in the scientific work of psychiatrist (psychotherapist and child and adolescent psychiatrist) Victoria Valerievna Krasavina, on whose material we will rely in this article.
Compound
The chemical composition of the drug Seroquel or Seroquel Prolong depends primarily on the form of release of the drug. One tablet of the above-mentioned drugs may contain 25, 50, 100, 150, 200, 300 or 400 mg. quetiapine (active substance).
The drug Seroquel also contains such auxiliary compounds as: calcium hydrogen phosphate, povidone, carboxymethyl starch, microcrystalline cellulose, lactose monohydrate, sodium carboxymethyl starch and magnesium stearate .
The film coating of the tablets contains macrogol 400, titanium dioxide , as well as hypromellose , and some dosage forms of the drug contain dyes, for example, yellow or red iron oxide.
In addition to the active compound quetiapine, contains such auxiliary components as: lactose monohydrate, microcrystalline cellulose, sodium dihydrate, magnesium stearate , and hypromellose . The film coating of the tablets contains titanium dioxide, macrogol, yellow or red iron oxide and hypromellose.
Release form
Seroquel film-coated tablets differ not only in the amount of the drug compound they contain, but also in color. The manufacturer produces pink tablets - 25 mg each. quetiapine (10 pieces in a blister, 3 or 6 blisters in a package), yellow - 100 mg. quetiapine (10 pieces in a blister, 3,6 or 9 blisters in a package) and white - 200 mg each. quetiapine (10 pieces per blister, 3,6 or 9 blisters per package).
In addition, one package of a medicinal product may contain a combination of different forms of release of the drug, i.e. contains 6 tablets of 25 mg each, 3 tablets of 100 mg each. and 1 – 200 mg. One side of the tablets is engraved, which indicates the amount of the medicinal compound contained in one or another form of the drug - Seroquel 25, Seroquel WO and Seroquel 200.
The drug Seroquel Prolong is also available in tablet form. Depending on the dosage form, the special film-coated oblong and biconvex tablet of this medicine may be engraved, which corresponds to the amount of quetiapine , for example, XR50, XR150, XR200, XR300 and XR400. As a rule, one blister contains 10 tablets of the drug, and one cardboard package contains 6 blisters.
The nineties of the last century were marked by the emergence of a new group of antipsychotic drugs - atypical neuroleptics (ANL; Fig. 1). The introduction of these drugs, which lack most of the disadvantages of traditional antipsychotics, into clinical practice has become a big step in psychopharmacotherapy. Traditionally, ANL refers to drugs characterized by a low risk of developing extrapyramidal side effects. During the study of their action, other features of ANL were identified, allowing us to speak about the advantages of these drugs over typical antipsychotics: reduction of secondary and, to a lesser extent, primary negative symptoms, reduction in the severity of manifestations of cognitive deficits, impact on comorbid affective disorders, lack of influence or minimal effect on the level of prolactin in the blood. In addition, ANLs are often effective in cases of resistance to traditional antipsychotics [9].
Quetiapine fumarate is a compound from the dibenzothiazepine group and is structurally similar to the reference ANL clozapine, due to which it has a number of pharmacological properties similar to the latter (Fig. 2). Under the trade name Seroquel, the drug is produced by AstraZeneca in dosages of 25, 100 and 200 mg.
Quetiapine has affinity for D1, D2, 5-HT1A, 5-HT2A, alpha1 and alpha2 adrenergic receptors. The drug has pronounced antihistamine properties, somewhat less - the ability to block alpha1-adrenergic, 5-HT2A-serotonergic and alpha2-adrenergic receptors. With D2-dopaminergic,
Quetiapine interacts weakly with 5-HT1A-serotonergic and D1-dopaminergic receptors. It practically does not bind to cholinergic receptors of the M1 type [5, 11]. The receptor binding properties of quetiapine make it possible to prescribe it for a single dose per day, although most recommendations suggest twice a day [11, 17].
Clinical use of Seroquel
S. Stahl (1999) identifies the following features of Seroquel that are relevant for clinical use, distinguishing it from other ANLs [17]:
- Patients who have demonstrated resistance to previous courses of ANL therapy often experience improvement with Seroquel therapy;
- the drug is successfully used not only for chronic schizophrenia, but also for bipolar and schizoaffective disorders;
- Seroquel affects behavior disorders within psychodic conditions, such as aggression, cognitive impairment and mood symptoms;
- During therapy with Seroquel, disorders such as extrapyramidal disorders or hyperprolactinemia are practically not observed.
Data on the effectiveness of Seroquel are quite numerous, they allow us to conclude that the overall effectiveness of this drug in the treatment of various psychotic conditions is not inferior to that of standard antipsychotics and other representatives of the ANL class. These conditions include:
- schizophrenia (at the stage of active and maintenance therapy);
- schizoaffective psychoses [3, 4];
- manic and manic-delusional states in bipolar disorder [10, 13];
- psychotic disorders of late age [5].
It is also worth mentioning the positive results of studying the effectiveness of Seroquel for neurosis-like disorders in low-grade schizophrenia, including:
- somatization disorders (senestoipochondriacal states) [1];
- anxiety-phobic disorders and obsessive-compulsive (“schizo-obsessive”) states [4].
The action profile of quetiapine has now been determined through studies of its effectiveness in various disorders (Fig. 3).
The most characteristic of Seroquel is traditionally considered to be a pronounced sedative effect . Among other ANLs, it is second only to the effect of clozapine and is due to high tropism for alpha1 and alpha2 adrenergic receptors and blockade of H1 histamine receptors [5, 8], which makes it preferable for use in acute psychotic conditions that occur with agitation and anxiety.
No less important is the ability of the drug to have an anti-aggressive effect . This property allows a number of authors to recommend Seroquel for a wide range of conditions, including acute schizophrenic psychoses occurring with psychomotor agitation, hostility and aggression, psychoses of late age, psychopathic states with impulsive behavior [2, 5]. It is noted that in this capacity the drug has a pronounced “socializing effect” that regulates behavior: even with persistent hallucinatory-delusional symptoms, the effect of Seroquel on disorganized behavior quickly manifested itself.
The antimanic effect is currently being actively studied [3]. Its effectiveness in acute manic states has been established at a level not different from the level of the reference drug (haloperidol), with a virtual absence, unlike the latter, of adverse events, including extrapyramidal disorders, hyperprolactinemia, etc.
It is indicated that the choice of Seroquel in these cases often allows one to avoid the prescription of concomitant therapy with benzodiazepines to relieve psychomotor agitation. A comparison of the antimanic effect of Seroquel with that of other atypical antipsychotics is shown in Fig. 4.
Among the additional effects of Seroquel, first of all, attention should be paid to the antidepressant effect noted by many authors [4, 5, 7], which is manifested by a decrease not only in affective disorders themselves, but also in the level of anxiety, tension and a number of negative disorders.
Considering that up to 60% of patients suffering from schizophrenia experience depression during the course of the disease (including postpsychotic and so-called pharmacogenic depression), it is important to note that the use of Seroquel in this category of patients allows, in some cases, to avoid the prescription of concomitant antidepressant therapy.
G.E. Mazo (2003) believes that the antidepressant and anxiolytic effect of Seroquel is “fast and immediate,” which allows it to be recommended as the drug of choice in the treatment of patients with schizophrenia and depression [7].
The question of the possibility of using Seroquel for low-grade schizophrenia with obsessions is quite relevant, due to the well-known resistance of these conditions to pharmacotherapy. In contrast to the pronounced anxiolytic effect, the anti-obsessive effect of Seroquel is less pronounced (total improvement - 41.5%), and, according to the authors who studied its effectiveness, an increase in the daily dosage of the drug to 600–800 mg was often required [4].
According to the results of a comparative study of the effectiveness of ANL and haloperidol in 150 patients, S.N. the speed of onset as a distinctive characteristic of Seroquel [9]. After the first week of therapy with Seroquel at an average dosage of 410 mg, the reduction in the total PANSS score was 24.3 ± 2.4, which exceeded the effects of all other drugs used during the first four weeks of treatment (Fig. 5).
Therapeutic resistance in schizophrenia
RA Emsley et al. (2000) compared the effects of Seroquel (600 mg/day) and haloperidol (20 mg/day) in 288 patients with schizophrenia with signs of therapeutic resistance (no therapeutic response or partial response to fluphenazine therapy at a dose of 20 mg/day) [12]. The results of treatment during 8-week courses of therapy with these drugs are presented in Fig. 6.
Noteworthy is the pronounced overall therapeutic effect of Seroquel, superior to that of haloperidol (52.2 versus 38% of responders, respectively), and its effect on negative disorders. This allows us to conclude that in order to overcome therapeutic resistance that has formed after courses of therapy with typical antipsychotics, the appointment of Seroquel is more preferable than haloperidol.
Seroquel dosing
S. Stahl (1999) provides recommendations for dosing of Seroquel [17]:
- the effective dosage of the drug varies between 75–400 mg twice a day (in elderly patients 25–75 mg twice a day);
- in some clinical studies, a dosage regimen of Seroquel was used in 3 doses, but in clinical practice, 2 doses per day are more often used, which in cases of using small dosages for maintenance therapy (< 400 mg / day) can be replaced with a single dose;
- with increasing dosages, the drug can be effectively used for the treatment of acute psychotic conditions, including those occurring with agitation, including cases of drug resistance;
- Therapeutic dosages of 300–400 mg/day are recommended to be achieved around the fifth day of Seroquel therapy, starting with a dosage of 50 mg on the first day.
M. Smith et al. (2005) studied the possibility of rapid dose escalation during Seroquel therapy [16]. It was noted that increasing the therapeutic dosage to 400 mg/day on the third and even on the second day of therapy is not associated with a noticeable increase in the number of side effects and can be recommended for patients who need to quickly achieve a therapeutic effect.
Side effects of Seroquel
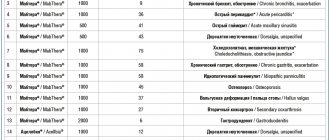
One of the most extensive materials available to judge the safety and tolerability of quetiapine is a premarketing study conducted on a large sample of patients (n = 1710). In this study, 5% of patients discontinued quetiapine therapy early due to the development of adverse events. The most common side effects are shown in the table.
Among the listed undesirable effects, the most common is drowsiness during the day, accompanied by a feeling of dizziness and orthostatic symptoms. The manifestation of these disorders occurs in the first few days of therapy with Seroquel and most often becomes the reason for patients’ refusal to continue therapy (1.4% of all patients).
Of interest are the data of PT Pollack and K. Zbuk (2000) on a case of quetiapine overdose (single dose of 30 tablets of 100 mg) [14]. The main observed disorders consistent with similar observations of overdose were hypotension, prolonged tachycardia (in the absence of other arrhythmias) and somnolence. These phenomena were reduced within 24 hours.
Pharmacoeconomic aspects of the use of Seroquel
It is known that the choice of an antipsychotic for long-term preventive therapy after psychosis is largely determined by its price.
S. Stahl (1999) notes that at dosages below 400 mg/day, quetiapine may be the most acceptable ANL in terms of the cost of the course of therapy.
E.B. Lyubov et al. (2005) present the results of a pharmacoeconomic study comparing the cost indicators of anti-relapse treatment for ANL in patients with schizophrenia [6]. According to these data, the cost of a daily dose of Seroquel (450 mg/day) is 197.5 rubles. and practically does not differ from the cost of a daily dose of risperidone (6 mg/day) – 176.33 rubles, but significantly lower than the cost of a daily dose of olanzapine (15 mg/day) – 286 rubles. However, this indicator is only part of the cost of treatment. It is known that the side effects of antipsychotics necessitate more frequent visits to the doctor, as well as appropriate therapy. Thus, calculating the full cost of treatment with a particular antipsychotic drug should take into account the overall level of costs for medical care, the cost of additional prescriptions, etc. The authors indicate that the share of the cost of the drug in the total cost of treatment when using Seroquel is 70% compared to 57% for risperidone and 77% for olanzapine. As a result, it turned out that the daily cost of treatment is 256.5 rubles. for Seroquel, 309.4 rubles. for risperidone and 371.4 rubles. for olanzapine. It was concluded that Seroquel, taking into account the total cost of treatment, dominates among the ANLs available in Russia.
The use of Seroquel at various stages of antipsychotic therapy
When conducting antipsychotic therapy, there are 3 stages [9]:
- Relieving or active therapy (acute treatment), aimed at quickly eliminating psychotic symptoms. Duration – 4–12 weeks.
- Aftercare, stabilizing or maintenance therapy (maintenance treatment), aimed at suppressing residual productive symptoms, correcting negative disorders, restoring social and labor adaptation and preventing or treating early relapses. At this stage, dosages are gradually reduced in order to reduce the sedative effect of the antipsychotic. Duration – 3–9 months.
- Anti-relapse or preventive therapy (prophylactic treatment) is carried out to prevent the development of new attacks and slow down the rate of progression of the disease. It lasts indefinitely, but not less than 1–2 years.
Each of these stages imposes its own requirements on the prescribed antipsychotic. If at the first stage of active therapy the severity of the antipsychotic effect and the speed of onset of the therapeutic effect are decisive, then at the second stage the ability of the drug to influence negative symptoms and the possibility of smoothly changing dosages come to the fore. Additional therapeutic effects of the drug also play a significant role, allowing one to avoid combinations with other drugs to combat comorbid disorders. For the third stage of antipsychotic therapy, the most important are the positive safety and tolerability profiles of the drug, as well as pharmacoeconomic factors. Taking into account the data presented above, we can conclude that the unique properties of Seroquel allow it to be successfully used at all stages of antipsychotic therapy, which is confirmed by the positive results of a number of studies.
Pharmacodynamics and pharmacokinetics
Since both drugs belong to the group of atypical antipsychotic drugs , they exhibit a high affinity for serotonin receptors of the 5HT2 class , in comparison with the brain dopamine receptors D1 and D2 . The drugs show similar properties in relation to adrenoreceptors and histamine receptors .
During scientific studies, the affinity of both drugs for benzodiazepine and cholinergic muscarinic receptors was not identified. When performing standard medical tests, the drugs show their antipsychotic properties. Seroquel Prolong, like Seroquel, causes mild catalepsy , which entails blocking dopamine D2 receptors.
Next, there is a selective decrease in the activity of dopaminergic mesolimbic neurons A10 in comparison with nigrostriatal neurons . When using both drugs, prolactin levels in the blood do not increase. As a result of research, experts discovered the ability of these medications to combat the symptoms and manifestations of schizophrenia .
When taking drugs orally, the medicinal compounds included in their composition are quickly absorbed into the stomach and then actively metabolized through the liver . It is worth noting that the bioavailability of quetiapine is not affected by food, so both drugs can be taken regardless of meals.
Both Seroquel Prolong and Seroquel are excreted from the human body in feces as well as urine .
Pharmacological properties of the drug Seroquel
An atypical antipsychotic drug that interacts with various types of neurotransmitter receptors. Quetiapine exhibits a higher affinity for serotonin receptors (5HT2) than for dopamine D1 and D2 receptors in the brain, as well as a high affinity for histamine and α1-adrenergic receptors and a lower affinity for α2-adrenergic receptors. It has no affinity for M-cholinergic receptors and benzodiazepine receptors, and exhibits antipsychotic activity. When studying extrapyramidal symptoms in an experiment, it was found that quetiapine causes only mild catalepsy when used in a dose that effectively blocks dopamine D2 receptors. Quetiapine causes a selective reduction in the activity of mesolimbic A10-dopaminergic neurons compared to A9-nigrostriatal motor neurons and has minimal effects on muscle tone in neuroleptic-sensitive monkeys. Quetiapine does not cause an increase in serum prolactin levels. The drug effectively eliminates both positive and negative symptoms of schizophrenia. When taken orally, it is well absorbed and actively metabolized. Food intake does not have a significant effect on the bioavailability of quetiapine. The main metabolites do not have pronounced pharmacological activity. The half-life is about 7 hours. Approximately 83% of quetiapine is bound to plasma proteins. Effective when taken 2 times a day. The effect of quetiapine on 5HT2 and D2 receptors lasts up to 12 hours, which is confirmed by positron emission tomography data. The pharmacokinetics of quetiapine is linear; there are no differences in the pharmacokinetics of the drug in men and women. The average clearance of quetiapine in elderly patients is 30–50% lower than in patients aged 18–65 years. Quetiapine clearance is reduced by 25% in patients with severe renal impairment (creatinine clearance less than 30 ml/min/1.73 m2) and in patients with liver damage (compensated alcoholic cirrhosis), but individual clearance levels are within the range corresponding to healthy people . Less than 5% of quetiapine is not metabolized and is excreted unchanged in urine or feces. Approximately 73% of quetiapine is excreted in urine and 21% in feces. The key enzyme in the metabolism of quetiapine is CYP 3A4, mediated by cytochrome P450. Quetiapine and some of its metabolites have a weak inhibitory effect on the enzymes cytochrome P450, 1A2, 2C9, 2C19, 2D6 and 3A4, but only at concentrations 10–50 times higher than the concentrations achieved when used at the usual dose (300–450 mg/day). In vitro , the ability of quetiapine to cause significant inhibition of the activity of cytochrome P450 and to influence the metabolism of other drugs mediated by it has not been established.
Indications for use
These drugs are indicated for:
- schizophrenia;
- chronic psychoses;
- manic states;
- depression;
- bipolar disorders.
Seroquel Prolong is also used for preventive purposes, for example, to prevent relapses of schizophrenic seizures in stable patients, as well as bipolar disorders
in patients who have previously successfully completed courses of treatment
with quetiapine . In addition, the drug is often included in the complex treatment of patients with a suboptimal response to monotherapy using antidepressants .
Child and adolescent therapy
At this time, few descriptions of the practical use of Seroquel in child and adolescent psychiatry can be found in the specialized literature. But they describe in sufficient detail the specifics of using the drug for this category of patients.
Due to good treatment results and mild side effects, experts suggest more active use of the drug in child and adolescent psychiatry. Already at 3-6 weeks, minor patients with schizophrenia taking Quetiapine in doses from 100 to 800 mg per day demonstrated a decrease in the symptoms of this disease, “extinguishing” hyperactivity and aggression.
Some patients experienced dry mouth, mild tremor, dizziness and hypotension as side effects. However, there were only a few such patients, and such manifestations were very weak. The usual strong increase in body weight after taking atypical antipsychotics was not observed, as well as disturbances in the endocrine system and problems with motor functions.
Also safe for children and adolescents is treatment with Quetiapine for bipolar and schizoactive disorders, antisocial behavior, psychopathy, Gilles de la Tourette syndrome and generalized tics, and other mental disorders. At the same time, experts warn about the danger of an overdose of the drug, which can cause tachycardia, hypotension, and agitation.
Contraindications
Both drugs are contraindicated if patients have an individual intolerance to certain components included in the chemical composition of the drugs, as well as lactase deficiency or galactose intolerance , or glucose-galactose malabsorption.
In addition, both medications are contraindicated in children under 18 years of age. Seroquel Prolong, like Seroquel, should be taken with extreme caution by elderly patients, people suffering from cerebrovascular and cardiovascular ailments or prone to hypotension , as well as those categories of patients whose history describes the risks of developing seizures, liver failure, aspiration pneumonia and stroke .
Structure and receptor activity of the drug
Chemically, Seroquel (quetiapine) is a derivative of dibenzothiazepine. This atypical antipsychotic interacts with many neuroreceptors, so its spectrum of therapeutic effects is very wide. The drug blocks H1 receptors according to the following scheme: H1 >α>α1>5-HT 2a>α2>D2>5-HT1a>D1>M1. Due to this binding of quetiapine and blockade of α1 and α2 receptors, a nonspecific sedative effect occurs, and anxious affect and arousal are eliminated.
The absence of side effects (hyperprolactinemia and minor extrapyramidal effects) is explained by the weak effect on 5-HT2a and D2 receptors.
Side effects of Seroquel
Among the most common side effects of Seroquel and Seroquel Prolong are the following:
- dizziness;
- drowsiness;
- dispersion;
- constipation;
- tachycardia;
- dry mouth;
- orthostatic hypotension;
- increased levels of triglycerides, liver enzymes, and insulin in the blood.
Patients often gain weight in the first weeks of using medications. Quite rarely, however, when taking these medications, side effects such as convulsions, priapism, neuroleptic syndrome, impaired consciousness, dystonia, vegetative-vascular disorders, neutropenia, akathisia, and leukopenia . , tardive dyskinesia may develop .
Side effects of the drug Seroquel
The most frequently reported side effects were drowsiness, dizziness, dry mouth, asthenia, constipation, tachycardia, orthostatic hypotension, and dyspepsia. As with treatment with other antipsychotic drugs, neuroleptic malignant syndrome, leukopenia, and peripheral edema were noted when using Seroquel. The incidence of side effects associated with the use of Seroquel is presented in the table.
Frequency | Organ and organ systems | Reaction |
| Very common (≥10%) | Nervous system | Dizziness 1, 5, drowsiness 2 |
| Common (≥1% but ≤10%) | Hematopoietic and lymphatic systems | Leukopenia |
| The cardiovascular system | Tachycardia 1.5, orthostatic hypotension 1.5 | |
| Digestive system | Dry mouth, constipation, dyspepsia | |
| General violations | Mild asthenia, neuroleptic malignant syndrome 1, peripheral edema, decreased neutrophil count 6, increased blood glucose to hyperglycemic levels 7, weight gain 3 | |
| Laboratory indicators | Increased activity of serum transaminases (ALAT, AST) 4 | |
| Nervous system | Loss of consciousness 1, 5 | |
| Respiratory system | Rhinitis | |
| Rare (≥0.1% but ≤1%) | Hematopoietic and lymphatic systems | Eosinophilia, neutropenia |
| The immune system | Hypersensitivity | |
| Laboratory indicators | Increased activity of γ-glutaryltransferase, TG and total cholesterol levels in blood plasma | |
| Nervous system | Cramps 1 | |
| General violations | Neuroleptic malignant syndrome 1 | |
| Reproductive system | Priapism |
1 See SPECIAL INSTRUCTIONS. 2 Drowsiness may develop in the first 2 weeks of treatment and, as a rule, disappears with prolonged use of the drug. 3 Occur, as a rule, at the beginning of treatment. 4 Asymptomatic increases in serum transaminase activity (ALT, AST, or gamma-glutaryltransferase) developed only in some patients taking Seroquel. These changes resolved with prolonged treatment. 5 Like other antipsychotic drugs with α-adrenergic blocking activity, Seroquel can cause the development of orthostatic hypotension, which is manifested by dizziness, tachycardia and, in some patients, loss of consciousness (especially at the beginning of treatment). 6 In placebo-controlled monotherapy studies in patients with baseline neutrophil counts ≥1.5 × 109/L, the incidence of at least one episode of neutrophil count ≤1.5 × 109/L was 1.72% in patients taking quetiapine. compared with 0.73% in patients taking placebo. In all clinical studies (placebo-controlled, open-label, active comparator; patients with baseline neutrophil count ≥1.5 x 109/L), the incidence of at least one episode of neutrophil count decline ≤1.5 x 109/L was 0.21% in patients treated with quetiapine and 0% in patients treated with placebo; incidence of ≥0.5–≤1×109/L was 0.75% in patients treated with quetiapine and 0.11% in patients treated with placebo. who used placebo. 7 At least 1 episode of glucose ≥126 mg/dL or fasting glucose ≥200 mg/dL.
Seroquel therapy was sometimes accompanied by a slight dose-dependent decrease in the level of thyroid hormones in the blood (total T4 and unbound T4). The maximum decrease in total and unbound T4 was observed during the first 2-4 weeks of quetiapine therapy, without further decrease in hormone levels with prolonged treatment. In almost all cases, cessation of treatment resulted in normalization of total T4 and free T4 levels, regardless of the duration of treatment. A slight decrease in the level of total T3 was noted only when using the drug in a high dose. The level of thyroxine-binding globulin did not change, and no increase in the level of thyroid-stimulating hormone was noted. No signs of hypothyroidism were noted while taking Seroquel. Very rarely, the development of hyperglycemia and decompensation of diabetes mellitus has been reported during treatment with quetiapine. As with other antipsychotic drugs, quetiapine therapy may be accompanied by weight gain, mainly in the first weeks of treatment. Like other antipsychotic drugs, quetiapine may cause an increase in the QTc on the ECG, but in clinical studies there was no relationship between the use of the drug and a persistent increase in QTc .
Instructions for use Seroquel Prolonga (Method and dosage)
Seroquel Prolong should be taken on an empty stomach; the tablets should not be chewed or broken. The dosage and duration of treatment with the drug depends on the type and severity of the disease, and, in addition, the health status of the patients should be taken into account. When treating schizophrenia , as well as bipolar disorders, this medicine should be taken according to the following plan:
- 300 mg each. on the first day;
- 600 mg each. over the next two days.
The optimal recommended daily dosage of the drug is 600 mg. may be increased to 800 mg. in case of urgent medical need.
During the treatment of depressive conditions, Seroquel Prolong is taken according to the following regimen:
- 50 mg each. on the first day;
- 100 mg each. on the second day;
- then 200 mg. during the third day;
- then 300 mg. throughout the fourth day.
The recommended daily dosage of the drug is 300 mg. may be increased to 600 mg. for medical reasons and in case of normal tolerability of the drug by patients. For preventive purposes, Seroquel Prolong is taken at night within a dose range of 300-800 mg.
As part of complex therapy, when have a suboptimal response to treatment with antidepressants, the drug is taken at a dose of 50 mg. the first two days, and then 150 mg. for another four days.
In accordance with the instructions for Seroquel, the drug is taken twice a day. The medication regimen, as well as the duration of the course of treatment, depends on the type of disease and the patient’s health condition.
When treating schizophrenia, as well as psychosis, the drug is taken:
- 50 mg each. first day;
- 100 mg each. on the second day;
- 200 mg each. on the third day;
- 300 mg each. on the fourth day.
The recommended daily dosage of the drug can vary from 150 to 750 mg.
When treating biopolar disorders , as well as manic-depressive states, Seroquel is taken according to the following regimen:
- 100 mg each. first day;
- 200 mg each. on the second day;
- 300 mg each. on the third day;
- 400 mg each. on the last fourth day.
Gradually, the therapeutic dose of the drug is increased and by the sixth day it can reach 800 mg.
Seroquel in general psychiatry
At the moment, there is a significant amount of data on the practical use of Quetiapine, accumulated by specialists over the past five years. As already mentioned, this atypical antipsychotic has been introduced as a treatment for schizophrenia. Its long-term use leads to an increase in the general activity of patients, a decrease in autistic manifestations, and an improvement in social adaptation. In this case, hyperprolactinemia and extrapyramidal disorders are not observed.
Seroquel has a positive effect on cognitive function in people with schizophrenia:
• after 3 months of use, attention improves significantly;
• after six months to a year, the quality of executive function and verbal productivity improves.
It should be clarified that this effect is achieved at an average dose of 517.9 mg/day of the drug per day. Long-term use of the drug is not dangerous, as it is well tolerated. Among other things, it reduces suicidal risks.
Experts who have used the atypical antipsychotic in practice indicate its positive results for depressive symptoms. It has a stronger antipsychotic effect than haloperidol, surpassing it and other drugs in antidepressant, anti-anxiety and anti-manic properties.
Such abilities of Quetiapine made it possible to use it and prove its effectiveness in the treatment of:
• anxiety states;
• affective disorders;
• behavioral disorders;
• bipolar disorders, etc.
The drug has also been successfully used to relieve hostility and aggression, in acute mania, and to reduce psychotic symptoms.
The following positive points can be mentioned:
1. Thanks to Seroquel, monotherapy has become possible, that is, treatment of mental disorders with excellent results without side effects is available using only one, maximum two drugs.
2. If we talk about obsessive-compulsive disorders, then Seroquel has also been tried to treat patients with strong resistance to antipsychotics such as selective serotonin reuptake inhibitors. However, a small dose of the drug in monotherapy was ineffective. But, in cases of combination of Quetiapine with SSRIs, patients experienced significant improvement in their condition.
3. They tried to use an atypical antipsychotic in the treatment of post-traumatic stress disorder. 18 war veterans with this problem took Seroquel for 6 weeks, 25-300 mg per day. By the end of therapy, the patients' condition improved significantly; no deterioration in neurological parameters or negative changes in internal organs were recorded. As a result, it was decided to expand research on the use of the drug in the treatment of this disorder.
4. There is evidence of success with this antipsychotic in elderly patients with psychotic symptoms, Parkinson's disease and Alzheimer's disease. Elderly patients had improved quality of life, motor functions, decreased behavioral disorders, and improved sleep. The attending physicians clarify that to achieve a positive effect, you should start with small doses of the drug and not increase them much.
5. There are isolated cases of effective use of Quetiapine for a patient with a mental illness aggravated by drug addiction and alcoholism.
Overdose
It is worth noting that if you follow the recommendations for taking both medications, cases of drug overdose are quite rare. However, in some cases, the consequences of an overdose were so incompatible with the lives of patients that they led to death or coma.
If daily doses of drugs are exceeded, symptoms such as drowsiness, decreased blood pressure, excessive sedation , and, in addition, tachycardia may be observed. In case of severe intoxication , symptomatic treatment is carried out, as well as measures aimed at maintaining the cardiovascular and respiratory systems of the human body.
Seroquel overdose, symptoms and treatment
Data on drug overdose are limited. Cases of taking the drug at a dose higher than 20 g have been described; no deaths have been recorded; symptomatic therapy is effective. After the widespread introduction of the drug into practice, there were isolated reports of cases of Seroquel overdose leading to coma or death. Symptoms of an overdose of quetiapine - sedation, tachycardia and hypotension were, as a rule, a consequence of increased pharmacological effects of the drug. There is no specific antidote. In cases of serious intoxication, multidirectional intensive care is recommended, including restoration and control of the upper airway, ensuring adequate oxygenation and ventilation, monitoring and support of the cardiovascular system. Careful medical supervision and monitoring should be carried out until the patient recovers completely.
Interaction
An increase in the concentration of quetiapine , and, consequently, an increase in the effectiveness of both drugs, can occur when Seroquel Prolong and Seroquel are taken simultaneously with antibiotics belonging to the macrolide , as well as with azole antifungals . Drug dosage adjustments may also be required when using drugs concomitantly with drugs that contain phenytoin or are designed to induce liver enzymes , such as carbamazepine.
Drug interactions Seroquel
Seroquel should be used with caution in combination with other drugs that act on the central nervous system. In this regard, during treatment it is necessary to avoid drinking alcohol. The pharmacokinetics of lithium with simultaneous administration of quetiapine does not change. The pharmacokinetics of sodium valproate and quetiapine do not change when used simultaneously. The pharmacokinetics of quetiapine did not change significantly when administered concomitantly with risperidone or haloperidol. Concomitant use of quetiapine and thioridazine resulted in increased clearance of quetiapine. The simultaneous administration of quetiapine and carbamazepine (an inducer of microsomal liver enzymes) led to an increase in the clearance of quetiapine. Co-administration of quetiapine and phenytoin (or other hepatic enzyme inducers such as barbiturates, rifampicin) may significantly reduce the systemic exposure of quetiapine; therefore, it may be necessary to increase the dose of quetiapine used concomitantly with hepatic enzyme inducers to maintain control of psychotic symptoms. The dose of quetiapine may be reduced when phenytoin, carbamazepine or other liver enzyme inducers are discontinued or replaced with a drug that does not have an inducing effect on liver microsomal enzymes (for example, sodium valproate). CYP 3A4 is a key enzyme involved in the cytochrome P450-mediated metabolism of quetiapine. The pharmacokinetics of quetiapine does not change significantly when used simultaneously with cimetidine, which is a cytochrome P450 inhibitor. Co-administration of quetiapine and the antidepressant imipramine (CYP 2D6 inhibitor) or fluoxetine (CYP 3A4 and CYP 2D6 inhibitor) does not cause significant changes in the pharmacokinetics of quetiapine. Co-administration of ketoconazole resulted in an increase in the mean maximum concentration and AUC of quetiapine by 235 and 522%, respectively, and a decrease in clearance by 84%. The mean half-life of quetiapine increased from 2.6 to 6.8 hours, but the mean time to reach maximum concentration remained unchanged. Caution is recommended during concomitant use of quetiapine and potential inhibitors of CYP 3A4 (azole antifungals and macrolide antibiotics), and a possible dose reduction of quetiapine should be considered.
special instructions
When transferring patients from Seroquel to Seroquel Prolong, the same daily dosage is used, although the number of medication doses is reduced. However, in some cases, adjustments to the dosage as well as the pill plan may be necessary. When using both drugs in the treatment of elderly patients, a reduced daily dose (25 mg) should be started.
Since the side effects of both drugs include drowsiness , you should not drive a vehicle or work with potentially dangerous units and mechanisms during treatment with these drugs.
Seroquel analogs
Level 4 ATX code matches:
Lakvel
Leponex
Zalasta
Quentiax
Closasten
Ketilept
Zyprexa
Clozapine
Quetiapine
Azaleptin
It is worth noting that the main analogue of Seroquel is Seroquel Prolong and vice versa. However, the list of similar drugs that are similar in their structure and mechanism of action to both drugs includes:
- Hedonin;
- Victoel;
- Quetiapine;
- Quentiax;
- Quetiapine fumarate;
- Quentiapin Stada;
- Quentiapine hemifumarate;
- Ketilept;
- Lakvel;
- Ketiap;
- Kutipin;
- Servitel;
- Nantharid.
During pregnancy (and lactation)
As a rule, experts do not recommend taking both drugs during pregnancy , since the effects of quetiapine . However, in cases where the expected benefit outweighs the possible risk, drugs are used in therapeutic treatment under strict medical supervision.
While taking medications, breastfeeding should be stopped.
Reviews of Seroquel
On the forums you can find various reviews of those taking the drugs Seroquel and Seroquel Prolong, as people’s opinions are divided. Some praise these medications, while others, on the contrary, speak negatively about their effectiveness and cost.
Therefore, although many patients leave positive reviews about Seroquel Prolong and Seroquel, a considerable number of patients note an extensive list of side effects, as well as a too “calm” and absolutely inactive state when using them, as a negative side of both drugs.
New possibilities for the use of the atypical antipsychotic Seroquel
The literature describes several approaches to overcoming resistance in cases of GAD [7,15]: 1) drug change - replacing an ineffective antidepressant with an antidepressant of a different pharmacological group; 2) combination therapy - the use of two antidepressants with different mechanisms of action; 3) potentiation of standard therapy - the use of drugs from other pharmacological groups that enhance the effect of serotonin systems (for this purpose, a combination of an antidepressant with thyroid hormone, lithium and other mood stabilizers, benzodiazepines, and also with antipsychotics is used). Today, one of the promising methods for overcoming the resistance of GAD is the potentiation of standard therapy for this disorder (antidepressants) with drugs from other pharmacological groups, most often antipsychotics. The prevalence of this approach is evidenced by the fact that 55–90% of patients with borderline mental disorders, including anxiety disorders, receive combined psychopharmacotherapy, and antidepressants are prescribed together with antipsychotics in approximately half of the cases [11,9]. Numerous studies have been devoted to the use of Seroquel Prolong (quetiapine sustained release) for GAD as monotherapy or as an optimizing treatment strategy, aimed at finding ways to increase effectiveness in resistant GAD. Thus, in a double-blind, placebo-controlled study, patients diagnosed with GAD were randomly divided into three groups. The first group received Seroquel Prolong at a dose of 50 or 150 mg, the second - paroxetine at a dose of 20 mg and the third - placebo. The results were assessed using the Hamilton Anxiety Scale. Analysis of the data obtained showed that the level of remission and response was significantly higher in the Seroquel Prolong and paroxetine groups compared to placebo (p<0.001). In contrast to the placebo group, a statistically significant improvement was observed already on the 4th day of therapy in the Seroquel Prolong group and was not observed in the paroxetine group. Thus, the most rapid improvement in condition and achievement of remission was observed in the Seroquel Prolong group [13]. The presented data were confirmed in three more clinical studies assessing the quality of life of patients with GAD using the Q–LES–Q questionnaire (questionnaire for pleasure and satisfaction with quality of life). The studies involved 2,588 patients who were observed for 8 weeks during therapy with Seroquel Prolong (average dose 150 mg). A generalized analysis of the data obtained led to the conclusion that patients taking Seroquel Prolong noted a statistically significant improvement in their condition in contrast to the placebo groups (p<0.001) [21]. In most studies, Seroquel Prolong was used as a drug that optimized previous therapy. Thus, in a study on the use of Seroquel Prolong as a drug for the treatment of GAD and depressive disorders, its effectiveness, safety and tolerability were assessed. Analysis of the data obtained revealed that Seroquel Prolong at a dose of 50 to 300 mg is effective both in monotherapy and in combination therapy with antidepressants, with incomplete effectiveness of monotherapy with anti-thymoanaleptics. The side effects of Seroquel Prolong assessed in this study, such as sedation and drowsiness, only in isolated cases led to the exclusion of patients from the study [14]. Another placebo-controlled 52-week study assessed the effectiveness of Seroquel Prolong for GAD comorbid with depressive conditions, as an additional drug with a tranquilizing effect. Analysis of the data obtained showed that Seroquel Prolong (dose 150 mg) was superior in effectiveness to placebo and comparable in effectiveness to paroxetine (20 mg) and escitalopram. However, the distinct tranquilizing effect of Seroquel Prolong led in these cases to a more rapid improvement in the patients’ condition [16]. In a 12-week open-label study [17], aimed at studying the tolerability and effectiveness of quetiapine in combination with traditional medications in the treatment of patients with refractory or chronic GAD, the following results were presented. The combination of conventional therapy and quetiapine (mean dose 386 mg) in 32 patients resulted in a significant reduction in baseline HAM-A total score (mean 30.7) at 12 weeks (mean 9.1); the reduction of this indicator averaged 21.7 points (p<0.001). A significant number of patients (75%) achieved remission by the end of week 12 (HARS total score ≥10). However, no serious adverse events were recorded during the study. However, not all studies have confirmed the effectiveness of Seroquel in the treatment of GAD resistant to standard pharmacotherapy. Thus, in a study on the potentiation of paroxetine with an antipsychotic (Seroquel) in resistant GAD, preliminary results were published. The study included patients who, despite pharmacotherapy with an antidepressant (paroxetine), experienced incomplete reduction of symptoms. The study was carried out in two stages. At the first stage, all patients received paroxetine at an average dose of 62.5 mg. Patients who had incomplete reduction of symptoms by the 10th week of therapy (Hamilton Anxiety Scale score > or = 7) were randomized to the quetiapine group (dose from 25 to 400 mg) or the placebo group (continued paroxetine and placebo). According to the study results, the effectiveness of therapy in the Seroquel group was slightly superior to the placebo group (a decrease in the average score on the Hamilton Anxiety Scale in the Seroquel group by an average of 2.6 points, in the placebo group by 0.3 points) [19]. The results of the described clinical studies provide us with heterogeneous data on the effectiveness of the combined use of SSRIs and atypical antipsychotics in patients with GAD who do not respond to standard antidepressant therapy. In this regard, the purpose of this study was to study the characteristics of the course of resistant GAD and evaluate the effectiveness of Seroquel as a potentiation of standard pharmacotherapy with antidepressants in these patients. At the initial stage, the study included 182 patients with GAD (DSM-IV criteria) aged 18–55 years, who for 12 weeks received 2 courses of monotherapy with antidepressants of different mechanisms of action, recommended as first-line drugs: SSRIs, SNRIs and TCAs , prescribed in average therapeutic dosages. Based on the results of assessing the effectiveness of therapy, the main stage of this work included patients who met the following criterion: non-responders to therapy (a decrease in the total number of HARS scores by less than 50%). This criterion, indicating the resistance of GAD, was met by the condition of 33.1% of the patients who compiled the clinical material for the main stage of the work. The psychopathological features of patients with resistant GAD included the leveling of features characteristic of non-resistant GAD and defining its typology with the formation of structurally homogeneous states, in the clinical picture of which the motor component of anxiety, obsessions predominated, as well as pronounced reactive lability of the “remitting reactivity” type with a sharp increase anxiety; expansion of the range of painful disorders due to the addition of dysthymic, severe insomnia (difficulty falling asleep, intermittent sleep) and asthenic symptoms. In accordance with the purpose of this study, all patients with resistant GAD were randomly divided into 2 groups: - the first (main) group was supplemented with Seroquel at a dose of 25–100 mg (30 cases) to a stable dose of a previously taken antidepressant for 6 weeks; – the second (control) group of patients continued to receive a stable dose of the previously taken antidepressant (control – 30 cases). Comparative socio-demographic and clinical characteristics showed that in both groups there was a predominance of females: 73.3% (22 people) in the Seroquel group and 63.3% (19 people) in the control group over males: 26.7 % (8 people) in the Seroquel group and 36.7% (11 people) in the control group. Analysis of the marital status of patients showed that in the first group 40% (12 patients) were married and 43.3% (13 patients) in the second group. 60% (18 people) in the first group and 56.7% (17 patients) in the second were unmarried or divorced. The average age of patients was 34±8.4 years in the Seroquel group and 31.9±9 years in the control group. More than half of the patients included in the study had permanent or part-time employment and stable income: 73.3% (22 patients) in the Serovkel group and 63.3% (19 patients) in the control group. The remaining patients did not work due to personal circumstances or illness - 26.7% (8 people) in the first group and 36.7% (11 people) in the second. A study of anamnestic data showed that among psychopathological disorders detected before the formation of GAD, affective disorders prevailed in all patients. A depressive episode in the first group was detected in 20% (6 patients), in the second in 10% (3 patients). Patients with a history of bipolar disorder were distributed as follows: 6.7% (2 patients) in the Seroquel group and 6.7% (2 patients) in the control group. Depressive reactions were found only in the Seroquel group – 13.3% (4 patients). Other psychopathological disorders in patients belonged to the anxiety-phobic circle (19.9% of patients in the first group and 12.3% in the second) and were represented by panic disorder, social phobia and obsessive-compulsive disorder. The duration of the disease in the studied patients in more than half of the observations varied in the range from 6 months. up to 3 years – 60% (18 patients) – in the first group and 66.7% (20 patients) – in the second. The duration of the disease for more than three years was observed almost half as often: in the Seroquel group – 40% (12 people) and 33.3% (10 people) in the control group. The average age of onset of the disease was 31.7±8.1 years in the main group and 29.4±8.2 years in the control group. One of the important characteristics of GAD used in this study was the clinical typology of GAD [Less Yu.E., 2008], according to which non-resistant GAD is represented by four variants, depending on the predominance of a certain anxiety component in the clinical picture: somato-vegetative, affective, tonic and phobic. The distribution of patients by type of GAD was presented as follows. The phobic type of GAD was observed in 46.7% (14 patients) in the Seroquel group and in 43.3% (13 patients) in the control group. The affective type of GAD occurred in 13.3% (4 patients) in the main group and in 13.3% (4 patients) in the control group. The somato-vegetative type was observed in 13.3% (4 patients) in the Seroquel group and in 16.7% (5 patients) in the control group. The tonic type of GAD was identified in 26.7% (8 patients) in the first group and in 26.7% (8 patients) in the second. The study sample was dominated by patients with schizoid: [40% (12 people) in the Seroquel group and 36.7% (11 people) in the control group] and anxiety circle: [26.7% (8 people) in the first group and 36 .7% (11 people) in the second. A hysterical personality type was observed less frequently: 26.7% (8 people) in the Seroquel group and 23.3% (7 people) in the control group. In isolated cases, patients with dependent and anancastic personality types were encountered in both groups. At the time of inclusion in the main stage of the study, the average value on the HARS scale in the first group was 22.4 (+4.1), and in the second – 21.9 (+3.6). The average Sheehan Anxiety Rating Scale (ShARS) score in the first group was 45.7 (+11.5), and in the second – 45.1 (+10.0). Thus, the presented data show that the differences in the distribution of clinical and demographic parameters between the two groups of patients were insignificant, which made it possible to conduct a comparative analysis of the effectiveness of therapy. Results Treatment effectiveness was assessed weekly using the Hamilton Anxiety Rating Scale (HARS) and the Sheehan Anxiety Rating Scale (ShARS). The results of therapy, assessed at the end of the 6th week, showed (Fig. 1) that the level of remission in the main group reached 26.7%, and in the control group – 6.7% (p<0.05). The number of responders in the main group reached 60%, while the rate in the control group was significantly lower (p<0.05) – 6.7%. Data assessed using the Sheehan Anxiety Scale (ShARS) fully confirmed the results obtained from the analysis of the HARS scale. To compare the time to remission in the groups, the average HARS score was assessed at each week of therapy. Thus, on the 4th week, the remission level reached 6.7% in the Seroquel group, on the 35th day, the percentage of remissions increased to 13.3%, while in the control group, remission was determined only in the last week of the study. Analysis of the rate of reduction in the average score on the HARS scale at each week of therapy compared with background indicators showed that after the first week of therapy in the main group there was a statistically significant decrease in the average score (p<0.05), while in the control group there were differences from the background indicators were detected much later - only at the 3rd week of therapy. Thus, optimization of Seroquel therapy led to a significant increase in the effectiveness of therapy, assessed by the level of remission and response achieved, as well as the time of their onset. To determine the severity of the effect of Seroquel on various components of anxiety (somatic and mental), an analysis of the corresponding subscales of the HARS scale was carried out, which showed that in terms of the rate of reduction in the average score of the “mental” and “somatic” anxiety subscales, statistical differences between the main and control groups were already revealed in the second week of therapy with the advantage of quetiapine. One of the important aspects of assessing the effectiveness of therapy is the study of correlations between the frequency of therapeutic response and the time of development of resistance. Available data on previous psychopharmacotherapy of patients with resistant GAD indicated different periods of its formation. In a larger number of patients (58.7%), it formed almost immediately, i.e. after two consecutive courses of antidepressant therapy – early resistance. In a smaller number of patients (41.5%), it did not develop immediately, but at least after one successful course of psychopharmacotherapy - late resistance. Taking these data into account, the effectiveness of optimizing therapy with Seroquel was analyzed in cases of development of early and late resistance of GAD. Thus, the level of remission was achieved by 87.5% of patients with early resistance, while among patients with late resistance the positive effect of therapy was only 12.5%. On the contrary, there were significantly fewer nonresponders in the group with early formation of resistance – 20%, and in the group with late resistance – 80%. Patients with responder were distributed as follows: 55.6% among patients with early resistance and 44.4% among patients with late resistance. Analysis of the socio-demographic and clinical characteristics of patients with early development of resistance, and therefore with greater effectiveness of optimizing therapy with Seroquel, showed the absence in their history of such anxiety-phobic disorders as panic, social phobia, obsessive-compulsive, absence of bipolar disorders, persistent comorbid symptoms, which, in turn, was typical for patients with late development of resistance and less effective treatment. Thus, adding the atypical antipsychotic Seroquel to the basic antidepressant therapy for patients with resistant GAD optimizes the psychopharmacotherapeutic effect, increasing the effectiveness of treatment by 87%. The greatest effectiveness of therapy is observed in patients over 30 years of age, with anxious, suspicious and schizoid personality accentuations without a history of psychopathological disorders, with favorable clinical variants of generalized anxiety (somato-vegetative and affective), with an early onset of response (in the 3rd week) and early formation of resistance. At the moment, the possibility of treating GAD with Seroquel is not registered in the Russian Federation. At the same time, this indication for Seroquel Prolong has been officially registered in a number of countries, which recently became available to psychiatrists in Russia.
Literature 1. Avedisova A.S., Synergism of the effects of “double” action antidepressants. Pharmaceutical Bulletin - May 2006 - No. 18 (423). 2. Aleksandrovsky, Yu. A. Borderline mental disorders: textbook. Allowance; Yu. A. Alexandrovsky. 3rd ed., revised. and additional M.: Medicine, 2000. 3. Smulevich A.B. Borderline mental disorders. Manual of Psychiatry. Ed. A.S. Tiganova. M.: Medicine, 1999; 2:527–606. 4. Vovin R. Ya., Aksenova L. I., Küne G. E. The problem of chronicization of psychoses and overcoming therapeutic resistance (using the model of depressive states) // Pharmacotherapeutic foundations of rehabilitation of mentally ill patients. - M.: Medicine, 1989. - P. 151–181. 5. Katzung B. G. Basic and clinical pharmacology: In 2 volumes / Transl. from English - M.-SPb: Binom, 1998. - T. 1. - P. 12–100 6. Lawrence D. R., Benitt P. N. Clinical pharmacology: In 2 volumes / Transl. from English - T. 1. - M.: Medicine, 1991. - P. 11–264. 7. G. E. Mazo, S. E. Gorbachev, N. N. Petrova. Treatment-resistant depression: modern approaches to diagnosis and treatment // Bulletin of St. Petersburg University. – Ser. 11. 2008. Issue. 2 – pp. 87–96. 8. Mosolov S. N. Clinical use of modern antidepressants. - St. Petersburg: Medical Information Agency, 1995. - 568 p. 9. Neznamov G. G., Combined psychopharmacotherapy: a modern concept Report at the symposium “Neuropsychotropic drugs”, Moscow, November 1994 10. Podkorytov V. S., Chaika Yu. Yu. Depression and resistance // Journal of Psychiatry and Medical Psychology . - 2002. - No. 1. - P. 118–124. 11. Yanichak F. J., Davis D. M., Aid F. J. Principles and practice of psychopharmacotherapy / Transl. from English - Kyiv: Nika-Center, 1999. - 694 p. 12. Altamura AC, Percudani M. The use of antidepressants for long-term treatment of recurrent depression // Journal of Clinical Psychiatry. - 1993. - Vol. 54, No. 8. - P. 29–38. 13. Bandelow B, Chouinard G, Bobes J, Ahokas A, Eggens I, Liu S, Eriksson H. Extended–release quetiapine fumarate (quetiapine XR): a once–daily monotherapy effective in generalized anxiety disorder. Data from a randomized, double-blind, placebo- and active-controlled study // Int J Neuropsychopharmacol. 2010 Apr;13(3):305–20. Epub 2009 Aug 20. 14. Baune BT. New disorder developments in the management of major depressive disorder and generalized anxiety: role of quetiapine // Neuropsychiatr Dis Treat. 2008 Dec;4(6):1181–91. 15. Cowen PJ Pharmacological management of treatment–resistant depression // Advances in Psychiatric Treatment. - 1998. - Vol. 4. - P. 320–327. 16. Gao K, Sheehan DV, Calabrese JR. Atypical antipsychotics in primary generalized anxiety disorder or comorbid with mood disorders // Expert Rev Neurother. 2009 Aug;9(8):1147–58. 17. M. Katzman, M. Vermani, L. Jacobs, M. Marcus, B. Kong, S. Lessard, W. Galarraga, L. Struzik, A. Gendron. An open-label study of the efficacy and safety of flexible-dose quetiapine (Seroquel) in combination therapy for generalized anxiety disorder. Review of Psychiatry and Medical Psychology named after. Bekhtereva No. 4 2008 18. Keller MB Course outcome and impact on the community // Acta Psychiat. Scand. - 1994. - Vol. 89. - P. 24–34. 19. Simon NM, Connor KM, LeBeau RT, Hoge EA, Worthington JJ 3rd, Zhang W, Davidson JR, Pollack MH. Quetiapine augmentation of paroxetine CR for the treatment of refractory generalized anxiety disorder: preliminary findings // Psychopharmacology (Berl). 2008 May;197(4):675–81. Epub 2008 Feb 2. 20. Way K., Young Ch. H. et al. Antidepressant utilization patterns in a National Managed Care Organization // Drug Benefit Trends. - 1999. - Vol. 11, No. 9. - P. 6–11. 21. Wyrwich K, Harnam N, Revicki DA, Locklear JC, Svedsater H, Endicott J. Assessing health–related quality of life in generalized anxiety disorder using the Quality Of Life Enjoyment and Satisfaction Questionnaire // Int Clin Psychopharmacol. 2009 Nov; 24(6):289–95.
Seroquel price, where to buy
You can buy both drugs in pharmacies with a doctor's prescription. It is worth noting that these drugs are not cheap, for example, the average price of Seroquel Prolonga 300 mg. (60 tablets in one package) reaches 1100 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
LuxPharma* special offer
- Seroquel Prolong tablet.
400 mg No. 60 RUR 10,500 order
ZdravCity
- Seroquel tab. p.p.o. 100 mg n60AstraZeneca Pharmaceutical Co., Ltd./AstraZeneca UK Limited
1125 rub. order
- Seroquel tab. p.p.o. 25mg n60AstraZeneca Pharmaceutical Co., Ltd./AstraZeneca UK Limited
925 rub. order
- Seroquel tab. p.p.o. 200 mg n60AstraZeneca Pharmaceutical Co., Ltd./AstraZeneca UK Limited
RUR 2,028 order
- Seroquel Prolong tab. prolong d-i p/o captivity. 0.3g 60pcs AstraZeneca Pharmaceuticals LP/LLC AstraZeneca Industries
RUB 2828 order
- Seroquel Prolong tab prolong. valid p/o captivity. 0.2g 60pcsAstraZeneca Pharmaceuticals LP/LLC AstraZeneca Industries
RUB 1,756 order
Pharmacy Dialogue
- Seroquel (tab.p.pl/vol. 25 mg No. 60)Astra Zenesa/AstraZeneca Industries
RUR 732 order
- Seroquel (tablet p/o 200 mg No. 60)Astra Zeneca/ZIO Zdorovye
RUR 1,984 order
- Seroquel (tablet p/o 100 mg No. 60)Astra Zeneca/ZIO Zdorovye
RUR 978 order
- Seroquel (tablet p/o 25 mg No. 60)Astra Zeneca/ZIO Zdorovye
RUB 774 order
show more
Pharmacy24
- Seroquel XR 50 mg No. 60 tablets Astra Zeneca UK Limited, UK
810 UAH.order - Seroquel XR 200 mg N60 tablets Astra Zeneca UK Limited, UK
1579 UAH. order


![Table 1. Bioavailability (absorption) of various organic forms of calcium within 2 hours after oral administration in the experiment [22]](https://laram-halal.ru/wp-content/uploads/tablica-1-biousvoyaemost-absorbciya-razlichnyh-organicheskih-form-kalciya-v-techenie-330x140.jpg)