Effect of risperidone
The mechanism of action is caused by the effect on dopamine, serotonin, adrenergic and histamine receptors of nerve cells. Due to the fact that in many endogenous, organic mental diseases the functions of these receptor systems are changed, risperidone has a fairly broad therapeutic effect:
- For productive symptoms of psychosis and schizophrenia (delusions and hallucinations), for negative ones - apathy, isolation, lack of emotions, autism.
- Reduces pathologically elevated mood (mania).
- Calming, anti-anxiety, hypnotic effect.
- Reduces (or removes) aggressiveness, self-aggression.
- Anti-suicidal action.
- Reducing the pathological craving for drugs and alcohol in case of addiction.
- Removes obsessive thoughts, actions and sensations.
Risperidone (Rispolept, Torendo, Rispaxol)
Contraindications
Hypersensitivity to risperidone.
Dosage
Individual. When taken orally, the initial dose for adults is 0.25-2 mg/day, on the 2nd day - 4 mg/day. Then the dose can either be kept at the same level or, if necessary, adjusted. Typically, the optimal therapeutic dose, depending on the indications, is in the range of 0.5-6 mg/day. In some cases, a slower dose escalation and lower initial and maintenance doses may be justified.
For schizophrenia, for elderly patients, as well as for concomitant liver and kidney diseases, an initial dose of 500 mcg 2 times a day is recommended. If necessary, the dose can be increased to 1-2 mg 2 times a day.
Maximum dose: When using risperidone at a dose of more than 10 mg/day, there is no increase in effectiveness compared to lower doses, but the risk of developing extrapyramidal symptoms increases. The safety of risperidone in doses greater than 16 mg/day has not been studied, so further excess of the dose is not allowed.
Side effects
From the side of the central nervous system: often - insomnia, agitation, anxiety, headache; possible - drowsiness, fatigue, dizziness, impaired ability to concentrate, impaired vision; rarely - extrapyramidal symptoms (including tremor, rigidity, hypersalivation, bradykinesia, akathisia, acute dystonia). Patients with schizophrenia may experience tardive dyskinesia, NMS, thermoregulation disorders, and seizures.
From the digestive system: constipation, dyspeptic symptoms, nausea, vomiting, abdominal pain, increased activity of liver enzymes.
From the reproductive system: priapism, erectile dysfunction, ejaculation disorders, orgasm disorders.
From the cardiovascular system: rarely - orthostatic hypotension and reflex tachycardia, arterial hypertension.
From the endocrine system: galactorrhea, gynecomastia, menstrual irregularities, amenorrhea, weight gain.
From the hematopoietic system: a slight decrease in the number of neutrophils and/or platelets.
Allergic reactions: rhinitis, skin rash, angioedema.
Other: urinary incontinence.
Drug interactions
With the simultaneous use of inducers of microsomal liver enzymes, a decrease in the concentration of risperidone in the blood plasma is possible.
When used simultaneously with phenothiazine derivatives, tricyclic antidepressants and beta-blockers, the concentration of risperidone in the blood plasma may increase.
When used simultaneously with carbamazepine, the concentration of risperidone in the blood plasma is significantly reduced.
When used concomitantly, risperidone reduces the effects of levodopa and other dopamine receptor agonists.
When used simultaneously with fluoxetine, an increase in the concentration of risperidone in the blood plasma is possible.
special instructions
Use with caution in patients with diseases of the cardiovascular system (including heart failure, myocardial infarction, cardiac muscle conduction disorders), as well as in cases of dehydration, hypovolemia or cerebrovascular disorders. In this category of patients, the dose should be increased gradually.
The risk of developing orthostatic hypotension is especially increased in the initial period of dose selection. If hypotension occurs, dose reduction should be considered.
When using drugs that have the properties of dopamine receptor antagonists, the occurrence of tardive dyskinesia, characterized by involuntary rhythmic movements (mainly of the tongue and/or face), was noted. There are reports that the occurrence of extrapyramidal symptoms is a risk factor for the development of tardive dyskinesia. Risperidone causes extrapyramidal symptoms to a lesser extent than classical antipsychotics. If symptoms of tardive dyskinesia occur, discontinuation of all antipsychotic medications should be considered.
If NMS develops, all antipsychotics, including risperidone, should be discontinued.
Risperidone should be used with caution in patients with Parkinson's disease, as it is theoretically possible that the disease may worsen.
Classical antipsychotics are known to lower the seizure threshold. Given this, risperidone is recommended to be used with caution in patients with epilepsy.
Risperidone should be used with caution in combination with other centrally acting drugs.
When discontinuing carbamazepine and other hepatic enzyme inducers, the dose of risperidone should be reconsidered and, if necessary, reduced.
During the treatment period, patients should be advised to refrain from overeating due to the possibility of weight gain.
There are no data on the safety of risperidone in children under 15 years of age.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, until individual sensitivity to risperidone is determined, patients should avoid driving vehicles and other activities that require high concentration and speed of psychomotor reactions.
Pregnancy and lactation
Use during pregnancy is possible if the expected benefit of therapy for the mother outweighs the potential risk to the fetus. If use is necessary during lactation, breastfeeding should be discontinued.
Use in childhood
There are no data on the safety of risperidone in children under 15 years of age.
For impaired renal function
For schizophrenia with concomitant kidney diseases, an initial dose of 500 mcg 2 times a day is recommended. If necessary, the dose can be increased to 1-2 mg 2 times a day.
For liver dysfunction
For schizophrenia with concomitant liver diseases, an initial dose of 500 mcg 2 times a day is recommended. If necessary, the dose can be increased to 1-2 mg 2 times / day.
Use in old age
For schizophrenia, an initial dose of 500 mcg 2 times a day is recommended for elderly patients. If necessary, the dose can be increased to 1-2 mg 2 times a day.
Release form
One of the advantages of this drug is the presence of all the dosage forms necessary for psychiatrists: tablets, drops, extended-release injections (depot).
Pills
2 or 4 milligrams per package of 10,20,30,50,60 or 100 pieces
Drops
. In bottles of 30 or 100 milliliters. A special graduated pipette is included, which is used to determine the amount of a single dose to take.
Depot
. In powder form for the preparation of a long-acting intramuscular suspension. Dosages: 25, 37.5 and 50 milligrams. It is used as an intramuscular injection, which will ensure slow release and entry of the drug into the blood over 2 - 3 weeks. Produced under the name RISPOLEPT CONST.
Rispolept oral solution 1 mg/ml 30 ml bottle in Moscow
Inside,
regardless of food intake.
Schizophrenia
Adults.
Rispolept® can be prescribed 1 or 2 times a day. The initial dose of Rispolept® is 2 mg/day. On the second day, the dose should be increased to 4 mg/day. From this point on, the dose can either be kept at the same level or individually adjusted if necessary. Typically the optimal dose is 4–6 mg/day. In some cases, a slower dose escalation and lower initial and maintenance doses may be justified.
Doses above 10 mg/day do not show greater efficacy than lower doses and may cause extrapyramidal symptoms. Due to the fact that the safety of doses above 16 mg/day has not been studied, doses above this level cannot be used.
Benzodiazepines can be added to Rispolept® therapy if additional sedation is required.
Elderly patients.
The recommended initial dose is 0.5 mg per dose 2 times a day. The dose can be individually increased by 0.5 mg 2 times a day to 1–2 mg 2 times a day.
Teenagers over 13 years old.
The recommended initial dose is 0.5 mg once daily in the morning or evening. If necessary, the dose can be increased after at least 24 hours by 0.5–1 mg per day to the recommended dose of 3 mg/day if well tolerated. The safety of doses above 6 mg/day has not been studied.
For patients who experience persistent drowsiness, it is recommended to take half the daily dose 2 times a day.
There is no information on the use of the drug for the treatment of schizophrenia in children under 13 years of age.
Behavioral disorders in patients with dementia
The recommended initial dose is 0.25 mg per dose 2 times a day. If necessary, the dose can be increased individually by 0.25 mg 2 times a day, no more than every other day. For most patients, the optimal dose is 0.5 mg 2 times a day. However, some patients are advised to take 1 mg 2 times a day.
Once the optimal dose is reached, it may be recommended to take the drug once a day.
Bipolar disorders with mania
Adults.
The recommended initial dose of the drug is 2 or 3 mg/day at a time. If necessary, this dose can be increased at least after 24 hours by 1 mg/day. For most patients, the optimal dose is 1–6 mg/day.
Teenagers and children over 10 years old.
The recommended initial dose is 0.5 mg once daily in the morning or evening. If necessary, the dose can be increased after at least 24 hours by 0.5–1 mg/day to the recommended dose of 2.5 mg/day if well tolerated. For most patients, the optimal dose is 0.5–6 mg/day.
The safety of doses above 6 mg/day has not been studied.
For patients who experience persistent drowsiness, it is recommended to take half the daily dose 2 times a day.
There is no information on the use of the drug for the treatment of bipolar disorders in children under 10 years of age.
Behavioral disorders
Patients weighing 50 kg or more.
The recommended initial dose of the drug is 0.5 mg once a day. If necessary, this dose can be increased by 0.5 mg/day no more than every other day. For most patients, the optimal dose is 1 mg/day. However, for some patients, 0.5 mg/day is preferable, while some require an increase in dose to 1.5 mg/day.
Patients weighing less than 50 kg.
The recommended initial dose of the drug is 0.25 mg once a day. If necessary, this dose can be increased by 0.25 mg/day no more than every other day. For most patients, the optimal dose is 0.5 mg/day. However, for some patients, 0.25 mg/day is preferable, while some require an increase in dose to 0.75 mg/day.
Long-term use of the drug Rispolept® in adolescents should be carried out under the constant supervision of a physician.
Use in children under 5 years of age has not been studied.
Autism in children and adolescents
The dose of Rispolept® should be selected individually. The recommended initial dose of the drug is 0.25 mg/day for patients weighing less than 20 kg and 0.5 mg/day for patients weighing 20 kg or more. On the 4th day of administration, the dose can be increased by 0.25 mg/day for patients weighing less than 20 kg and by 0.5 mg/day per day for patients weighing 20 kg or more.
This dose should be used until approximately the 14th day of treatment, when it is necessary to evaluate the effectiveness. Further increase in dose is carried out only in case of lack of effectiveness. The dose can be increased at intervals of 2 weeks or more by 0.25 mg/day for patients weighing less than 20 kg and by 0.5 mg/day for patients weighing 20 kg or more.
In clinical studies, the maximum daily dose did not exceed 1.5 mg/day for patients weighing less than 20 kg and 2.5 mg/day for patients weighing 20 kg or more, and 3.5 mg/day for patients with weight body more than 45 kg.
Table
Doses of the drug Rispolept® in the treatment of autism in children (per day)
| Body weight, kg | Days 1–3, mg | Days 4–14+, mg | Increase the dose (if necessary) | Recommended dose, mg |
| Less than 20 | 0,25 | 0,5 | +0.25 mg after 2 weeks or more | 0,5–1,5 |
| 20 or more | 0,5 | 1 | +0.5 mg after 2 weeks or more | 1–2,5* |
* For patients weighing more than 45 kg, higher doses may be required, the maximum dose studied is 3.5 mg/day.
Rispolept® can be prescribed 1 or 2 times a day.
For patients who experience persistent drowsiness, it is recommended to take a daily dose 1 time before bedtime or 2 times a day.
If consistent efficacy is observed, the decision may be made to gradually reduce the dose to achieve an optimal balance of efficacy and safety.
Use in children under 5 years of age has not been studied.
Other patient groups
Patients with liver and kidney diseases.
Patients with kidney disease have a reduced ability to eliminate the active antipsychotic fraction compared to other patients. In patients with liver disease, there is an increased concentration of the free fraction of risperidone in the blood plasma.
The initial and maintenance dose, in accordance with the indications, should be reduced by 2 times; the dose increase in patients with liver and kidney diseases should be carried out more slowly.
Rispolept® should be prescribed with caution in this category of patients.
Indications
Risperidone was originally used to treat schizophrenia and psychosis. But as experience has accumulated about the action of this medicine, the indications for its use have expanded. Currently indicated for the following diseases and conditions:
- Schizophrenia
- Schizotypal disorder
- Organic mental disorders
- Schizoid personality disorder
- Manic and hypomanic states in bipolar affective disorder, schizoaffective disorder
- Psychoses
- Delusions: paranoia, paranoid, paraphrenia
- Depressive and anxiety states, neuroses and neurosis-like conditions
- Aggressiveness
- Autism
The drug is recommended for adults and children over 13 years of age. At a younger age, it is prescribed by the doctor’s decision in cases where the potential risk of side and negative effects of the drug is less than the risk of worsening the condition as the disease progresses.
Instructions for use RISPOLEPT®
The drug should be used with caution in patients with diseases of the cardiovascular system (including chronic heart failure, previous myocardial infarction, conduction disorders), dehydration, hypovolemia, cerebrovascular accident, Parkinson's disease, convulsions (including history), severe renal or hepatic failure, drug abuse or drug dependence, conditions predisposing to the development of torsade de pointes (bradycardia, electrolyte imbalance, concomitant use of drugs that prolong the QT interval), brain tumors , intestinal obstruction, in cases of acute drug overdose, in Reye's syndrome (since the antiemetic effect of risperidone can mask the symptoms of these conditions), during pregnancy, in patients under the age of 15 years (since the safety and effectiveness of the drug have not been established) .
In case of schizophrenia, at the beginning of treatment with Rispolept, it is recommended to gradually discontinue previous therapy if clinically justified. At the same time, if patients are transferred from depot therapy with antipsychotic drugs, it is recommended to start Rispolept therapy instead of the next scheduled injection. The need to continue current antiparkinsonian drug therapy should be periodically assessed.
Due to the alpha-adrenergic blocking effect of Rispolept, orthostatic hypotension may occur, especially during the initial dose selection period. If arterial hypotension occurs, dose reduction should be considered. In patients with diseases of the cardiovascular system, as well as in cases of dehydration, hypovolemia or cerebrovascular disorders, the dose should be increased gradually.
There are reports that the occurrence of extrapyramidal symptoms is a risk factor for the development of tardive dyskinesia. Rispolept is less likely to cause extrapyramidal symptoms than classic antipsychotics. If signs and symptoms of tardive dyskinesia occur, discontinuation of all antipsychotic medications should be considered.
In case of development of NMS, characterized by hyperthermia, muscle rigidity, instability of autonomic functions, disturbances of consciousness and increased CPK levels, it is necessary to discontinue all antipsychotic drugs, including Rispolept.
When carbamazepine and other liver enzyme inducers are discontinued, the dose of Rispolept should be reduced.
During treatment with Rispolept, patients should be advised to refrain from overeating due to the possibility of weight gain.
Use in pediatrics
Data on the safety and effectiveness of Rispolept in children under 15 years of age
are absent, so prescribing the drug to this category of patients is not recommended. Long-term use of Rispolept in adolescents should be carried out under the constant supervision of a physician.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, until individual sensitivity to the drug is determined, patients should avoid driving vehicles and other activities that require high concentration and speed of psychomotor reactions.
Use during pregnancy and breastfeeding
There are no absolute contraindications to taking risperidone during pregnancy and lactation. However, due to the lack of special research in this direction, use during pregnancy is allowed only in cases described by the following formulation: when the benefits of taking it for the pregnant woman outweigh the potential risks to the fetus.
Due to the fact that risperidone passes into breast milk, it is recommended to transfer the child to artificial nutrition for the period of treatment of a breastfeeding mother.
Rispolept drops 1mg/ml 30ml N1 (Johnson)
Use in elderly patients with dementia
Increased mortality in older patients with dementia
Elderly patients with dementia treated with atypical antipsychotics experienced increased mortality compared with placebo in studies of atypical antipsychotics, including risperidone. When using risperidone in this population, the incidence of death was 4.0% for patients taking risperidone compared with 3.1% for placebo. The mean age of patients who died was 86 years (range, 67–100 years). Data collected from two large observational studies show that older patients with dementia treated with typical antipsychotic medications also have a slightly increased risk of death compared with patients not treated. At present, insufficient data have been collected to accurately assess this risk. The reason for the increase in this risk is also unknown. Also unknown is the extent to which the increased mortality may be attributable to antipsychotic drugs rather than to the characteristics of this patient population.
Combined use with furosemide
In elderly patients with dementia, there was an increased mortality rate when taking furosemide and oral risperidone concomitantly (7.3%, mean age 89 years, range 75-97 years) compared with the risperidone alone group (3.1%, mean age 84 years , range 70-96 years) and the furosemide-only group (4.1%, mean age 80 years, range 67-90 years). An increase in mortality in patients taking risperidone with furosemide was observed in 2 of 4 clinical studies. Concomitant use of risperidone with other diuretics (mainly low-dose thiazide diuretics) was not associated with an increase in mortality.
No pathophysiological mechanisms have been established to explain this observation. However, special care should be taken when prescribing the drug in such cases. Before prescribing, the risk/benefit ratio must be carefully assessed. There was no increase in mortality in patients taking other diuretics concomitantly with risperidone. Regardless of treatment, dehydration is a common risk factor for mortality and should be carefully monitored in older patients with dementia.
In elderly patients with dementia, an increase in cerebrovascular adverse events (acute and transient cerebrovascular accidents), including patient deaths (mean age 85 years, range 73-97 years) was observed with risperidone compared with placebo.
Cardiovascular effects
In placebo-controlled clinical trials, an approximately 3-fold increased risk of cerebrovascular side effects was observed in patients with dementia taking certain atypical antipsychotic drugs. Pooled data from 6 placebo-controlled studies involving primarily elderly patients with dementia (age >65 years) demonstrate that cerebrovascular adverse events (serious and non-serious) occurred in 3.3% (33/1009) of patients treated with risperidone. and in 1.2% (8/712) of patients receiving placebo. The risk ratio was 2.96 (1.34, 7.50) with a 95% confidence interval. The mechanism by which this risk increases is unknown. An increased risk cannot be excluded for other antipsychotic drugs, as well as for other patient populations. Rispolept® should be used with caution in patients with risk factors for stroke.
The risk of cerebrovascular side effects is much higher in patients with mixed or vascular dementia compared to patients with Alzheimer's dementia. Therefore, patients with any type of dementia other than Alzheimer's should not take risperidone.
Physicians should assess the risk/benefit ratio of using Rispolept® in elderly patients with dementia, taking into account the precursors of stroke risk individually for each patient.
Patients and caregivers should be cautioned to immediately report signs and symptoms of cardiovascular events, such as sudden weakness or stiffness/numbness in the face, legs, arms, as well as difficulty speaking and vision problems. All possible treatment options should be considered, including discontinuation of risperidone.
Rispolept® should only be used for the short-term treatment of persistent aggression in patients with moderate to severe Alzheimer's dementia, as an adjunct to non-pharmacological treatments when they are ineffective or of limited effectiveness, and when there is a risk of harm to the patient himself or herself to other persons.
Patients' condition and the need for continued risperidone therapy should be continually assessed.
Orthostatic hypotension
Risperidone has alpha-blocking activity and may therefore cause orthostatic hypotension in some patients, especially during initial dose titration. Clinically significant hypotension has been observed in the post-marketing period when used concomitantly with antihypertensive drugs. Rispolept® should be used with caution in patients with known cardiovascular disease (eg, heart failure, myocardial infarction, cardiac conduction disorders, dehydration, hypovolemia or cerebrovascular disease). Appropriate dose adjustment is also necessary. It is recommended to evaluate the possibility of dose reduction if hypotension occurs.
Tardive dyskinesia and extrapyramidal disorders
Drugs with dopamine receptor antagonist properties can cause tardive dyskinesia, which is characterized by rhythmic involuntary movements, mainly of the tongue and/or facial muscles. The occurrence of extrapyramidal symptoms is a risk factor for the development of tardive dyskinesia. If a patient experiences objective or subjective symptoms indicating tardive dyskinesia, the advisability of discontinuing all antipsychotic drugs, including Rispolept®, oral solution, should be considered.
Neuroleptic malignant syndrome (NMS)
Antipsychotics, including risperidone, may cause neuroleptic malignant syndrome (NMS), which is characterized by hyperthermia, muscle rigidity, instability of autonomic nervous system function, depression of consciousness, and increased serum concentrations of creatine phosphokinase. Myoglobinuria (rhabdomyolysis) and acute renal failure may also occur in patients with NMS. If a patient experiences objective or subjective symptoms of NMS, all antipsychotic drugs, including Rispolept®, must be immediately discontinued.
Parkinson's disease and dementia with Lewy bodies
Antipsychotic medications, including Rispolept®, should be prescribed with caution to patients with Parkinson's disease or dementia with Lewy bodies. Both groups of patients have an increased risk of developing neuroleptic malignant syndrome and increased sensitivity to antipsychotic drugs (including dullness of pain sensitivity, confusion, postural instability with frequent falls and extrapyramidal symptoms). Parkinson's disease may worsen when taking risperidone.
Hyperglycemia and diabetes mellitus
Hyperglycemia, diabetes mellitus, and exacerbation of existing diabetes mellitus were observed during treatment with Rispolept®. It is likely that weight gain prior to treatment is also a predisposing factor. Very rarely, ketoacidosis and rarely, diabetic coma can occur. All patients should be clinically monitored for symptoms of hyperglycemia (such as polydipsia, polyuria, polyphagia and weakness). Patients with diabetes mellitus should be regularly monitored for worsening glucose control.
Weight gain
During treatment with Rispolept®, a significant increase in body weight was observed. It is necessary to monitor patients' body weight.
Hyperprolactinemia
Based on the results of tissue culture studies, it has been suggested that the growth of breast tumor cells may be stimulated by prolactin. Although clinical and epidemiological studies have not shown a clear association between hyperprolactinemia and antipsychotic drug use, caution should be exercised when prescribing risperidone to patients with a history of this. Rispolept® should be used with caution in patients with existing hyperprolactinemia and in patients with possible prolactin-dependent tumors.
Prolongation of the QT interval
QT prolongation has been observed very rarely during post-marketing surveillance. As with other antipsychotics, caution should be exercised when prescribing Rispolept® to patients with known cardiovascular diseases, family history of QT interval prolongation, bradycardia, electrolyte imbalance (hypokalemia, hypomagnesemia), as this may increase the risk of an arrhythmogenic effect; and when used together with drugs that prolong the QT interval.
Convulsions
Rispolept® should be used with caution in patients with a history of seizures or other medical conditions that may lower the seizure threshold.
Priapism
Priapism may occur with risperidone due to alpha-blocking effects.
Body temperature regulation
Antipsychotic drugs are associated with such undesirable effects as disruption of the body's ability to regulate temperature. Caution should be exercised when prescribing Rispolept® to patients with conditions that may contribute to an increase in core body temperature, such as intense physical activity, dehydration, exposure to high external temperatures, or concomitant use of drugs with anticholinergic activity.
Venous thromboembolism
Cases of venous thromboembolism have been reported with the use of antipsychotic drugs. Since patients taking antipsychotic drugs are often at risk of developing venous thromboembolism, all possible risk factors should be identified before and during treatment with Rispolept®, and preventive measures should be taken.
Children and teenagers
Before prescribing Rispolept® to children or adolescents with mental retardation, their condition must be carefully assessed for the presence of physical or social causes of aggressive behavior, such as pain or inadequate demands of the social environment.
The sedative effect of risperidone should be carefully monitored in this population due to the possible effect on learning ability. Changing the timing of risperidone administration may improve control of the effects of sedation on attention in adolescents and children. Risperidone use was associated with mean increases in body weight and body mass index. Height changes in longitudinal studies were within expected age-related norms. The effects of long-term use of risperidone on sexual development and growth have not been fully studied.
Due to the possible impact of prolonged hyperprolactinemia on growth and sexual development in children and adolescents, regular clinical assessment of hormonal status should be carried out, including measurement of height, weight, monitoring of sexual development, menstrual cycle and other possible prolactin-dependent effects.
During treatment with risperidone, regular monitoring for the presence of extrapyramidal symptoms and other movement disorders should be carried out.
Side effects
The drug is usually well tolerated. According to clinic doctors, it is one of the well-tolerated antipsychotics. In approximately 10% of cases, the following side effects are possible.
- Increased muscle tone, restlessness, trembling, feeling of stiffness, “extrapyramidal syndrome,” parkinsonism. To prevent these phenomena, correctors may be additionally prescribed: trihexyphenidyl (Cyclodol), biperiden (Akineton, Mendylex, Bezac), amantadine (PK-Merz), etc.
- Headache.
- Insomnia.
Rare but unpleasant side effects include metabolic (metabolic) disorders: weight gain and the development of diabetes. As a rule, such effects develop in persons predisposed to this.
Therefore, to avoid them, it is recommended to conduct an examination with blood tests before starting therapy to exclude an increase in glucose and prolactin in the blood.
Rispolept®
Side effects of the drug Rispolept® in therapeutic doses are given with a distribution by frequency and system-organ classes. Determination of the frequency of side effects: very often (≥1/10), often (≥1/100 and <1/10), infrequently (≥1/1000 and <1/100), rarely (≥1/10,000 and <1 /1000), very rare (< 1/10,000).
Infections:
very often - in elderly patients with dementia - urinary tract infections; often - nasopharyngitis, upper respiratory tract infections, sinusitis, urinary tract infections, in elderly patients with dementia - pneumonia, phlegmon, in children - rhinitis, influenza-like diseases; uncommon - ear infections, viral infections, pharyngitis, tonsillitis, bronchitis, eye infections, localized infections, cystitis, onychomycosis, acrodermatitis, bronchopneumonia, respiratory tract infections, tracheobronchitis.
Mental disorders:
very often - insomnia; often - anxiety, nervousness, in elderly patients with dementia - confusion, in children - lethargy; infrequently - agitation, flattening of affect, sleep disturbances, weakened libido, anorgasmia; very rarely - mania.
From the nervous system:
very often - parkinsonism (including extrapyramidal disorders, cogwheel syndrome, akinesia, bradykinesia, hypokinesia, muscle rigidity), in children - drowsiness, headaches, sedation; often - akathisia (including restlessness), drowsiness, dizziness, sedation, tremor, dystonia (including muscle spasms, involuntary muscle contractions, muscle contracture, involuntary eye movements, tongue paralysis), lethargy, postural dizziness, dyskinesia (including muscle twitching, chorea and choreoathetosis), fainting, in elderly patients with dementia - a depressed state, in children - dysarthria, impaired attention, gait disturbance; uncommon - lack of response to stimuli, loss of coordination, loss of consciousness, speech impairment, hypoesthesia, movement disorder, tardive dyskinesia, cerebral ischemia, cerebrovascular disorders, NMS.
From the senses:
often - impaired visual acuity, ear pain, in elderly patients with dementia - conjunctivitis; uncommon - tinnitus, conjunctival hyperemia, blurred vision, involuntary rotation of the eyeballs, swelling of the eyelids, periorbital edema, crust formation on the edges of the eyelids, dry eyes, increased lacrimation, photophobia, increased intraocular pressure.
From the cardiovascular system:
often - tachycardia, orthostatic hypotension, decreased blood pressure, in elderly patients with dementia - transient ischemic attack, myocardial infarction, stroke, in children - palpitations; uncommon - sinus bradycardia, sinus tachycardia, palpitations, AV block, right and left bundle branch block, flushing; very rarely - atrial fibrillation.
From the respiratory system:
often - nasal congestion, shortness of breath, nosebleeds, sinus congestion, in elderly patients with dementia - cough, rhinorrhea, in children - cough, rhinorrhea, pain in the larynx and pharynx, pulmonary congestion; uncommon - wheezing, aspiration pneumonia, dysphonia, productive cough, airway obstruction, moist rales, respiratory distress, nasal swelling, hyperventilation; very rarely - sleep apnea syndrome.
From the digestive system:
often - nausea, constipation, dyspepsia, vomiting, diarrhea, salivation, dry mouth, stomach discomfort, abdominal pain; in elderly patients with dementia - dysphagia, fecaloma; infrequently - encopresis, gastritis, swelling of the lips, cheilitis, aptialism; very rarely - intestinal obstruction, pancreatitis, jaundice.
From the hematopoietic system:
often - anemia; uncommon - granulocytopenia; very rarely - thrombocytopenia, agranulocytosis.
Allergic reactions:
uncommon - hypersensitivity; very rarely - Quincke's edema, anaphylactic shock.
From the endocrine system:
uncommon - hyperprolactinemia, diabetic coma; very rarely - impaired ADH secretion.
From the side of metabolism:
often in elderly patients with dementia there is a decrease in appetite, in children there is an increase in appetite; infrequently - polydipsia, anorexia; rarely - diabetic ketoacidosis, diabetes mellitus, hypoglycemia, water intoxication.
Dermatological reactions:
often - rash, dry skin, dandruff, seborrheic dermatitis, hyperkeratosis, in elderly patients with dementia - erythema, in children - itching, acne; uncommon - skin pigmentation disorders, erythematous rashes, papular rashes, generalized rash, maculopapular rash; very rarely - alopecia.
From the musculoskeletal system:
often - back pain, arthralgia, pain in the limbs, in elderly patients with dementia - gait disturbances, swelling of the joints, in children - myalgia, neck pain; Uncommon: muscle pain in the chest, joint stiffness, muscle weakness, rhabdomyolysis.
From the urinary system:
often - urinary incontinence, in children - enuresis, pollakiuria; uncommon - pain when urinating; very rarely - urinary retention.
From the reproductive system:
often - lack of ejaculation, in children - galactorrhea; uncommon - menstrual irregularities, amenorrhea, gynecomastia, vaginal discharge, erectile dysfunction, ejaculation disorders, breast enlargement, sexual dysfunction, retrograde ejaculation; very rarely - priapism.
From the side of metabolism:
often - fatigue, asthenia, fever, pain in the chest; in elderly patients with dementia - peripheral edema, gait disturbance; in children - slowness, discomfort in the chest; infrequently - thirst, flu-like condition, edema, poor health, facial swelling, general edema, chills, cold extremities, withdrawal syndrome; very rarely - hypothermia.
From the laboratory parameters:
often - increased CK activity, increased heart rate, in elderly patients with dementia - increased body temperature, in children - increased body weight, increased prolactin concentration; uncommon - increased ALT activity, ECG disturbance, increased number of eosinophils in the blood, increased AST activity, increased number of leukocytes in the blood, increased blood glucose levels, decreased hemoglobin concentration, decreased hematocrit, decreased body temperature, decreased blood pressure; very rarely - prolongation of the QT interval on the ECG.
Below are additionally listed the adverse reactions that are observed when using risperidone intramuscularly (the drug Rispolept Konsta).
Infections:
lower respiratory tract infections, gastroenteritis, subcutaneous abscess.
From the blood and lymphatic system:
neutropenia.
From the side of metabolism:
hyperglycemia, weight loss.
From the mental side:
depression, sleep disorders.
From the nervous system:
paresthesia, convulsions.
From the senses:
blepharospasm, vertigo.
From the cardiovascular system:
bradycardia, increased blood pressure.
From the digestive system:
toothache, tongue spasm, increased GGT activity.
Dermatological reactions:
eczema.
From the musculoskeletal system:
pain in the buttocks.
From the reproductive system:
delayed menstruation, delayed ejaculation, oligomenorrhea, discomfort in the mammary glands.
Other:
pain, gait disturbances, detection of glucose in the urine, increased activity of microsomal liver enzymes.
Experience of using rispolept in the treatment of childhood schizophrenia
The collection of conference materials can be purchased by calling and ordering it by phone.
Rostov State Medical University Rostov-on-Don, Russia
Rispolept (risperidone) is a drug belonging to a new class of antipsychotic compounds - benzisoxazole derivatives, developed by the pharmaceutical company JANSSEN (Denmark).
According to the manufacturer’s description, rispolept provides improvement in the productive symptoms of schizophrenia; the therapeutic effect of the drug covers affective (anxiety, fear, melancholy) and negative (blunted affect, social withdrawal, poverty of speech) symptoms of schizophrenia. It causes less suppression of motor activity and induces catalepsy to a lesser extent than classical antipsychotics, and reduces the tendency to extrapyramidal side effects, which was the reason for attempting to use this drug in pediatric psychiatric practice.
There is no information on the use of rispolept in children under 15 years of age.
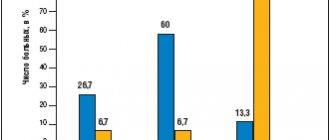
We used rispolept in 4 children (1 girl and 3 boys) aged from 6 to 13 years, suffering from various forms of childhood schizophrenia (malignant continuously progressive, continuous moderately progressive: paroxysmal-progressive close to malignant, recurrent), receiving long-term antipsychotic therapy traditional antipsychotics (haloperidol, triftazine, azaleptin) without any visible effect. In all cases, a significant proportion of catatonic symptoms of varying severity was found. Negative disorders were represented in three cases by symptoms of autism and in one case by the formation of a pseudo-oligophrenic defect. Rispolept was used as a basic antipsychotic, in one patient in combination with lithium carbonate, phenazepam. Rispolept was used in tablets of 1 and 2 mg. The initial dosage was 0.5 mg/day, followed by an increase of 0.5–1 mg/day, the maximum dosage was 6 mg/day. The duration of therapy ranged from 5 to 360 days. The low severity of side effects made it possible to use rispolept without correctors in all cases. In three children, rispolept was used on an outpatient basis.
It should be noted that the effect of the drug on productive symptoms in the treatment of paroxysmal forms (according to ICD-10 - episodic F20.xl-2) was less effective. On the third day of taking the drug at a dose of 3 mg per day, catatonic symptoms (motor and speech stereotypies, impulsive aggression) intensified, which necessitated discontinuation of the drug on the fifth day of use in one of the cases. The use of rispolept in a child with a catatonic attack and negative disorders as part of episodic schizophrenia, in the absence of an antipsychotic effect, was characterized by a decrease in the severity of autism symptoms; Contact, active use of speech, and initiative in communication have increased.
The use of rispolept in children with a continuously progressive type of schizophrenia in the acute phase of the disease contributed to the normalization of night sleep in the form of an increase in its duration and depth, relief of anxious affect and obsessive fears, and partial compensation of hebephrenic symptoms in one of the cases. In both children, the use of rispolept in therapy contributed to a significant reduction in negative disorders, namely autism. Thus, a 6-year-old patient with signs of the formation of a pseudo-oligophrenic defect, using rispolept in a daily dose of 1 mg, began to show interest in the environment in the form of contemplation, non-verbal forms of communication improved, and the range of interests expanded. In speech, along with the usual stereotypies, simple sentences of 2-3 words on everyday topics appeared. Syntonic emotional reactions began to arise, which made it possible to use rispolept for a long time as maintenance therapy in patients.
Attempts to increase the evening dose of rispolept above 0.5 mg resulted in difficulty falling asleep and frequent awakenings in three cases of long-term use of the drug.
Analysis of the effectiveness of rispolept in the treatment of childhood schizophrenia shows the feasibility of its use. This small experience of therapy allows us to draw some preliminary conclusions:
- Rispolept had a significant effect on negative symptoms, in particular on the symptoms of autism in both continuous and episodic schizophrenia.
- The absence of significant side effects made it possible to use rispolept long-term as maintenance therapy in an outpatient setting.
- Further assessment of the effectiveness of rispolept requires the development of standardized scales.
The collection of conference materials can be purchased by calling and ordering it by phone.
Source: Psychiatry at the turn of the millennium: Materials of the scientific and practical conference of psychiatrists in the South of Russia (with international and All-Russian participation) (December 21-23, 1999; Rostov-on-Don, Russia)
Rispolept Consta
Release form, composition and packaging
The powder for the preparation of a suspension for intramuscular administration of prolonged action is white or almost white, free from visible inclusions; The enclosed solvent is a clear, colorless, aqueous solution free of visible inclusions.
1 g risperidone (in the form of extended-release microgranules) 381 mg.
1 fl. risperidone (in the form of extended-release microgranules) 25 mg.
Excipients: polymer 7525 DLJN (poly-D,L-lactide-coglycolide), trace amounts of ethyl acetate, benzyl alcohol, anhydrous ethanol, and water are possible.
Solvent: polysorbate 20, sodium carmellose with a viscosity of 40 mPa.s, sodium hydrogen orthophosphate dihydrate, anhydrous citric acid, sodium chloride, sodium hydroxide, water for injection.
The powder for the preparation of a suspension for intramuscular administration of prolonged action is white or almost white, free from visible inclusions; The enclosed solvent is a clear, colorless, aqueous solution free of visible inclusions.
1 g risperidone (in the form of extended-release microgranules) 381 mg.
1 fl. risperidone (in the form of extended-release microgranules) 37.5 mg.
Excipients: polymer 7525 DLJN (poly-D,L-lactide-coglycolide), trace amounts of ethyl acetate, benzyl alcohol, anhydrous ethanol, and water are possible.
Solvent: polysorbate 20, sodium carmellose with a viscosity of 40 mPa.s, sodium hydrogen orthophosphate dihydrate, anhydrous citric acid, sodium chloride, sodium hydroxide, water for injection.
The powder for the preparation of a suspension for intramuscular administration of prolonged action is white or almost white, free from visible inclusions; The enclosed solvent is a clear, colorless, aqueous solution free of visible inclusions.
1 g risperidone (in the form of extended-release microgranules) 381 mg.
1 fl. risperidone (in the form of extended-release microgranules) 50 mg.
Excipients: polymer 7525 DLJN (poly-D,L-lactide-coglycolide), trace amounts of ethyl acetate, benzyl alcohol, anhydrous ethanol, and water are possible.
Solvent: polysorbate 20, sodium carmellose with a viscosity of 40 mPa.s, sodium hydrogen orthophosphate dihydrate, anhydrous citric acid, sodium chloride, sodium hydroxide, water for injection.
Clinical and pharmacological group: Antipsychotic drug (neuroleptic).
pharmachologic effect
Antipsychotic drug, benzisoxazole derivative. It is a selective monoaminergic antagonist. It has high affinity for serotonin 5-HT2 and dopamine D2 receptors. Binds to α1-adrenergic receptors and, to a lesser extent, to histamine H1 receptors and α2-adrenergic receptors. Has no affinity for cholinergic receptors. Risperidone is a powerful antagonist of dopamine D2 receptors, but compared to classical antipsychotics, it inhibits motor activity to a lesser extent and is less likely to cause catalepsy.
Due to its balanced central antagonism at serotonin and dopamine receptors, risperidone is less likely to cause extrapyramidal side effects and has a therapeutic effect on the negative and affective symptoms of schizophrenia.
Pharmacokinetics
Suction
Risperidone is completely absorbed from the Rispolept Konsta suspension. After intramuscular injections of Rispolept Konsta in doses of 25 mg or 50 mg once every 2 weeks, the average values of Cmin and Cmax of the active fraction are 9.9-19.2 ng/ml and 17.9-45.5 ng/ml, respectively. With this dosing regimen, the pharmacokinetics of risperidone is linear. In a long-term (12 months) study in patients who were administered Rispolept Consta in doses of 25 mg or 50 mg once every 2 weeks, no accumulation of risperidone was observed.
Due to the nature of the dosage form, after a single IM administration of Rispolept Consta, the release profile of risperidone consists of a small initial phase (<1% of the dose), followed by an interval of 3 weeks. After intramuscular injection, the main release of risperidone begins after 3 weeks, is maintained from 4 to 6 weeks and stops by 7 weeks. Thus, during the first 3 weeks after starting treatment with Rispolept Consta, the patient should take an additional antipsychotic drug.
The combination of the release profile of risperidone and the dosing regimen (im injection once every 2 weeks) ensures the maintenance of therapeutic concentrations of risperidone in plasma. Therapeutic concentrations last up to 4-6 weeks after the last injection of Rispolept Konsta.
Distribution
Risperidone is rapidly distributed in the body, Vd is 1-2 l/kg. In plasma, risperidone binds to albumin and alpha1-glycoprotein. Risperidone is 90% bound to plasma proteins, 9-hydroxyrisperidone is 77% bound.
Metabolism
Risperidone is metabolized in the liver with the participation of the CYP2D6 isoenzyme with the formation of 9-hydroxyrisperidone, which has a pharmacological effect similar to risperidone. Risperidone and 9-hydroxyrisperidone constitute the active antipsychotic fraction. Another route of metabolism for risperidone is N-dealkylation.
Removal
In fast metabolizers, the clearance of the active fraction and risperidone is 5.0 and 13.7 l/h, respectively, and in slow metabolizers it is 3.2 and 3.3 l/h, respectively.
The elimination phase is completed approximately 7-8 weeks after the last injection.
Indications
- treatment and prevention of exacerbations of schizophrenia and schizoaffective disorders.
Dosage regimen
Rispolept Konsta is administered once every 2 weeks deep intramuscularly, using the sterile needle attached to the syringe. Injections should be done alternately into the right and left buttocks. The drug cannot be administered intravenously!
For adults, Rispolept Konsta is administered at a dose of 25 mg IM once every 2 weeks. Some patients require higher doses - 37.5 mg or 50 mg. The maximum dose should not exceed 50 mg once every 2 weeks.
For 3 weeks after the first administration of Rispolept Konsta (i.e., before the drug begins to act), the patient must take an effective antipsychotic drug.
The dose of the drug can be increased no more often than once every 4 weeks. The effect of such an increase in dose should be expected no earlier than 3 weeks after the first injection of the increased dose.
For elderly patients, the recommended dose is 25 mg IM once every 2 weeks. For 3 weeks after the first administration of Rispolept Konsta (i.e., before the drug begins to act), the patient must take an effective antipsychotic drug.
Currently, there is no data on the use of Rispolept Konsta in patients with impaired liver or kidney function. If it is still necessary to use Rispolept Konsta in this category of patients, then in the first week it is recommended to take 500 mcg of risperidone 2 times a day in the form of tablets or oral solution. During the second week, the patient can take 1 mg 2 times a day or 2 mg 1 time a day. If the patient tolerates an oral dose of at least 2 mg well, then he can be administered 25 mg of Rispolept Konsta intramuscularly once every 2 weeks.
Rules for preparing the solution
Rispolept Konsta sustained release microgranules can only be suspended with the solvent contained in the supplied syringe; For intramuscular administration of the suspension, you must use the supplied needle.
1. Remove the Rispolept Konsta package from the refrigerator and allow it to warm to room temperature. Remove the colored plastic cap from the bottle containing the microgranules.
2. Open the syringe by breaking off the connection of the white cap, and remove the white cap along with the rubber tip inside it. Attach one of the Hypoint needles to the luer lock of the syringe by turning it slightly clockwise.
3. Remove the protective cap from the needle without turning it.
4. Pierce the rubber stopper of the bottle with a needle and inject the entire contents of the syringe into the bottle with microgranules.
5. Remove the syringe along with the needle from the rubber stopper closing the bottle.
6. Disconnect the needle from the syringe. The used needle should be thrown away.
7. Attach a second Hypoint needle to the syringe. At this stage, do not remove the protective cap from the needle!
8. Shake the bottle vigorously for 10 seconds. The mixing process can be considered complete when the suspension becomes homogeneous, thick, milky in color, and all the powder is suspended.
9. After preparation, the suspension should be used immediately, otherwise the suspension may separate.
10. Remove the protective cap from the Hypoint needle attached to the syringe without turning it.
11. Pierce the bottle cap with a needle.
12. Slowly suck the suspension into the syringe from the bottle, which is in a vertical position with the stopper up, to ensure complete removal of the suspension.
Rispolept tablets po 2mg bl N10x2 Janssen Pharmaceuticals N.V.
Schizophrenia. Adults. Rispolept can be prescribed once or twice a day. The initial dose of Rispolept is 2 mg per day. On the second day, the dose can be increased to 4 mg per day. From this point on, the dose can either be kept at the same level or individually adjusted if necessary. Usually the optimal dose is 4-6 mg per day. In some cases, a slower dose escalation and lower initial and maintenance doses may be justified. Doses higher than 10 mg per day have not been shown to be more effective than lower doses and may cause extrapyramidal symptoms. Due to the fact that the safety of doses above 16 mg per day has not been studied, doses above this level are not recommended. Elderly patients. An initial dose of 0.5 mg twice daily is recommended. The dosage can be individually increased by 0.5 mg twice daily to 1-2 mg twice daily. Children from 13 years old. The recommended initial dose is 0.5 mg once daily in the morning or evening. If necessary, the dosage can be increased after at least 24 hours by 0.5 - 1 mg per day to the recommended dose of 3 mg per day if well tolerated. Despite the effectiveness demonstrated in the treatment of schizophrenia in adolescents with doses of 1-6 mg per day, no additional effectiveness was observed at doses above 3 mg per day, and higher doses caused more side effects. Doses higher than 6 mg per day have not been studied. For patients who experience persistent drowsiness, it is recommended to take half the daily dose 2 times a day. Manic episodes associated with bipolar disorder. Adults. The recommended initial dose of the drug is 2 mg per day at a time. If necessary, this dose can be increased after at least 24 hours by 1 mg per day. For most patients, the optimal dose is 1-6 mg per day. Doses higher than 6 mg per day have not been studied in patients with manic episodes. As with any other symptomatic therapy, the advisability of continuing treatment with Rispolept should be regularly assessed and confirmed. Elderly patients. An initial dose of 0.5 mg twice daily is recommended. The dosage can be individually increased by 0.5 mg twice daily to 1-2 mg twice daily. Caution must be exercised due to limited experience with the drug in elderly patients. Children from 10 years old. The recommended initial dose is 0.5 mg once daily in the morning or evening. If necessary, the dosage can be increased after at least 24 hours by 0.5 - 1 mg per day to the recommended dose of 1-2.5 mg per day if well tolerated. Despite the effectiveness demonstrated in the treatment of manic episodes associated with bipolar disorder in children with doses of 0.5-6 mg per day, no additional effectiveness was observed at doses above 2.5 mg per day, and higher doses caused more side effects. Doses higher than 6 mg per day have not been studied. For patients who experience persistent drowsiness, it is recommended to take half the daily dose 2 times a day. Persistent aggression in patients with dementia due to Alzheimer's disease. A starting dose of 0.25 mg twice daily is recommended. If necessary, the dosage can be increased individually by 0.25 mg 2 times a day, no more than every other day. For most patients, the optimal dose is 0.5 mg twice daily. However, some patients are advised to take 1 mg 2 times a day. Rispolept should not be used for more than 6 weeks in patients with persistent aggression in patients with dementia due to Alzheimer's disease. During treatment, patients' condition should be assessed on a regular basis, as well as the need for continued therapy. Persistent aggression in the structure of conduct disorder. Children from 5 to 18 years old. Patients weighing 50 kg or more - the recommended initial dose of the drug is 0.5 mg once a day. If necessary, this dose can be increased by 0.5 mg per day, no more than every other day. For most patients, the optimal dose is 1 mg per day. However, for some patients, 0.5 mg per day is preferable, while some require an increase to 1.5 mg per day. Patients weighing less than 50 kg - the recommended initial dose of the drug is 0.25 mg once a day. If necessary, this dose can be increased by 0.25 mg per day, no more than every other day. For most patients, the optimal dose is 0.5 mg per day. However, for some patients, 0.25 mg per day is preferable, while some require an increase in dose to 0.75 mg per day. As with any symptomatic therapy, the appropriateness of continued treatment with Rispolep should be regularly assessed and confirmed. Use in children under 5 years of age is not recommended due to lack of data. Liver and kidney diseases. Patients with kidney disease have a reduced ability to eliminate the active antipsychotic fraction compared to other patients. In patients with liver disease, there is an increased concentration of the free fraction of risperidone in the blood plasma. The initial and maintenance dose, in accordance with the indications, should be reduced by 2 times; the dose increase in patients with liver and kidney diseases should be carried out more slowly. Rispolept should be prescribed with caution in this category of patients. Mode of application. Inside. Eating does not affect the absorption of the drug. If it is necessary to use doses less than 1.0 mg, it is recommended to use the drug Rispolept, an oral solution. It is recommended to discontinue taking the drug gradually. Acute withdrawal symptoms, including nausea, vomiting, sweating and insomnia, have been observed very rarely after abrupt cessation of high-dose antipsychotic medications. Transition from therapy with other antipsychotic drugs. When starting treatment with Rispolept, it is recommended to gradually discontinue previous therapy if clinically justified. Moreover, if patients are transferred from therapy with depot forms of antipsychotic drugs, then it is recommended to start therapy with Rispolept instead of the next scheduled injection. The need to continue current antiparkinsonian drug therapy should be periodically assessed.