Hiberix (HIBERIX) is a vaccine produced by GlaxoSmithKline Biologicals, intended for children from 6 weeks (1.5 months) to 5 years. According to the National Preventive Vaccination Calendar, children at risk should be vaccinated against hemophilus influenzae at the ages of 3, 4.5 and 6 months. Revaccination is carried out at the age of 1.5 years.
Since this vaccination is scheduled to be given simultaneously with immunization against whooping cough, diphtheria, tetanus and polio, as a rule, parents choose a complex option - Pentaxim or Infanrix Hexa, which include toxoids of all these diseases. Therefore, few people know about the existence of a separate vaccine against hemophilus influenzae infection. However, there are many cases when neither Pentaxim nor Infanrix is suitable for a child, but Hiberix is still needed. What are these cases?
Description of the drug
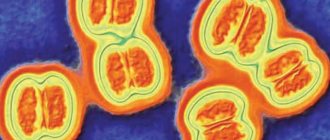
The Hiberix vaccine is intended for the prevention of purulent-septic diseases caused by Haemophilus influenzae type b (hemophilus influenzae), such as meningitis (inflammation of the meninges), sepsis (generalized bacterial infection), purulent arthritis (often accompanied by ostemyelitis), epiglotitis (inflammation of the epiglottis), pneumonia, inflammation of the subcutaneous tissue.
Hemophilus influenzae infection is transmitted by airborne droplets (and in children of the first year of life, contact transmission is also possible) and is extremely dangerous for children in the first years of life, since most often Hemophilus influenzae causes complications of a common acute respiratory viral infection, which can lead to serious life-threatening conditions (sepsis, meningitis, epiglotitis). Therefore, it is extremely important to form strong immunity in a child against Haemophilus influenzae type b.
The Hiberix vaccine contains purified Haemophilus influenzae type b capsular polysaccharide conjugated to tetanus toxoid.
The vaccine meets WHO requirements for the production of biological products and for Hib conjugate vaccines.
The Hiberix vaccine is used in more than 100 countries around the world. Vaccination against Hib infection has made it possible to virtually eliminate Hib meningitis and reduce the incidence of severe pneumonia by 20%. Vaccination has led to the almost complete disappearance of epiglottitis: in Finland, the incidence of epiglottitis has decreased from 7.6 to 0.0 per 100,000 children under 4 years of age. Similar data are available for other countries. The US Food and Drug Administration (FDA) has approved Hiberix for booster vaccination in children in the second year of life. The Hiberix vaccine was registered in Russia in 2004.
Hiberix or polyvaccine
So, should you choose a multi-vaccine - Pentaxim or Infanrix Hexa - or a stand-alone HIB vaccine? Polyvaccine is more convenient if:
- the child is vaccinated in strict accordance with the National Calendar, without medical withdrawals or postponements;
- he had not previously been vaccinated against whooping cough, tetanus and diphtheria;
- there is no strong reaction to the pertussis component (the most reactogenic component in the pertussis-diphtheria-tetanus vaccinations).
It is better to choose Hiberix if:
- the child was vaccinated with DPT, ADS-M or three-component Infanrix (NOT Hexa);
- The child, in principle, was not vaccinated against Haemophilus influenzae type b until 1.5 years old - after reaching this age he only needs one dose. Remember that after 4 years (the child’s fifth birthday), Hiberix should not be administered to him!
- The goal is to reduce the cost of vaccination (DPT+Hiberix on average will cost less than a polyvaccine).
Hiberix vaccine for the prevention of infection caused by Hemophilus Influenzae type b. Manufacturer: GlaxoSmithKline Biologicals (France), Packer SmithKline Beecham-Biomed LLC Russia hemophilus influenzae + Examination before vaccination - 1900 rubles.
MAKE AN APPOINTMENT PRICES
Compatibility with other vaccines
The Hiberix vaccine can be administered simultaneously with all drugs from the national schedule of preventive vaccinations on the same day, in different parts of the body, in different syringes, with the exception of the BCG vaccine.
The use of the Hiberix vaccine in combination with other vaccinations does not affect their immunogenicity (ability to develop immunity). Tolerability of vaccines does not deteriorate, and the number of adverse reactions does not increase. Administering several vaccines on the same day does not place an excessive burden on the immune system. Hiberix can be used to continue and complete a course of vaccination started with other vaccines against Haemophilus influenzae. All vaccines in the Russian national vaccination calendar are interchangeable.
Principles and purposes of vaccination
Haemophilus influenzae type b is a vaccine-preventable cause of serious illness (meningitis and pneumonia) and death among infants and young children.
Vaccination remains the only effective method of preventing Hib infection, which is becoming increasingly important in light of the increasing resistance of the pathogen to antibiotics. Unlike older children and adults, children under 5 years of age, due to insufficient development of the immune system, cannot independently, without vaccination, form adequate immunity to Hib.
By the end of 2013, the Hib vaccine had been introduced in 189 countries. Global coverage of three doses of this vaccine is estimated at 52%. Coverage levels vary widely across regions. In the Americas, coverage is estimated at 90%, while in the Western Pacific and South-East Asian regions it is only 18% and 27%, respectively.
Good tolerability allows you to combine and combine Hib vaccines with other vaccines in the vaccination schedule and, in particular, with DTP vaccines.
Conjugation of the main Hib antigen with a protein molecule made it possible to use the so-called booster effect. In other words, Hib vaccines have a revaccination effect, when repeated administration of the vaccine causes not just a linear increase in the concentration of antibodies, but an increase in their concentration in geometric progression. The peculiarity of the booster effect is that up to a certain stage, with each repeated administration, the increase in the number of antibodies also increases. This explains why the primary vaccination course consists of several vaccinations, and subsequent booster vaccinations are always carried out with just one dose of the vaccine. This is the basis for the basic scheme for the use of Hib vaccines, when 3 vaccinations with a single booster are given as part of the primary course.
Vaccination scheme
According to the National Calendar of Preventive Vaccinations of Russia, immunization with the Hiberix vaccine consists of 3 doses of the vaccine administered at 3-4.5-6 months of life; revaccination is carried out at 18 months. Vaccination against hemophilus influenzae is included in the National Calendar of Preventive Vaccinations of Russia by Order No. 51 of January 31, 2011. The Hiberix vaccine can be administered simultaneously with vaccination against polio, whooping cough, diphtheria, and tetanus.
The course of primary immunization depends on the age at which vaccination began. When vaccination begins at the age of 6 weeks to 6 months: 3 injections at intervals of 1-2 months. Revaccination is carried out once a year after the 3rd vaccination. Thus, the first injection is carried out, then the second injection 45 days after the first, then the third 45 days after the second. The immunization course is completed by revaccination, carried out one year after the third one is completed.
When starting vaccination between 6 and 12 months of age: 2 injections 1 month apart. Revaccination is carried out once at the age of 18 months. Thus, the first injection is carried out, then the second injection 30 days after the first. The immunization course is completed by revaccination, carried out one year after the second one is completed.
When starting vaccination between 1 and 5 years of age: single injection.
Antibodies with a protective titer of ≥0.15 μg/ml appear 1 month after the end of the vaccination course in 95-100% of children, and 1 month after revaccination - in 100% of children.
Prevention of purulent meningitis - Hib vaccine
15.Apr.2021
Children under 5 years of age are predominantly affected, and the disease is characterized by inflammatory processes of the respiratory system and central nervous system with the possible formation of purulent foci in various tissues and organs.
One of the common causes of pneumonia in children is Haemophilus influenzae. Such pneumonia in 70% of cases is complicated by pleurisy (inflammation of the membranes of the lungs). Penetration of Haemophilus influenzae into the blood sometimes causes sepsis, more often among children 6-12 months old. It flows hard, even lightning fast. There is a high risk of developing septic shock and death.
Epiglottitis mainly occurs in children from 2 to 5 years of age and is characterized by a severe course. Against the background of high temperature, severe pain in the throat, problems with swallowing, and breathing problems appear due to narrowing of the larynx in the area of the inflamed epiglottis. If help is not provided in time, complete blockage of the larynx in the area of inflammation is possible, leading to loss of consciousness and death.
In 160 countries around the world, including Russia, vaccinations against hemophilus influenzae are included in the national preventive vaccination calendars. Where vaccines are used to vaccinate the entire child population, in those countries Hib meningitis and epiglottitis have been practically eliminated, and the incidence of severe pneumonia has decreased by 25%. In Russia, vaccinations are carried out for all children belonging to risk groups. The vaccine contains capsular polysaccharide of Haemophilus influenzae type b. The Hib vaccine is also part of combination vaccines (Pentaxim, Infanrix-Hexa).
The most effective way to prevent the disease is to get vaccinated.
A number of scientific studies have shown that as a result of vaccination, a significant number of children who, due to their health status, belonged to the group of frequently ill people, stopped getting sick altogether or suffered from acute respiratory infections 1-2 times a year. Vaccination is carried out in 170 countries around the world, which has made it possible to practically eliminate meningitis. 3 Hib vaccines are registered in Russia: hemophilus influenzae type b conjugate dry vaccine (Russia), ACT-HIB (France), the Hib component is also contained in the Pentaxim vaccine (DPT+IPV+HIB). The ACT-HIB vaccine guarantees high immunogenicity after an initial series of three vaccinations. Vaccinations are carried out starting from 3 months of age three times along with DPT, HBV and IPV with revaccination 12 months after the 3rd vaccination.
The effectiveness of vaccination is 95-100%. The protective effect lasts for at least 4 years.
In 2022, 991 children were vaccinated against hemophilus influenzae at the Nyagan children's clinic. In three months of 2022, 50 children received Hib protection against hemophilus influenzae infection. Currently, the Nyagan Children's Clinic has the multicomponent Pentaxim vaccine, which is not inferior in its protective properties to foreign analogues. The monovaccine against hemophilus influenzae is temporarily unavailable, so the need for vaccination is determined by the local pediatrician.
REMEMBER! VACCINATION IS THE BEST PROTECTION OF THE BODY AGAINST INFECTIONS!
Composition, release form and analogues
Act Hib is available in the form of a lyophilisate for the preparation of a solution for subcutaneous and intramuscular injections along with a solvent. 1 dose of vaccine contains:
- 10 mcg of Haemophilus influenzae type b polysaccharide and 18-30 mcg of conjugated tetanus protein (active ingredients);
- 0.6 mg trometamol, 42.5 mg sucrose (excipients);
0.5 ml of solvent (sodium chloride solution 0.4%) contains 2 mg of sodium chloride and up to 0.5 ml of water for injection.
Vaccine Act Hib is a white homogeneous lyophilisate, and the solvent is produced in the form of a colorless transparent liquid. One cell package contains a bottle with 1 dose of vaccine and 0.5 ml of solvent in a syringe with a fixed needle. In cases where the needle is not attached to the syringe, 2 separate sterile needles are included in the package.
The main analogue of the Act Hib vaccine is Hiberix, produced in Belgium.
Reviews about the effectiveness of vaccination
There are a small number of reviews about the Act-HIB vaccine collected online, but we found some of them and presented them in our article:
- Olga, 34 years old . My son went to kindergarten and started getting sick very often. The doctor recommended vaccinating the child against hemophilus influenzae infections with the Act-HIB vaccine. My son tolerated the vaccination well. Only in the evening the temperature rose slightly (up to 37.3). But in the morning he was already like a cucumber. Since then, my son hasn’t stopped getting sick at all, but all sorts of ARVIs have begun to happen much less frequently for us. Therefore, I am very pleased;
- Maria, 45 years old. The doctor suggested vaccinating my granddaughter with the Act-HIB vaccine because she often gets sick. But we refused because it only protects against one type of meningitis. That is, it turns out that if the causative agent is not Hemophilus influenzae, then there will be no point in vaccination. Together with another doctor, we will try to choose a vaccine with a more extensive effect in order to have protection against a larger number of diverse infections, and not from one type of pathogen.
Indications for use
The use of the vaccine is indicated for:
- babies from six months to five years of age;
- people over 55 years of age;
- pupils of preschool educational institutions, orphanages;
- children from large families;
- patients with chronic diseases, HIV;
- patients after removal of the spleen (splenectomy);
- persons suffering from hematological diseases (lymphogranulomatosis, hereditary sickle cell anemia).
It is recommended to vaccinate adults with chronic diseases of the respiratory system, heart and endocrine system.
Contraindications
Contraindications to vaccination with the drug Act Hib are:
- Acute course of diseases. Vaccination is allowed no earlier than 2-4 weeks after complete recovery;
- Mild forms of respiratory and intestinal infections. Vaccination can be carried out after the temperature has normalized;
- Chronic diseases in the acute stage;
- Having an allergy to the components included in the vaccine, especially to tetanus toxoid.
Also, according to reviews, the Hib Act is not prescribed in cases of an allergic reaction to the previous administration of the medication.
Vaccine effectiveness
Current Hib vaccines are very effective. The incidence of all forms of infection in developed countries where routine immunization is carried out has decreased by 85-98%. This can be achieved both through individual protection of the vaccinated and through the effect of collective protection, which is explained by the interruption of the chain of transmission of the bacterium by the immunity of the vaccinated. In one of the Russian studies conducted in closed children's groups of the Moscow region, vaccination over the course of a year made it possible to reduce the level of carriage of Haemophilus influenzae from 41% to 3%, reducing the incidence of all pneumotropic diseases (ARI, bronchitis, pneumonia, etc.) several times.
The effectiveness of vaccination today is estimated at 95–100%. Numerous trials of polysaccharide vaccines have been conducted in Europe and North America. In particular, a clinical trial in the UK (1991-1993) showed an 87% reduction in the incidence of haemophilus influenzae meningitis. In Holland, during a similar study, a complete absence of cases of meningitis of hemophilic etiology was recorded within 2 years after the start of immunization.
What is the danger of hemophilus influenzae infection?
Haemophilus influenzae infection is caused by a bacterium called Haemophilus influenzae (Afanasyev-Pfeiffer bacillus). There are only six known types of Haemophilus influenzae. The most dangerous disease in terms of severity and complications is the disease caused by Haemophilus influenzae type b. Up to 90% of adults and about 40% of children are carriers of this infection. This fact is not surprising, because Hib is a conditional pathogen and its presence in the body in a certain amount is considered normal. It is especially common in children's groups. In 5% of carriers of hemophilus influenzae infection, type b bacillus is detected.
The infection is transmitted by airborne droplets. That is, the risk of infection is very high. In kindergartens, it is transmitted not only through the air, but also through toys, dishes, towels and other common items. There are two possible outcomes when bacteria enter the body. They depend on the number of sticks hit. With significant contamination, a disease occurs, with small contamination, carriage. Neither is a favorable option. If you are a carrier, there are no clinical manifestations, but as soon as your immunity weakens, the bacteria begins to multiply and a disease occurs.
Children aged 6 months to 5 years are most susceptible to hemophilus influenzae infection, but the period from six months to a year is considered the most dangerous in terms of the development of complications.
- Meningitis can lead to organic brain damage or even death. Up to 15% of purulent meningitis caused by CHIB result in death.
- Epiglottitis is dangerous due to asphyxia (suffocation).
- Pneumonia is characterized by severity and a large number of deaths. Haemophilus influenzae pneumonia is in second place in frequency among the children's population.
- Sepsis can be a complication of any disease.
- Bronchitis is a less dangerous complication than pneumonia in terms of consequences, but there is a high probability of the process becoming chronic.
In addition to the above complications, CHIB can cause acute respiratory infections, otitis media, and arthritis. The danger also lies in the fact that the initial manifestations of the disease are often absent, that is, it proceeds secretly. And clinical symptoms appear when complications occur. Treatment of Haemophilus influenzae infection is quite difficult due to the high resistance of Hib bacillus strains to antibiotics. That is why the issue of preventing the very fact of infection through vaccination is so urgent.
Side effects Act HIB
Most often, the act of Hib, according to reviews, causes local reactions, which manifest themselves in the form of erythema, soreness, inflammation, induration or swelling at the site of drug administration.
Also, according to reviews, the Hib Act can cause irritability, fever, prolonged crying, and vomiting in children.
In extremely rare cases, the temperature rises to 39 degrees, and febrile or afebrile seizures, rash, hypersensitivity reactions, urticaria and itching may also occur.
Side effects and complications
Act-HIB vaccination is usually well tolerated by patients. In some cases, there may be an increase in temperature up to 37.5 C, thickening, redness or itching of the skin at the injection site, nervousness or drowsiness.
But the listed deviations are not among the dangerous pathologies and do not always occur. They usually go away within 1 or 2 days.
In some cases, significant complications may develop: fever up to 39 C or more, headaches and other serious manifestations.
If symptoms continue to worsen, you should urgently seek help from a doctor.