"I have seen cases
when a person felt good at breakfast,
and by lunchtime he was already dead!
Dr Clayton Golledge, microbiologist, infectious disease specialist, USA.
Meningococcal infection is an acute infectious disease caused by the bacterium Neisseria meningitidis. The severity of meningococcal infection ranges from nasopharyngitis to fulminant sepsis, leading to death within a few hours.
In Russia, the incidence averages 5 per 100 thousand population per year, which is a fairly high figure. The highest prevalence of meningococcal infection in the world occurs in Central Africa, China, and South America (the so-called “meningitis belt”), where large epidemics of this disease regularly occur. Outbreaks of infection occur mainly in conditions of unsanitary conditions and crowded populations.
Meningococcal infection is characterized by seasonality - the incidence is highest in winter and early spring, because The immune system during this period is weakened by the entry into the body of a large number of viruses, which are also activated at this time of year - ARVI, influenza, etc. In addition, hypothermia is an important trigger for the development of meningococcal infection.
The only carrier of the bacterium Neisseria meningitidis is humans.
The infection spreads through airborne droplets and through direct contact with a patient or carrier. The incubation period averages 3-4 days, but can vary from 2 to 10 days. In the fulminant form of the disease, symptoms develop within a few hours from the moment the meningococcal infection enters the body.
The most common target for menigococcal infection is children under 5 years of age. The immune system of children at this age is not fully formed; In addition, children tend to touch their mouths with unwashed hands and various objects; they still poorly observe the rules of general hygiene, such as covering their mouths when coughing and sneezing, and regularly washing their hands. In addition, the spread of infection is facilitated by preschool institutions, where children closely interact with each other while playing and eating.
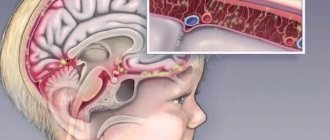
The mildest form of the disease is meningococcal nasopharyngitis, which symptomatically occurs as an uncomplicated acute respiratory viral infection, and therefore is often not diagnosed. At this stage, the disease may end, after which the infection becomes asymptomatic carriage, which occurs in 8-25% of patients. However, bacteria often enter the bloodstream and cause meningococcemia (or meningococcal sepsis). In this case, bacteria rapidly multiply in the blood and cause disruption of the blood coagulation system, which leads to hemorrhages in the skin and internal organs, and often ends in death. Meningococcal sepsis can be complicated by meningitis. Meningitis is an inflammation of the meninges that cover the brain and spinal cord. Meningitis is not only meningococcal - other bacteria (pneumococcus, staphylococcus, Haemophilus influenzae type B) can cause inflammation, and viral and fungal forms of meningitis also occur. Meningococcal infection has an increased tendency to affect the meninges.
Manifestations of meningococcal infection are insidious and deceptive. The first symptoms are often nonspecific; making a correct diagnosis at the initial signs of the disease can be extremely difficult. However, when a detailed picture of the disease appears, the patient often cannot be saved. There are three forms of meningococcal infection, each of which can occur independently, or have a sequential development - from nasopharyngitis to bacteremia (sepsis) and meningitis.
***
About 1 in 10 people who contract meningitis die, and up to a quarter are left with lifelong complications, including amputations and deafness.
***
Symptoms characteristic of menigococcal nasopharyngitis (similar to the symptoms of ARVI):
- Increase in body temperature to febrile levels (on average up to 38-38.5ºС)
- Phenomena of rhinitis
- A sore throat
- Headache
- Pale skin
- General weakness.
Among the above symptoms, it is extremely important not to miss a sharp deterioration in the condition, which usually develops in the shortest possible time.
Symptoms characteristic of meningococcal meningitis (50%):
- Fever that does not respond well to antipyretics and headache (flu-like symptoms)
- Stiffness of the neck (neck) muscles
- Nausea, vomiting
- Photophobia
- Impaired consciousness, confusion and disorientation
- Cramps.
Symptoms characteristic of bacteremia (sepsis), including meningococcemia (37.5%):
- Fever
- Petechial and purpuric rash (usually begins on the lower extremities)
- Hypotension
- Shock
- Multiple organ failure
- Death can occur within the first 24 hours from the onset of the first symptoms.
About 10% of people with meningococcal infection die, and 20% experience disabling complications. The basis of effective treatment is early diagnosis of the disease; prevention also plays an important role, in particular, vaccination against meningococcal infection.
According to WHO recommendations, one of the recommended approaches to the prevention of meningococcal infection is primary mass vaccination of all children and adolescents aged 9 months to 18 years, followed by inclusion of the vaccine in the routine childhood immunization program. In countries with lower incidence (<2 cases/100 thousand people per year), vaccination against meningococcal disease is recommended only in certain risk groups:
- children and adolescents in closed institutions, i.e. boarding schools, military camps;
- bacteriology laboratory workers at high risk of exposure to meningococci;
- Travelers to highly endemic regions of the world should be vaccinated against serogroups common in those regions.
At Children's Medical, you can protect your child from a dangerous disease with Menactra.
Manufacturer: Sanofi Pasteur, France.
Compatibility with other vaccines
Menactra was administered concomitantly with a polysaccharide typhoid vaccine and with an adsorbed tetanus and diphtheria toxoid vaccine for use in adults (Td) in persons aged 18–55 years and 11–17 years, respectively. The BCG vaccine should not be used simultaneously with the Menactra vaccine. Vaccines must always be administered to different parts of the body, using separate syringes for each of them.
Administering several vaccines on the same day does not place an excessive burden on the immune system. All vaccines in the Russian national vaccination calendar are interchangeable.
Post-vaccination reactions
Vaccines against meningococcal disease are well tolerated. In 25% of vaccinated people, a post-vaccination local reaction is possible in the form of soreness and redness of the skin at the injection site. Sometimes there is a slight increase in temperature, which normalizes after 24-36 hours. These vaccines are not required for routine immunization in our country, but you need to know about them, especially for those parents whose child is at high risk of developing meningococcal infection, or those who are planning a vacation in countries with unfavorable conditions for the spread of this infection.
Personal application experience
At the Sanare clinic, patients (children) aged 9 months and older were vaccinated with Menactra. The vaccine was well tolerated. There were no complaints in the post-vaccination period. (All patients at the clinic were called and interviewed by a nurse the next day).
The first to be vaccinated with the drug "Menactra", after its arrival at the clinic, were pediatricians, clinic staff, as well as their children (aged from 2 to 11 years). The drug was also well tolerated.
How great is the risk of getting sick?
Approximately 10-20% of people are carriers of meningoccal infection. Not all of them are sick - the carrier himself may be healthy. The bacteria live in the nasopharynx and are transmitted by airborne droplets. The sick person is contagious for about 3 weeks, of which 1 week is the incubation period, when the disease does not manifest itself in any way. You cannot get infected from animals or objects.
“We are riding the wave of a rise in meningococcal meningitis.”
The infectiousness of this infection is quite low. However, the incidence of meningococcal disease has a wave-like nature, and 2022 appears to have seen a surge in incidence. For example, V.S. Kovalev, a pediatrician at the Children's Research and Clinical Center for Infectious Diseases of the FMBA in St. Petersburg, in an interview given in February 2022 to the website miloserdie.ru, notes that such rises occur approximately once every 20-25 years, and now Russia is on the rise.
“A large number of people in Russia have already fallen ill with meningitis”
The Business Information Agency of Khakassia cites data from Rospotrebnadzor, according to which the epidemiological threshold for meningococcal infection was exceeded back in March 2022:
According to Rospotrebnadzor, in the first six months of this year, 549 Russian residents fell ill with meningococcal infection. This is 23% more than in the same period last year.
How is vaccination carried out?
Vaccination is carried out in a vaccination room, in compliance with all sanitary requirements. All drugs are certified. A certificate for the drug is provided upon request.
Without reminders, before vaccination, the medical worker must show the drug and the expiration date of the vaccine.
Only sterile and disposable instruments are used. The vaccination must be carried out using disposable medical gloves.
On the day of vaccination, the child is examined by a pediatrician and the temperature is measured. In the absence of contraindications, vaccination is carried out. Information about the vaccination performed is entered into the card, vaccination certificate, and detailed recommendations for caring for the child in the post-vaccination period are given.
Before vaccination, the doctor will answer all your questions. Be sure to bring information about previous vaccinations to your appointment!
Please note that vaccination of a child, Mantoux test, Diaskintest can only be carried out in the presence of parents or legal representatives of the child (guardians), or if the accompanying person has a NOTARIZED power of attorney to carry out the manipulation (indicating the drug planned for administration) . Otherwise, vaccination will be denied. We comply with the laws of the Russian Federation.
Only here!
What is meningococcal infection?
Meningococci are the bacteria Neisseria meningitidis that cause meningococcal disease. Contrary to popular belief, meningococcal disease is not the same as meningitis, although both are extremely dangerous diseases. Meningitis, or inflammation of the meninges, can be caused by meningococci, pneumococci, or even Haemophilus influenzae. Unfortunately, it is meningococcal meningitis that causes the greatest number of deaths. In the so-called “meningitis belt” of West Africa, it accounts for 80% of all meningitis cases.
But meningococcal infection does not necessarily manifest itself as inflammation of the meninges. Bacteria can cause mild forms of infection, for example, nasopharyngitis (this is a standard sore throat and stuffy nose, as with ARVI), and very severe ones, for example, meningococcemia (sepsis, that is, blood poisoning). It happens that the disease develops at lightning speed and cannot be stopped. It is most dangerous for children.
What complications may there be?
As mentioned above, if meningococcal infection is detected late, there is a high probability of death. However, even if treatment was prescribed on time, often the disease does not go away harmlessly. The consequences can lead to a variety of complications, ranging from hearing loss, vision and speech disorders, to amputation of limbs, paralysis, epilepsy and hydrocephalus. And here is another video (video by our partners - Sanofi Pasteur) with a girl who, at the age of 5, suffered a meningococcal infection and was left deaf for the rest of her life:
The nature of the inflammatory process in meningitis
Meningitis is classified according to several criteria. According to the nature of inflammation, they are purulent and serous.
Purulent
Pathogens: streptococci, staphylococci, pneumococci and others. Meningococcus enters the brain through the bloodstream. This is a dangerous type of disease, as the risk of death is high. When the first symptoms appear, urgent treatment with antibiotics is necessary. Features include the release of pus and the development of cell necrosis.
Serous
Occurs in epidemic outbreaks. The peculiarity is the release of serous exudate. It consists of a small number of leukocytes. How a secondary infection develops after influenza, mumps, and fungal diseases. The prognosis is favorable.
DESCRIPTION OF THE MEDICINE
Appearance: Colorless transparent or slightly cloudy solution.
Pharmacotherapeutic group: MIBP vaccine.
ATX code: J07AH08.
The Menaktra vaccine is a solution of purified capsule polysaccharides of Neisseria meningitidis groups A, C, Y and W-135 individually conjugated to a carrier protein (purified Carynebacterium diphtheriae toxoid).
Immunological properties
The causative agent of meningococcal infection, including meningitis and septicemia, is the bacterium N. meningitidis. a number of serotypes of the pathogen have been identified. The use of the Menactra vaccine causes the production of specific antibodies against capsular polysaccharides of the serogroups of the causative agent of meningococcal infection, included in the vaccine C, C, Y and W-135), which have bactericidal activity.
Immunological effectiveness
Clinical efficacy studies have not been conducted because serum bactericidal antibodies (SBA) are considered to be an indicator of the effectiveness of meningococcal vaccines.
The immunological properties of the Menactra vaccine were studied in 3 clinical studies in children aged 9-18 months, in 4 clinical studies in children aged 2-10 years and in 6 clinical studies in a group of people aged 11-55 years. Immunogenicity was assessed by the level of these functional antibodies determined using a serum bactericidal assay using rabbit complement (BAC).
The primary immunological profile was studied in clinical studies on participants from 2 to 10 years of age. The immune response was assessed immediately before a single administration of the Menactra vaccine and 28 days later. study participants observed a significant increase in geometric mean titers (GMT) of bactericidal antibodies. In all sero groups, 86-100 participants with initially undetectable SBA titers "1: seroconversion was noted, defined as a 4-fold (or more) increase in antibody titers 28 days after vaccination.
The immune response was assessed immediately before a single administration of the Menactra vaccine and 28 days later. study participants observed a significant increase in geometric mean titers (GMT) of bactericidal antibodies. In all sero groups, 86-100 participants with initially undetectable SBA titers "1: seroconversion was noted, defined as a 4-fold (or more) increase in antibody titers 28 days after vaccination.
RELEASE FORM
Appearance: Solution for intramuscular administration 0.5 ml/dose.
1 dose (0.5 ml) of the drug in bottles made of transparent borosilicate glass (type 1) with a capacity of 3 ml, which are sealed with a stopper made from a mixture of chlorobutyl (latex-free) and synthetic polyisoprene, and rolled up with an aluminum cap equipped with a tear-off plastic lid "flip-off" type.
1 or 5 bottles along with instructions for medical use in a cardboard pack.
When is it undesirable to get vaccinated?
Contraindications and conditions requiring precautionary measures during vaccination are: severe allergic reaction (for example, anaphylaxis) after a previous dose of the vaccine or to its components. Tell the doctor who is giving you or your child the meningococcal vaccine if:
- you or your child have had a life-threatening allergic reaction;
- you had a severe allergic reaction after a previous dose of meningococcal vaccine - a second dose of this vaccine is prohibited;
- you are pregnant or breastfeeding;
- moderate to severe illness with or without fever (vaccination delayed until recovery if possible).
Conjugate vaccines may be given to pregnant women who are at increased risk of contracting meningococcal serogroups A, C, W, or Y. It is recommended that vaccination against meningococcal serogroup B be delayed during pregnancy. The exception is for women at increased risk of disease caused by serogroup B pathogens, when the benefits of vaccination are expected to outweigh the potential risks.
COMPOUND
One dose (0.5 ml) contains:
Active substances:
Monovalent meningococcal conjugates (polysaccharide + carrier protein):
- Polysaccharide serogroup A* - 4 µg;
- Polysaccharide serogroup C* - 4 mcg;
- Polysaccharide serogroup Y* - 4 mcg;
- Polysaccharide of serogroup W-135* - 4 mcg.
* - each polysaccharide is conjugated with diphtheria toxoid. The protein content of diphtheria toxoid in the vaccination dose is about 48 µg.
Excipients:
- Sodium chloride 4.35 mg;
- Sodium hydrogen phosphate 0.348 mg;
- Sodium dihydrogen phosphate monohydrate 0.352 mg;
- Water for injection - up to 0.5 ml.
SIDE EFFECTS
The nature and frequency of side effects identified in studies varied depending on the age of those vaccinated.
Adverse reactions in children from 9 to 18 months
- Loss of appetite;
- Drowsiness;
- Vomit;
- Diarrhea;
- Rash;
- Hives;
- Arthralgia;
- Soreness and hardness at the injection site;
- Irritability, redness at the injection site, swelling at the injection site, fever.
Adverse reactions in children from 2 to 10 years of age
- Decreased appetite;
- Drowsiness;
- Diarrhea;
- Vomit;
- Rash, urticaria;
- Arthralgia;
- Soreness and hardness at the injection site;
- Irritability, redness at the injection site, swelling at the injection site, fever.
Adverse reactions in adolescents from 11 to 18 years of age and adults from 18 years of age
- Decreased appetite;
- Headache;
- Diarrhea;
- Vomit;
- Rash;
- Arthralgia;
- Pain, hardness, redness and swelling at the injection site, increased fatigue, general malaise;
- Chills, fever.
Symptoms of meningitis
Children and adolescents are more susceptible to developing pathology. The most common symptoms of meningitis are:
- stiffness and pain in the neck muscles, especially when tilting the head;
- hyperthermia;
- headache;
- nausea, vomiting;
- sleep cycle disturbance;
- irritability, tearfulness;
- A rash and cough may occur.