ARVI, which includes influenza, are the most common infections. More than 30 million cases of infection are registered in Russia every year. Moreover, the incidence of ARVI varies from year to year. But even in non-epidemic years, the recorded incidence of influenza infections and colds is many times higher than the incidence of other infectious diseases. The highest number of infections is usually observed between September and April, with the peak incidence occurring in February and March. In summer, colds and flu do not disappear anywhere, they just occur about 3-5 times less often than in winter.
- Mechanism of action of antiviral drugs
- In what cases is it used for ARVI?
- The situation in global practice
- Discovery and methods of obtaining interferon
- Selection of antiviral agents
- Use for prevention
The particularly important position of ARVI among other viral diseases is determined by the lack of a radical solution to the problem of their prevention using any one universal method. Scientists have invented a vaccine, but it is used only against influenza infections and is powerless against colds. When making vaccines, it is also impossible to take into account possible mutations of viruses.
Acute respiratory viral infections (ARVI) are diseases that are caused by certain viruses. This disease causes damage to various parts of the respiratory tract and general intoxication.i Viruses are non-cellular life forms that can reproduce only inside the cells of highly developed creatures. Based on their composition, viruses are divided into two large groups - simple (for example, polio viruses, hepatitis A) and complex (measles, herpes, influenza viruses). In total, experts know more than 300 types of viruses that cause ARVI. Quite often, bacteria join viruses, which causes the development of various complications.
The intensity, frequency of occurrence and dominance of various respiratory viruses depend on the time of year and climate. In some cases, acute respiratory viral infections may have a combined etiology, when several pathogens are involved in the development of an infectious disease.
When viewed under a microscope, the influenza virus looks like a chestnut fruit that is encased in a spiked shell. And these so-called “spikes” consist of proteins on which the virus’s mutability directly depends. This characteristic distinguishes it from other known viruses. And even the most minor changes in the structure of these “spikes” lead to the emergence of new strains that have not yet been studied by humans. Such unpredictability makes influenza infection one of the most dangerous for the human population. In the Russian Federation, the annual economic loss from ARVI is estimated at about 40 billion rubles.ii
The difficulty lies in the similarity of the clinical picture of many ARVI viruses. For example, a differential diagnosis needs to be made between influenza and other acute respiratory infections, including the COVID-19 virus that led to the 2020 pandemic.iii
Antiviral drugs for influenza: main mechanisms of action
By introducing themselves into the cells of the respiratory tract, viruses cause damage to structures that perform barrier functions. Antiviral for flu and colds blocks some stages of viral infection:
- At the stage of infection and penetration into the cell, the drug blocks viral activity. The medicine can slow down or prevent the process of bringing viral particles closer to the cell membrane.
- At the second stage, if the virus does become close to the cell, the viral genome is copied. By using anti-viral drugs, the replication of viral DNA and RNA is blocked.
- During the synthesis of viral proteins and at all stages of virus assembly, various drugs are used: interferon-based, protease inhibitors and structural protein inhibitors.
- When the virus comes out and tries to invade other cells, it can be defeated with drugs based on neuraminidase inhibitors and antibodies.
The incubation period of the influenza virus in the body is on average three days. In order to choose the right treatment and antiviral for influenza and ARVI with minimal side effects, it is important not to confuse these diseases.iv
| Clinical manifestations | ARVI | Flu |
| Onset of the disease | Discomfort increases gradually | Acute and sudden, a person can sometimes name the exact time when he felt that he had become infected |
| Fever | The thermometer readings rarely reach 38 0C | Within a few hours, the readings on the thermometer can reach 39 0C, 40 0C and higher. Fever bothers you for several days |
| Manifestations of intoxication | Intoxication is mild, the patient feels relatively well | There are chills, a severe headache, “shooting” in the temples and forehead, eyes hurt from bright light, aching muscles and joints |
| Nasal discharge | Almost always found | There is no severe runny nose, but I am worried about slight congestion, which appears after a few days. |
| Sore throat, hyperemia | Common with colds | Identified as the disease progresses, the doctor notices redness of the pharynx |
| Cough | With a cold, a cough is bothersome from the first days of infection; the patient has difficulty clearing his throat | There is a cough, the patient feels pain in the chest, which appears due to damage to the trachea |
| Sneezing | Occurs frequently | Rarely observed |
| Red eye syndrome | Observed when bacteria attach | Diagnosed frequently |
| Painful state of fatigue, lethargy | After the illness it is almost not expressed | After the end of the period of illness, the patient experiences irritability, insomnia, and weakness during the day for several weeks. I often have a headache. |
Features of infection and symptoms
Most often, the development of acute respiratory infections occurs against the background of infection with viruses or bacteria. The infection is transmitted by airborne droplets or by contact when in public places or when personal hygiene rules are not observed. Once on the mucous membranes of the respiratory system, pathogens multiply and cause unpleasant symptoms against a background of general malaise.
Pronounced signs of acute respiratory infections usually appear a couple of days after infection. This:
- A sore throat.
- Sneezing.
- Headache.
- Loss of appetite.
- Runny or stuffy nose.
Treatment should begin when the first symptoms appear. ARI at the initial stage of development can be successfully treated with modern medications. Otherwise, the intensity of the symptoms will increase, in addition, the body temperature will rise, fever will occur, and the lymph nodes will enlarge, which will lead to a deterioration in the general condition. Against this background, there are risks of developing complications and the need for treatment in a hospital setting.
When should you use an antiviral drug for influenza and acute respiratory viral infections, and do doctors recommend this?
Many people, under the influence of certain media, are sure that there is no point in taking medications for ARVI. After all, as the old proverb says, a cold goes away in a week without treatment, and in seven days with treatment. This means that this disease can be survived without medication. However, unfortunately, statistics speak of disappointing facts. According to the World Health Organization, up to 650 thousand people die annually from respiratory diseases associated with seasonal influenza infection.v Not everyone knows that influenza infection and colds can negatively affect the heart. This reduces the average life expectancy by several years.vi After a severe course of ARVI, serious damage to the respiratory system, including pneumonia, is often diagnosed. Also, after acute respiratory viral infections, diseases of the blood vessels and the central nervous system are often detected.
Therefore, the main argument in favor of taking anti-viral medications is the need to reduce the high risks that accompany influenza infection. The second reason is due to the fact that timely and adequate treatment shortens the duration of the disease and weakens its symptoms. If you take a good flu antiviral when you develop symptoms of influenza infection and colds, you may experience a shorter period of runny nose, headaches, and fever.
Mechanisms of effectiveness of first-generation antihistamines for ARVI
Despite the known effectiveness of first generation antihistamines for ARVI, the mechanisms of their action remained poorly understood.
Individual symptoms of ARVI are caused by multiple, sometimes specific to different symptoms, inflammatory mechanisms. Sneezing was usually explained by the release of histamine from nasal mast cells and basophils, which occurs when these cells are activated during acute respiratory viral infection. As evidence, they cited the fact that intranasal administration of histamine (but not other mediators) to healthy people causes sneezing. It is also known that treatment with first generation antihistamines is highly effective in reducing sneezing during acute respiratory viral infections both under normal and experimental conditions. However, unlike allergic rhinitis, in ARVI, the level of histamine in nasal secretions is not increased, although the sensitivity of the nasal mucosa to histamine in ARVI increases.
Antihistamines of both the first and second generation are competitive histamine antagonists at the level of H1 receptors. In addition, unlike second-generation drugs, first-generation antihistamines exhibit competitive antagonism towards acetylcholine at the level of neuronal and neuromuscular muscarinic receptors, and also penetrate the blood-brain barrier. Limited studies have shown that second generation antihistamines are not able to reduce sneezing in ARVI.
These data raised the question for researchers about the mechanisms through which first-generation antihistamines (Suprastin and others) are able to reduce rhinorrhea, swelling of the nasal mucosa and sneezing during ARVI, and why this effect is not characteristic of second-generation drugs. Research into ARVI in natural conditions is associated with certain technical difficulties. Thus, it is difficult to recruit patients in the early stages of the disease, when the effectiveness of treatment can be most accurately assessed. Therefore, it would be useful to confirm the results of studies of antihistamines in acute respiratory viral infections conducted in natural conditions using an experimental rhinovirus infection that allows accurate assessment of sneezing. Such a study was conducted by PS Muether and JM Gwaltney, who studied the effects of loratadine, a second generation antihistamine, in experimental rhinovirus infection.
Materials and methods
The study included 66 adult volunteers whose antibody titres to type 16 rhinovirus did not exceed 2 units and who had not suffered from acute respiratory viral infection or other illness with fever in the last week. In addition, patients with any serious concomitant diseases, bronchial asthma, allergic rhinitis were excluded; who have recently taken (according to the characteristics of their pharmacokinetics) antihistamines, cold remedies and other drugs that may affect the results of the study.
Rhinovirus infection was caused by double (with a 20-minute break) intranasal administration of a standardized culture of type 16 rhinovirus. Nasal lavages for subsequent identification of the virus were obtained 8 days and immediately before infection (to exclude accidental infection with a “wild” strain of rhinovirus), as well as every morning before taking the drug. Neutralizing type-specific antibodies were determined in blood tests 7 days before inoculation and 2–3 weeks after it.
Patients rated symptoms of the disease (sneezing, nasal discharge, nasal congestion, sore throat, cough, headache, weakness, chills) over the previous day on a 5-point scale: 0 - no symptoms, 1 - mild, 2 - moderate, 3 – pronounced, 4 – very pronounced. Overall symptom severity was calculated as the sum of all symptom scores. Assessment of disease severity also included daily measurements of nasal secretions. Each patient recorded the frequency of sneezing and coughing in a diary. The presence and severity of side effects were assessed daily.
Patients were randomized in a double-blind manner to loratadine or placebo. Loratadine or placebo was prescribed from days 1 to 13 of the study, and virus inoculation was performed on day 8.
results
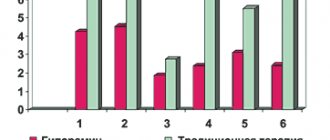
Of the 66 patients included in the study, 34 received loratadine and 32 received placebo. Four people in the loratadine group and one in the placebo group were infected with a wild strain of rhinovirus at the start of the study, so their data were not assessed. One person in the placebo group stopped taking it due to the onset of migraines on day 10. Thus, data from 60 people were assessed.
After inoculation, the virus was detected in the nasal secretions of 28 (93%) people in the loratadine group and 24 (80%) in the placebo group; an increase in type-specific antibodies was noted in 40% and 37%, respectively. The overall infection rates were 97% and 80% (differences not significant).
Mean viral titers did not differ between groups. According to the Jackson criterion, the disease developed in 23 (79%) of 29 infected people in the loratadine group and in 14 (58%) of 24 infected people in the placebo group (differences not significant).
The severity of sneezing did not differ between groups in the first 3 days and was slightly less in the placebo group on day 4. The severity of nasal congestion, sore throat, cough, and overall symptom severity also did not differ between groups. Headache and malaise were reduced with loratadine in the final days of the study. Rhinorrhea was less in the placebo group on days 2–3, but more on days 4–5. When objectively measuring the volume of nasal secretion, there was a trend toward greater volume in the loratadine group (the differences were not significant).
Side effects were noted in the placebo group: 2 cases of vomiting and 1 case of migraine.
Discussion
Thus, there were no differences between the loratadine and placebo groups in the incidence of rhinovirus infection and disease development, or in the severity of symptoms.
The results also showed no therapeutic effect of loratadine on sneezing. This confirms publications that show that second generation antihistamines are not able to reduce sneezing in ARVI. Why are first generation antihistamines effective against sneezing, but second generation drugs are not?
Rice. 1. Mechanisms of the sneezing reflex. N - nicotinic synapses, M - muscarinic synapses, ? — mediators are not installed.
First generation antihistamines block not only H1 receptors, but also muscarinic receptors, and also penetrate the blood-brain barrier. The last two properties are not inherent in second generation antihistamines.
Information about the neurological mechanisms of the sneeze reflex comes mainly from animal experiments. The reflex arc includes peripheral nerves and the medulla oblongata, and involves histamine H1 receptors, muscarinic and nicotinic receptors. In acute respiratory viral infections, the reflex is triggered by infectious damage to the cells of the mucous membrane. Involvement of mast cells and basophils with a subsequent release of histamine during ARVI is not observed, but stimulation of the free nerve endings of the ethmoidal branch of the trigeminal nerve by inflammatory mediators, such as bradykinin, occurs. The nerve impulse then travels along afferent fibers to the sensory nucleus of the trigeminal nerve and the adjacent sneezing center. Through the synapse, the impulse reaches the superior salivary nucleus of the facial nerve and, having passed another synapse, enters the sphenopalatine ganglion along the preganglionic branches. The excitation is then transmitted through postganglionic fibers by muscarinic synapses to the mucous glands and blood vessels. As a result, secretion and exudation stimulate the endings of the trigeminal nerve and the impulse is again sent to the sneezing center in the medulla oblongata. With sufficient signal strength, excitation is transmitted to the respiratory neurons of the reticular formation, and from them along the fibers of the vagus, phrenic and intercostal nerves through nicotinic synapses - to the respiratory muscles involved in the act of sneezing.
Histamine may potentially be involved in the sneezing process at several sites in the reflex arc, which may therefore be sites of application for antihistamines. The first of these is the nasal mucosa, where H1 receptors are present on the free nerve endings of the trigeminal nerve. The fact that the effect of antihistamines in ARVI is realized at the level of the mucous membrane is argued against by the normal levels of histamine in nasal secretions during ARVI, as well as the lack of effect from second generation antihistamines, which reach the mucous membrane and block H1 receptors in it. But since the sensitivity of the nasal mucosa to histamine during ARVI increases, this point of application of antihistamines during ARVI cannot be completely excluded.
The next point of application for first generation antihistamines is the medulla oblongata, where a number of synaptic switches of the sneezing reflex occur. H1- and muscarinic receptors are found in these zones. These nicotinic receptors may be targets for first-generation antihistamines that cross the blood-brain barrier. It should be taken into account that the mediators of the synapses of the medulla oblongata involved in the sneeze reflex have not yet been identified. The ineffectiveness of second generation antihistamines in acute respiratory viral infections confirms the possible important role of these nerve centers.
Parasympathetic stimulation of glandular secretion and vasodilation is mediated exclusively by muscarinic receptors. At this level, the application of anticholinergic activity inherent in first generation antihistamines is quite likely. Indeed, they reduce the volume of nasal secretion during ARVI. The second afferent impulse into the medulla oblongata is also caused by stimulation of the endings of the trigeminal nerve. Exudation from blood vessels triggers the kinin system. The resulting kinins stimulate nerve endings both on their own and by leading to the release of histamine from mast cells, which represents a new target for antihistamines. When excitation reaches the medulla oblongata, it can be suppressed by first generation antihistamines (as described above). Further, impulse transmission depends on nicotinic receptors and is not sensitive to antihistamines.
It can be concluded that the therapeutic effect of first generation antihistamines on sneezing may be largely due to the blockade of H1- and muscarinic receptors in the medulla oblongata. H1 receptors are also present in large numbers in the hypothalamus, where histamine, as a neurotransmitter, is involved in maintaining wakefulness and in a number of other functions. This fact may be associated with drowsiness caused by first generation antihistamines.
First generation antihistamines, like scopolamine (an anticholinergic drug that penetrates the blood-brain barrier), can reduce nausea in motion sickness (motion sickness). This once again suggests the important role of muscarinic receptors in the central nervous system.
Conclusion
Treatment of ARVI with first generation antihistamines (Suprastin, etc.), in contrast to second generation drugs, is highly effective in reducing symptoms such as rhinorrhea, swelling of the nasal mucosa and sneezing. Although information about the subtle neurotransmitter mechanisms of this phenomenon is still insufficient, it can be assumed that this occurs due to the activity of first-generation antihistamines in relation to H1-histamine and muscarinic receptors, as well as their ability to penetrate the blood-brain barrier.
Prepared by Ph.D. A.N. Nikolaev based on materials:
P. S. Muether, J. M. Gwaltney. Variant effect of first– and second–generation antihistamines as clues to their mechanism of action on the sneeze reflex in the common cold. // Clinical Infectious Diseases, 2001; 33:1483–8.
Antiviral drugs for influenza in global practice
According to the most conservative estimates, today the number of potential consumers of anti-virus drugs is hundreds of millions of people per year. At the same time, people have always tried to fight ARVI viruses, including in ancient times, when there were no diagnostic laboratories, humanity had not yet invented the microscope and did not know that the cause of their diseases were harmful viruses. However, as the ancient Roman physician and philosopher Claudius Galen said, the people were thirsty for medicine. And I received them. In ancient times, analogues of modern drugs - remedies in the form of tinctures and lotions - were widely and not always effectively used to treat viral diseases. The first effective antiviral drugs for colds and flu appeared only when scientists identified viruses and began serious work in the field of pharmacy.
Today, antiviral drugs are substances that have antiviral activity. Frequently used drugs for the treatment and prevention of acute respiratory viral infections and influenza include:
- Drugs of narrowly targeted action (act only on influenza);
- Broad-spectrum drugs (for example, interferon acts against more than 300 types of various acute respiratory viral infections and influenza);
- Symptomatic remedies (relieve symptoms of the disease, including fever, runny nose, aching joints, but do not act on the cause of the disease).
Antivirals and immunomodulators to enhance immune defense
One striking example is the antiviral drug umifenovir.
For the first time, encouraging clinical experience with its use was reported by Chinese doctors who published an article in The Lancet on the therapeutic strategy for treating COVID-19 in several clinics [2]. It talks about the use of umifenovir [Arbidol], approved for the treatment of influenza in China, for coronavirus pneumonia. The basis for this prescription was the results of in vitro studies demonstrating the inhibitory effect of umifenovir on SARS [3]. Let us remember that SARS is the closest relative of the coronavirus SARS-CoV-2, the causative agent of severe acute respiratory syndrome, which caused an epidemic in 2002. It is known that the genome of SARS-CoV-2 is 79.5% identical to the genetic code of SARS [4]. Read about the biology of coronavirus here.
The preventive capabilities of umifenovir are due to interferon-inducing activity, stimulation of cellular and humoral immunity. Among its indications is the prevention and treatment of influenza A and B and other acute respiratory viral infections in children from two years of age and adults.
Currently, umifenovir and two other antiviral drugs not registered in the Russian Federation - remdesivir and favipiravir - are undergoing clinical trials in patients with COVID-19. While remdesivir and favipiravir are new and insufficiently studied, umifenovir has quite a wealth of experience in clinical use. What's more, it is available over-the-counter and is generally well tolerated, so it can be recommended to consumers.
What can you offer?
Along with umifenovir for the prevention of acute respiratory viral infections, including COVID-19, other over-the-counter drugs can be recommended - immunomodulators and immunostimulants, for example, azoximer bromide in the form of tablets and suppositories (used in adults and children from three years of age for the treatment and prevention of acute and chronic respiratory diseases in the stage of exacerbation and remission); an antiviral drug that induces the production of interferons, kagocel (prevention and treatment of influenza and other acute respiratory viral infections in adults and children over three years of age), meglumine acridone acetate in tablet form (prevention and complex therapy of influenza and other acute respiratory viral infections in adults and children over four years of age), tilorone tablets 125 mg (prevention and complex therapy of influenza and ARVI in adults and children from seven years of age).
What should you tell your visitor about?
Drugs with antiviral and immunomodulatory properties help resist infection and the development of respiratory viral infections, increasing the immune response and preventing viral replication. And although there is no proven data on their effectiveness against the causative agent of the current pandemic, SARS-CoV-2, it is nevertheless appropriate to take drugs from this group.
History of the discovery of interferon and methods of its production
Interferon is a number of proteins with similar properties that are secreted by cells in response to the invasion of an infectious agent. Scientists first announced the discovery of interferon in the mid-20th century. Prior to this, through research it was discovered that when infected with one virus, the body cannot be infected with other viruses. It was found that infected cells are capable of producing a special protein, which became a kind of shield and antiviral protection. This phenomenon was called interference, and the protein was called interferon. Over time, this great discovery has gone far beyond the scope of virology and is now used in many areas of medicine and pharmacology.
In the USSR, the widespread use of IFN began in the late 1960s. To produce the drugs, leukocytes from placental blood were used, which were taken from postpartum women. In those years, human leukocyte IFN was successfully used during epidemics of influenza infection, which made it possible to reduce the incidence and reduce the symptoms of viral infection. Unfortunately, there are risks associated with the production of human leukocyte IFN. A drug obtained using donated blood is very difficult to perfectly purify, including from blood-transmitted diseases - hepatitis and HIV. Also, such drugs are quite expensive. Therefore, today donated blood is used very rarely for the production of medicines and only in cases where the expected benefits from their use outweigh the possible risks.
The development of genetic engineering and the development of recombinant IFN technology has made it possible to use drugs en masse, since their cost has noticeably decreased, and the absence of blood components in the composition has made it possible to level out the risks of contracting various infections. It is safe to say that with the invention of recombinant IFN, a new era in the use of interferons began. In particular, recombinant interferon alpha-2b is part of the antiviral drug VIFERON.
IFN has not only activity against viruses, but also antibacterial, antiproliferative (including antitumor), immunomodulatory and radioprotective activity.
Every year, researchers write a lot of articles and monographs about the positive effects of IFN on the body, which contain fundamental data on the structure, mechanisms of action and biological effect of interferons, and also provide proven results of the long-term use of IFN in medicine.
Good antiviral drugs for influenza: how to choose
A special group should include medications that help the body resist the invasion of foreign agents. Many anti-virus drugs have a complex effect. In modern medicine, drugs containing nucleoside derivatives, adamantane, deoxyuridine, synthetic amino acids, pyrophosphate analogues, substances of plant origin and many other drugs are widely used.
The attending physician should prescribe treatment and select antiviral drugs, taking into account the age and condition of the patient.
Antiviral drug VIFERON
One of the drugs that helps strengthen the immune system and has a wide spectrum of activity against viruses is the drug VIFERON. Recombinant interferon alpha-2b, which is part of this drug, interferes with the synthesis of viral DNA and RNA, thereby blocking the replication of the virus. The drug also helps restore the immune system.
The drug, which is available in the form of suppositories, gel and ointment, was developed as a result of fundamental research in the field of immunology, which has proven that the presence of antioxidants (vitamins C, E) enhances the effect of interferon. The list of advantages of drugs containing interferon includes their high non-selective antiviral activity. This means that such drugs are able to fight a wide range of acute respiratory viral infections. The use of the drug VIFERON as part of complex antiviral therapy makes it possible to reduce therapeutic doses of antibiotics and hormonal drugs, as well as reduce the toxic effects of this therapy.
The drug in the form of suppositories can be used during pregnancy (from the 14th week), as well as during breastfeeding and when treating children.
VIFERON Gel is also used for the treatment of ARVI. For the treatment of ARVI, including influenza, including those complicated by a bacterial infection, the application of VIFERON gel must be repeated 3-5 times a day for 5 days. VIFERON Ointment can also be used to treat respiratory diseases.
Modern drugs for the treatment of ARVI and influenza
Acute respiratory infections (ARVI) are the most common among all infectious diseases. ARVI and influenza account for at least 70% of infectious diseases. In Russia, about 50 million infectious diseases are registered annually, of which up to 90% of cases are ARVI and influenza.
Almost 90% of the population experience one of the respiratory infections of viral etiology at least once a year, which generally determines high morbidity and even affects the mortality rate [2].
Such a high incidence of respiratory tract diseases is explained by a variety of etiological factors (influenza viruses, parainfluenza, adenoviruses, rhinoviruses, reoviruses, respiratory syncytial (RS) viruses, mycoplasmas, chlamydia, bacterial agents), as well as the ease of transmission of the pathogen and the high variability of viruses.
Differential diagnosis of influenza and ARVI is difficult due to the similarity of the clinical picture of these diseases, but it is quite possible. The main differences can be considered the initial signs of the disease, symptoms of intoxication, the nature of catarrhal symptoms and fever, the type of complications that develop, etc. The clinical diagnosis, confirmed by laboratory tests, determines the choice of therapy.
The clinical picture of ARVI and influenza depends on the causative virus (see table).
It should be noted that complications from ARVI, especially during an epidemic, are recorded in 20–30% of cases. The main causes of complications are disorders of the immune defense, leading to long-term insufficiency in the functioning of the immune system. A decrease in the body's antibacterial resistance leads to protracted periods of convalescence and creates the possibility of complications over a long period of time. A special place among complications is occupied by the so-called post-viral asthenia syndrome (PAS), which can develop in 65% of patients within 1 month from the onset of the disease. The leading symptoms of SPA are fatigue, emotional disturbances and various mental disorders.
The range of drugs used in the treatment of ARVI and influenza is wide and varied. It includes live and inactivated vaccines, chemotherapy drugs with etiotropic action, as well as drugs used for immunocorrective and pathogenetic therapy.
However, the course of influenza and other acute respiratory viral infections remains difficult to control. This is due not only to the polyetiology of these diseases, but also to the unique variability of viruses and the global nature of epidemics. The spread of ARVI largely depends on the environmental, socio-economic situation, the presence of allergic diseases in patients and a number of other factors.
Antiviral drugs
Chemotherapy
The mechanism of action of this group of drugs is based on the selective suppression of individual stages of viral reproduction, without interfering with the vital activity of the cell of the macroorganism. For respiratory infections, two groups of drugs are used - M2 channel blockers and neuroaminidase inhibitors, as well as ribavirin, which is active against the RS virus.
M2 channel blockers
In 1961, a symmetrical amine, amantadine, was synthesized, and then a number of its derivatives (rimantadine, midantan, deutiforin). In our country, rimantadine is widely used, which is used for the treatment and prevention of influenza caused by the type A virus. The effectiveness of this drug is 70–90%.
The antiviral effect is realized by blocking special ion channels (M2) of the virus, which is accompanied by a violation of its ability to penetrate cells and release ribonucleoprotein. This inhibits the most important stage of viral replication. In approximately 30% of cases, resistance to rimantadine may develop [6].
Rimantadine is available in the form of rimantadine in tablets of 50 mg and syrup for children from 1 to 7 years of age - algirem - 2 mg/ml. For therapeutic purposes, the drug is prescribed from the moment the first symptoms are registered. The duration of therapy should not exceed 5 days to avoid the emergence of resistant forms of the virus. As a preventative measure, rimantadine should be taken for at least 2 weeks.
Neuroamindase inhibitors
Drugs in this group are effective not only against type A influenza viruses, but also against type B viruses.
Neuroamindase (sialidase) is one of the key enzymes involved in the replication of influenza viruses. When neuroamindase is inhibited, the ability of viruses to penetrate healthy cells is impaired, their resistance to the protective effect of respiratory tract secretions is reduced, and thus the further spread of the virus in the body is inhibited. Neuroamindase inhibitors are able to reduce the production of cytokines (IL-1 and tumor necrosis factor), preventing the development of a local inflammatory reaction and weakening systemic manifestations of a viral infection such as fever, pain in muscles and joints, and loss of appetite [7].
Preliminary studies have shown that the effectiveness of such an inhibitor as a prophylactic agent is 70–80%. Taking these drugs can reduce the duration of the disease by 1–1.5 days (if you start taking the drug no later than 36–48 hours from the moment the first symptoms appear). At the onset of the disease and in its early stages, the average duration of viral replication is reduced by an average of 3 days, and the number of severe forms of ARVI and influenza, characterized by elevated temperature, by 85%. The drugs do not have a harmful effect on the central nervous system. However, it should be noted that it is not always possible to use them in the first 48 hours: due to the difficulties associated with the differential diagnosis of influenza and other acute respiratory viral infections.
Representatives of neuroamindase inhibitors are oseltamivir and zanamivir.
Oseltamivir (Tamiflu) is prescribed 75–150 mg 2 times a day for 5 days. For prevention - 75 mg 1 or 2 times a day for 4–6 weeks. In patients with creatinine clearance less than 30 ml/min, the dose is reduced by 2 times.
Zanamivir (Relenza) is a structural analogue of sialic acid, a natural substrate of influenza virus neuroamidase, and therefore has the ability to compete with it for binding to the active site. It is inhaled using a special device - a diskhaler. For therapeutic purposes, 10 mg is prescribed 2 times a day (with an interval of 12 hours) for 5 days, for prevention - 10 mg 1 time a day for 4-6 weeks. The inhalation route of administration has the advantage of providing a fairly rapid antiviral effect in the area of the primary source of infection.
Adverse reactions of this group of drugs account for no more than 1.5% of cases. Most often these are headache, dizziness, nausea, diarrhea, and sinusitis. Patients with obstructive bronchopulmonary diseases may develop bronchospasm.
Drugs active against other viruses
Ribavirin (virazol, rebetol), which acts on many RNA and DNA viruses, is used in aerosol dosage form to treat infections caused by the RS virus. It is assumed that the drug inhibits the early stages of viral transcription, disrupting the synthesis of ribonucleoproteins, messenger RNA, and blocking RNA polymerase. It is used inhalation using a nebulizer only in a hospital setting.
When taking ribavirin, bronchospasm, rash, and eye irritation may occur, not only in patients, but also in medical staff. In rare cases, leukopenia, insomnia, and irritability are observed. There is a risk of drug crystallization in the respiratory tract and endotracheal tubes. Has a teratogenic effect.
A promising antiviral drug is plenoconaril, recently developed in the USA. In vitro studies and animal experiments have revealed its activity against enteroviruses and rhinoviruses. Data from the first placebo-controlled studies indicate the effectiveness of the drug against respiratory infections and enteroviral meningitis [8].
In Russia, original antiviral drugs are used, created on the basis of domestic developments. The most widely known of them is arbidol. It has an inhibitory effect on influenza viruses type A and B and other respiratory viruses, the mechanism of which is not fully understood. It is believed that such an effect is associated with both the interferon-inducing and immunomodulatory properties of the drug. In particular, arbidol stimulates the activity of phagocytic cells. Available in tablets of 0.1 g. For medicinal purposes, 0.2 g is prescribed 3-4 times a day for 3-5 days. For prophylactic purposes, 0.2 g/day is used for 10–14 days.
Interferons
Interferons (IFNs) are among the regulators of immunogenesis. They are produced by various cells and not only implement the antiviral response, but also regulate immunological reactions. The main effects of interferons can be divided into antiviral, antimicrobial, antiproliferative, immunomodulatory and radioprotective.
Despite the diversity of the genetic material of viruses, IFNs suppress their reproduction at a stage required for all viruses: they block the onset of translation, i.e., the synthesis of virus-specific proteins. This may explain the universality of the antiviral action of interferon. Under the influence of interferon in the body, the activity of natural killer cells, T-helper cells, cytotoxic T-lymphocytes, phagocytic activity, the intensity of B-lymphocyte differentiation, and the expression of MHC type I and II antigens increases [1].
α- and β-interferons are used to treat viral infections. A good effect in treatment is achieved by the combined use of chemotherapy and IFN drugs.
β-interferon (betaferon) is available in powder form, in bottles containing 9.5 million units of IFN. For influenza, it is instilled or sprayed into the nasal passages at least 4–5 times a day [2].
Human leukocyte interferon is a mixture of interferons synthesized by leukocytes of donor blood in response to exposure to a viral inducer. The drug is administered by inhalation or an aqueous solution prepared from a dry substance in an ampoule or bottle is instilled into the nasal passages.
Viferon - recombinant interferon-α 2b - is available in the form of rectal suppositories and is used in the treatment of acute respiratory viral infections and influenza. Damage to cell membranes observed during the development of the infectious process is the reason for the decrease in the antiviral activity of interferon. Tocopherol acetate and ascorbic acid, which are part of Viferon, are membrane-stabilizing components, antioxidants, in combination with which the antiviral activity of recombinant interferon-α 2b increases 10–14 times [1].
The peculiarities of the administration of the dosage form ensure long-term circulation of interferon-α 2b in the blood.
The drug is used both in newborns and in adult patients with ARVI and influenza in age-specific dosages. Children under 7 years of age are prescribed Viferon-1, children over 7 years of age and adults - Viferon-2.
Interferon inducers
Exogenous interferon preparations are logically combined with the use of its inducers in clinical practice. They represent a very heterogeneous family of high- and low-molecular natural and synthetic compounds, united by the ability to induce in the body the formation of its own (endogenous) interferon α- and β-interferons in different proportions by leukocytes, macrophages, epithelial cells, as well as tissues of the spleen and liver , lungs, brain. The drugs penetrate the cytoplasm and nuclear structures and activate the synthesis of “early” interferons. Helps correct the immune status of the body [3].
Amiksin is a low molecular weight synthetic inducer of endogenous aromatic interferon, belonging to the class of fluorenones. The main structures that produce interferon in response to the administration of amixin are intestinal epithelial cells, hepatocytes, T-lymphocytes, and granulocytes. In human leukocytes, amixin induces the formation of interferon, the level of which in the blood is 250 U/ml. After taking amixin orally, the maximum interferon in humans is determined sequentially in the intestines, liver, and blood after 4–24 hours [2].
When treating influenza and acute respiratory viral infections, amixin is prescribed in the first hours of the disease; 5–6 tablets are enough per course. For the purpose of prevention, it is prescribed once a week for 4–6 weeks.
Cycloferon is a low-molecular-weight inducer of IFN-α, which determines a wide range of its biological activity. It quickly penetrates cells, accumulating in the nucleus and cytoplasm. Cycloferon intercalates cell DNA, which is responsible for the mechanism of its interferon-inducing activity [3].
Cycloferon quickly penetrates the blood. There is low binding to blood proteins and at the same time widespread distribution in various organs, tissues, and biological fluids of the body.
Due to the fact that cycloferon is a low-molecular drug, it easily crosses the blood-brain barrier, causing the formation of IFN in the brain. Cycloferon is quickly eliminated from the body: 99% of the administered drug is eliminated unchanged by the kidneys within 24 hours.
Cycloferon is well tolerated by patients and is prescribed from the first day from the onset of the disease in tablet form or parenterally [4].
Ridostin is a high molecular weight IFN inducer of natural origin. Ridostin is a double-stranded RNA obtained from the lysate of the killer yeast Saccharamyces cervisiae.
Systemic administration of ridostin stimulates the production of early IFN. The maximum accumulation of IFN in serum is observed 6–8 hours after injection; after 24 hours it is not detected in the bloodstream [1].
The drug exhibits a pronounced immunomodulatory effect. It stimulates T-cell and humoral immunity, proliferation of bone marrow stem cells and phagocytic activity of macrophages and neutrophils in peripheral blood. Ridostin increases the level of corticosteroid hormones; used for the treatment and prevention of influenza and other acute respiratory viral infections.
Currently, the drug dibazol, used for the treatment and prevention of influenza and ARVI, is undeservedly forgotten. Dibazol has immunomodulatory activity and induces the production of endogenous interferon. For prevention, 1 tablet (0.02–0.05 g) is prescribed once a day for 3–4 weeks; for treatment, 1 tablet 3 times a day for 5 days.
Indispensable in the treatment of influenza and ARVI are complex drugs such as Grippostad, Rinza, Theraflu, Fervex, as well as drugs for external and local use - Doctor Mom cold ointment, Tussamag cold balm.
Despite the variety of drugs presented for the treatment of acute respiratory viral infections and influenza at the present stage, the choice of a drug remains an urgent task for the practicing physician. The choice of tactics for prescribing and managing a patient with ARVI or influenza is directly related to the severity of the infectious process, the form of the disease and the presence of complications. The success of treatment depends on the correct assessment of the patient’s condition and early initiation of treatment.
O. A. Melnikov , Candidate of Medical Sciences L. V. Averkieva “GUTA-Clinic”, Moscow