Features of the use of indirect anticoagulants
Indirect anticoagulants disrupt the synthesis of coagulation factors in the liver (prothrombin and proconvertin). Their effect appears 8-12 hours after administration and lasts from several days to two weeks. The most important advantage of these drugs is that they have a cumulative effect. Vitamin K antagonists (the second name for indirect anticoagulants) have been used for primary and secondary prevention of thromboembolism for more than 50 years. Vitamin K is an integral part of the coagulation process.
Vitamin K antagonists are called indirect anticoagulants.
Warfarin and other coumarin derivatives are the most commonly used indirect anticoagulants. VKAs (short name for vitamin K antagonists) have many limitations, so you should not start taking them on your own. Only a qualified doctor can select the correct dose based on test results. Regular monitoring of blood counts is of great importance for timely dosage adjustment. Therefore, you need to keep in mind that if your doctor has prescribed you to take warfarin 2 times a day, then you are prohibited from reducing or increasing the dose on your own.
It is also not recommended to resume taking the drug at the same dosage after a long break. Warfarin has a half-life of 40 hours and takes at least 7 days to take effect. The drug is metabolized in the liver and excreted from the body in the urine. Currently, warfarin remains the optimal treatment option for patients with ischemic stroke.
Secondary hemostasis (coagulation)
The formed platelet plug (without subsequent formation of fibrin) can only temporarily stop bleeding, and if the platelet thrombus does not thicken with insoluble fibrin, then such a thrombus will disintegrate after a few hours. Simultaneously with platelet activation, plasma coagulation factors are activated (secondary hemostasis). Goal: stabilization of the primary platelet plug due to the formation of fibrin networks and the formation of a dense and stable fibrin clot.
Clinical significance:
- if disturbances are present at the stages of primary hemostasis (vascular-platelet), for example, thrombocytopenia (< 50,000 cells/mm3) or taking antiplatelet drugs (Aspirin, Plavix), then prolonged and continuous bleeding should be expected during and immediately after surgery (due to disturbances in the formation of the primary platelet plug);
- if disturbances are present at the stages of secondary hemostasis (coagulation), and primary hemostasis is not impaired (for example, taking anticoagulants), bleeding problems will be detected only a few hours, or even the next day, after surgery (when the patient is no longer in the clinic) .
List of indirect anticoagulants and their mechanism of action
The list of indirect anticoagulants is headed by warfarin (another trade name “Coumadin”). It is one of the most popular medications prescribed to prevent blood clots. Less popular vitamin K antagonist drugs are syncumar, acenocoumarol and dicumarol. The mechanism of action of these drugs is identical: a decrease in the activity of vitamin K absorption, which leads to the depletion of vitamin K-dependent blood clotting factors.
Patients taking warfarin and synonymous anticoagulants should limit daily intake of vitamin K from food and dietary supplements. Sudden changes in vitamin K levels in the body can significantly increase or decrease the effect of anticoagulant therapy.
Disadvantages of Vitamin K Antagonists
Warfarin is a real “old-timer” of the pharmaceutical market
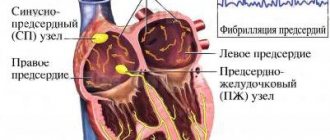
Until the end of 2010, a vitamin K antagonist (warfarin) was the only oral anticoagulant approved by the World Health Organization for the prevention of thromboembolic complications in patients with non-valvular atrial fibrillation and the treatment of venous thromboembolism. For half a century, pharmacists have studied in detail the effectiveness of the drug, and also clearly identified the disadvantages and side effects.
The most common include:
- narrow therapeutic window (for poisoning it is enough to take a minimum number of tablets);
- interaction with foods rich in vitamin K (taking the tablets in combination with daily consumption of green vegetables can lead to hyperkalemia);
- delayed anticoagulant effect (this means that several weeks must pass between the start of therapy and the first results). For the prevention of venous thrombosis, this period is too long;
- the need for frequent blood monitoring and dose adjustments;
- the possibility of bruising and bleeding.
Advantages and disadvantages of direct anticoagulant drugs
Over the past 6 years, new direct anticoagulants have appeared on the pharmaceutical market. They are an alternative to vitamin K antagonists for the treatment of thromboembolism and the prevention of thrombosis. Direct oral anticoagulants (DOAs) are a more effective and safer analogue of vitamin K antagonists.
Direct anticoagulants are the only alternative to vitamin K antagonists
The popularity of PPA among cardiologists and patients is not surprising, because the advantages include:
- rapid onset of action;
- relatively short half-life;
- the presence of specific antidote agents (may be useful in the treatment of acute ischemic strokes, as well as for eliminating post-stroke negative symptoms);
- fixed dosage;
- no direct effect of dietary supplements on the daily dose of the drug;
- no need to undergo regular laboratory blood monitoring.
The most common side effect that occurs after taking DOACs is an increased risk of bleeding. But the perceived threat of severe bleeding is quite small compared to the benefits provided by direct anticoagulants.
Patient taking antiplatelet drugs
Monotherapy
Recent studies have shown that basic surgical skills and local bleeding control measures are sufficient to control bleeding. Antiplatelet monotherapy does not pose a significant risk during or after surgery.
Recommendations [6]: it is strictly not recommended to interrupt the intake of oral antiplatelet agents during outpatient dental procedures, including surgical procedures.
Dual antiplatelet therapy after stent implantation in patients with stable coronary artery disease or acute coronary syndrome (ACS)
Cardiologists recommend dual antiplatelet therapy for at least six weeks after bare metal (inactive) stent implantation, and for 12 months after an episode of ACS or drug-eluting stent (active stent) implantation.
Recommendations [7]: Low-risk dentoalveolar surgery does not require any changes in the treatment plan.
Dentoalveolar surgery with an average risk of bleeding requires consultation with a cardiologist about temporarily stopping one of the drugs before the surgical procedure (monotherapy does not pose a serious risk). If it is not possible to cancel one of the drugs, you can perform the surgical procedure in stages: divide the surgical procedure with an average risk of bleeding into several smaller interventions.
Dentoalveolar surgical procedures with a high risk of bleeding require consultation with a cardiologist regarding temporary discontinuation of one of the medications before the surgical procedure. If it is not possible to discontinue one of the drugs, major surgical operations should be delayed for 1 year.
Trade names of direct anticoagulants and their mechanism of action
The classification of direct-acting drugs is a little more extensive. Dabigatran etexilate (trade name Pradaxa) is a direct thrombin inhibitor. This drug was the first direct oral anticoagulant approved by the medical community. Literally within a few years, rivaroxaban inhibitors (xalerto and edoxaban) were added to the list of direct anticoagulants. Long-term clinical trials have shown the high effectiveness of the above drugs in the prevention of stroke and treatment of thrombosis. DOACs have clear advantages over warfarin, and most importantly, the drugs can be administered without regular monitoring of blood counts.
Pradaxa is the most studied direct-acting anticoagulant
The mechanism of action of DOACs differs significantly from the mechanism of vitamin K antagonists. Each direct anticoagulant contains small molecules that selectively bind to the catalytic site of thrombin. Because thrombin promotes coagulation by converting fibrinogen into fibrin filaments, dabigatran has the effect of blocking these fibrin filaments.
Additional effective mechanisms of direct anticoagulants include platelet deactivation and reduction of blood clotting activity. The half-life of this group of drugs is 7-14 hours, the time for the onset of the therapeutic effect ranges from one to four hours. Direct anticoagulants accumulate in the liver with the formation of active metabolites and are excreted from the body in the urine.
Also, two types of heparins are used as anticoagulants - unfractionated (UFH) and low molecular weight (LMWH). Low-fraction heparin has been used for the prevention and treatment of mild thrombosis for several decades. The disadvantages of UFH are that it has a variable anticoagulant effect, as well as limited bioavailability. Low molecular weight heparin is obtained from low-fraction heparin by depolymerization.
Low molecular weight heparin has a specific molecular weight distribution, which determines its anticoagulant activity and duration of action. The advantage of LMWH is that you can easily calculate the required dosage and not have to worry about severe side effects. For these reasons, it is the low molecular weight heparin that is used in most hospitals around the world.
Heparin solution is used as an anticoagulant.
Consistency and regularity are essential for effective treatment with direct anticoagulants. Because this type of drug has a short half-life, patients who miss doses intentionally or accidentally are at risk for thrombosis or inadequate coagulation. Considering that the positive effect of taking PPA quickly disappears when the drug stops entering the body, it is extremely important to follow the dosage schedule prescribed by your doctor.
The leading role in the formation of a blood clot in the venous vascular bed is played by the activation of blood coagulation processes, which ultimately leads to the appearance of fibrin clots. In this regard, the most effective way to prevent and treat venous thromboembolic complications (VTEC) is the use of anticoagulants - drugs that inhibit the functional activity of coagulation factors present in the blood or prevent the formation of full-fledged coagulation factors in the liver [1-6]. The positive effect of drugs that inhibit the functional activity of platelets (antiplatelet agents), if they exist, is not well documented and is noticeably inferior to anticoagulants. Therefore, antiplatelet agents (acetylsalicylic acid) are not recommended for the prevention and treatment of VTEC.
Features of the practical use of anticoagulants for parenteral administration.
Parenteral (intravenous or subcutaneous) administration of anticoagulants is indispensable in cases where a rapid and guaranteed effect is required.
The greatest experience has been accumulated with the use of heparin
. It is currently believed that the main effect of heparin as an anticoagulant is its ability to interact with antithrombin. This interaction causes a change in the antithrombin molecule, many times enhancing its ability to bind a number of blood coagulation factors, irreversibly inhibiting their procoagulant activity. Among the blood coagulation factors that are neutralized by heparin, the most important are activated factor X (Xa) and thrombin. As a result, during the use of heparin, the number of thrombin molecules decreases, which leads to a decrease in the formation of fibrin, which forms the basis of the blood clot (Fig. 1).
Figure 1. Mechanism of action of anticoagulants administered parenterally.
At the same time, heparin has a number of other effects on the blood coagulation system, the clinical significance of which has not yet been determined. Heparin preparations are obtained from biological raw materials - various tissues of domestic animals, mainly from the intestinal mucosa of pigs. It is a mixture of highly sulfated glycosaminoglycans (mucopolysaccharides) of various lengths with a rather complex structure. In other words, heparin is a drug of biological origin, containing as an active substance chemical compounds extracted from living organisms using biotechnology. Low molecular weight heparin
(LMWH) are obtained from unfractionated substances using additional processing - various chemical or enzymatic depolymerization processes. Accordingly, the composition of LMWH is even more complex, since even with a comparable molecular length, the depolymerization process uniquely changes the structure of the polysaccharide chains. Differences in manufacturing characteristics lead to noticeable discrepancies in the properties of existing LMWH drugs, which are currently considered as separate, non-interchangeable drugs, each of which has its own specific indications, doses and methods of use. In addition, it is obvious that due to the complexity of the structure of the active substance, it is impossible to create an exact copy of the original LMWH drugs, and when developing analogues we are talking only about similar, and not absolutely identical, drugs. The latter presents significant difficulties when creating generics, since in such a situation they require not only evidence of similarity to the original drug in basic physicochemical and pharmacological properties, but also sufficiently convincing evidence of similar clinical efficacy and safety. The final stage of the study, designed to demonstrate comparable effects of the original LMWH drug and its analogue on clinically important outcomes of the disease, has not yet been passed by any of the proposed generic LMWHs [7].
Unlike unfractionated and low molecular weight heparins, fondaparinux
- a drug created using chemical synthesis. It is a small molecule - a pentasaccharide (the synthesized catalytic center of heparin molecules, responsible for their connection with antithrombin). Unlike heparin drugs, fondaparinux promotes the removal of only one blood clotting factor, Xa, from the bloodstream (see Fig. 1).
Main features of the practical use of unfractionated heparin (UFH).
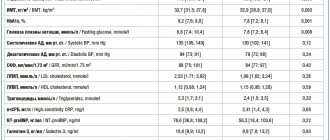
Intravenous UFH is used to treat deep vein thrombosis (DVT) and pulmonary embolism (PE). When administered intravenously, the half-life of UFH depends on the dose and averages 1-1.5 hours (Table 1).
In this regard, to maintain a constant therapeutic concentration of the drug in the blood, it is necessary to carry out continuous intravenous infusion. In addition, UFH neutralize (bind) various cells and proteins circulating in the bloodstream, including acute phase proteins, the content of which increases significantly during massive thrombosis. As a result, the extent of the impact of UFH on a particular patient is unpredictable. Accordingly, the therapeutic dose of UFH must be selected individually, taking into account the severity of the anticoagulant effect of the already administered drug. For general medical practice, it is recommended to use the determination of activated partial thromboplastin time (aPTT) as a control method when selecting the dose of UFH. APTT during the period of UFH dose selection should be determined every 6 hours, with persistent therapeutic values of the indicator (at least with two consecutive determinations) - once in the morning. To simplify the process of selecting the dose of UFH as much as possible, protocols (nomograms) have been proposed that prescribe what to do in cases where certain aPTT values are obtained against the background of intravenous infusion of the drug (Table 2).
Despite all the inconveniences, intravenous infusion of UFH is the most manageable among the treatment regimens of anticoagulation created with the help of parenteral drugs, since the effect of this drug practically ceases 4-6 hours after discontinuation. In addition, UFH has a complete antidote (protamine sulfate). Finally, the renal route of elimination is not the main route for UFH. These circumstances underlie the idea that intravenous infusion of UFH is preferable in the treatment of thrombotic complications in patients with a high risk of bleeding (including severe renal impairment).
Due to the large length of the molecules, UFH poorly enters the bloodstream from the subcutaneous tissue. Therefore, to create a sufficiently high (therapeutic) concentration of the drug in the blood necessary for the treatment of VTEC, it is necessary to use high doses of the drug. Thus, it is recommended to start with subcutaneous administration of 17,500 units (or alternatively 250 units/kg). With subcutaneous administration, the half-life of UFH (8-12 hours) is much longer than with intravenous administration, which allows the drug to be administered no more than 2-3 times a day. In addition, since the goal of heparin treatment is to maintain a therapeutic level of anticoagulation in the blood, when administered subcutaneously, the dose of UFH should also be adjusted to ensure an appropriate increase in aPTT. It is proposed to control the latter halfway between injections (i.e., 6 hours after the next injection with a double subcutaneous administration of a therapeutic dose of UFH).
Prophylactic doses of UFH are used to prevent (but not treat) VTEC. According to modern concepts, in this situation there is no need for individual dose selection under the control of aPTT, and the drug should be administered at a dose of 5000 units 2 or 3 times a day (twice administration is suggested to be used in patients with a moderate risk of DVT or an increased risk of bleeding, with a higher triple injections are recommended at the risk of DVT).
Main features of practical application of LMWH.
By reducing the length of the molecules, LMWHs are able to inactivate blood coagulation factor Xa to a greater extent, enter the bloodstream almost completely when administered subcutaneously, and interact to a lesser extent with blood proteins and cells (see Table 1). Accordingly, when using LMWH there is no need to carry out intravenous infusion of drugs, and a sufficiently long-lasting effect allows LMWH to be administered subcutaneously 1 or 2 times a day. In addition, a more predictable action makes it possible, in most cases, to do without monitoring the severity of the effect of LMWH on the blood coagulation system. The therapeutic dose of LMWH is selected taking into account the patient’s body weight, while for the prevention of DVT, a fixed (same for all patients) dose of LMWH is usually used (with the exception of nadroparin, the prophylactic dose of which in people at high risk of DVT is selected taking into account body weight). The standard prophylactic dose of LMWH has been proposed to be reduced in patients with low body weight and increased by 25% in patients with severe obesity, but these approaches have not been adequately tested.
Since LMWHs have a greater effect on coagulation factor Xa, the only informative way to assess their concentration in the blood is to determine the level of anti-Xa activity. The feasibility of such control (at least once) is discussed in patients with severe (morbid) obesity, when body weight exceeds 150 kg and body mass index is 50 kg/m2, as well as when administering therapeutic doses to pregnant women (for example, 1 time in 3 months). In addition, LMWHs are excreted by the kidneys, and in patients with severe renal failure, a gradual accumulation of the active substance in the blood (cumulation) with an increased risk of bleeding cannot be ruled out. However, the greatest problems usually arise in cases where creatinine clearance does not reach 30 ml/min. In these situations, it is advised to either reduce the dose of LMWH in accordance with the achieved level of activity against activated coagulation factor X, or to prefer UFH, the effect of which is easier to monitor using aPTT. However, on the other hand, experience has been accumulated in the use of LMWH in pregnant women without mandatory coagulological monitoring, and for some LMWH drugs, dose adjustment algorithms have been proposed for patients with creatinine clearance less than 30 ml/min, which do not involve determining anti-Xa activity in the blood. In particular, it is recommended to reduce the daily dose of enoxaparin by half. On the other hand, according to some data [8], no adjustment of the prophylactic dose of dalteparin is required for severe renal failure.
Main features of the practical application of fondaparinux.
Fondaparinux almost completely enters the bloodstream when administered subcutaneously, and the long half-life allows you to limit yourself to one injection per day. The effect of the drug is even more predictable, since it practically does not interact with blood proteins and cells. However, the renal route of elimination poses the same problems with drug accumulation in the blood in patients with impaired renal function as with LMWH (fondaparinux is currently contraindicated in patients with creatinine clearance less than 30 ml/min).
Ensuring safety during parenteral administration of anticoagulants.
The use of anticoagulants is associated with an increased risk of bleeding. Therefore, during their administration, it is necessary to monitor the level of hemoglobin and hematocrit in the blood and actively look for external signs of bleeding (Table 3).
In addition, these indicators should be urgently determined if there is any deterioration in the patient’s condition (for example, the occurrence of arterial hypotension).
UFH and, to a lesser extent, LMWH can cause the development of immune thrombocytopenia, which most often occurs in the first 2 weeks from the start of treatment. Therefore, during these periods it is necessary to regularly monitor the level of platelets in the blood (its decrease by more than half from the initial level is an indication for immediate discontinuation of any heparin drug). In cases where the patient has been administered heparin in the last 3.5 months, this reaction can occur quite quickly (after the first administration of the drug), so the platelet level in the blood should be monitored in the next 24 hours, and if the patient’s condition worsens, immediately. Features of the practical use of anticoagulants for oral administration.
Despite all the advantages of parenteral anticoagulants, the need for intravenous infusion or subcutaneous injection poses serious problems if long-term (often multi-year) treatment is necessary. For a long time, the only way to benefit from the convenience of oral anticoagulants was with vitamin K antagonists (VKAs).
The action of VKAs is fundamentally different from the action of anticoagulants for parenteral administration. VKAs prevent the synthesis in the liver of a number of complete blood clotting factors, as well as proteins that are natural anticoagulants (Fig. 2).
Figure 2. Mechanism of action of vitamin K antagonists.
Of the drugs in this group, warfarin, acenocoumarol and phenindione are registered in the Russian Federation (Fig. 3).
Figure 3. Vitamin K antagonist drugs. In general, coumarin derivatives are the most well studied and most commonly used, and among them is warfarin, so approaches to the management of patients who require long-term use of anticoagulants are usually considered using the example of warfarin. Due to its short half-life, phenindione must be taken several times a day and is less likely to maintain stable levels of anticoagulation. There are many factors that influence individual sensitivity to VKA. These include age, gender, race, body weight, concomitant diseases, dietary habits (vitamin K content in food), numerous drug interactions, as well as genetic factors (for warfarin, at least polymorphism of the cytochrome P450 isoenzyme 2C9 and VCORK1 genes). Therefore, the dose of VKA is selected individually under the control of the International Normalized Ratio (INR). Target (therapeutic) INR values for the prevention and treatment of VTEC range from 2 to 3. If there is no opportunity to regularly monitor the INR, VKAs should not be used.
The effect of VKA increases and decreases slowly. Therefore, treatment of VTEC begins with parenteral administration of anticoagulants (heparin or fondaparinux), and then switches to oral VKA. After starting to take VKA, the liver loses its ability to synthesize complete blood clotting factors, and the faster the higher the initial dose of the drug (Fig. 4).
Figure 4. Onset of action of vitamin K antagonists. FCK - blood clotting factors. At the same time, normally functioning coagulation factors that were formed before the start of VKA dose selection begin to disappear from the bloodstream, each of which has its own half-life. This process cannot be accelerated by increasing the dose of VKA. The manifestation of the full antithrombotic effect of VKA is associated with the disappearance of fully functioning prothrombin from the bloodstream. Therefore, since prothrombin has a fairly long half-life (about 60-72 hours), at least 5 days pass before the required effect of VKA occurs. At the same time, a protein with anticoagulant properties, protein C, disappears from the bloodstream quite quickly, when most blood clotting factors have not yet been replaced by proteins with reduced coagulation activity. Therefore, at the beginning of VKA use, prerequisites for the occurrence of thrombosis may be created. This complication can be avoided by prescribing low starting doses of VKA and selecting the dose of VKA against the background of ongoing parenteral administration of heparin or fondaparinux. The second mandatory condition indicating the end of the VKA dose selection is the receipt in two consecutive blood tests, taken at intervals of approximately 24 hours, of two close INR values that are within the therapeutic range (Fig. 5).
Figure 5. Rapid creation and long-term maintenance of a therapeutic level of anticoagulation: a technique for switching from parenteral administration of anticoagulants to vitamin K antagonists. Stopping parenteral administration of therapeutic doses of heparin or fondaparinux is possible only if two conditions are met: at least 5 days after the start of VKA dose selection and no earlier than stable therapeutic INR values are achieved (at least 2 with two consecutive determinations with an interval of about a day). A common mistake is to stop the parenteral anticoagulant too quickly, which puts patients with VTEC at increased risk of new thrombotic complications during the period of drug changes.
When using warfarin on the 1st and 2nd days, it is recommended to use doses of 5 to 10 mg. However, given the above considerations, it is reasonable to limit the maximum dose to 7.5 mg. Lower initial doses (up to 5 mg) are recommended in patients who are elderly, intellectually impaired, malnourished, have chronic heart failure, liver disease, have had recent major surgery, or are taking drugs that increase sensitivity to warfarin (eg, amiodarone), and in cases where genetic sensitivity to warfarin is not known. INR monitoring may be initiated after taking 2 or 3 doses of warfarin. In this case, in hospitalized patients, the INR is usually determined daily until stable therapeutic values of the indicator are obtained, then 2-3 times a week for 1-2 weeks, and then less often depending on the stability of the INR. When starting warfarin on an outpatient basis, the frequency of INR determinations at the beginning of treatment can be reduced to once every few days until a stable dose of the drug is selected. Once the dose of VKA is selected, the INR should be determined at least every 4 weeks. More frequent determination of INR helps to more effectively maintain this indicator within the therapeutic range. In particular, this approach is recommended for patients with an unstable response to VKAs, the elderly, those with an increased risk of bleeding, liver disease, the occurrence of intercurrent illnesses, major changes in diet and drinking patterns, as well as taking medications that interact with VKAs. If dose adjustment is required, repeat the cycle of more frequent INR monitoring until a stable response to the adjusted dose is again achieved.
Numerous difficulties associated with the practical use of VKAs have stimulated the development of new anticoagulants for oral administration. Among them, the closest to widespread practical use are drugs that selectively and directly (without the participation of cofactors) inhibit activated blood coagulation factor X (apixaban, rivaroxaban) or thrombin (dabigatran) (Fig. 6, Table 4).
Figure 6. Mechanism of action of new oral anticoagulants.
The advantages of these drugs, in addition to the possibility of oral administration, include the use of fixed doses with no need for monitoring of anticoagulant effect, predictable response, absence of immune thrombocytopenia, few drug interactions, and the first dose after surgery for the prevention of DVT in orthopedic surgery. Among the disadvantages are the need to take certain drugs 2 times a day (for some indications), the significant role of the kidneys in the elimination of drugs, studied in a limited number of patients, the lack of an antidote (however, due to the relatively short half-life of the drugs, the expected need for it is small), high price.
Anticoagulants and prevention of VTEC.
Anticoagulants are the most effective currently existing method of preventing VTEC. With their help, you can reduce the risk of these events by 50-60%, and the expected benefit is approximately the same regardless of which pathology is leading (surgical, therapeutic or neurological). There are numerous features associated with the selection of patients, the choice of drugs, their doses, as well as the duration of use of anticoagulants for the purpose of preventing VTEC, which are set out in the relevant clinical recommendations and guidelines and are described in detail in the manufacturer’s recommendations for the use of individual drugs [1, 4]. In general, approaches to the prevention of DVT are presented in Table. 5.
Drug prophylaxis can be started both before and after surgery, since no significant differences in the effectiveness and safety of these regimens have been found.
In the latter case, the sooner after surgery prophylaxis begins, the higher its effectiveness, on the one hand, and the risk of bleeding, on the other. The recommended approach depends on the chosen drug and the clinical situation (nature of surgical treatment, planned method of anesthesia, etc.). In cases where surgery is delayed, in patients at high risk of venous thrombosis (trauma), prophylaxis should be started upon admission to the hospital. In certain groups of high-risk patients, the benefit of prolonging prophylaxis has been proven: up to 28 days (at least after major abdominal and pelvic surgery for cancer) or 35 days (at least after hip replacement or hip fracture surgery). The main results of completed studies [9-18] of new oral anticoagulants in the prevention of DVT and PE are presented in Table. 6-8.
Anticoagulants and treatment of venous thromboembolic complications.
Anticoagulants are the basis of drug treatment for VTEC. For DVT and PE, the same drugs and dosage regimens are used (Table 9).
For DVT and non-massive PE, it is recommended to prefer subcutaneous administration of LMWH or fondaparinux, which are at least as good as intravenous infusion of UFH and are much more convenient.
In case of massive pulmonary embolism, when persistent arterial hypotension or shock is noted, intravenous infusion of UFH should be used. This is due to the fact that other methods of treatment with anticoagulants in such patients have practically not been studied and in this situation thrombolytic therapy or surgical interventions are indicated, which, according to modern concepts, are combined only with intravenous administration of UFH [2-4]. Intravenous infusion of UFH is also reasonable to prefer in the most severe patients with submassive pulmonary embolism, when the possibility of thrombolytic therapy cannot be excluded. In cases where UFH is used, a bolus of drug is initially administered intravenously to quickly achieve therapeutic blood concentrations. Immediately after this, it is necessary to start an intravenous infusion or make the first subcutaneous injection of UFH. Typically, to make the response to the initial intravenous administration of UFH more predictable, it is suggested that the patient's body weight be taken into account when choosing the dose. In addition, the dose of the drug must be high enough to overcome the neutralizing effect of proteins circulating in the blood that neutralize UFH. In the future, regardless of how UFH is administered (intravenous infusion or subcutaneous), the goal of treatment is to increase the aPTT by 1.5-2 times higher than the upper limit of normal for the laboratory of a particular medical institution. However, there is evidence that when using modern equipment and reagents to determine APTT during treatment with UFH, higher values of this indicator should be maintained, increasing it 2-3 times above the upper limit of normal. Ideally, one should aim for a concentration of UFH in the blood that provides a level of activity against activated coagulation factor X of 0.3 to 0.7 IU/ml. To do this, it is necessary to establish in advance for the laboratory of a particular medical institution which APTT values the level of anti-Xa activity of 0.3 and 0.7 IU/ml corresponds to, and during the treatment process, strive to keep the APTT in this therapeutic range.
According to some data, the administration of UFH in fairly high doses (about 35,000 units per day and 250 units/kg 2 times a day subcutaneously) can provide a sufficient clinical effect even in cases where the aPTT is not controlled. However, it seems that such an approach needs to be treated with a fair degree of caution. Thus, the available evidence on the acceptability of uncontrolled administration of high doses of UFH is limited. At the same time, knowing how unpredictable the effect of UFH is in a particular patient, in cases where it is not possible to control the aPTT, it is still advisable to prefer LMWH, leaving uncontrolled subcutaneous administration of high doses of UFH for cases where LMWH are not available. For each of the LMWHs with proven clinical efficacy (dalteparin, nadroparin, enoxaparin), there are dosing regimens with subcutaneous injections 2 times a day or a higher dose once a day. Fondaparinux is administered once a day and its dose depends on the patient’s body weight. The accumulated facts do not allow us to judge the preference of a particular dosage regimen or LMWH drug, as well as LMWH or fondaparinux in the treatment of VTEC.
Once occurring, DVT and PE can recur over a long period. Depending on the clinical situation, the risk of recurrent episodes of VTE remains elevated from several months to many years. According to modern concepts, the duration of the initial antithrombotic treatment of VTEC should be 3 months, after which we are talking about secondary prevention, the duration of which is determined by weighing the risk of relapse after stopping anticoagulant treatment and the risk of bleeding when prolonging the use of anticoagulants in each individual patient. Recommendations for the duration of use of anticoagulants after VTEC are given in Table. 10.
Typically, such long-term treatment involves the use of oral medications (VKAs). In this case, the duration of parenteral administration of therapeutic doses of anticoagulants is determined by the timing of selection of the dose of VKA, ensuring the maintenance of a stable therapeutic effect. It should be at least 5 days (if the selection of the VKA dose began on the 1st day of treatment of the patient) and may be longer in cases where during this time it is not possible to achieve stable therapeutic INR values or the selection of the VKA dose was not started on the 1st day day of patient treatment (Fig. 7).
Figure 7. Duration of use of anticoagulants in VTEC.
There are situations in which extending the period of parenteral administration of LMWH is more effective than standard switching to oral VKA. This at least applies to patients with malignant neoplasms. Evidence was obtained from the multicenter, randomized, open-label CLOT trial [20], performed in 336 patients with symptomatic proximal DVT or PE and active cancer. In it, extending the period of subcutaneous administration of the LMWH dalteparin to 6 months (200 IU/kg once a day in the first month with a transition to approximately 150 IU/kg once a day) turned out to be significantly more effective than the standard approach with a 5-7-day administration of a therapeutic dose dalteparin and switching to VKA. The recurrence rate of clinically significant VTE with long-term administration of dalteparin was 8%, with standard treatment using VKA - 15.8%, which corresponds to a significant reduction in risk in the dalteparin group by 52%. However, there were no significant differences in the incidence of major bleeding. Evidence in favor of the effectiveness and safety of prolonged use of LMWH for DVT or PE in cancer patients was also obtained in a clinical trial with a 3-month administration of a therapeutic dose of enoxaparin (1.5 mg/kg once daily) [21]. In it, the sum of cases of recurrent VTE and major bleeding, as well as the incidence of major bleeding and mortality, taken separately, were 2 times lower in patients receiving enoxaparin. However, the small number of patients (146 in total) did not make it possible to draw definite conclusions from the results of this study.
If VKAs cannot be used (eg, pregnancy or inability to control the INR), the only alternative currently is to continue subcutaneous injections of UFH or LMWH. However, in addition to the obvious inconvenience, this approach has another significant drawback - the optimal dose of heparin in this situation remains unknown. Thus, it is logical to continue administering the full therapeutic dose of heparin, but there are concerns that with long-term use this will be unacceptable due to the risk of bleeding. In addition, they suggest switching to 75-80% of the treatment dose (as for cancer) or using a slightly higher prophylactic dose. The latter is for dalteparin 5000 IU 2 times a day, for enoxaparin 40 mg 2 times a day, for UFH - subcutaneously 2 times a day in order to maintain anti-Xa activity in the blood from 0.1 to 0.3 U/ml (approximately 10,000 units per injection). The effectiveness and safety of none of the above approaches have been adequately studied. Therefore, the results of studies of new oral anticoagulants after an episode of DVT or PE are awaited with particular interest. Currently, only one such study using dabigatran (RE-COVER) has been completed (see Table 4). This multicenter, randomized, double-blind clinical trial included 2564 patients with symptoms of proximal DVT or PE who did not have severe renal impairment. Taking dabigatran at a fixed dose of 150 mg 2 times a day for 6 months after the initial parenteral administration of anticoagulants was not inferior to the standard use of VKA in its ability to prevent clinically significant relapses of VTE. There were also no significant differences in the incidence of major bleeding between the two approaches. However, when using dabigatran, any bleeding was less frequently observed, as well as a combination of major and clinically significant non-major bleeding. In some categories of patients who have experienced VTEC, we can soon expect a significant simplification of approaches to long-term use of anticoagulants.
Is it possible to combine direct and indirect anticoagulants?
As has already become clear, anticoagulants are used for therapeutic and prophylactic purposes for heart attacks, angina pectoris, vascular embolism of various organs, thrombosis, and thrombophlebitis. In acute conditions, direct anticoagulants are usually prescribed, which provide an immediate effect and prevent blood clotting. After 3-4 days (subject to the success of primary treatment), therapy can be enhanced with indirect anticoagulants.
Combined anticoagulant therapy is also carried out before operations on the heart and blood vessels, during blood transfusions, and also for the prevention of thrombosis. Treatment with a combination of different types of anticoagulants should be carried out under the constant supervision of medical professionals. Due to the increased frequency of angina attacks and paroxysmal atrial fibrillation, when treated with two types of drugs simultaneously, the presence of sediment in the urine, the rate of blood clotting and the level of prothrombin in the blood are constantly monitored.
Combined anticoagulant therapy should occur under medical supervision
Treatment with a combination of different anticoagulants is contraindicated in:
- hemorrhagic diathesis;
- diseases accompanied by decreased blood clotting;
- during pregnancy;
- liver and kidney dysfunction;
- malignant neoplasms;
- peptic ulcer disease.
It is also necessary to urgently interrupt combination therapy if blood appears in the urine.
Complexes with this research
Male check-up No. 1 39 studies for annual preventive examination 16,200 ₽ Composition
Preventive check-up Universal annual preventive screening 4,870 ₽ Composition
Examination during pregnancy. 3rd trimester 7,630 ₽ Composition
IN OTHER COMPLEXES
- Miscarriage RUB 35,200
- For those at risk of COVID-19 RUB 3,520
- Examination during pregnancy. 1st trimester 13,820 RUR
- Risk of severe COVID-19 960 RUR
- Joining IVF RUB 19,370
How to determine the effectiveness of taking anticoagulants?
Indirect coagulants are easy to detect in the blood and even measure their effectiveness. For this purpose, a special indicator called “international normalized ratio” has been developed.
- A person not taking indirect anticoagulants will have an INR just below 1.
- A patient taking warfarin will have an INR between 2.0 and 3.0. Seeing such high numbers, doctors will be prepared for the possibility of sudden bleeding.
- An INR between 1 and 2 will indicate that the patient may be at risk of developing an ischemic stroke.
- With an INR of 4 or higher, there is the greatest risk of blood non-coagulation and the development of hemorrhagic stroke.
A blood test for INR is indicative of therapy with indirect anticoagulants
But a blood test for INR will not provide objective indicators if the patient is taking direct anticoagulants. The biggest problem with the newer direct anticoagulants is the lack of a reliable way to assess their effectiveness. Doctors can tell when bleeding stops, but there is no indicator that assesses the presence of anticoagulant effects. For example, this is very important when treating patients who are admitted to the emergency room in an unconscious state. If the medical record does not indicate any information about the patient taking direct-acting anticoagulants, it is quite difficult to quickly detect them in the blood.
What to do in case of overdose?
Despite all of the above benefits, doctors are still concerned about the lack of specific antidotes to use in the event of an overdose. To prevent such a serious condition, doctors adhere to the following rules:
- reduce the dose of epobaxan after 7 days of use;
- Xalerto requires a dose reduction after a course of 21 days.
Currently, when life-threatening bleeding occurs, including those caused by indirect anticoagulants, the patient is administered fresh frozen plasma, prothrombin complex concentrate, and Phytonadione.
Phytonadione is one of the few antidotes to anticoagulants
The pharmacology and mechanism of action of each antidote are different. Different anticoagulants will require different doses and strategies for administering antidotes. The duration of the course and dosage of antidotes is calculated depending on how the patient reacts to the drugs already administered (there are cases when some antidotes not only stop bleeding, but also activate platelet aggregation).
Mortality rates with DOACs and VKAs
Patients receiving direct anticoagulants to prevent complications of heart disease had a higher incidence of sudden bleeding, but at the same time lower mortality rates, compared with patients who received vitamin K antagonists. It should not be concluded that the presence of bleeding is what - thus helping to reduce mortality rates.
These conflicting results are due to the fact that most studies are conducted in hospital settings. All bleeding that occurs when the patient is in the hospital and receives direct anticoagulants through an IV is very quickly stopped by qualified medical personnel and does not lead to death. But the patient most often takes indirect anticoagulants without medical supervision, which leads to a higher mortality rate.
Antiplatelet drugs (drugs that disrupt primary hemostasis)
Acetylsalicylic acid (ASA)
Egyptian papyri that date back to approximately 1550 BC. e., mention the use of a decoction of white willow leaves for many diseases. Hippocrates prescribed willow bark extract for headaches and fever. Willow is the first source of aspirin. Acetylsalicylic acid, the active ingredient in Aspirin, was synthesized from willow bark by Edward Stone in 1897. The age of medicine is shorter than the age of man and many of them quickly become obsolete. But Aspirin not only has not become obsolete over the last hundred years, it has also demonstrated new qualities. It seems to cure everything from colds to strokes.
Acetylsalicylic acid (ASA) has been the gold standard of antiplatelet therapy for many years. Aspirin in low doses (40-100 mg) irreversibly blocks the action of the enzyme cyclooxygenase-1 in platelets with a subsequent decrease in the formation of thromboxane A2, which is a powerful vasoconstrictor and proplatelet agent. Since ASA blocks COX-1 irreversibly, the antiplatelet effect persists throughout the life cycle of the platelet (7–10 days). The ability to irreversibly block platelet COX-1 distinguishes ASA from other non-steroidal anti-inflammatory drugs, the antiplatelet effect of which is short-term [1]. Considering the above, I would like to draw attention to the following clinical point.
What happens when a dentist prescribes an NSAID to a patient taking Aspirin? Data from epidemiological studies indicate that taking drugs from the NSAID group can cancel or significantly reduce the cardioprotective effect of aspirin.
Why? Aspirin and NSAIDs compete for the same substrate - COX 1. Therefore, with parallel administration, part of the platelets will be reversibly associated with NSAIDs, and the other part will be irreversibly associated with acetylsalicylic acid. After a few hours, platelets that were temporarily inactivated by NSAID drugs will restore their function and the patient will be left without cardioprotective action.
Which analgesics are contraindicated and which are the drug of choice in such patients can be learned in detail from my lectures.
In the RISK (Research on Instability in Coronary Artery Disease) study, when ASA was prescribed at a dose of 75 mg/day to patients with unstable angina, the risk of developing myocardial infarction decreased by 50% [2]. In another study in patients with acute MI, the effectiveness of ASA (160 mg/day) was comparable to the effectiveness of thrombolytic therapy [3].
Many patients receive dual antiplatelet therapy (Aspirin + Clopidogrel). In acute coronary syndrome, as well as after percutaneous coronary intervention (PCI) or stent placement, ASA is usually prescribed in combination with Clopidogrel. According to numerous studies, discontinuation of antiplatelet therapy in patients with an active stent is correlated with a 90-fold increase in the risk of stent thrombosis [4]. The literature has also documented thromboembolic complications with a fatal outcome due to unauthorized discontinuation of anticoagulant/antiplatelet drugs by the dentist before surgery. The risk of bleeding increases dramatically with dual antiplatelet therapy during surgery.