Sumamed
Antacids do not affect the bioavailability of azithromycin, but reduce Cmax in the blood by 30%, so Sumamed® should be taken at least 1 hour before or 2 hours after taking these drugs and food.
Concomitant use of azithromycin with cetirizine (20 mg) for 5 days in healthy volunteers did not lead to pharmacokinetic interaction or a significant change in the QT interval.
The simultaneous use of azithromycin (1200 mg/day) and didanosine (400 mg/day) in 6 HIV-infected patients did not reveal changes in the pharmacokinetic parameters of didanosine compared to the placebo group.
Simultaneous use of macrolide antibiotics, incl. azithromycin, with P-glycoprotein substrates such as digoxin, leads to increased concentrations of P-glycoprotein substrate in the blood serum. Thus, with the simultaneous use of azithromycin and digoxin, it is necessary to take into account the possibility of increasing the concentration of digoxin in the blood serum.
The simultaneous use of azithromycin (single dose of 1000 mg and multiple doses of 1200 mg or 600 mg) has a minor effect on pharmacokinetics, incl. renal excretion of zidovudine or its glucuronide metabolite. However, the use of azithromycin caused an increase in the concentration of phosphorylated zidovudine, a clinically active metabolite in peripheral blood mononuclear cells. The clinical significance of this fact is unclear.
Azithromycin interacts weakly with isoenzymes of the cytochrome P450 system. Azithromycin has not been shown to participate in pharmacokinetic interactions similar to erythromycin and other macrolides. Azithromycin is not an inhibitor or inducer of cytochrome P450 isoenzymes.
Given the theoretical possibility of ergotism, the simultaneous use of azithromycin with ergot alkaloid derivatives is not recommended.
Pharmacokinetic studies were conducted on the simultaneous use of azithromycin and drugs whose metabolism occurs with the participation of isoenzymes of the cytochrome P450 system.
Concomitant use of atorvastatin (10 mg daily) and azithromycin (500 mg daily) did not cause changes in atorvastatin plasma concentrations (based on an HMC-CoA reductase inhibition assay). However, in the post-marketing period, isolated case reports of rhabdomyolysis have been received in patients receiving concomitant azithromycin and statins.
Pharmacokinetic studies involving healthy volunteers did not reveal a significant effect on the plasma concentrations of carbamazepine and its active metabolite in patients receiving concomitant azithromycin.
In pharmacokinetic studies of the effect of cimetidine when taken in a single dose on the pharmacokinetics of azithromycin, no changes in the pharmacokinetics of azithromycin were detected, provided that cimetidine was used 2 hours before azithromycin.
In pharmacokinetic studies, azithromycin did not affect the anticoagulant effect of warfarin when taken in a single dose of 15 mg in healthy volunteers. Potentiation of the anticoagulant effect has been reported after simultaneous use of azithromycin and indirect anticoagulants (coumarin derivatives). Although a causal relationship has not been established, the need for frequent monitoring of prothrombin time should be considered when using azithromycin in patients receiving indirect oral anticoagulants (coumarin derivatives).
In a pharmacokinetic study involving healthy volunteers who took azithromycin (500 mg/day once) orally for 3 days, followed by cyclosporine (10 mg/kg/day once), a significant increase in plasma Cmax and AUC0-5 of cyclosporine was detected. . Caution is required with this combination. If concomitant use of these drugs is necessary, plasma concentrations of cyclosporine should be monitored and the dose adjusted accordingly.
Concomitant use of azithromycin (600 mg/day once) and efavirenz (400 mg/day) daily for 7 days did not cause any clinically significant pharmacokinetic interaction.
Concomitant use of azithromycin (1200 mg once) did not change the pharmacokinetics of fluconazole (800 mg once). The total exposure and T1/2 of azithromycin did not change with simultaneous use of fluconazole, however, a decrease in Cmax of azithromycin was observed (by 18%), which had no clinical significance.
The simultaneous use of azithromycin (1200 mg once) did not cause a statistically significant effect on the pharmacokinetics of indinavir (800 mg 3 times a day for 5 days).
Azithromycin does not have a significant effect on the pharmacokinetics of methylprednisolone.
The simultaneous use of azithromycin (1200 mg) and nelfinavir (750 mg 3 times / day) causes an increase in the Css of azithromycin in the blood plasma. No clinically significant side effects were observed and no dose adjustment of azithromycin was required when used concomitantly with nelfinavir.
The simultaneous use of azithromycin and rifabutin does not affect the concentration of each drug in the blood plasma. Neutropenia has sometimes been observed with simultaneous use of azithromycin and rifabutin. Although neutropenia has been associated with the use of rifabutin, a causal relationship between the use of the combination of azithromycin and rifabutin and neutropenia has not been established.
When used in healthy volunteers, there was no evidence of the effect of azithromycin (500 mg/day daily for 3 days) on the AUC and Cmax of sildenafil or its main circulating metabolite.
In pharmacokinetic studies, there was no evidence of interaction between azithromycin and terfenadine. There have been isolated cases reported where the possibility of such an interaction could not be completely excluded, but there was no concrete evidence that such an interaction occurred. It has been found that the simultaneous use of terfenadine and macrolides can cause arrhythmia and prolongation of the QT interval.
No interaction has been detected between azithromycin and theophylline.
No significant changes in pharmacokinetic parameters were detected with simultaneous use of azithromycin with triazolam or midazolam in therapeutic doses.
When trimethoprim/sulfamethoxazole was co-administered with azithromycin, there was no significant effect on Cmax, total exposure or renal excretion of trimethoprim or sulfamethoxazole. Azithromycin serum concentrations were consistent with those found in other studies.
Sumamed® (Sumamed®)
Antacids
Antacids do not affect the bioavailability of azithromycin, but reduce the maximum blood concentration by 30%, so the drug should be taken at least one hour before or two hours after taking these drugs and eating.
Cetirizine
Concomitant use of azithromycin with cetirizine (20 mg) for 5 days in healthy volunteers did not lead to pharmacokinetic interaction or a significant change in the QT interval.
Didanosine (dideoxyinosine)
The simultaneous use of azithromycin (1200 mg/day) and didanosine (400 mg/day) in 6 HIV-infected patients did not reveal changes in the pharmacokinetic indications of didanosine compared to the placebo group.
Digoxin (P-glycoprotein substrates)
Concomitant use of macrolide antibiotics, including azithromycin, with P-glycoprotein substrates, such as digoxin, leads to increased concentrations of P-glycoprotein substrate in the blood serum. Thus, with the simultaneous use of azithromycin and digoxin, it is necessary to take into account the possibility of increasing the concentration of digoxin in the blood serum.
Zidovudine
Concomitant use of azithromycin (single dose of 1000 mg and multiple doses of 1200 mg or 600 mg) has a minor effect on the pharmacokinetics, including renal excretion of zidovudine or its glucuronide metabolite. However, the use of azithromycin caused an increase in the concentration of phosphorylated zidovudine, a clinically active metabolite in peripheral blood mononuclear cells. The clinical significance of this fact is unclear.
Azithromycin interacts weakly with isoenzymes of the cytochrome P450 system. Azithromycin has not been shown to participate in pharmacokinetic interactions similar to erythromycin and other macrolides. Azithromycin is not an inhibitor or inducer of cytochrome P450 isoenzymes.
Ergot alkaloids
Given the theoretical possibility of ergotism, the simultaneous use of azithromycin with ergot alkaloid derivatives is not recommended.
Pharmacokinetic studies were conducted on the simultaneous use of azithromycin and drugs whose metabolism occurs with the participation of isoenzymes of the cytochrome P450 system.
Atorvastatin
Concomitant use of atorvastatin (10 mg daily) and azithromycin (500 mg daily) did not cause changes in atorvastatin plasma concentrations (based on an HMC-CoA reductase inhibition assay). However, in the post-marketing period, isolated case reports of rhabdomyolysis have been received in patients receiving concomitant azithromycin and statins.
Carbamazepine
Pharmacokinetic studies involving healthy volunteers did not reveal a significant effect on the plasma concentrations of carbamazepine and its active metabolite in patients receiving concomitant azithromycin.
Cimetidine
In pharmacokinetic studies of the effect of a single dose of cimetidine on the pharmacokinetics of azithromycin, no changes in the pharmacokinetics of azithromycin were detected when cimetidine was used 2 hours before azithromycin.
Indirect anticoagulants (coumarin derivatives)
In pharmacokinetic studies, azithromycin did not affect the anticoagulant effect of a single 15 mg dose of warfarin administered to healthy volunteers. Potentiation of the anticoagulant effect has been reported after simultaneous use of azithromycin and indirect anticoagulants (coumarin derivatives). Although a causal relationship has not been established, the need for frequent monitoring of prothrombin time should be considered when using azithromycin in patients receiving indirect oral anticoagulants (coumarin derivatives).
Cyclosporine
In a pharmacokinetic study involving healthy volunteers who took azithromycin (500 mg/day once) orally for 3 days and then cyclosporine (10 mg/kg/day once), a significant increase in maximum plasma concentration (Cmax) and area under the concentration-time curve (AUC0-5) of cyclosporine. Caution is advised when using these drugs together. If simultaneous use of these drugs is necessary, it is necessary to monitor the concentration of cyclosporine in the blood plasma and adjust the dose accordingly.
Efavirenz
Concomitant use of azithromycin (600 mg/day once) and efavirenz (400 mg/day) daily for 7 days did not cause any clinically significant pharmacokinetic interaction.
Fluconazole
Concomitant use of azithromycin (1200 mg once) did not change the pharmacokinetics of fluconazole (800 mg once). The total exposure and half-life of azithromycin did not change with simultaneous use of fluconazole, however, a decrease in Cmax of azithromycin was observed (by 18%), which had no clinical significance.
Indinavir
Concomitant use of azithromycin (1200 mg once) did not cause a statistically significant effect on the pharmacokinetics of indinavir (800 mg three times a day for 5 days).
Methylprednisolone
Azithromycin does not have a significant effect on the pharmacokinetics of methylprednisolone.
Nelfinavir
The simultaneous use of azithromycin (1200 mg) and nelfinavir (750 mg 3 times a day) causes an increase in the equilibrium concentrations of azithromycin in the blood serum. No clinically significant side effects were observed and no dose adjustment of azithromycin was required when used concomitantly with nelfinavir.
Rifabutin
The simultaneous use of azithromycin and rifabutin does not affect the concentration of each drug in the blood serum. Neutropenia has sometimes been observed with simultaneous use of azithromycin and rifabutin. Although neutropenia has been associated with the use of rifabutin, a causal relationship between the use of the combination of azithromycin and rifabutin and neutropenia has not been established.
Sildenafil
When used in healthy volunteers, there was no evidence of the effect of azithromycin (500 mg/day daily for 3 days) on the AUC and Cmax of sildenafil or its main circulating metabolite.
Terfenadine
In pharmacokinetic studies, there was no evidence of interaction between azithromycin and terfenadine. There have been isolated cases reported where the possibility of such an interaction could not be completely excluded, but there was no concrete evidence that such an interaction occurred.
It has been found that the simultaneous use of terfenadine and macrolides can cause arrhythmia and prolongation of the QT interval.
Theophylline
No interaction has been detected between azithromycin and theophylline.
Triazolam/midazolam
No significant changes in pharmacokinetic parameters were detected with simultaneous use of azithromycin with triazolam or midazolam in therapeutic doses.
Trimethoprim/sulfamethoxazole
Concomitant use of trimethoprim/sulfamethoxazole with azithromycin did not reveal a significant effect on Cmax, total exposure or renal excretion of trimethoprim or sulfamethoxazole. Azithromycin serum concentrations were consistent with those found in other studies.
Sumamed 500 mg 3 pcs. film-coated tablets
pharmachologic effect
Antibiotic azalide.
Composition and release form Sumamed 500 mg 3 pcs. film-coated tablets
Tablets - 1 tablet:
- active substance azithromycin dihydrate 524.109 mg, respectively, in terms of azithromycin 500.00 mg;
- excipients: anhydrous calcium hydrogen phosphate 93.891 mg, hypromellose 6.00 mg, corn starch 48.00 mg, pregelatinized starch 40.00 mg, microcrystalline cellulose 33.60 mg, sodium lauryl sulfate 2.40 mg, magnesium stearate 12.00 mg;
- shell: hypromellose 13.60 mg, indigo carmine dye (E132) 0.40 mg, titanium dioxide (E171) 2.24 mg, polysorbate 80 0.56 mg, talc 11.20 mg.
3 tablets per blister made of PVC/aluminum foil.
1 blister along with instructions for use in a cardboard box.
Description of the dosage form
Oval, biconvex tablets, blue, engraved with “PLIVA” on one side and “500” on the other side.
The fractured appearance is white to almost white.
Directions for use and doses
Orally, without chewing, at least 1 hour before or 2 hours after meals, 1 time per day.
Adults and children over 12 years of age weighing more than 45 kg
For infections of the upper and lower respiratory tract, ENT organs. Skin and soft tissues: 1 tablet (500 mg) 1 time per day for 3 days (course dose 1.5 g).
For moderate acne: 1 tablet (500 mg) once a day for 3 days, then 1 tablet (500 mg) once a week for 9 weeks (course dose 6.0 g).
The first weekly tablet should be taken 7 days after taking the first daily tablet (8th day from the start of treatment), the subsequent 8 weekly tablets should be taken at intervals of 7 days.
For Lyme disease (initial stage of borreliosis) - erythema migrans: 1 time per day for 5 days: 1st day - 1.0 g (2 tablets of 500 mg), then from 2nd to 5th day - 1 tablet (500 mg) (course dose 3.0 g).
For urinary tract infections caused by Chlamydia trachomatis (urethritis, cervicitis): uncomplicated urethritis/cervicitis - 1 g (2 tablets of 500 mg) once.
Fly aged 3 to 12 years with a body weight of less than 45 kg
For infections of the upper and lower respiratory tract, ENT organs, skin and soft tissues: at the rate of 10 mg/kg body weight once a day for 3 days (course dose 30 mg/kg).
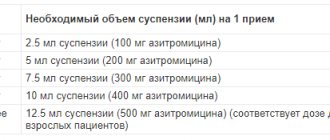
Calculation of the dose of Sumamed® for children weighing less than 45 kg
- Body weight 18-30 kg - 2 tablets (250 mg azithromycin).
- Body weight 31-44 kg - 3 tablets (375 mg azithromycin).
- Body weight of at least 45 kg - doses recommended for adults are used.
In children under 3 years of age, it is recommended to use Sumamed®, powder for the preparation of an oral suspension 100 mg/5 ml and Sumamed® forte, powder for the preparation of an oral suspension 200 mg/5 ml.
For pharyngitis/tonsillitis caused by Streptococcus pyogenes, the drug Sumamed® is used at a dose of 20 mg/kg/day for 3 days (course dose 60 mg/kg). The maximum daily dose is 500 mg.
For Lyme disease (initial stage of borreliosis) - erythema migrans: 20 mg/kg once a day on the 1st day, then at the rate of 10 mg/kg once a day from the 2nd to the 5th day.
For ease of use in children of a course dose of 60 mg/kg, it is recommended to take Sumamed®, powder for the preparation of an oral suspension 100 mg/5 ml and Sumamed® forte, powder for the preparation of an oral suspension 200 mg/5 ml.
In case of renal dysfunction: when used in patients with mild to moderate renal dysfunction (creatinine clearance more than 40 ml/min), no dose adjustment is required.
For liver dysfunction: When used in patients with mild to moderate liver dysfunction, no dose adjustment is required.
Elderly patients: no dose adjustment is required. Since elderly people may already have current proarrhythmogenic conditions, caution should be exercised when using the drug Sumamed® due to the high risk of developing cardiac arrhythmias, including arrhythmias.
Pharmacodynamics
Has a wide spectrum of antimicrobial action. By binding to the 50S ribosomal subunit, it inhibits the biosynthesis of microorganism proteins. In high concentrations it has a bactericidal effect. It is active against gram-positive, gram-negative anaerobes, intracellular and other microorganisms.
Has no effect on gram-positive bacteria resistant to erythromycin.
Pharmacokinetics
When taken orally, azithromycin is well absorbed and quickly redistributed from plasma to tissues and organs. After a single oral dose of 500 mg of azithromycin, 37% of the drug is absorbed and after 2-3 hours the Cmax of the drug is 0.41 mcg/ml in the plasma. It is known that food intake can reduce the absorption of azithromycin, however, due to the insufficiency of the manufacturer's own data on the effect of food on the pharmacokinetics of azithromycin when taking Sumamed® in the form of a suspension, it should be taken at least 1 hour before or after 2 h after eating.
The drug is rapidly distributed throughout the body, high concentrations, 50 times higher than the concentration of azithromycin in plasma, are observed in tissues. Depending on the organ/tissue, the drug concentration ranges from 1-9 mcg/ml. The volume of distribution averages 31 l/kg.
The therapeutic concentration of azithromycin in tissues is observed within 5-7 days after taking the last dose. Penetrates into cells, including phagocytes, which migrate to the site of inflammation, helping to create therapeutic concentrations of the drug that exceed the MIC for infectious agents. Concentrations of azithromycin in infected tissues are higher compared to uninfected tissues. It has a long T1/2 and is slowly eliminated from tissues (on average 2-4 days).
Excretion of azithromycin into bile is the main route of elimination. On average, up to 50% is excreted in bile in unchanged form. The remaining 50% is excreted in the form of 10 metabolites formed during the process of N- and O-demethylation, hydroxylation of desosamine and aglycone ring and as a result of cleavage of the cladinose conjugate. Metabolites do not have antibacterial activity. An average of 6% of the administered dose of the drug is excreted in the urine.
In elderly patients (over 65 years of age), the volume of distribution is slightly higher (30%) compared to patients under 45 years of age, which is not clinically significant and does not require dosage changes.
The pharmacokinetics of azithromycin in healthy volunteers after a single intravenous infusion lasting more than 2 hours at a dose of 1000-4000 mg (solution concentration 1 mg/ml) has a linear relationship and is proportional to the administered dose. T1/2 of the drug is 65-72 hours. The high level of observed volume of distribution (33.3 l/kg) and plasma clearance (10.2 ml/min/kg) suggests that the long T1/2 of the drug is a consequence of the accumulation of the antibiotic in tissues followed by its slow release.
In healthy volunteers, with an intravenous infusion of azithromycin at a dose of 500 mg (solution concentration 1 mg/ml) for 3 hours, the Cmax of the drug in the blood serum was 1.14 μg/ml. The minimum serum level (0.18 μg/ml) was observed over 24 hours and the area under the concentration-time curve was 8.03 μg/ml/h.
Similar pharmacokinetic values were obtained in patients with community-acquired pneumonia who were prescribed intravenous infusions (3 hours) for 2 to 5 days. After daily administration of azithromycin at a dose of 500 mg (infusion duration - 1 hour) for 5 days, an average of 14% of the dose is excreted in the urine over a 24-hour dosing interval.
Indications for use Sumamed 500 mg 3 pcs. film-coated tablets
- infections of the upper respiratory tract and ENT organs;
- lower respiratory tract infections: acute bronchitis, exacerbation of chronic bronchitis, pneumonia, incl. caused by atypical pathogens;;
- skin and soft tissue infections;
- genitourinary tract infections (urethritis, cervicitis).
Contraindications
- severe dysfunction of the liver and kidneys;
- lactation period;
- simultaneous use with ergotamine and dihydroergotamine;
- hypersensitivity to azithromycin and other components of the drug;
- increased sensitivity to macrolide antibiotics;
- children under 12 years of age and body weight less than 45 kg (for capsules and tablets 500 mg);
- children under 3 years of age (for tablets 125 mg).
Sumamed should be prescribed with caution in cases of moderate impairment of liver and kidney function, in patients with disorders or predisposition to arrhythmias and prolongation of the QT interval.
Application of Sumamed 500 mg 3 pcs. film-coated tablets during pregnancy and breastfeeding
During pregnancy, the use of sumamed is possible only if the potential benefit of therapy for the mother outweighs the possible risk to the fetus.
If it is necessary to use sumamed during lactation, breastfeeding should be stopped
special instructions
When using the drug Sumamed® in patients with diabetes mellitus, as well as on a low-calorie diet, it is necessary to take into account that the suspension contains sucrose (0.32 XE/5 ml).
If you miss one dose of Sumamed®, the missed dose should be taken as soon as possible, and subsequent doses should be taken at intervals of 24 hours. Sumamed® should be taken at least one hour before or two hours after taking antacids.
The drug Sumamed® should be taken with caution in patients with mild to moderate liver dysfunction due to the possibility of developing fulminant hepatitis and severe liver failure.
If there are symptoms of liver dysfunction, such as rapidly increasing asthenia, jaundice, darkening of urine, tendency to bleeding, hepatic encephalopathy, therapy with Sumamed® should be stopped and a study of the functional state of the liver should be performed.
In case of mild to moderate renal dysfunction (creatinine clearance more than 40 ml/min), therapy with Sumamed® should be carried out with caution under monitoring the state of renal function.
As with the use of other antibacterial drugs, during therapy with Sumamed®, patients should be regularly examined for the presence of non-responsive microorganisms and signs of the development of superinfections, including fungal ones. The drug Sumamed® should not be used in longer courses than indicated in the instructions, since the pharmacokinetic properties of azithromycin allow us to recommend a short and simple dosage regimen.
There is no data on a possible interaction between azithromycin and ergotamine and dihydroergotamine derivatives, but due to the development of ergotism with the simultaneous use of macrolides with ergotamine and dihydroergotamine derivatives, this combination is not recommended.
With long-term use of the drug Sumamed®, the development of pseudomembranous colitis caused by Clostridium difficile, both in the form of mild diarrhea and severe colitis, is possible. If antibiotic-associated diarrhea develops while taking Sumamed®, as well as 2 months after the end of therapy, clostridial pseudomembranous colitis should be excluded.
When treated with macrolides, including azithromycin, prolongation of cardiac repolarization and QT interval was observed, increasing the risk of developing cardiac arrhythmias, including arrhythmias, which can lead to cardiac arrest.
Caution should be exercised when using the drug Sumamed® in patients with the presence of proarrhythmogenic factors (especially in elderly patients), including congenital or acquired prolongation of the QT interval; in patients taking antiarrhythmic drugs of classes IA (quinidine, procainamide), III (dofetilide, amiodarone and sotalol), cisapride, terfenadine, antipsychotic drugs (pimozide), antidepressants (citalopram), fluoroquinolones (moxifloxacin and levofloxacin), with fluid and electrolyte disorders balance, especially in the case of hypokalemia or hypomagnesemia, clinically significant bradycardia, cardiac arrhythmia or severe heart failure.
The use of Sumamed® may provoke the development of myasthenic syndrome or cause an exacerbation of myasthenia.
Impact on the ability to drive vehicles and operate machinery
If undesirable effects on the nervous system and organ of vision develop, caution should be exercised when performing actions that require increased concentration and speed of psychomotor reactions.
Overdose
Symptoms: nausea, temporary hearing loss, vomiting, diarrhea.
Treatment: gastric lavage, symptomatic therapy.
Side effects Sumamed 500 mg 3 pcs. film-coated tablets
From the hematopoietic system: rarely - thrombocytopenia, neutropenia, eosinophilia.
From the central nervous system and peripheral nervous system: sometimes - dizziness/vertigo, headache, drowsiness, convulsions; rarely - paresthesia, asthenia, insomnia, hyperactivity, aggressiveness, anxiety, nervousness.
From the digestive system: often - nausea, vomiting, diarrhea, abdominal pain and cramps; sometimes - diarrhea, flatulence, digestive disorders, anorexia; rarely - constipation, discoloration of the tongue, pseudomembranous colitis, cholestatic jaundice, hepatitis, changes in laboratory parameters of liver function; very rarely - liver dysfunction and liver necrosis (possibly fatal).
Allergic reactions: sometimes - itching, skin rashes; rarely - angioedema, urticaria, photosensitivity, anaphylactic reaction, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis.
Drug interactions
Sumamed® (capsules, film-coated tablets, powder for oral suspension)
Antacids (containing aluminum, magnesium, ethanol) and food intake significantly reduce the absorption of azithromycin (capsules and suspension), so the drug should be taken at least 1 hour before or 2 hours after taking these drugs and food. It does not bind to the enzymes of the cytochrome P-450 complex and, unlike macrolide antibiotics, to date there has been no interaction with theophylline, terfenadine, carbamazepine, methylprednisolone, cimetidine, triazolam, digoxin. Macrolides, when taken simultaneously with cycloserine, indirect anticoagulants, methylprednisolone, felodipine and drugs subject to microsomal oxidation (cyclosporine, hexobarbital, ergot alkaloids, valproic acid, disopyramide, bromocriptine, phenytoin, oral hypoglycemic agents) slow down the elimination, increase the concentration and toxicity of these drugs, while with the use of azalides such an interaction has not been observed to date.
If it is necessary to take it together with warfarin, it is recommended to carefully monitor the PT (there may be an increase in PT and the incidence of hemorrhages). When macrolides are taken simultaneously with ergotamine and dihydroergotamine, their toxic effects (vasospasm, dysesthesia) may occur. Lincosamides weaken, and tetracycline and chloramphenicol enhance the effectiveness of azithromycin. Pharmaceutically incompatible with heparin.
Sumamed® (lyophilisate for the preparation of solution for infusion)
Although there is no data on interactions between azithromycin and ergot alkaloids, caution must be exercised as simultaneous administration can lead to an increase in the concentration of alkaloids in the blood and to the development of overdose symptoms (ergotism), which is observed when alkaloids are taken together with macrolides; Antibiotics of the macrolide group increase the blood concentration of theophylline, terfenadine, warfarin, carbamazepine, phenytoin, digoxin, cyclosporine, ergotamine, triazolam and midazolam, thereby enhancing their effect. Unlike macrolides, azithromycin does not inhibit cytochrome P450, therefore, when it is prescribed with the above drugs, similar interactions are not observed.
SUMAMED FORTE por. d/prig. susp. 200 mg/5 ml vial. 37.5 ml
Interaction
Antacid drugs
Antacid drugs do not affect the bioavailability of azithromycin, but reduce the maximum concentration in the blood by 30%, so the drug should be taken at least one hour before or two hours after taking these drugs and eating.
Cetirizine
Concomitant use of azithromycin with cetirizine (20 mg) for 5 days in healthy volunteers did not lead to pharmacokinetic interaction or a significant change in the QT interval.
Didanosine (dideoxyinosine)
The simultaneous use of azithromycin (1200 mg/day) and didanosine (400 mg/day) in 6 HIV-infected patients did not reveal changes in the pharmacokinetic indications of didanosine compared to the placebo group.
Digoxin (P-glycoprotein substrates)
Concomitant use of macrolide antibiotics, including azithromycin, with P-glycoprotein substrates, such as digoxin, leads to increased concentrations of P-glycoprotein substrate in the blood serum. Thus, with the simultaneous use of azithromycin and digoxin, it is necessary to take into account the possibility of increasing the concentration of digoxin in the blood serum.
Zidovudine
Concomitant use of azithromycin (single dose of 1000 mg and multiple doses of 1200 mg or 600 mg) has a minor effect on the pharmacokinetics, including renal excretion of zidovudine or its glucuronide metabolite. However, the use of azithromycin caused an increase in the concentration of phosphorylated zidovudine, a clinically active metabolite in peripheral blood mononuclear cells. The clinical significance of this fact is unclear. Azithromycin interacts weakly with isoenzymes of the cytochrome P450 system. Azithromycin has not been shown to participate in pharmacokinetic interactions similar to erythromycin and other macrolides. Azithromycin is not an inhibitor or inducer of cytochrome P450 isoenzymes.
Ergot alkaloids
Given the theoretical possibility of ergotism, the simultaneous use of azithromycin with ergot alkaloid derivatives is not recommended. Pharmacokinetic studies were conducted on the simultaneous use of azithromycin and drugs whose metabolism occurs with the participation of isoenzymes of the cytochrome P450 system.
Atorvastatin
Concomitant use of atorvastatin (10 mg daily) and azithromycin (500 mg daily) did not cause changes in atorvastatin plasma concentrations (based on HMG-CoA reductase inhibition assay). However, in the post-marketing period, isolated case reports of rhabdomyolysis have been received in patients receiving concomitant azithromycin and statins.
Carbamazepine
Pharmacokinetic studies involving healthy volunteers did not reveal a significant effect on the concentration of carbamazepine and its active metabolite in the blood plasma in patients receiving concomitant azithromycin.
Cimetidine
In pharmacokinetic studies of the effect of a single dose of cimetidine on the pharmacokinetics of azithromycin, no changes in the pharmacokinetics of azithromycin were detected when cimetidine was used 2 hours before azithromycin.
Indirect anticoagulants (coumarin derivatives)
In pharmacokinetic studies, azithromycin did not affect the anticoagulant effect of a single 15 mg dose of warfarin administered to healthy volunteers. Potentiation of the anticoagulant effect has been reported after simultaneous use of azithromycin and indirect anticoagulants (coumarin derivatives). Although a causal relationship has not been established, the need for frequent monitoring of prothrombin time should be considered when using azithromycin in patients receiving indirect oral anticoagulants (coumarin derivatives).
Cyclosporine
In a pharmacokinetic study involving healthy volunteers who took azithromycin (500 mg/day once) orally for 3 days and then cyclosporine (10 mg/kg/day once), a significant increase in maximum plasma concentration (Cmax) and area under the concentration-time curve (AUC0-5) of cyclosporine. Caution is advised when using these drugs together. If simultaneous use of these drugs is necessary, it is necessary to monitor the concentration of cyclosporine in the blood plasma and adjust the dose accordingly.
Efavirenz
Concomitant use of azithromycin (600 mg/day once) and efavirenz (400 mg/day) daily for 7 days did not cause any clinically significant pharmacokinetic interaction.
Fluconazole
Concomitant use of azithromycin (1200 mg once) did not change the pharmacokinetics of fluconazole (800 mg once). The total exposure and half-life of azithromycin did not change with simultaneous use of fluconazole, however, a decrease in Cmax of azithromycin was observed (by 18%), which was not of clinical significance.
Indinavir
Concomitant use of azithromycin (1200 mg once) did not cause a statistically significant effect on the pharmacokinetics of indinavir (800 mg three times a day for 5 days).
Methylprednisolone
Azithromycin does not have a significant effect on the pharmacokinetics of methylprednisolone.
Nelfinavir
The simultaneous use of azithromycin (1200 mg) and nelfinavir (750 mg 3 times a day) causes an increase in the equilibrium concentrations of azithromycin in the blood serum. No clinically significant side effects were observed and no dose adjustment of azithromycin was required when used concomitantly with nelfinavir.
Rifabutin
The simultaneous use of azithromycin and rifabutin does not affect the concentration of each drug in the blood serum. Neutropenia has sometimes been observed with simultaneous use of azithromycin and rifabutin. Although neutropenia has been associated with the use of rifabutin, a causal relationship between the use of the combination of azithromycin and rifabutin and neutropenia has not been established.
Sildenafil
When used in healthy volunteers, there was no evidence of the effect of azithromycin (500 mg/day daily for 3 days) on the AUC and Cmax of sildenafil or its main circulating metabolite.
Terfenadine
In pharmacokinetic studies, there was no evidence of interaction between azithromycin and terfenadine. There have been isolated cases reported where the possibility of such an interaction could not be completely excluded, but there was no concrete evidence that such an interaction occurred. It has been found that the simultaneous use of terfenadine and macrolides can cause arrhythmia and prolongation of the QT interval.
Theophylline
No interaction has been detected between azithromycin and theophylline.
Triazole
m/
midazolam
No significant changes in pharmacokinetic parameters were detected with simultaneous use of azithromycin with triazolam or midazolam in therapeutic doses.
Trimethoprim/sulfamethoxazole
Concomitant use of trimethoprim/sulfamethoxazole with azithromycin did not reveal a significant effect on Cmax, total exposure or renal excretion of trimethoprim or sulfamethoxazole. Azithromycin serum concentrations were consistent with those found in other studies.