Mercury thermometers are used to determine body temperature and are an integral part of a home medicine cabinet. The advantage of the device is its high accuracy - up to 0.01 degrees. The downside is the toxicity of the liquid metal and its health hazard. Mercury poisoning from a thermometer is common in medical practice.
How does mercury poisoning occur?
Mercury poisoning is a condition of the body caused by ingestion of mercury vapor or the substance itself into the respiratory tract through the gastrointestinal tract, as well as mercury compounds.
When the concentration of mercury is more than 0.25 milligrams per cubic meter, various problems with the respiratory system begin to develop; at higher densities, almost all other internal organs and systems of the body are affected.
In human blood, an excessive concentration of mercury is considered to be 35 ng/ml or more, in urine – 150 μg/l. Experts believe that children and women are most susceptible to mercury vapor.
Both organic and inorganic mercury can cause poisoning. Elemental or inorganic mercury is used in sphygmomanometers, thermometers, and materials for making fillings. Mercury salts are used in the production of certain medicines, plastics, and food products. Organic mercury can be found in cosmetics, paints, foods and medicines.
Mercury salts are often methylated in bacteria, which leads to contamination of the environment with this metal and its deposition in living organisms, for example, in fish. Further, it turns out that by eating such poisoned fish, a person poisons his body.
Inorganic mercury vapor enters the human body along with the air and settles in the lungs. Afterwards, through the pulmonary alveoli they penetrate into the circulatory system and are carried with the blood to all internal organs and systems. The absorption of this metal by the gastrointestinal tract is very small. Elemental mercury is excreted from the human body in feces and urine. Quite a bit of it comes back out with the help of the lungs. Its half-life is approximately two months.
Inorganic mercury and its compounds that enter the human body with food cause the greatest harm to the digestive system: it corrodes the mucous membranes of the stomach and intestines, due to which it spreads throughout the body. Mercury salts settle mostly in the kidneys, the rest of them affect the liver, spleen, intestines, lungs, skin, bone marrow and blood. It is also excreted through the urinary system and feces. In such cases, its half-life is about forty days.
Organic methylated mercury and its compounds enter the body mainly orally - through the mouth. It is usually quickly absorbed in the intestines, as well as through the pores of the skin. Such mercury is also dangerous because it easily penetrates the placental and blood-brain barriers, as well as into breast milk. Due to its binding to blood proteins, methylated mercury is distributed throughout the body, settling mostly in the circulatory system, kidneys and central nervous system. Organic metal is excreted from the human body with urine. The half-life reaches seventy days.
Toxic dose for humans
The toxic dose of a toxic substance depends on the individual characteristics of the person, the age of the victim, the route of entry of mercury into the body, and the duration of exposure to the poison. Separately, one should take into account the form in which the liquid metal was at the time it entered the body.
Table 1. Lethal doses of mercury
| Form of mercury | Lethal dose | |
| In an adult | In children | |
| In inorganic compounds | 10–42 mg/kg | 10–42 mg/kg |
| In organic compounds | 10–60 mg/kg | 10–60 mg/kg |
| Metal in the form of vapors | 2.5 g | |
| Oral Compounds | From 0.1–0.3 g to 3 g | |
Chronic intoxication develops when the concentration of toxic metal vapors in the air is from 0.001 to 0.005 mg/m3. For acute inhalation injury, the MPC is 0.13–0.80 mg/m3.
Symptoms of mercury poisoning
The first symptoms indicating mercury poisoning begin to appear when the concentration of this metal in the blood is more than 500 ng/ml and in the urine more than 600 μg/ml. There are acute and chronic mercury poisoning.
Signs characteristic of acute metal poisoning:
- severe cough, asthma attacks, catarrh of the upper respiratory tract;
- sore throat when swallowing, shortness of breath, chest pain, pneumonia;
- headaches and dizziness, body tremors;
- increased excitability;
- increased body temperature up to 40 degrees, chills;
- severe fluid loss leading to dehydration;
- abdominal pain, nausea, tenesmus, vomiting and bloody diarrhea;
- bleeding gums, gingivitis;
- metallic taste in the mouth, profuse salivation.
The manifestation of signs of chronic mercury poisoning is called mercurialism. The phenomenon of micromercurialism is also known, in which a person exhibits some signs of mercury poisoning when exposed to slightly small doses of the metal for five to ten years.
Signs of incipient mercurialism are:
- general weakness, apathy, severe fatigue;
- frequent urination, severe swelling of the limbs;
- nausea, vomiting, loss of appetite;
- decreased taste, sense of smell, skin sensitivity;
- stomatitis, gingivitis, tooth loss;
- excessive salivation, increased sweating;
- tremor of the limbs, turning into trembling throughout the body;
- skin rashes, hyperkeratosis and hypertrichosis of the skin, dermatitis;
- photophobia, increased excitability, insomnia or drowsiness, decreased intellectual abilities, irritability, headaches and dizziness;
- heart rhythm disturbances, low blood pressure, acrodynia or pink disease.
Classification
The disease is divided according to severity (severe, moderate, mild), causes (domestic, criminal, professional), type of damaging agent (metallic mercury or its salts), and the presence of complications (liver, renal failure, encephalopathy). The most common classification criterion is the nature of the pathology:
- Acute mercury poisoning. It occurs due to the simultaneous entry into the body of a large amount of a toxic substance. Occurs in cases of criminal intoxication, industrial accidents, and inhalation of high concentration vapors. A similar type is diagnosed in 18-20% of victims.
- Mercurialism. Variant of the chronic course of the disease. Symptoms of pathology are determined in people who have been receiving small doses of Hg for a long time. It is often diagnosed in production workers who operate liquid metal, even when the necessary precautions are taken. The share in the overall structure of the disease is 30-32%.
- Micromercurialism. Signs of exotoxicosis are detected in patients who have been in contact with mercury compounds for 5-15 years. The reason is the regular intake of microdoses of the xenobiotic, leading to its accumulation. Characterized by a less specific course. Micromercurialism accounts for about 40% of the total number of mercury exotoxicoses.
Complications and consequences of mercury poisoning
Mercury poisoning does not leave its mark on the body and, without proper treatment, in most cases leads to serious complications and unforeseen consequences, which are expressed in:
- delirium;
- paralysis;
- respiratory failure;
- coma and death.
If a pregnant woman inhales high concentrations of mercury vapor, this does not go away without consequences for the unborn baby. In severe cases, this leads to atrophy of the cerebellum or cerebral cortex and the development of cerebral palsy in the fetus.
Postpartum poisoning with mercury vapor or mercury compounds in some cases leads to:
- headaches;
- hearing, speech and vision impairment;
- impaired movement coordination;
- paresthesia and paralysis;
- memory loss;
- stupor, coma and death.
It happens that some of these symptoms remain with the poisoned person for the rest of his life.
Diagnostics
Immediate mercury poisoning is diagnosed by an ambulance paramedic. The diagnosis is confirmed in the hospital, where the patient is prescribed a series of laboratory and instrumental examinations. Consultations with a neurologist, gastroenterologist, and therapist are required. Mercurialism is detected when a patient goes to a clinic or poison control center. The following diagnostic methods are used:
Causes of mercury poisoning
Sources of mercury poisoning are:
- mercury lamps;
- mercury thermometers;
- fluorescent gas-discharge energy-saving lamps;
- mercury-zinc batteries;
- dental fillings with amalgam;
- medications: mercuzal, calomel, sublimate;
- industrial combustion of gas or coal in large quantities;
- fish or shellfish living in environmentally polluted waters;
- places of natural origin of mercury.
First aid for mercury poisoning
If a person has signs of acute mercury vapor poisoning, it is necessary:
- Remove the injured person from the affected area.
- Make him drink several glasses of salted water or a weak solution of potassium permanganate.
- Induce vomiting mechanically.
- Rinse your throat with a weak solution of manganese.
- Give a few glasses of water again.
- Give the victim "Unitiol" - a universal remedy that is an antidote for heavy metal poisoning. Activated carbon in this case is useless and its use will not affect the patient’s condition in any way.
- Give the poisoned person laxatives.
After providing first aid, it is necessary to transport the injured person to a medical facility for further treatment.
All treatment of a person poisoned by heavy metals, in particular mercury, comes down to removing them from the victim’s body as quickly as possible. For this purpose, complex medications with active dithiol groups are used. If renal failure is detected, it is advisable to prescribe hemodialysis or peritoneal dialysis.
Symptomatic treatment is also often used to improve the patient's condition.
Forecasts
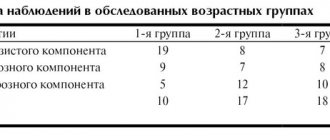
Patients recovering from mercury intoxication
The prognosis for mercury poisoning is favorable only in mild stages of the acute form of the disease or mercurialism. At the same time, competent treatment allows you to almost completely remove the toxicant.
Moderate intoxication usually has delayed consequences in the form of neurological pathology and mental disorders (insomnia, outbursts of anger).
Severe and terminal stages of poisoning require a full course of therapy: antidotes, hemodialysis, infusion, forced diuresis, symptomatic treatment, etc. However, even with successful detoxification, such patients usually experience negative consequences throughout their lives, often becoming disabled.
Prevention of poisoning by mercury vapors and compounds
To prevent this type of poisoning, it is necessary to observe safety measures.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
When working at industrial enterprises in conditions of possible poisoning by mercury vapor, you should rinse your mouth daily with a solution of potassium permanganate or potassium chlorate. Keep the mercury thermometer away from children. It is best to replace mercury thermometers with safer ones: electronic or infrared. Stop using energy-saving mercury lamps and replace them with more energy-efficient LED lamps. Do not eat fish and shellfish caught in polluted waters. Do not leave a child unattended while measuring their temperature with a mercury thermometer. Do not self-medicate and take medications prescribed by your doctor.