Symptoms of acute tracheitis
Acute tracheitis is manifested primarily by attacks of coughing - dry, painful, quite rough and intrusive. It intensifies at night and in the morning, which is associated with the accumulation of sputum in the respiratory tract. A coughing attack during tracheitis can also be provoked by other factors: laughter, screaming, deep breaths, contrasting air temperature, strong aromas and smoke. In the first days, sputum is hardly formed or remains so viscous that it is difficult to pass away. Therefore, at the beginning of the disease, the cough is dry, annoying, and does not bring relief. As tracheitis develops and when the bronchi are involved in the inflammatory process, sputum production increases and it becomes thinner. At the same time, the cough becomes moist, more productive and less exhausting, and its attacks are repeated less frequently. The patient's well-being improves significantly.
In addition to cough, other symptoms of acute tracheitis are often observed:
- pain, a feeling of rawness and burning behind the sternum, especially pronounced after another coughing attack;
- changes in the frequency and depth of breathing;
- increased body temperature (usually up to 38°C), which is typical mainly for infectious and complicated tracheitis;
- headache;
- general weakness, fatigue, fatigue and other signs of general intoxication.
It is important to know!
The inflammatory process with tracheitis often spreads to neighboring areas of the respiratory system, because there is no clear boundary between them, the mucous membrane smoothly passes from one part of the respiratory tract to another. The drainage of sputum or its upward movement when coughing contributes to tissue irritation and the spread of the pathogen. When the bronchi are involved in inflammation, tracheobronchitis develops. This is accompanied by a deterioration in the patient’s condition: his body temperature rises, coughing attacks become more frequent, chest pain becomes stronger, shortness of breath may appear. If tracheitis is accompanied by laryngitis, you need to be prepared for hoarseness or even temporary loss of voice. And with accompanying swelling of the subglottic space of the larynx (it is located approximately under the vocal cords), acute respiratory failure may develop with difficulty inhaling and a feeling of fear.
Diagnosis in children
When examining children, much attention is paid to objective examination data. The child often cannot describe his complaints, so the doctor conducts a more thorough examination.
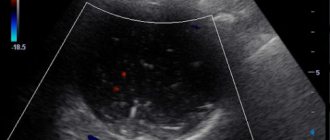
When auscultating the chest, harsh breathing is heard. Wheezing is not characteristic of tracheitis (if they are found in a child, they indicate the development of bronchitis or pneumonia).
In children, an X-ray of the lungs is more often prescribed, since there is a greater likelihood of the process “lowering” into the bronchi and lungs.
Examination of the larynx using a laryngoscope allows you to timely diagnose the spread of edema to the vocal cords and avoid a dangerous complication for the child - false croup.
Why does acute tracheitis occur?
Infection
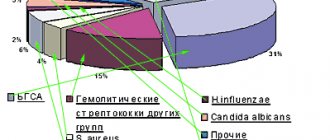
The development of the disease is most often caused by viral infections - influenza and other viruses that affect the respiratory tract and respiratory system. Bacteria can also be causative agents: pneumo-, strepto-, staphylococci and others. Often there is a so-called mixed infection, when inflammation is caused by several different pathogens at once. In this case, most often the bacterial infection is secondary; it complicates the course of ARVI.
Non-infectious factors
Acute tracheitis in an adult can also be non-infectious in nature, although this is less common.
- Mechanical injuries
. Traumatic tracheitis is possible when foreign bodies enter the respiratory tract, for example, as a result of insufficiently careful endoscopic examination of the bronchial system and tracheal intubation during surgical anesthesia.
- Thermal effects - inhalation of cold or (less often) very dry hot air
. In this case, the key point in the development of inflammation is not irritation of the walls of the trachea, but the vascular spasm that occurs in them. This leads to disruption of the functioning of the glands in the walls of the trachea and a decrease in the protective function of its mucous membrane.
- Chemical burns that occur when inhaling fumes from alkaline or acidic products
. These can be aggressive household chemicals, industrial waste, paint and varnish products, petroleum products, chemical reagents. This type of tracheitis is especially difficult.
- Irritation of the mucous membrane of the respiratory tract by polluted, dusty or excessively dry air
. Tobacco smoke, including passive smoking, is of particular importance.
- An allergic reaction in response to the entry of individually significant allergens into the respiratory tract
. In this case, tracheitis is usually combined with laryngitis, obstructive bronchitis (complete obstruction of the bronchial tubes) or even pulmonary edema.
Sometimes tracheitis becomes an occupational disease, that is, its occurrence is associated with harmful factors at work. Therefore, workers in hot shops, farms, chemical and oil refineries, as well as miners and stonemasons are at risk.
Prevention
What should be the prevention of tracheitis? All preventive measures are aimed at strengthening the immune system, as well as desensitization, that is, reducing the body’s sensitivity to the effects of allergens. To prevent inflammation of the trachea, it is recommended:
- treat diseases in a timely manner - eliminate dental caries, colds and exacerbations of chronic diseases in a timely manner;
- normalize nutrition - include vegetables and fruits high in vitamins in the diet;
- take vitamins and immunostimulants - in the spring-autumn period it is advisable to use “Aevit”, “Immunal”, “Ascovit”, etc.;
- give up bad habits - eating fatty foods, smoking, alcohol abuse.
If you are prone to allergies, you need to carefully monitor the cleanliness of your home, since dust, animal hair and polluted or dry air irritate the throat and, as a result, provoke the development of allergic tracheitis.
What contributes to the development of tracheitis?
Tracheitis does not develop in all people who have an acute respiratory viral infection, have been in contact with irritating substances, or have been frozen. The risk of tracheal damage increases in the presence of predisposing factors. First of all, these are any background diseases of the upper respiratory tract, accompanied by impaired nasal breathing. A runny nose of any nature, sinusitis, severe curvature of the nasal septum lead to the fact that a person begins to breathe through the mouth. As a result, insufficiently warmed and humidified air enters the larynx and trachea, which irritates the mucous membrane and increases the risk of inflammation during infection. Predisposing factors include heart disease, accompanied by chronic heart failure with stagnation in the pulmonary circulation. The resulting swelling of the mucous membrane leads to a decrease in its barrier function. Lack of vitamins and nutrients, decreased immunity, excess toxins in the body - all this also increases the risk of inflammation of the trachea in response to the introduction of a pathogen or hypothermia.
Complications
We have already mentioned some dangerous complications of tracheitis. Let's look at them in more detail:
- Development of bronchial tracheitis and pneumonia. A frequent complication of incorrect, untimely therapy and in patients with a weakened immune system. The differences between tracheitis and bronchitis are as follows: the patient’s general condition worsens, intoxication, shortness of breath and other signs of respiratory failure increase, and a creak appears in the lung after tracheitis. This complication requires immediate hospitalization of the patient in a hospital.
- False croup in children. Due to the anatomical narrowness of the glottis in a child, the spread of edema to the mucous membrane of the larynx leads to acute attacks of suffocation. Such a complication is a reason to immediately call an ambulance.
- Bronchial asthma is a severe complication of allergic tracheitis.
Treatment of acute tracheitis
Acute tracheitis must be treated under the supervision of a specialist. In some cases, additional examination is required to clarify the cause and nature of the disease.
The main objectives are:
- impact on the cause of the disease. This includes stopping an allergic reaction, eliminating an infection, removing a foreign body, avoiding the action of provoking factors;
- relief of coughing, transformation of a dry cough into a wet one;
- reducing the severity of inflammation;
- elimination of background and aggravating conditions of tracheitis: lack of vitamins, exhaustion, weakened immunity;
- reducing the severity of intoxication and (if necessary) lowering body temperature. It is important to remember that fever is a natural mechanism to fight infection. Therefore, you should not abuse antipyretics. They can improve your well-being, but do not affect the course of the disease.
Uncomplicated forms of tracheitis can be treated on an outpatient basis. But severe cases of the disease may require hospitalization. Particular attention is paid to the treatment of weakened and elderly patients, especially if they are unable to move independently for health reasons, because tracheitis in them quite easily turns into tracheobronchitis and even pneumonia. Treatment is carried out comprehensively, using medications and non-drug methods. You should not interrupt therapy after the condition improves; you must follow the time limits for taking medications recommended by your doctor.
Drug treatment of tracheitis
The drug treatment regimen for acute tracheitis is drawn up taking into account the nature of the disease and the severity of the patient’s symptoms.
Impact on the cause
If the causative agent is a particular virus, antiviral agents are usually used, as well as immunostimulants (for example, preparations based on echinacea). For severe and protracted tracheitis of a bacterial nature, the doctor may introduce antibiotics into the treatment regimen. If the disease proceeds without complications, it is usually possible to cope with it without these remedies. But the decision on the rationality and duration of antibiotic therapy should be made only by a doctor. In some cases, with tracheitis, a bacteriological examination of sputum is carried out before starting treatment with antimicrobial agents. It is sown on nutrient media to determine the type of pathogen and its sensitivity to the main groups of drugs. This will help you choose the most suitable antibiotic.
Treating coughs and clearing the airways
When treating acute tracheitis, great attention should be paid, of course, to cough, the main symptom of the disease. For a dry, debilitating, nonproductive cough, medications that suppress the cough reflex are used. This measure may be necessary in the first days of tracheitis. At the next stage of the disease, the main goal of treatment is to clear the airways of the mucus that forms. To do this, it is necessary to facilitate its passage with the help of mucolytic and expectorant agents. But they cannot be used simultaneously with antitussive drugs. It is also unacceptable to suppress a wet cough. This is fraught with stagnation of sputum and the transition of inflammation to the underlying parts of the respiratory system, up to the development of bronchopneumonia.
Maintenance therapy
Herbal remedies may be helpful to relieve the symptoms of tracheitis. For tracheitis, they can be used in the form of decoctions and infusions. But a more convenient and reliable method of treatment is the use of ready-made herbal products with a carefully selected and balanced composition. For example, in a complex treatment regimen for tracheitis, you can include Doctor MOM® cough syrup, which contains extracts of licorice, elecampane, Vasiki adatodes, Indian nightshade and other medicinal plants - 10 medicinal plants in total. It is suitable for both adults and children over 3 years old. This remedy helps thin mucus and helps remove it from the respiratory tract, and also relieves inflammation. For adults, there are also herbal cough lozenges Doctor MOM® based on extracts of licorice, ginger and Emblica officinalis. They also soften coughs and have anti-inflammatory and expectorant effects. Such lozenges can be used as an aid in the treatment of tracheitis. They help cope with coughing attacks and ease the course of the disease.
Folk remedies
Effective folk remedies for tracheitis:
- Marshmallow root. Available in syrup form. The basis of the drug is plant mucilage. It softens the throat, eliminating pain and promoting mucosal restoration. A protective film is formed on the surface of the epithelium, which reduces the irritating effect during a coughing attack. Marshmallow root also contains substances that thin phlegm and promote its removal.
- Marshmallow root. Available in syrup form. The basis of the drug is plant mucilage. It softens the throat, eliminating pain and promoting mucosal restoration. A protective film is formed on the surface of the epithelium, which reduces the irritating effect during a coughing attack. Marshmallow root also contains substances that thin phlegm and promote its removal.
- Heat the milk, put a teaspoon of butter and half a teaspoon of soda into a cup, drink the mixture in small sips.
- Oak bark. The main therapeutic effect of the bark is associated with tannins (their concentration can reach 20%). They promote the desquamation of epithelium affected by microbial agents and the improvement of the mucous membrane.
Compresses stand apart in folk medicine. It makes sense to administer them when there is no fever, the cough has become productive, but night attacks torment the patient, that is, approximately starting from the fourth day of illness. The compress for tracheitis is applied for 20 minutes an hour before bedtime. Under no circumstances should you put a compress on your throat, so as not to catch the thyroid gland. Only on the chest.
Compress recipes:
- A tablespoon of honey and 3 drops of eucalyptus essential oil.
- A tablespoon of dry mustard, two teaspoons of honey, 20 ml of sunflower oil, 3 drops of fir oil.
- Boil two potatoes, mash, add a spoonful of sunflower oil.
General tips on how to help the body cope with illness
For any disease of the respiratory tract, including tracheitis, you should follow some simple rules.
- Drink more warm liquids: fruit drinks and heated mineral water without carbon, decoctions of rose hips, raspberries and linden blossoms. This will not only help relieve intoxication, but will also help thin the sputum.
- Eat high-calorie, vitamin-rich foods. During illness, the body needs nutrients to repair tissue and maintain the functioning of the immune system.
- Stop smoking and ask family members to smoke only outside the home.
- Eliminate irritating factors: smoke, dust, strong odors. During illness, it is advisable not to use household chemicals and temporarily stop using perfumes and eau de toilette.
- Ventilate the room and maintain a sufficient level of humidity. Dry air irritates the mucous membrane of the respiratory tract and provokes coughing attacks.
With timely treatment, tracheitis resolves within 10–14 days, without leaving any consequences and without subsequently limiting the ability to work.
First signs
Usually tracheitis begins according to a similar scenario with acute respiratory infections. First, the patient has a runny nose and a dry cough. A person may complain of weakness, sore throat, pain in the head. Hyperthermia up to 38-39 degrees can last up to 3 days, but sometimes it may not increase at all or rise to subfebrile levels of 37.5-38.0.
In young children, when tracheitis begins to develop, wheezing that can be heard at a distance may occur in the morning. Such wheezing usually goes away after the patient has cleared his throat. Shortness of breath with tracheitis, as a rule, does not occur.