Otitis is one of the most common diagnoses in the daily practice of an otolaryngologist. In acute otitis media, we observe an inflammatory process affecting one of the parts of the human hearing organ. The appearance of acute pain in the ear is the main symptom signaling the onset of inflammation.
The disease is common among both children and adults. Although children are at increased risk of developing acute inflammation. This is due to the structural features of the child’s ear and weak, fragile immunity.
Diseases of the hearing organ, like any other disease concentrated in the head area, must be treated carefully and responsibly, since an infection through the bloodstream can easily reach the brain and cause irreversible consequences. Therefore, it is necessary to treat an acute inflammatory process as soon as the first prerequisites for the disease appear. Treatment of the disease should be carried out in a hospital, under the supervision of a competent doctor.
In this article we will look at how the disease develops, what treatment methods are available today, how complications of otitis manifest themselves and how to avoid them.
Types of disease
Inflammation that occurs in the organ of hearing can be chronic or acute. In acute cases of otitis, the disease lasts for up to three weeks, in chronic cases - more than three months. The chronic process starts when treatment of the acute form of otitis was not carried out or was not carried out at the proper level. There is also an intermediate form - subacute, when the duration of the disease ranges from three weeks to three months.
The human hearing organ is divided into three parts: the outer, middle and inner ear. Otitis may appear in each of these areas. Based on the location of the inflammation, acute otitis media is distinguished, and inflammation of the inner ear, otherwise known as labyrinthitis.
External manifestations of inflammation, in turn, are divided into limited, manifesting mainly in the form of a boil of the auricle, and diffuse otitis media. With diffuse otitis, a significant area of the outer ear is affected.
Acute inflammation of the middle ear involves the tympanic cavity of the ear, the auditory (Eustachian) tube and the mastoid process. This type of hearing disease is the most common.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
The disease of the internal part is called labyrinthitis (this part of the ear is called the labyrinth because of the similarity of its shape to the cochlea). As a rule, inflammation covers the internal part if the treatment of inflammatory disease of the middle ear was carried out late or the treatment for otitis media was chosen incorrectly.
Based on the causes of occurrence, infectious otitis media is distinguished, caused by various pathogens, and non-infectious (for example, arising due to exposure to allergens or ear injuries).
Otitis in acute form can occur in catarrhal (without the formation of secretion in the ear cavity), exudative (with the formation of fluid in the tympanic cavity) and purulent (with the presence of purulent masses) forms.
Causes
Acute purulent inflammation of the middle ear is a consequence of the penetration of pathogenic microflora into it and its activation against the background of a decrease in the body’s own defenses.
Often the infection enters the middle part of the hearing organ through the inflamed auditory tube connecting the nasopharynx to the ear. With sinusitis, sinusitis, proliferation of adenoid vegetations, tonsillitis and other ENT diagnoses, pathogenic microflora enters the auditory tube (for example, with sharp blowing of the nose), it becomes inflamed - eustachitis develops. If treatment was ignored or was ineffective, pathogenic organisms enter the ear through the auditory tube. This is the first variant of infection.
The second way is through a rupture in the eardrum or damage in the mastoid process (the area of the temporal bone associated with the middle ear). Otitis of this etiology is called traumatic.
A rarer route is through the blood, when during infectious diseases, for example, scarlet fever or measles, pathogenic flora spreads through the bloodstream and enters the hearing organ.
The disease develops due to decreased immunity. Factors provoking this may be:
- problems with the endocrine system;
- lack of vitamins;
- bad habits;
- diseases of the ENT organs;
- diabetes;
- frequent entry of water into the ear (local immunity decreases).
Acute otitis media of the middle ear: what causes inflammation?
The inflammatory process is always caused by pathogenic microorganisms, which means that the prerequisites for their activation must be present in the body. The causes of otitis media are:
- hypothermia;
- diseases caused by infection (flu, ARVI, measles);
- inflammatory processes of the ENT organs (the tympanic cavity is connected to the nasopharynx via the Eustachian tube, it is not surprising that the infection from the nasopharynx easily penetrates into the middle ear);
- improper nose blowing;
- hypertrophy of adenoid vegetations;
- rhinitis, sinusitis;
- allergic reactions;
- deviated nasal septum;
- foreign object in the ear;
- damage to the hearing organ.
Classification of the disease according to the nature of its course.
There are many classifications of diagnosis. We will dwell on a few in more detail.
Based on duration, the disease is divided into three forms: acute, subacute and chronic. The acute form lasts no more than three weeks. If the disease does not go away within three months, then we are dealing with a subacute variation of the disease. Chronic inflammation is characterized by sluggish symptoms that prevent an adult from leading a full lifestyle for more than six months in a row.
Based on the type of causative agent of the disease, the following types of disease are distinguished:
- bacterial - when the cause of infection is bacteria;
- viral - provoked by viruses;
- fungal - the causative agents are fungi;
- allergic - manifests itself against the background of the action of allergens;
- traumatic - due to damage to the hearing organ (more often occurs when improperly manipulating a cotton swab when cleaning the ears or a pressure drop during diving or air travel).
There is an exudative type of disease, when fluid is released from the ear cavity, catarrhal (no discharge, but severe swelling is present) and purulent. Purulent otitis is accompanied by discharge from the organ of hearing and is fraught with complications.
If the inflammatory process occurs in the right ear, we talk about right-sided inflammation, if in the left ear, we talk about left-sided inflammation. The most difficult course is for bilateral ear lesions.
Outer and inner ear: causes of inflammation
Otitis externa can develop due to improper ear hygiene. If you don't take care of your ears, dirt will accumulate in them, and this is a favorable environment for the growth of bacteria. Excessive hygiene is also harmful: earwax is a natural barrier against the penetration of bacteria into the ear. If you diligently clean the ear canals every day, a person loses this barrier and opens the way for pathogens. Another mistake that leads to acute ear inflammation is cleaning the ears with sharp objects that are not intended for this (toothpicks, matches, hairpins). Such actions can lead to damage to the auricle, which in turn leads to infection entering the wounds. Another factor is dirty water that gets into the ear, which contains pathogens. “Swimmer’s ear” is another name for this type of disease.
As we have already said, inflammation of the internal region occurs due to undertreated otitis media, if due attention has not been paid to the treatment of otitis media. Bacteria can also get here from the meninges, for example, with meningitis. This type of inflammation can be caused by injuries and fractures of the skull or temporal bone.
In order to recognize the disease in time and choose the right treatment, you need to be able to identify its signs.
Structure of the human ear
The human ear consists of three sections. The outer section consists of the auricle and the auditory canal, which ends in the eardrum. The middle ear conducts sound impulses and is formed by the tympanic cavity between the opening of the temporal bone and the eardrum. The hammer, one of the sound ossicles, is attached to the eardrum. When exposed to sound waves, the hammer vibrates. These vibrations are transmitted along a chain to other sound bones: from the malleus to the incus, then to the stapes and to the inner ear.
The inner ear is located deep in the temporal bone and is a complex system of canals. Special hair cells located on the surface of the canal convert mechanical vibrations into nerve impulses, which are transmitted to the corresponding parts of the brain. Otitis can spread in different parts of the ear, so there are external, middle and internal types of pathology.
Symptoms
The acute course of the disease is characterized by a rapid onset and pronounced symptoms.
With a disease of the outer ear, a person experiences pain inside, which intensifies when pressing on it from the outside. Acute pain occurs when swallowing and chewing food. The ear itself swells and turns red. The skin of the auricle is itchy, the patient's complaints are reduced to a state of stuffiness and ringing in the ear.
In acute otitis media, the main sign of inflammation is the sudden appearance of sharp shooting pains, which become stronger by night. The pain can radiate to the temples, left or right frontal parts, to the jaw - it is very difficult to endure even for an adult, not to mention children. The following symptoms are also characteristic of acute otitis media:
Friends! Timely and correct treatment will ensure you a speedy recovery!
- fever (up to 39°C);
- tinnitus;
- hearing loss;
- lethargy, malaise, loss of appetite;
- in the exudative form, discharge comes from the ear (usually this discharge is transparent or white);
- Acute purulent otitis media is characterized by suppuration from the ear.
The main symptom of labyrinthitis is dizziness. They can last a few seconds, or they can last for several days.
If you notice one or more of the symptoms described above, you should immediately consult a doctor for treatment.
Prevention
There are no specific preventive measures to avoid suppurative otitis media. To reduce your risk of getting sick, strengthen your immune system and promptly treat any ENT infection you encounter. An important point: treatment should not only be timely, but of high quality: no self-medication, only competent assistance from an otolaryngologist. There is no need to start the disease. At an early stage, any disease is much easier to treat: in many cases, the accumulation of purulent masses in the middle ear could be easily avoided by contacting an ENT doctor in time.
If you or your loved ones are faced with hearing problems, do not waste time: make an appointment by calling +7 (495) 642-45-25 and come.
We will definitely help you!
Stages of disease development
Treatment of acute otitis lasts from one to three weeks. There are several stages in the development of the disease. But it is not at all necessary that the patient will go through all of them. If treatment for infectious otitis is started on time and the acute disease is treated by a competent ENT doctor, recovery will not take long.
So, the course of the disease is conventionally divided into several stages:
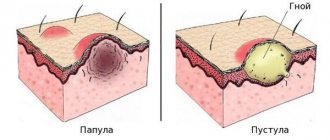
- Catarrhal. Pathogenic microorganisms begin to actively multiply, triggering an inflammatory process in the ear. At this time, catarrhal edema and inflammation are observed.
- Exudative. Inflammation leads to active formation of fluid (secret). It accumulates and pathogenic microorganisms continue to multiply here. Timely treatment at this stage will allow you to cure otitis media, avoiding complications.
- Purulent. Acute purulent inflammation is characterized by increased formation of purulent masses in the middle ear cavity. They accumulate, the patient experiences pressure from the inside. The state of congestion does not go away. This phase usually lasts from several days to several hours.
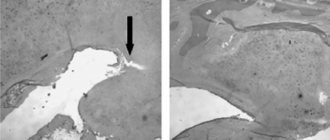
- Perforated. At this stage, accumulated pus causes a rupture of the eardrum, and purulent masses emerge from the tympanic cavity to the outside. At this moment, the patient begins to feel noticeable relief, the high temperature decreases, and the pain gradually disappears. It happens that the eardrum is unable to rupture, then the doctor manually punctures the eardrum (paracentesis) and thereby releases purulent masses out into the ear canal.
- Reparative phase - the release of pus is completed. The hole in the eardrum closes. As a rule, after proper symptomatic treatment, the patient quickly recovers.
Otitis
One of the most common diseases of the ENT organs. Every fourth patient of an otolaryngologist is a patient with acute or chronic otitis media. People of any age can get sick, but otitis media is much more common in children under 5 years of age.
Causes of otitis media
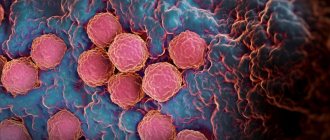
Otitis media can be caused by various pathogenic microorganisms: bacteria, viruses, fungi (otomycosis) and various microbial associations. Most often, influenza and ARVI viruses, pneumococcus and Haemophilus influenzae are the infectious agents in otitis media. Recently, there has been an increase in the number of cases of fungal otitis media.
Mechanism of development of otitis media
Normally, the pressure in the middle ear cavity is equal to atmospheric pressure. Pressure equalization and ventilation of the tympanic cavity are carried out using the Eustachian tube, which connects the tympanic cavity to the pharynx.
Some conditions (increased formation of mucus in the nasopharynx, sniffing, pressure drop when divers descend to depth, etc.) lead to the patency of the Eustachian tube being impaired. A change in pressure in the tympanic cavity leads to the fact that the cells of the mucous membrane of the middle ear cavity begin to actively produce inflammatory fluid. Increased fluid levels cause pain and hearing loss.
The infection enters the middle ear tubarically (through the Eustachian tube), transmetally (through the eardrum when it is traumatically damaged), hematogenously (through the bloodstream during scarlet fever, measles, influenza or typhus) or retrogradely (from the cranial cavity or mastoid process of the temporal bone) .
Microbes quickly multiply in the inflammatory fluid, after which otitis media becomes purulent. The pressure in the middle ear cavity rises sharply, the eardrum ruptures, and pus begins to leak out through the ear canal.
Risk factors
Otitis media rarely develops as an independent disease. In the vast majority of cases, it is a complication of diseases of other ENT organs of an inflammatory nature. There are general and local factors that increase the risk of developing otitis media.
- Local risk factors for the development of otitis media
Inflammatory and allergic diseases of the nose and nasopharynx cause swelling of the mucous membrane, leading to a deterioration in the patency of the Eustachian tubes. Microbes that enter the middle ear from the source of inflammation increase the risk of developing purulent otitis media. The group of local risk factors also includes conditions after surgical interventions in the nasopharynx and nasal cavity, accompanied by a deterioration in the patency of the Eustachian tubes.
Otitis media develops more often in children, which is due to the peculiarities of the anatomical structure of the children's middle ear. The Eustachian tube in children is narrower than in adults, therefore the likelihood of violations of its patency increases. In children, adenoids often enlarge, compressing the Eustachian tube. Children often suffer from ARVI and other colds, often cry and actively sniffle.
- Common risk factors for otitis media
The likelihood of developing otitis increases with congenital and acquired immunodeficiency conditions.
Symptoms of otitis media
- Acute otitis media
Acute otitis media is characterized by severe hyperthermia, which is accompanied by shooting pain in the ear. Children who cannot yet speak cry when the pain intensifies and calm down when it subsides.
After 1-3 days from the onset of the disease, a rupture forms in the eardrum, and suppuration begins. The patient's condition improves. Body temperature returns to normal, ear pain decreases or disappears. Subsequently, the rupture in the eardrum heals and does not cause hearing impairment.
If the disease develops unfavorably, pus may break out not outward, but inward, spreading into the cranial cavity and leading to the development of a brain abscess or meningitis. Since the disease is fraught with dangerous complications, you should consult a doctor at the first signs of acute otitis media.
- Chronic otitis media
As a rule, it is the outcome of acute purulent otitis. There are two forms of chronic suppurative otitis media, which differ in both severity and clinical course.
In 55% of cases, chronic otitis media occurs in the form of mesotympanitis, in which the inflammatory process covers the mucous membrane of the auditory tube, lower and middle parts of the tympanic cavity. The eardrum has a perforation at the bottom. Part of the membrane remains stretched.
With mesotympanitis, patients complain of decreased hearing, constant or periodic discharge of pus from the ear, and extremely rarely - dizziness and noise in the ear. Pain appears only during exacerbation of otitis media, in some cases accompanied by hyperthermia. Mesotympanitis progresses quite favorably and relatively rarely causes severe complications. The degree of hearing loss is determined by the preservation of the function of the auditory ossicles and the activity of the inflammatory process.
Chronic otitis media, which occurs in the form of purulent epitympanitis, mainly affects the epitympanic space. The perforation is located at the top of the eardrum, so natural drainage of the cavity is often insufficient. The severity of the flow is also determined by the peculiarities of the anatomical structure of this area, which is replete with winding narrow pockets.
The temporal bone is often involved in the inflammatory process, and the pus becomes foul-smelling. Patients complain of a feeling of pressure in the ear, periodic pain in the temporal region, and sometimes dizziness. This form of chronic otitis media is usually accompanied by a sharp decrease in hearing.
Both forms of chronic otitis media can occur with a predominance of certain pathological processes.
Chronic catarrhal otitis media can develop with chronic eustachitis, after suffering scarlet fever or acute otitis. Sometimes it is of an allergic nature. In the absence of suppuration, it proceeds quite favorably.
Chronic purulent otitis media is usually the outcome of a protracted acute process and develops against a background of decreased immunity. With good drainage of the tympanic cavity, purulence from the ear is sometimes not accompanied by other symptoms. The erased clinical symptoms lead to the fact that patients rarely seek help. The purulent process tends to spread gradually and can affect the auditory ossicles, periosteum, surrounding bone structures and labyrinth.
Acute and chronic purulent otitis media can be complicated by the development of chronic adhesive otitis media. With adhesive otitis media, adhesions actively form in the tympanic cavity, leading to hearing loss. Adhesive otitis often has few symptoms, and patients do not associate heavy sweats, chills and hyperthermia that appear during an exacerbation with ear disease. With adhesive otitis, complications may develop.
Complications of otitis media
Acute otitis media can be complicated by mastoiditis (inflammation of the mastoid process of the temporal bone), brain abscess, labyrinthitis (inflammation of the inner ear), meningitis, cerebral sinus thrombosis and sepsis. With purulent epitympanitis, cholestetoma often occurs - a tumor formation consisting of decay products of the epidermis. Cholestetomas destroy the temporal bone, forming granulations and polyps.
Chronic otitis media can cause damage to the facial nerve passing through the tympanic cavity. Neuritis of the facial nerve is accompanied by flattening of the nasolabial fold, drooping of the corner of the mouth and lagophthalmos (the eye on the affected side does not close). With chronic otitis media (purulent epitympanitis), as with acute otitis, labyrinthitis, meningitis or meningoencephalitis, brain abscess, sinus thrombosis and epidural abscess can develop.
Diagnosis of otitis media
The diagnosis of acute otitis media is based on medical history, otoscopy results and characteristic symptoms (general intoxication, ear pain, suppuration). To determine the sensitivity of the microflora, culture of the discharge from the ear is performed.
In case of chronic otitis media, to assess the condition of the bone structures, in addition to the listed studies, radiography of the temporal bone is performed. Otoscopy in chronic otitis reveals clouding and sharp retraction of the eardrum. The hammer handle appears shortened. The location of the perforation is determined by the shape of the otitis media.
Treatment of otitis media
- Treatment of acute otitis media
Patients with acute otitis media are recommended to rest in bed, undergo antibacterial therapy, and in case of hyperthermia, antipyretics are prescribed. Physiotherapy (UHF, Sollux) and warming compresses are used locally. To reduce pain, warm 96% alcohol is instilled into the ear (only until pus appears). If the tympanic cavity does not drain on its own within the first three days, dissection of the eardrum is indicated. In cases where hearing loss persists after scarring of the eardrum, blowing, UHF and pneumatic massage are prescribed.
- Treatment of chronic otitis media
The primary task is to ensure sufficient drainage of the tympanic cavity. To do this, polyps and granulations are removed from the middle ear cavity. The cavity is washed and proteolytic enzymes are introduced into it. The patient is prescribed sulfonamides and antibiotics, immunity is corrected, and foci of infection in the ENT organs are sanitized. If allergic otitis is suspected, antihistamines are used. Electrophoresis and microwave therapy are used locally.
If there is no effect, anthrodrainage is performed (a hole is formed in the area of the mastoid process of the temporal bone and followed by drainage). For cholesteatomas, the spread of the process to the bone and internal structures, surgical removal of the source of inflammation is indicated. If possible, sound-conducting structures are preserved; if not, tympanoplasty is performed. If the tympanic ring is intact, it is possible to restore the eardrum (myringoplasty).
Prevention of otitis media
Preventive measures include normalization of immune status, prevention of acute respiratory viral infections and other infectious diseases of the ENT organs. Patients with chronic otitis should protect the ear canal from hypothermia and water ingress.
Complications and preventive measures
As a rule, if you start treating the disease on time, treatment of acute purulent otitis, exudative or inflammation of any other kind, you can avoid any complications.
However, if treatment is not carried out and the disease progresses, the diagnosis can become chronic. The most serious consequences are: meningitis, encephalitis, brain abscess, facial neuritis, hearing loss. But these dangerous conditions can only appear when patients persistently neglect treatment for otitis media.
Preventive measures include the fight against existing foci of inflammation in the body, competent and timely treatment of ENT diseases, proper ear hygiene and, of course, strengthening the immune system.
Physiotherapy for acute purulent otitis media
An important stage in the treatment of the disease, which enhances the effect of drug therapy and accelerates the recovery process, are physiotherapeutic procedures.
For acute purulent otitis, the following types of physiotherapy are effective:
- infrared laser therapy (reduces inflammation and relieves swelling of tissues);
- vibroacoustic therapy (improves blood and lymph flow, providing a good therapeutic effect for inflammation of the middle ear);
- ultraviolet irradiation (has a bactericidal effect);
- ultrasonic medicinal irrigation (has an anti-inflammatory effect);
- photodynamic therapy (helps relieve inflammation);
- ultrasound therapy (promotes deeper penetration of medicinal ointment, relieving inflammation and swelling of tissues);
- infrared laser exposure (stops the inflammatory process).
Which procedures should be used and how many sessions will be needed is determined by the ENT doctor, based on the patient’s condition.
Carrying out treatment
It is much easier to cure acute otitis media if treatment for the disease begins as early as possible. Treatment should be carried out under the supervision of an otolaryngologist. Complex treatment includes the following activities:
- for acute pain, taking analgesics is indicated to relieve pain;
- to bring down the temperature you need to take antipyretic drugs;
- in difficult cases, antibiotic treatment is carried out;
- local treatment consists of using special ear drops, which are prescribed individually in each case. Self-selection of drops, as well as antibacterial drugs, is fraught with dangerous consequences for health.
- Antihistamines help relieve swelling;
- a good effect is achieved during physiotherapeutic procedures;
- surgical intervention: opening of the eardrum (paracentesis) is carried out if spontaneous rupture has not occurred.
All ENT doctor’s prescriptions must be followed in full: after all, following treatment recommendations is the key to a quick recovery.
Treatment in our clinic.
Dear friends! Please do not forget that if you do not seek help in a timely manner, you will advance the disease and may cause the inflammatory process to become chronic. If the problem of chronic or acute otitis is not addressed in time, serious complications may occur (for example, brain abscess, meningitis or encephalitis).
Our profile is the treatment of ENT diseases, and otitis media is one of them. Our clinic is known for its proprietary treatment methods. We work with the most modern equipment, and our doctors are graduates of the best medical universities in the country with extensive experience.
Please come to us! We will help you effectively cope with your problem and will definitely tell you what measures should be taken to prevent otitis media in order to avoid unpleasant symptoms in the future.
We will always be happy to help you! You are welcome!
What not to do during treatment
Some patients are overly self-confident and believe that a disease such as otitis media can be easily cured with the help of folk remedies and “grandmother’s” recipes. A wide variety of methods are used. This is a huge misconception!
The first mistake is that no foreign objects should be placed in the ear canal. Some are trying to use phytocandles, others, for example, geranium leaves. Such measures are fraught with the fact that leftover leaves may get stuck in the ear, which will provoke increased inflammation.
The second mistake is the use of heat and warming compresses for the purulent form of the disease. Some people replace compresses with a heating pad. At this stage of the disease, thermal heating will only increase the proliferation of bacteria.
The third mistake is trying to instill various oils or variations of alcohol into the ears. If during such treatment a perforation of the eardrum occurs, such instillations will not only cause pain, but will also cause scarring in the middle ear and eardrum.
Diagnostics
For an experienced otolaryngologist, diagnosing the disease is not difficult. When making a diagnosis, the ENT doctor relies on the patient’s complaints and the results of otoscopy (examination of the hearing organ). The patient may be referred for a number of laboratory tests that will confirm or refute the presence of inflammation. To assess the degree of hearing impairment, audiometry or tuning fork testing is performed. To assess the condition of the components of the middle ear, tympanometry is performed. In severe cases, the patient is sent for X-ray, CT, MRI.
What is otitis media and how to recognize it
Traditional symptoms of otitis media are:
- fairly severe ear pain (most often described as shooting), may be accompanied by tinnitus, hearing loss
- increase in body temperature
- on days 1-3 of the disease, purulent discharge from the ear cavity may be observed (after this the patient’s condition usually improves, the pain goes away, and the temperature subsides)
These symptoms indicate an inflammatory process occurring in the patient’s ear. Otitis media is caused by pathogenic microorganisms: pneumococci, streptococci, staphylococci, hemophilus influenzae and others. In a normal state, these bacteria are always found on the skin and mucous membranes of a person, but due to certain factors they can multiply excessively and become more active, causing the development of inflammation.
These factors include:
- hypothermia
- weak immunity
- inflammatory processes in other ENT organs and penetration of infection from there into the ear cavity
- presence of infectious diseases (ARVI, influenza, measles)
- diseases of the nose, sinuses and septum - rhinitis, sinusitis, deviated septum, adenoids
- hearing injuries
- presence of a foreign object in the ear cavity
- allergy to something
Sometimes otitis media (especially in children) can be accompanied by a seemingly paradoxical reaction - gastrointestinal disorder: bloating, diarrhea, vomiting. This occurs because the ear cavity is connected to the gastrointestinal tract by one nerve. That is why diseases of the stomach or intestines in young children should not be avoided without examination by an ENT doctor.
It has been established that preschool children are most prone to otitis media. Statistics say that the peak of diseases (about 80% of patients) occurs before the age of 3 years. However, adults also suffer from otitis media, so it is necessary to be vigilant at any age.
Labyrinthitis
It develops as a result of a bacterial or viral infection of the inner ear, and is often a complication of otitis media and meningitis.
The disease manifests itself as severe dizziness, often with nausea and vomiting, as well as hearing loss and noise in the ear. Differential diagnosis of brain diseases in order to exclude tumors and strokes is carried out using MRI and computed tomography, videonystagmography, and audiometry are performed.
Treatment of labyrinthitis involves eliminating symptoms - eliminating nausea and vomiting, reducing inflammation, relieving anxiety, etc. If the inflammation is bacterial, antibiotics are prescribed. Vestibular rehabilitation, which begins as early as possible, and hearing aids for severe hearing loss are important.
Inflammation of the outer ear - what causes it?
Inflammation of the outer ear is caused by various microorganisms. Pseudomonas (Pseudomonas aeruginosa) and Staphylococcus aureus (Staphylococcus aureus)
are most often responsible for bacterial infections , while infections of viral origin correspond to herpes simplex virus or varicella zoster virus. Candida and Aspergillus are the dominant microorganisms in cases of fungal infections.
Some dermatoses, including psoriasis, lupus erythematosus and atopic dermatitis, can also cause otitis externa.
Doctors also mention a localized inflammation of the ear canal called a boil, which people with diabetes or severe malnutrition are more prone to. This type of infection is mainly caused by Staphylococcus aureus and Streptococcus species.