The Eustachian tube is a canal in the human middle ear that connects the nasopharynx and the tympanic cavity. Normally he:
- drains mucous membranes, removing exudate and transudate;
- provides air exchange between the cavity and the nasopharynx, expanding when swallowing;
- produces a bactericidal secretion.
If one or all functions are disrupted, eustachitis occurs (other names are tubotympanitis, tubootitis, salpingootitis) - an inflammatory process that affects the mucous membrane of the auditory canal and often develops into otitis media.
Causes
Unilateral or bilateral eustachitis is a consequence of low air exchange in the tympanic cavity caused by certain factors. This:
Complications after:
- ARVI;
- measles, whooping cough, influenza;
- tonsillitis;
- sinusitis.
Structural pathologies, neoplasms:
- overgrowth of adenoids;
- nasopharyngeal polyps;
- irregular shape of the nasal septum;
- enlargement of the posterior ends of the inferior turbinates (hypertrophy).
Medical procedures:
- nasal tamponade in the treatment of bleeding;
- condition after operations on ENT organs.
Sudden changes in pressure:
- in divers, divers during a rapid dive or ascent (mareotite);
- on an airplane during climb and landing (aerootitis).
Allergic reactions with constant inflammation of the mucous membranes (allergic eustacheitis becomes a consequence of vasomotor rhinitis).
Regardless of the cause, the mechanism of occurrence of the disease is the same:
- the tympanic cavity is not sufficiently ventilated;
- the mucous membrane of the Eustachian tube absorbs air;
- pressure in the middle ear decreases;
- transudate (fluid) is formed, inflammation of the auditory tube develops, then otitis media occurs.
How long does it take to treat eustachitis? The process often occurs in an acute form and goes away within a week, but without proper attention it can become chronic. In order to cope with the disease as soon as possible, it is important to contact an otolaryngologist in time for diagnosis and treatment.
Clinical picture
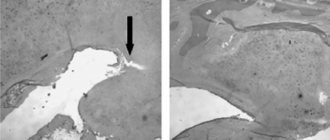
It is interesting that patients with this disease, as a rule, do not experience pain, but complain of periodic or constant ear congestion, annoying tinnitus, and in some cases a feeling of fluid transfusion or rolling. When performing otoscopy, otomicroscopy, or video microscopy, it is clearly visible that the eardrum is retracted and has a cloudy tint. Quite often, calcareous plaques are visible, which shine through the fibrous and epidermal layers of the eardrum (which confirms myringosclerosis). With idiopathic hematotympanum, which is a type of exudative otitis, the eardrum is blue. In chronic tubo-otitis, there is a conductive nature of hearing loss caused by obstruction of the auditory tubes. But at the same time, no disturbances of the vestibular apparatus are observed. Quite often, with recurrent tubootitis, cicatricial obliteration of the tympanic cavity occurs, which means complete immobility of the auditory ossicles and tympanic membrane, which are soldered to the medial wall.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
In children
The disease usually results from acute respiratory viral infections and upper respiratory tract infections. The younger the child, the more often bilateral eustachitis is diagnosed. Older children suffer from unilateral damage to the auditory tube. Without treatment, painful otitis media can quickly develop. The temperature is normal or slightly elevated, but the child gets tired quickly and eats poorly.
With inflammation of the Eustachian tube, children complain of:
- slight periodic congestion in one or both ears;
- mild pain;
- nausea, dizziness, noise;
- balance disorders;
- the feeling of an “echo” of your own voice in your head, its unusual volume;
- feeling as if water is pouring in the ear or ears.
Infants react to poor health with low-grade fever, tearfulness, refusal to eat, lethargy, poor sleep at night, and regurgitation.
Treatment
The treatment process includes the following significant stages:
- eliminating the causes that caused the disease and disrupted the functioning of the auditory tubes;
- hearing restoration;
- carrying out measures aimed at preventing the development of persistent hearing loss;
- If conservative treatment does not give the desired effect, it is necessary to undergo a timely surgical operation - eardrum bypass.
For conservative treatment, antibiotics, vasoconstrictors, as well as hyponsitizing agents, proteolytic enzymes, pneumomassage of the eardrums, blowing of the auditory tubes, aerosol therapy using an elastic catheter, catheterization of the auditory tubes, laser therapy, ultraviolet irradiation, and vibroacoustic therapy sessions are used.
In adults
Adult patients are characterized by left- or right-sided eustachitis affecting one side without fever, but with a complex of unpleasant symptoms. Patients suffer from:
- congestion in the ears, decreased hearing (low frequencies are almost not perceived);
- autophony (loud distorted perception of one’s own voice in the form of an echo);
- sensation of fluid in the ear;
- headaches or earaches.
Improvement occurs briefly when chewing or after swallowing saliva, food, or when tilting the head due to a short-term opening of the Eustachian tube and a change in fluid level.
Causes of eustachitis
The most common cause of eustachitis is respiratory infections of the nasopharynx, which can be viral or bacterial. The localization of infections is not of fundamental importance; rhinitis, pharyngitis, tonsillitis, adenoiditis, and sinusitis are equally likely to cause eustachitis and tubo-otitis. These can be acute processes or chronic, becoming a persistent focus of infection. In the latter case, eustacheitis also develops chronic; it often leads to irreversible hearing loss.
Most often, infectious eustachitis is caused by respiratory viruses, but specific microflora (chlamydia, syphilis, tuberculosis) and the fungal nature of the disease cannot be excluded. Inflammation can also be aseptic, for example, with allergic rhinitis or hay fever. If there are organic obstacles to normal air circulation (deviated nasal septum, neoplasms, developmental abnormalities), the development of eustachitis is also possible.
Diagnostics
Since the symptoms of the disease are sometimes disguised as other ailments, a doctor is needed for an accurate diagnosis. Treatment of eustachitis in adults and children should be carried out exclusively by specialists after the diagnosis has been clarified.
To confirm the disease the following are used:
1. Otoscopy.
The doctor uses an otoscope to examine the outer ear, ear canal, and eardrum. The examination reveals characteristic signs of tubootitis:
- the eardrum is cloudy and retracted;
- the location of structural components is disrupted;
- the auditory canal is narrowed.
2. Audiometry.
Measuring hearing parameters with an electroacoustic audiometer and speech tests. With tubo-otitis, a decrease in perception of up to 20-35 dB is detected.
3. Laboratory examination of discharge (smear).
It is done to determine the causative agents of infection or the allergic nature of the disease.
Diagnosis of tubootitis
Diagnosis of tubo-otitis is based on the following data:
- Patient complaints and medical history (ear congestion, pain, etc.).
- Visual inspection and endoscopic examination of the eardrum.
- Endoscopic examination of the nasopharynx - the doctor pays special attention to the condition of the mouths of the auditory tubes.
- Tuning fork tests.
Often, tubo-otitis occurs without significant symptoms, especially in children. In addition, it is not always possible to visually determine a violation of the mobility of the eardrum. Therefore, instrumental methods are very important:
- classic tympanogram and ETF test - a special device shows how well the eardrum moves. Based on these data, conclusions can be drawn about the condition of the auditory tube.
- For a more precise diagnosis of hearing loss, an audiogram is used.
To identify the cause of tubo-otitis, the doctor may prescribe the following tests:
- Blood tests (general and biochemical).
- Laboratory examination of a swab from the ear, nose or throat.
- Allergy tests.
Computed tomography of the temporal bones, paranasal sinuses and nasopharynx to exclude or confirm a violation of the ventilation of the auditory tubes caused by anatomical features.
Acute eustachitis
An acute form of inflammation is a common complication of viruses and infections of the nasopharynx. With insufficient treatment, inflammation continues in the auditory tube. Children often experience pain in both ears; adolescents and adults suffer from unilateral manifestations. When asked how long it takes to treat eustachitis, doctors answer: adequate measures can get rid of it in 5-7 days. If:
- no treatment;
- therapy is insufficient or prescribed incorrectly;
- the course is not completed;
- there are pathologies in the nasopharynx or nasal cavities;
- there is constant allergic inflammation of the mucous membrane
there is a high probability of a prolonged course of tubo-otitis and its chronicity.
Symptoms of tubootitis
The acute form of inflammation (swelling without membrane deformation) has more pronounced symptoms, may be accompanied by pain, and is cured in 4-5 days. In the absence of timely treatment, it often becomes chronic.
Symptoms of acute tubo-otitis:
- stuffy ear effect;
- autophony (a person hears his own voice louder than usual);
- a feeling of flowing liquid when turning the head or tilting (sometimes the quality of hearing may change with different actions);
- deterioration of hearing function (up to 30-35 dB) with loss of low frequencies;
- When swallowing, congestion disappears for a while.
Chronic tubo-otitis is characterized by deformation (retraction) of the eardrum. It manifests itself less clearly, but its symptoms are more persistent. They can only be determined by inspection. The main signs of chronic eustachitis include:
- retracted eardrum, decreased mobility;
- persistent hearing loss;
- long-term narrowing of the lumen of the auditory tube.
Complications
Over time, untreated eustacheitis causes:
- acute otitis after ARVI;
- hearing impairment;
- unpleasant sensations of echo, congestion, fluid in the ear;
- problems with coordination;
- headache.
During flights or when diving, patients with chronic eustachitis experience severe discomfort.
It is important to diagnose inflammation of the auditory canals in a child in a timely manner, since without treatment, ARVI will be complicated by catarrhal otitis. Chronic eustachitis and the changes it causes in the middle ear gradually worsen hearing.
Eustachite: what is it?
The auditory tube has a very small diameter, only 2 mm, and in children it is even smaller. With the development of inflammation, accompanied by edema, the lumen of the tube is blocked, which leads to disruption of air exchange between the middle ear and the external environment. The result is catarrhal inflammation - otitis media. Since eustachitis and otitis usually develop simultaneously, this condition is often called tubo-otitis, less often - tubotympanitis, salpingo-otitis. With long-term inflammation, catarrhal otitis media can turn into purulent, and when adhesions appear, into adhesive.
Treatment of eustachitis
For the treatment of eustacheitis in adults and children in the acute period, the following can be used:
1. Medicines to destroy infection (antiseptics, antibiotics, anti-inflammatory), relieve swelling (vasoconstrictors, antihistamines).
2. Physiotherapy to shorten the duration of the disease. UV irradiation, sessions on UHF devices, and electrical stimulation are prescribed.
3. Therapeutic manipulations - blowing out the ear (Politzer method), introducing medications directly into the ear canal through a catheter.
To eliminate allergic eustacheitis, or tubootitis, caused by pathology of the ENT organs, you should work with the root causes of the disease - allergies, deviated nasal septum, adenoid growths, etc.
At the multidisciplinary clinic "K+31", treatment of eustachitis in adults and young patients is carried out in the otolaryngology department. Specialists perform diagnostics, develop an action plan, monitor the progress of therapy and strive to prevent relapses of the disease.
Among the advantages of the medical center:
- qualified patient care on an outpatient basis or in a day hospital;
- a full range of necessary laboratory and hardware tests for diagnostics;
- drawing up a treatment regimen using drugs and physiotherapy, innovative techniques;
- if necessary, attracting doctors of other profiles;
- results in the form of recovery or attenuation of the chronic process.
For accurate diagnostics, expert-level equipment is used:
- special installation MODULA EUROPA Paris (Duo) HEINEMANN. It helps make a diagnosis and works as a device for therapeutic manipulations;
- audiometer-impedance meter for analyzing the hearing of young and adult patients.
Thanks to the professionalism of doctors and modern equipment of the department, diagnostics are performed quickly and accurately. After the first visit, the course of treatment begins.
Treatment options
The main thing in the treatment of infectious tubo-otitis is to eliminate the cause of the disease, stop the inflammatory process in the mucous membrane of the auditory tube and, if necessary, take measures aimed at strengthening the immune system.
Elimination of the inflammatory process.
In some cases, to treat eustachitis, it is necessary to eliminate the source of chronic infection in the nasopharynx - adenoids or tonsils - and prescribe a course of antibiotic treatment. Only a doctor can do this. If you suspect tubo-otitis, it is very important to immediately contact a specialist.
Elimination of swelling of the mucous membrane of the auditory tube and tympanic cavity.
The use of vasoconstrictor drugs in the form of nasal drops and sprays, as well as antihistamines (that is, blocking receptors that can trigger an allergic reaction) helps eliminate swelling of the mucous membrane of the auditory tube. In some cases, for greater effectiveness of treatment of eustachitis, it is necessary to relieve swelling in the nasal cavity, paranasal sinuses and nasopharynx. For this purpose, preparations based on sea water and xylometazoline can be used. Xylometazoline constricts blood vessels, reducing swelling of the mucous membrane, and sea water moisturizes the mucous membrane, restores and protects it and normalizes the production of nasal mucus. In addition, the presence of sea water in the composition of the drug for nasal congestion smooths out the negative effect of the vasoconstrictor on the mucous membrane, which occurs with prolonged use - the appearance of dryness and a burning sensation. The innovative drug Rinomaris®, created on the basis of xylometazoline and sea water, helps reduce swelling of the mucous membrane and thin the nasal mucus, thus preventing the further development and proliferation of pathogenic microorganisms.
Restoring the patency and functions of the auditory tube.
If you notice signs of tubo-otitis, you need to contact an ENT doctor who can make a diagnosis and prescribe the correct treatment. To improve the patency of the Eustachian tube, the doctor may administer adrenaline or hydrocortisone through the catheter. If any structural defects are identified that prevent full nasal breathing (deviated nasal septum, benign neoplasms in the nasopharynx, enlarged nasal turbinates, etc.), if necessary, they are surgically corrected.
Improved ventilation and drainage of the auditory tube.
The doctor may prescribe pneumomassage of the eardrum or the use of special enzymes that dilute the fluid that accumulates in the auditory tube and tympanic cavity during eustachitis.
Increasing local immunity.
For this purpose, physiotherapeutic procedures are used: UHF, microwave and laser therapy, UV irradiation, electrical stimulation. There are contraindications! Before the procedures, you must consult with an ENT doctor.
Elimination of concomitant inflammatory processes in the respiratory tract.
Elimination of diseases such as adenoiditis (enlarged nasopharyngeal tonsils), rhinitis (runny nose), rhinopharyngitis (inflammation of the nasal mucosa caused by infection), pharyngitis (inflammation of the pharyngeal mucosa) and others should be carried out using medications prescribed by a doctor and physiotherapeutic procedures . For eustachitis of allergic origin, complex treatment of allergies and tubo-otitis is prescribed.
Treatment of tubootitis
For patients who are faced with this diagnosis, the question logically arises: “How to cure tubo-otitis at home?” Without contacting an otolaryngologist - no way! The disease requires an integrated approach, which consists of taking medications prescribed by an ENT doctor at home and performing physiotherapeutic procedures in an ENT clinic.
The patient may be prescribed the following medications:
- antibiotics for oral administration (for example, Amoxiclav, Azithromycin);
- antibacterial ear drops for eustachitis and tubootitis (Otofa, Normax).
Important: both oral antibiotics and drops should be prescribed only as prescribed by an ENT doctor. The drug for treatment and its dosage are determined only by the doctor after examining the patient.
- vasoconstrictor drugs for the nose (“Otrivin”, “Nazivin”, “Galazolin”, for children, respectively, children’s drops);
- antihistamines for the allergic form of the disease (Zyrtec, Zodak, Suprastin);
- immunomodulators (for example, “Bronchomunal”);
- Ear drops of the Otipax type for tubo-otitis are used to relieve pain and relieve inflammation in the ear.
Effective for tubo-otitis are procedures carried out in an ENT clinic, for example, blowing out the auditory tubes using an ENT machine. It is carried out in combination with the procedure - pneumomassage of the eardrum. Both manipulations reduce and relieve persistent ear congestion. Another complex but very effective procedure is catheterization of the auditory tube using a Hartmann cannula. Catheterization for tubo-otitis requires a lot of experience and skill of an ENT doctor, but brings a huge therapeutic effect.
Physiotherapy in the ENT clinic also helps speed up the healing process: infrared laser therapy, vibroacoustic therapy, ultraviolet irradiation, ultrasound therapy, photodynamic therapy, magnetotherapy.
Symptoms of eustachitis
The main signs of inflammation of the auditory tube are a feeling of water in the ears and hearing loss. General malaise with headache and fever is also possible.
Earache
Infectious eustachitis usually occurs without pain. However, if the cause of tubo-otitis is a pressure difference, pressing or bursting pain is quite possible.
Hearing problems
Sounds come in unclearly due to congestion, and are also drowned out by tinnitus. The picture is complemented by autophony - the patient hears an echo of his own voice.
Heaviness in the head
Heaviness in the head is one of the manifestations of chronic eustachitis. The cause is an atrophic change in the structure of the eardrum.
Improvement seen with muscle contraction
Yawning or swallowing saliva gives relief for a few seconds: hearing improves, the feeling of stuffiness and water in the ear disappears. However, symptoms return quickly.
Symptoms of tubootitis
Most often, patients complain of the following manifestations:
- Hearing impairment;
- Ear congestion;
- Autophony (hears oneself);
- Whistling;
- Headache;
- When moving the head, it feels like there is liquid inside.
Other symptoms (more common in children):
- Fever;
- Balance imbalance;
- Nausea.
When swallowing or yawning, the patient begins to hear better. This is due to a short-term dilation of the Eustachian tube.
There are 2 types of tubo-otitis: chronic and acute. Their symptoms are no different. The only difference between the two types of disease is that chronic tubo-otitis is more protracted, and hearing deteriorates more severely after it.
When should you see a doctor?
Whether the treatment is infectious or the treatment of allergic tubo-otitis, you need to start as quickly as possible if you notice that your hearing is decreasing and your ears are constantly “stuffed up”. This is a rather dangerous inflammation that cannot be dealt with without medical help. Long-term dysfunction of the eustachian tube can lead to adhesions between the auditory ossicles (stapes, malleus and incus), which are involved in sound transmission. This is fraught with permanent hearing loss. The disease can also cause pathologies of the auditory nerve and lead to sensorineural hearing loss. If inflammation leads to the accumulation of purulent masses in the ear, acute purulent otitis media may develop. This diagnosis also has a lot of complications: at a minimum, in the absence of full-fledged therapy, it can develop into chronic otitis in a child and in an adult patient, and at maximum, lead to meningitis, sepsis or complete deafness. Therefore, the disease must be diagnosed as early as possible, as soon as the slightest discomfort appears and does not go away.
Forecast and prevention of eustachitis
With adequate treatment, acute eustachitis resolves within a few days. However, it can transform into adhesive otitis media or chronic eustachitis. This can occur if there are concomitant diseases that impair the ventilation of the auditory tube.
Prevention of eustachitis involves timely treatment of allergic and infectious diseases of the nasopharynx. Also, for respiratory diseases that are accompanied by nasal congestion, it is necessary to use decongestants (antihistamines, nasal vasoconstrictor drops).