Leukopenia is a pathological condition that is characterized by a decrease in leukocytes in the blood (less than 4 x 109/l), including all cells of the leukocyte formula (neutrophils, monocytes, lymphocytes, basophils). Such changes may be reactive, or may be indicators of a malfunction of the bone marrow, which produces white blood cells.
This condition is caused by massive destruction of young blood cells and a decrease in the formation of mature leukocytes, which are the basis for the proper functioning of the immune system.
| Leukocytes are protective blood cells that are an integral part of the immune system. They “destroy” foreign elements, produce biologically active substances, and take part in inflammatory processes. · Therefore, an imbalance of leukocytes leads to a decrease in the body’s defenses, thereby increasing its vulnerability to various types of infections. The severity of the pathological process depends on the rate of reduction of leukocytes in the blood. |
In some clinically healthy people, leukopenia is considered normal.
However, in most cases, a decrease in leukocytes is a pathological condition that develops against the background of primary or secondary causes.
By origin they are:
- Endogenous (hormonal imbalance, inflammatory process in the body, genetic predisposition).
- Exogenous (bacteria, viruses, fungi, parasites).
Infectious and non-infectious.
Classification
Low levels of white blood cells can occur in completely healthy individuals - constitutional harmless leukopenia occurs in approximately 2-5% of people. Based on their origin, pathological leukopenias are divided into:
- Hereditary (primary)
. The low white blood cell count is caused by genetically determined disorders in the formation and maturation of cells in the red bone marrow. These include Kostman neutropenia, hereditary neutropenia of the autosomal dominant type, etc. - Acquired (secondary)
. More common option. Leukopenia develops as a result of the action of ionizing radiation, the adverse effect of drugs, biological agents (bacteria, viruses) or factors of immune autoaggression.
According to pathogenesis (mechanism of development), leukopenias that arise as a result of:
- Disturbances in the flow of leukocytes into the blood from the bone marrow.
The development of leukopenia is caused by damage to hematopoietic cells or ineffective leukopoiesis due to defects in mitosis and leukocyte maturation. It is observed with long-term use of cytostatic drugs, exposure to ionizing radiation, genetic diseases, severe deficiency of vitamin B12, folic acid. - Redistribution of leukocytes.
There is a change in the ratio between the circulating and parietal pool of white blood cells as a result of their accumulation in the dilated capillaries of the depot organs. Occurs in states of shock. - Reducing the residence time in the blood.
The time of presence of leukocytes in the blood may decrease due to their destruction by antibodies (in autoimmune pathologies), toxic factors (in severe infections), and overly activated macrophages (in hypersplenism). Increased excretion of white blood cells can be observed during purulent processes - cholangitis, endometritis.
Depending on the type of cells of the leukocyte series, the following types of leukopenia are distinguished:
- Neutropenia.
The decrease in the content of neutrophils is less than 47% of the total number of leukocytes. The most common type of leukopenia. Occurs with viral and bacterial infections, toxic effects of medications. Hereditary forms of neutropenia are also possible. - Lymphopenia.
Decrease in lymphocyte level below 19%. Characteristic of viral infections, collagenosis, granulomatous processes. - Eosinopenia.
The eosinophil content is less than 1%. It is observed with excess production of adrenal hormones (Cushing's disease/syndrome). Eosinopenia is an indicator of an unfavorable prognosis in septic processes. - Monocytopenia.
The indicators of monocytes in the leukocyte formula drop below 2%. Occurs in acute infections and long-term use of glucocorticoids. - Agranulocytosis.
A rare severe life-threatening condition characterized by complete or almost complete disappearance of neutrophils in the blood (below 0.75x10^9/l). It is observed when taking myelotoxic drugs (cytostatics, thyreostatics, some NSAIDs), or exposure to radiation.
Leukopenia is determined in a general blood test
Revealing
The syndrome may not have pronounced symptoms. If this form is mild, they will not exist at all. If the number of white blood cells decreases significantly, infectious pathologies will begin to develop.
One of the symptoms of the syndrome is a feverish state. This is due to infectious effects, the body’s reaction to chemotherapy drugs taken, or a tumor.
Among the symptoms of the syndrome:
- Feeling weak;
- State of dizziness;
- The mucous membranes bleed;
- Hemorrhages appear on the skin, some others.
Serious infectious consequences include sepsis and septic shock.
A low white blood cell count is detected by a blood test.
Pulmonary hemorrhage
Causes of leukopenia
Infections
One of the most common causes of leukopenia is viral and generalized bacterial infections. The pathogenesis of a decrease in the level of leukocytes can be different - direct damage to cells by lymphotropic viruses (HIV, Varicella-Zoster, measles), suppression of formation in the bone marrow, increased loss with exudation.
- Viral infections.
Leukopenia develops mainly due to a decrease in the content of lymphocytes (lymphopenia). With infectious mononucleosis, influenza, and viral hepatitis, leukocytes decrease slightly and quickly return to normal after recovery. With HIV infection, the level of lymphocytes often reaches zero during the AIDS stage. Even after treatment, white blood cell counts may remain low, as HIV drugs themselves can cause leukopenia. - Bacterial infections.
Leukopenia occurs only in severe generalized infections (meningococcemia, rickettsial infections, peritonitis). A drop in the number of leukocytes is one of the criteria for diagnosing a septic condition and systemic inflammatory response syndrome. Neutropenia is mainly observed, its degree correlates with the severity of the disease. Regression occurs almost immediately after antibiotic therapy.
Taking medications
A wide range of drugs can lead to the development of leukopenia. There are two main mechanisms of drug-induced leukopenia: toxic damage to the bone marrow, leading to impaired hematopoiesis, and the formation of immune complexes, which results in the production of antibodies that attack the body’s own leukocytes.
Leukopenia occurs on average 15 days from the start of taking the medicine. The severity can vary from a slight decrease in the number of white blood cells to agranulocytosis. Due to the defeat of all 3 germs of hematopoiesis, a combination with anemia and thrombocytopenia (pancytopenia) is often found. In most cases, discontinuation of the drug is sufficient. If agranulocytosis develops, the use of colony-stimulating factors may be required. Medicines that most often cause leukopenia:
- Cytostatics
: cyclophosphamide, clopambucil, methotrexate. - Thyreostatics
: propylthiouracil, mercazolil. - Non-steroidal anti-inflammatory drugs
: analgin, amidopyrine. - Antibacterial agents
: chloramphenicol, sulfonamides. - Anti-inflammatory drugs
: D-Penicillamine, sulfasalazine. - Antipsychotic drugs (neuroleptics)
: chlorpromazine, chlorpromazine. - Anticonvulsants
: carbamazepine, diazepam.
Autoimmune inflammatory diseases
Leukopenia can be caused by autoimmune diseases. In these cases, lymphocytes and neutrophils are predominantly reduced. There are two main pathogenetic mechanisms of autoimmune leukopenia - the formation of anti-leukocyte antibodies and a decrease in the expression of special proteins on the membranes of immune cells (CD55, CD59), which protect cells from cytolysis. Leukopenia is usually moderate, regresses during remission or under the influence of pathogenetic treatment. Leukopenic syndrome is characteristic of the following pathologies:
- Joint diseases
: rheumatoid arthritis, Felty's syndrome. - Diffuse connective tissue diseases (collagenoses)
: systemic lupus erythematosus, Sjogren's syndrome. - Demyelinating diseases
: multiple sclerosis. - Systemic vasculitis:
granulomatosis with polyangiitis, Takayasu nonspecific aortoarteritis. - Inflammatory bowel diseases (IBD)
: ulcerative colitis, Crohn's disease.
Blood diseases
There are several mechanisms of leukopenia in hematological pathologies - replacement of hematopoietic tissue with malignant cells, fibrous or adipose tissue, synthesis of anti-leukocyte antibodies, deficiency of certain chemical elements for granulocytopoiesis (iron, cyanocobalamin, folic acid):
- Oncohematological diseases.
Leukopenia, up to agranulocytosis, can make the debut of acute leukemia (aleukemic form) - this onset of the disease occurs in approximately 20% of cases. Almost always, blood tests additionally reveal thrombocytopenia and anemia. Leukopenia is characteristic of lymphogranulomatosis (Hodgkin's lymphoma). White blood cell levels often remain low after treatment. - Hemolytic anemia.
With autoimmune hemolytic anemia, hemoglobinopathies, hereditary microspherocytosis, moderate neutropenia is possible. It is noteworthy that a drop in leukocyte levels occurs outside of a crisis. The period of hemolytic crisis, on the contrary, is accompanied by slight leukocytosis. - Dyserythropoietic anemia.
With aplastic anemia, as well as long-term deficiency of vitamin B12 and folic acid, pancytopenia is observed due to inhibition of the functioning of all hematopoietic germs. Leukopenia in iron deficiency anemia develops only with extreme iron deficiency and is moderate in nature.
Radiation sickness
The effect of ionizing radiation adversely affects the entire human body. First and most severely affected are organs with a high rate of cellular turnover, which include the bone marrow. Under the influence of gamma rays, which have a high penetrating ability, hematopoietic stem cells lose mitotic activity.
This inevitably leads to a drop in the level of leukocytes in the blood, as well as platelets and red blood cells. In acute radiation sickness, leukopenia occurs quickly, 48-96 days after irradiation; in chronic radiation sickness, leukopenia occurs gradually, over 1 year. The severity of leukopenia directly depends on the radiation dose received. The restoration of the number of blood cells occurs slowly or does not occur at all.
Hereditary forms of leukopenia
Primary leukopenias include genetic diseases caused by mutations in genes that regulate the maturation or differentiation of leukocytes. Some mutations lead to changes in the structure of leukocyte antigens, due to which they are subject to autoimmune destruction. In the vast majority of cases, primary neutropenia occurs.
The debut occurs from the first years of life. Some of these diseases are benign in nature (cyclic neutropenia, primary immune neutropenia, lazy leukocyte syndrome, Henslen syndrome), the decrease in the number of neutrophils is insignificant, associated infections are mild, and leukopenia regresses on its own.
Other hereditary leukopenias are often accompanied by infectious complications, which often become fatal in childhood: Kostman's disease (genetically determined agranulocytosis), primary immunodeficiencies (DiGeorge syndrome, Wiskott-Aldrich syndrome), Chediak-Hegashi syndrome. In these diseases, specific treatment is required to restore normal white blood cell values.
Other reasons
- Protein fasting.
- Blood or leukocyte transfusion.
- Endocrine disorders
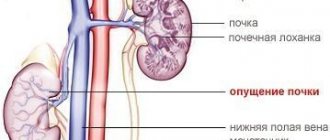
: hypothyroidism, acromegaly, hypercortisolism. - Diseases occurring with hypersplenism
: liver cirrhosis, malaria, visceral leishmaniasis. - Storage diseases
: Gaucher disease, Niemann-Pick disease.
Diagnostics
Leukopenia is detected by clinical blood testing. Due to the variety of etiological factors of this deviation, if it is detected, you should consult a general practitioner for a thorough history taking, physical examination, and additional examination:
- Blood tests.
The leukocyte formula is calculated, the concentration of inflammatory markers is determined - ESR, CRP, procalcitonin. The presence of autoantibodies (antibodies to DNA, neutrophil cytoplasm, aCCP) is studied. - Identification of infectious pathogen.
The enzyme immunoassay method identifies antibodies to pathogens (viruses, bacteria). To confirm HIV infection, immunoblotting is prescribed. Bacterial culture of blood, sputum, and urine is carried out. - Biopsy.
If leukemia is suspected, a morphological examination of the bone marrow is performed, which reveals hyperplasia of the granulocytic lineage and a large number of blast cells. To diagnose lymphomas, an aspiration biopsy of an enlarged lymph node is performed; the biopsy specimen reveals lymphocytic hypercellularity and collagen proliferation. - Genetic research.
To confirm hereditary forms of leukopenia, it is necessary to detect mutations using polymerase chain reaction and cytogenetic studies.
Examination of a blood smear under a microscope
Correction
Constitutional leukopenia does not require any intervention. If the development of this deviation is caused by a drug, its immediate discontinuation is necessary. With a pronounced decrease in leukocytes or agranulocytosis, they resort to the introduction of granulocyte colony-stimulating factor (G-CSF) or infusion of donor granulocytes. The main condition for successful therapy is treatment of the underlying pathology:
- Elimination of the pathogen.
Oseltamivir is used to treat influenza, and antiretroviral drugs (zidovudine, saquinavir) are used to combat HIV infection. For bacterial infections, antibiotics are prescribed. - Anti-inflammatory therapy.
To achieve remission of autoimmune diseases, glucocorticosteroids, immunosuppressants, and 5-aminosalicylic acid derivatives are used. - Chemotherapy.
If oncohematological pathology is confirmed, combinations of chemotherapeutic agents are prescribed - chlorambucil, vincristine, etoposide. - Bone marrow transplantation.
In case of ineffectiveness of chemotherapy for hematological malignancies, as well as in severe primary neutropenia, hematopoietic stem cell transplantation is performed.
Symptoms
Leukopenia, as a rule, is determined accidentally during a preventive study, since it does not have specific clinical symptoms.
The first signs of a decrease in leukocytes may appear when bacterial, viral or infectious complications are involved in the pathological process.
What this entails:
- Increased body temperature;
- The appearance of aphthae on the mucous membranes of the mouth;
- Increased gum bleeding;
- Pustular infections;
- Tachycardia;
- Headache;
- Anxiety;
- Pain in the left hypochondrium (associated with an enlarged spleen).
All symptoms of leukopenia must be carefully examined, so in this case, consultation with a doctor is mandatory.