Systemic lupus erythematosus is a disease that causes an immune response against the body's own cells. The causes of the pathology are not fully understood. Provoking factors contributing to the development of the disease are identified. The symptomatic picture of SLE depends on which organ it affects. A comprehensive diagnosis of the disease makes it possible to determine the location and degree of activity of the pathology. Despite the fact that systemic lupus erythematosus is currently considered an incurable disease, long-term use of medications can minimize the number of exacerbations of autoimmune pathology. In the international classification of diseases ICD-10, systemic lupus erythematosus is coded M32.
Lupus erythematosus - what is this disease?
Systemic lupus erythematosus is a chronic autoimmune disease in which the body's own cells are recognized as foreign. In this regard, an immune response develops, causing inflammatory processes in the organs. Currently, experts have not come to a consensus regarding the causes of the disease. There are a number of predisposing factors that increase the risk of developing SLE. Most often, autoimmune pathology affects females under the age of 30. Systemic lupus erythematosus is characterized by a severe course. It affects various organs and tissues. The most specific symptom of the presence of pathology is “lupus butterfly”. Due to the fact that the clinical signs of the disease are similar to other diseases, the diagnosis and treatment of SLE is delayed. Modern diagnostic tests can accurately detect the presence of systemic lupus erythematosus. Therapy for the disease is aimed at suppressing the mechanisms of its development, as well as alleviating clinical symptoms.
At the moment, systemic lupus erythematosus is an incurable disease. Thanks to constant use of medications, long-term remission is achieved. There are a number of preventive measures, the observance of which reduces the risk of exacerbation of systemic lupus erythematosus.
The Yusupov Hospital provides a full course of treatment and diagnostic measures necessary to identify this chronic autoimmune disease. The appearance of the first signs of pathology requires immediate medical attention.
Expert opinion
Author:
Anna Olegovna Pchelintseva
Rheumatologist, doctor of the highest category
Compared to the mid-20th century, modern medicine has made significant progress in the treatment of systemic lupus erythematosus. The survival rate has increased to 90–95%. It depends on the stage at which the diagnosis was made and what therapy the patient receives. In the structure of mortality, systemic lupus erythematosus does not occupy a leading position. The number of deaths varies depending on different conditions. It has been proven that women are several times more likely to suffer from SLE compared to men.
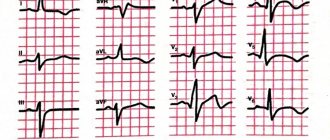
The disease is still considered incurable. However, properly selected therapy can achieve long-term remission. At the Yusupov Hospital, systemic lupus erythematosus is diagnosed using radiography, angiography, echocardiography, and ECG. A modern laboratory performs a blood test to identify markers of inflammation. In accordance with the data obtained, rheumatologists select suitable treatment. For each patient, a therapeutic plan is developed individually. The drugs are selected according to the latest European recommendations for the treatment of systemic lupus erythematosus.
Observation
A rheumatologist monitors the patient's condition throughout treatment for SLE. To monitor the effectiveness of the therapy, the doctor performs regular diagnostics and, if necessary, adjusts the treatment.
sign up for a consultation
Forecast
Despite the fact that we are talking about a chronic inflammatory autoimmune disease that affects various vital organs, the prognosis for SLE has improved significantly in recent years, primarily due to the constant improvement of diagnostic and therapeutic options.
Important! It is fundamental that treatment should always be tailored to the activity of the disease in order to avoid adverse consequences of both the disease and the therapy.
Pregnancy with SLE
A separate complex problem is planning and managing pregnancy in women with lupus. It is especially relevant due to the fact that the disease most often occurs in young women of childbearing age. Planning pregnancy is possible only with complete, stable remission of the renal process, stable kidney function and blood pressure. Recent studies have shown that the outcome of pregnancy directly depends on the degree and duration of remission of the disease before conception. During pregnancy, systematic observation by both a gynecologist and a rheumatologist is mandatory. Regular monitoring of disease activity, blood pressure, and fetal development is especially important.
Causes and mechanism of development of SLE
Until now, it has not been possible to establish the exact causes of the development of systemic lupus erythematosus. In this regard, there is no etiotropic treatment of the disease. Experts identify some predisposing factors, the presence of which significantly increases the risk of systemic lupus erythematosus. These include:
- Hereditary predisposition. This factor is not the main one, however, the presence of SLE in relatives increases the possibility of developing an autoimmune disease.
- Prolonged exposure to direct sunlight. Systemic lupus erythematosus is accompanied by the development of photosensitivity. Ultraviolet radiation provokes an exacerbation of the disease.
- Occupational hazards. Frequent contact with chemicals has a negative impact on health. This situation can lead to the onset or exacerbation of systemic lupus erythematosus.
- Smoking. It has been proven that tobacco impairs blood microcirculation. Smoking significantly worsens the course of systemic lupus erythematosus, leading to long-term relapses.
- Taking certain medications. Hormonal drugs in high doses provoke an exacerbation of the disease.
- Stressful situations and excessive physical activity. These factors can worsen the course of SLE or provoke its exacerbation.
- Female. According to statistics, women are more susceptible to systemic lupus erythematosus than men.
An autoimmune disease is characterized by the fact that the body perceives its own cells as foreign. The mechanism of development of systemic lupus erythematosus is associated with the formation of antibodies to one’s own cells. This leads to the formation of circulating complexes that settle on the surfaces of organs. This process leads to the development of an inflammatory process.
Goal of treatment
- achieving remission of the disease.
- General notes on therapy
Treatment of patients is based on the use of systemic antimalarial drugs and glucocorticosteroid drugs for external use.
In case of limited skin lesions, topical glucocorticosteroid drugs are prescribed: for lesions on the skin of the body - in the form of creams and ointments, for lesions on the scalp - in the form of lotion.
Antimalarial drugs are effective both in the form of combination therapy and monotherapy. Hydroxychloroquine sulfate is preferred due to better tolerability. Due to the possible development of retinopathy when taking antimalarial drugs, an ophthalmological examination, including an examination of the fundus, is performed before starting the drug and at least once every 6 months. Laboratory parameters are regularly monitored. In the presence of resistance to antimalarial drugs, reserve drugs are used: dapsone, retinoids or methotrexate. Systemic retinoids are indicated in the presence of severe hyperkeratosis (discoid, verrucous). Treatment of the bullous form is carried out with the drug dapsone, which inhibits the migration of neutrophil leukocytes, and systemic glucocorticosteroids.
Indications for hospitalization
- severe dermatosis;
- lack of effect from outpatient treatment.
Treatment regimens
External therapy
Glucocorticosteroid drugs
When skin lesions are localized on the face, it is recommended to use topical glucocorticosteroid drugs of weak or moderate activity:
- fluocinolone acetonide, cream, gel, ointment, liniment 2 times a day externally to the lesions for 12 weeks.
If the trunk and limbs are affected, it is recommended to use topical glucocorticosteroid drugs of moderate activity:
- triamcinolone ointment 2 times a day externally under occlusion on the lesions for 1 week or
- betamethasone, cream, ointment 2 times a day externally to the lesions for 8 weeks.
When rashes are located on the scalp, palms and soles, it is recommended to use topical high-potency glucocorticosteroid drugs:
- clobetasol, cream, ointment 2 times a day externally to the lesions for 4 weeks.
Intralesional administration of glucocorticosteroid drugs can be used on localized lesions that are not amenable to other therapy. The use of this method is limited by the possibility of developing persistent atrophy.
- triamcinolone 5-10 mg per ml intralesional or
- betamethasone 0.2 ml per cm2 intralesional, the weekly dose should not exceed 1 ml.
If the need for intralesional administration of drugs continues, it is recommended to maintain an interval between injections of at least 4 weeks.
Systemic therapy
Antimalarials:
- Hydroxychloroquine 5-6 mg per kg body weight per day orally (or 2 tablets of 200 mg for an average weight adult). Once clinical response is achieved, the dosage of hydroxychloroquine can be gradually reduced to 200 mg per day with continued therapy for at least 2-3 months. Taking the drug can last up to 2-3 years. Stopping maintenance doses increases the risk of relapse by 2.5 times or
- chloroquine 250-500 mg orally daily for at least 2-3 months. Taking the drug can last up to 2-3 years.
Considering the important role in the pathogenesis of ultraviolet irradiation-induced free radical damage to membranes and microcirculation disorders, the inclusion of antioxidants in the therapeutic complex is indicated:
vitamin E 50-100 mg per day orally in intermittent courses: 1 week taking the drug, 1 week off, for 4-8 weeks.
It is also recommended to take angioprotectors and microcirculation correctors:
- pentoxifylline 200 mg orally 3 times a day for 1 month
- nicotinic acid 0.05-0.1 g orally 2-3 times a day for 21-30 days or 2-3 ml intramuscularly every other day, for a course of 8-10 injections.
Special situations
Treatment in pregnant women is carried out only with topical corticosteroids of class I or II. The use of antimalarial drugs is contraindicated due to the possibility of disruption of normal intrauterine development of the fetus.
Tactics in the absence of treatment effect
Second-line drugs prescribed in the absence of effectiveness of topical glucocorticosteroid drugs are topical calcineurin inhibitors:
- tacrolimus, ointment 0.1% 2 times a day on the lesions for 4-8 weeks or
- pimecrolimus cream 1% 2 times a day on the affected areas for 4-8 weeks.
Second-line drugs for systemic therapy are retinoids. Treatment should begin with lower doses (10-20 mg per day) and gradually increase them, focusing on tolerability and the absence of side effects:
- acitretin 50 mg per day orally for 8 weeks or
- acitretin 0.2-1.0 mg per kg body weight per day orally for 8 weeks or
- isotretinoin 0.2-1.0 mg per kg body weight per day orally for 8 weeks.
Prevention
All patients are recommended to take measures to protect their skin from sun rays: wearing hats, clothes with long sleeves, with a closed neckline, trousers and long skirts, regular applications of photoprotective creams with a high SPF index (>50).
Symptoms of systemic lupus erythematosus
The disease is accompanied by damage to various systems. Systemic lupus erythematosus is characterized by a chronic course with periods of remission and relapse. The clinical picture of the disease includes the following general symptoms:
- Weakness, increased fatigue.
- Loss of body weight.
- Hyperthermia.
- Decreased performance.
- Headache, heaviness in the head.
Symptoms of systemic lupus erythematosus may develop gradually or occur acutely and suddenly. This factor is determined by the location of the lesion. In accordance with this, the lesion is distinguished:
- Musculoskeletal and muscular system.
- Skin.
- Respiratory system.
- Organs of the cardiovascular system.
- Urinary system.
- Nervous system.
- Gastrointestinal tract.
- Blood.
Damage to the musculoskeletal and muscular system
Connective tissue, which is most affected by systemic lupus erythematosus, is found in large quantities in joints and bones. This determines the prevalence of articular manifestations of the disease. The main signs of SLE with damage to the musculoskeletal system include:
- Pain. Appears in 90% of cases with systemic lupus erythematosus. The pain syndrome most often affects small joints on the hands. The clinical sign may spread to symmetrical joints. However, this rarely happens.
- Joint deformity. Changes in the configuration of the joint are permanent.
- Myositis. Pain in the muscles causes stiffness of movement, severe weakness and decreased performance.
Skin damage
Clinical signs of skin lesions in systemic lupus erythematosus appear in 60-75% of cases. The disease is characterized by the following symptoms:
- "Lupus butterfly." One of the most striking signs of systemic lupus erythematosus. The rashes are localized in the cheeks, nose, bridge of the nose, rarely on the torso and arms. The appearance of redness can be provoked by prolonged exposure to the sun or a stressful situation.
- Alopecia. Hair loss with systemic lupus erythematosus is rare. Skin appendages (hair, nails) become brittle and dry.
- Photosensitivity. The symptom is diagnosed in more than half of the cases. This results in increased sensitivity to sunlight.
Respiratory system damage
Symptoms of the presence of systemic lupus erythematosus in the respiratory system are detected in more than half of the cases. The most common diagnoses are lupus pneumonitis or pleurisy. Clinically, this is expressed in the appearance of shortness of breath, cough with sputum, which may contain bloody discharge. An autoimmune disease makes the body accessible to infectious agents. In this regard, infectious lung lesions may develop.
Damage to the cardiovascular system
Systemic lupus erythematosus causes damage to all structures of the heart. When diagnosing inflammation, the infectious agent is not detected. At the beginning, the disease is accompanied by the appearance of myocarditis, pericarditis, or endocarditis. As the pathology progresses, the process spreads to the valves. The mitral and tricuspid are most often affected. The presence of systemic lupus erythematosus increases the risk of developing atherosclerotic disease. Vascular damage is also possible, which provokes the development of heart attacks.
Damage to the urinary system
SLE most often affects the renal system. Lupus nephritis occurs, characterized by an inflammatory process in the kidneys. In this case, fibrin deposited in the glomerular membrane forms hyaline blood clots. Systemic lupus erythematosus leads to decreased renal function. Proteinuria and erythrocyturia appear in the urine. There may be cases when laboratory changes in urine are the only clinical manifestation of damage to the renal apparatus.
Damage to the nervous system
Damage to the blood vessels of the brain caused by systemic lupus erythematosus causes disorders of the central nervous system. Clinical symptoms of the disease are:
- Irritability, anxiety.
- Obsessive ideas, psychoses, hallucinatory phenomena.
- Migraine-type headache.
- Myelopathy, polyneuropathy.
Damage to the gastrointestinal tract
The frequency of diagnosing clinical symptoms of damage to the gastrointestinal tract in SLE is about 25%. The main signs of pathology include:
- Swallowing disorder. The symptom occurs due to damage to the esophagus.
- Peptic ulcer of the stomach or duodenum. An exacerbation may be caused by the presence of SLE or the effect of its treatment.
- Feeling of nausea, possibly vomiting.
- Abdominal pain of various types. Systemic lupus erythematosus acts as a cause of exacerbation of chronic diseases. For example, chronic pancreatitis.
Blood damage
For systemic lupus erythematosus, a specific sign of blood damage is the appearance of LE cells. The disease is accompanied by the recognition of the body's own cells as foreign. As a result, white blood cells destroy and absorb similar blood cells. SLE causes anemia, thrombocytopenia, and leukopenia. These signs may be clinical manifestations of an exacerbation of the disease or occur as a result of drug treatment.
Systemic lupus erythematosus is a disease characterized by a variety of clinical manifestations. Late seeking medical help occurs due to the disguise of signs of pathology as other diseases.
Tuberculous lupus
This type of lupus is a form of skin tuberculosis. Its causative agent is Mycobacterium tuberculosis. This disease mainly affects the skin of the face. Sometimes the lesion spreads to the skin of the upper lip and oral mucosa.
Initially, the patient develops a specific tuberculous tubercle, reddish or yellow-red, 1-3 mm in diameter. Such tubercles are located on the affected skin in groups, and after their destruction, ulcers with swollen edges remain. Later, the lesion affects the oral mucosa, and the bone tissue in the interdental septa is destroyed. As a result, teeth become loose and fall out. The patient's lips swell, become covered with bloody purulent crusts, and cracks appear on them. Regional lymph nodes enlarge and become dense. Often, lupus lesions can be complicated by a secondary infection. In approximately 10% of cases, lupus ulcers become malignant.
In the diagnostic process, diascopy is used and a probe is examined.
Treatment uses medications, as well as large doses of vitamin D2 . Sometimes X-ray irradiation and phototherapy are practiced. In some cases, it is advisable to remove tuberculosis lesions surgically.
Diagnosis of lupus erythematosus
Systemic lupus erythematosus requires a complex of diagnostic studies. The American College of Rheumatology has developed criteria, the presence of which helps in making a diagnosis. Identification of 4 of 11 criteria is the basis for diagnosing SLE. These include:
- Joint pain. The symptom is accompanied by swelling in the area of the affected joint, limited mobility, and stiffness of movement. A small amount of fluid may accumulate in the joint cavity.
- Skin rashes. Systemic lupus erythematosus is characterized by red rashes of various shapes. Scales form on the surface of the affected area, which do not separate on their own. The most common localization of rashes is the face, skin of the hands, and neck.
- Increased sensitivity to light. Prolonged exposure to direct sunlight is a risk factor for the development of systemic lupus erythematosus.
- Damage to mucous membranes. The disease manifests itself in the form of ulcerations in the nasopharynx. Most often, such rashes are painless.
- Rash on the nose and cheeks. Lupus butterfly is a specific symptom of systemic lupus erythematosus.
- Damage to the urinary system. Due to the spread of the autoimmune process to the kidney area, daily protein loss occurs in the urine.
- Lung damage. SLE often affects the body's respiratory system. This manifests itself in inflammation of the serous membranes. As a result of the pathological process, pleurisy is formed.
- Damage to the central nervous system. Clinical manifestations of this localization of systemic lupus erythematosus are not specific. Psychosis, seizures, and hallucinations may occur.
- An increase in antibodies in the blood. One of the criteria for the presence of SLE is an increase in the concentration of antinuclear antibodies (ANA).
- Blood damage. The autoimmune disease is accompanied by anemia, thrombocytopenia, and leukopenia. In addition, the diagnosis of systemic lupus erythematosus allows one to determine the presence of LE cells in the blood.
- Changes in the immune system. SLE is an autoimmune disease in which the body's own cells are perceived as foreign.
To confirm the presence of systemic lupus erythematosus, laboratory and instrumental studies are performed. Among them are:
- Blood analysis. This study is necessary to determine markers of the inflammatory process. These include C-reactive protein, ESR, and leukocytes.
- Analysis of urine. With systemic lupus erythematosus, an increased content of protein, red blood cells, casts and leukocytes in the urine is determined.
- Blood chemistry. It is carried out to determine the degree of organ damage. An increase in creatinine concentration indicates the presence of kidney damage; transaminases increase if the process spreads to the liver area.
- ECG, EchoCG. These studies are necessary to determine the extent of heart damage. SLE may present as endocarditis, myocarditis, or pericarditis.
- X-ray of the chest organs. An instrumental examination is carried out to identify lung damage. Pleurisy and pulmonary embolism are diagnosed in a similar way.
- Angiography. Suspicion of a stroke or vascular damage requires a contrast study.
There are specially designed diagnostic tests to detect systemic lupus erythematosus. Among them are:
| Name | The essence of the test | Determination frequency in % |
| A.N.A. | Allows you to determine specific antibodies to cell nuclei. | 90-95% |
| Anti DNA | Disease activity is characterized by the level of antibodies to DNA. | 50-60% |
| Anti-Sm | Specific antibodies to the Smith antigen are part of RNA. | 40% |
| Anti-SSA or Anti-SSB | This test is performed if a systemic connective tissue disease is suspected. This determines the number of antibodies to specific proteins in the cell nucleus. | 50-60% |
| Anticardiolipin | Antibodies to mitochondrial membranes | 40% |
| Antihistones | The test is specific for drug-induced lupus. Antibodies are determined against proteins involved in packaging DNA into chromosomes. | 60% |
There are several forms of lupus erythematosus, which must be differentiated from each other. These include:
- Drug-induced lupus erythematosus. It is a reversible disease. The main reason for the development of pathology is the use of certain medications. Clinical symptoms do not differ from those of systemic lupus erythematosus. Treatment consists of discontinuing medications that cause exacerbation of the disease.
- Discoid (cutaneous). This form of pathology is characterized by the appearance of specific skin manifestations in the form of a “lupus butterfly”. However, laboratory and instrumental studies show no signs characteristic of SLE.
- Neonatal. Diagnosed in newborns whose mother suffers from systemic lupus erythematosus. Clinical signs of the disease disappear after 6 months without treatment. This is due to the cessation of circulation of maternal antibodies in the child’s blood.
Currently, diagnosing systemic lupus erythematosus is not difficult. The Yusupov Hospital carries out all types of diagnostic measures necessary to identify this autoimmune disease. The latest equipment allows you to accurately determine the localization of the pathological process and carry out appropriate treatment.
Symptoms
The skin manifestations of lupus erythematosus are diverse. A significant manifestation, almost always associated with a systemic disease, is a rash on the face, shaped like a butterfly: with wings on the cheekbones and cheeks and a body on the bridge of the nose and bridge of the nose. The rash may appear as raised or deep-lying elements of pink and bluish-red color. There is a tendency to form ring-shaped lesions covered with very dense scales that are painful when removed. In some cases, the so-called lupus erythematosus pernio is formed, in which painful bright red bluish nodules appear on the toes, hands, nose, and ears in cold weather. Damage to blood vessels is accompanied by the appearance of rashes resembling bruises; dilated vessels can be visible in the nail beds. Some patients with SLE have symptoms resembling lichen planus.
There are also severe lesions with the formation of blisters and peeling of the skin, which is more typical for the onset of a systemic disease. Changes can affect the mucous membranes, especially often the mucous membranes of the lips and oral cavity. Lupus lesions on the scalp may result in hair loss. Diffuse hair loss and hair thinning are also possible.
SLE treatment
Due to the lack of exact causes causing systemic lupus erythematosus, there is currently no specific etiotropic treatment. The course of therapy is aimed at suppressing the mechanisms of development of CRS, as well as symptomatic relief of the symptoms of the disease. The main groups of drugs prescribed for systemic lupus erythematosus include:
- Glucocorticosteroids.
- Cytostatics.
- Non-steroidal anti-inflammatory drugs.
- Aminoquinoline drugs.
- Biological products.
Glucocorticosteroids
They are among the most common and effective drugs for the treatment of systemic lupus erythematosus. Long courses of taking glucocorticosteroids significantly alleviate the general condition and reduce the severity of clinical signs. There are several ways to take medications. One of them is pulse therapy, in which a large dose of the drug is administered simultaneously. The dosage is individual and depends on body weight. The combined use of glucocorticosteroids and cytostatics is recommended. Indications for pulse therapy are:
- Rapidly developing lupus nephritis.
- Damage to the central nervous system.
- High disease activity.
Cytostatics
A group of anticancer drugs whose mechanism of action is to disrupt cell division. The main indications for the use of this group of drugs for systemic lupus erythematosus include:
- Ineffectiveness of taking glucocorticosteroids.
- High disease activity.
- Vasculitis.
- Presence of acute lupus nephritis.
- Carrying out pulse therapy in combination with glucocorticosteroids.
Nonsteroidal anti-inflammatory drugs
To reduce the activity of the inflammatory process and relieve pain, NSAIDs are prescribed. When body temperature rises, anti-inflammatory drugs are used as antipyretic therapy.
Aminoquinoline drugs
Systemic lupus erythematosus occurs with the development of photosensitivity. To reduce the severity of this symptom, aminoquinoline drugs are used. They have anti-inflammatory and immunosuppressive effects.
Biological products
Biological drugs are considered a promising development in the treatment of systemic lupus erythematosus. Medicines in this group have fewer side effects compared to glucocorticosteroids. Mass use of biological drugs is difficult due to their high cost.
In case of severe disease, extracorporeal therapy is performed. Her methods include:
- Plasmapheresis. The method of blood purification involves partial removal of plasma from the body. This reduces the number of antibodies that cause SLE.
- Hemosorption. Specific sorbents used in hemosorption purify blood outside the body.
The choice of treatment method depends on the stage of development of systemic lupus erythematosus. Specialists at the Yusupov Hospital provide a full course of therapy for autoimmune diseases, taking into account the individual characteristics of the pathology, as well as concomitant diseases. The clinic's rheumatologists have many years of experience in dealing with the manifestations of systemic lupus erythematosus, which helps to alleviate the condition and reduce the severity of clinical symptoms in the shortest possible time.
Diagnostics
Given the fact that lupus patients experience a very wide range of symptoms, special criteria have been developed that are used in the diagnostic process. If there are four or more symptoms out of the eleven listed, we can talk about a probable diagnosis of lupus erythematosus.
The following symptoms are assessed: rash on the face in the form of a “butterfly”; discoid rash (red patches of skin where scarring may later appear); high photosensitivity (rash after exposure to the sun); ulcers on the mucous membranes of the nose, mouth, throat; kidney damage; arthritis; pleurisy/pericarditis; brain damage; changes in laboratory parameters (decrease in the number of red blood cells, platelets in the blood, the presence of specific antibodies, a false positive reaction to syphilis ).
biopsies are also taken into account .
Prognosis for life and complications
Systemic lupus erythematosus is an incurable disease, the treatment of which is limited to maintaining long-term remission. During the period of exacerbation, medications are prescribed to influence the mechanism of development of the disease, as well as symptomatic relief of the signs of SLE. The prognosis depends on the stage of detection of the disease. The earlier the pathology was diagnosed, the more favorable the prognosis for survival. A severe form of systemic lupus erythematosus with the development of multiple organ damage has an unfavorable prognosis and significantly reduces life expectancy. In order to minimize the number of relapses of the disease, there are preventive recommendations, which include:
- Regular visits to the doctor. The appearance of the first signs of exacerbation of the disease requires immediate consultation with a doctor for timely diagnosis and adjustment of therapy. During the period of long-term remission of SLE, scheduled consultations with the attending physician are necessary to conduct control studies.
- Strict adherence to recommendations for drug therapy. Glucocorticosteroids for SLE are taken on an ongoing basis. The dosage and frequency of administration are determined by the doctor based on previous diagnosis. It is forbidden to independently adjust the dosage of drugs; a complete refusal of therapy is excluded.
- Refusal of vaccinations and vaccinations.
- Maintaining a rational and balanced diet. Prevention of systemic lupus erythematosus requires limiting the consumption of salt, sweets, and flour products. Hot, spicy, smoked dishes are excluded from the diet. The daily menu should include a sufficient amount of protein.
- Limit exposure to direct sunlight. For additional skin protection on sunny days, you should use sunscreen.
- Elimination of overvoltage. A stressful situation or excessive physical activity can cause a relapse of systemic lupus erythematosus. It is recommended to follow a gentle regimen with proper rest.
- Selective use of medications. Autoimmune disease requires special attention to the choice of medications. Therefore, before taking the drug, you should consult your doctor.
Thanks to modern methods of treating systemic lupus erythematosus, the average life expectancy has increased. The five-year survival rate for diagnosed SLE is about 80-90%.
The severe course of the disease leads to the development of complications, which include multiple organ lesions:
- Kidney and liver failure.
- TELA.
- Ischemic or hemorrhagic stroke.
- Pulmonary edema, pleurisy, pulmonary hypertension.
- Intestinal gangrene.
- Internal bleeding of various locations.
Answers to common questions
How to cure lupus permanently?
Unfortunately, the problem cannot be eliminated forever. Drug and extracorporeal treatment is aimed at improving the patient’s quality of life and prolonging it. Methods that guarantee absolute recovery are deception; cases of complete recovery are not known in medical practice.
What does lupus look like?
Externally, the disease has common symptoms with various dermatological pathologies; there are similarities with psoriasis and dermatitis. But these pathologies cannot be confused. Lupus is a truly dangerous systemic disorder that can lead to irreversible consequences.
How does the disease manifest itself?
The main symptom of SLE is a butterfly-shaped rash that appears on the skin. Further, the condition worsens, the patient constantly feels tired, pain, his joints swell, his skin color changes, and swelling forms. As the disease progresses, complications develop, progressing due to a malfunction of the internal organs.
Can you die from lupus?
Systemic disease leads to severe consequences. The disease affects the entire body, organs change their structure and cannot ensure the fulfillment of the functions assigned to them in full. With poor-quality medication, the patient rapidly develops complications from the liver, kidneys and other systems, which can lead to death.
How to treat lupus erythematosus?
Systemic lupus erythematosus requires timely diagnosis and correct treatment with the selection of ongoing therapy. You can undergo a full examination to identify systemic lupus erythematosus in Moscow in the Yusupov Hospital. The clinic is equipped with modern equipment that allows for a full range of diagnostic measures necessary to make an accurate diagnosis. Based on the data obtained, highly qualified staff of rheumatologists selects individual treatment in accordance with the stage of development of the disease. You can make an appointment with a doctor, as well as find out more about prices by phone or on the official website of the Yusupov Hospital.