Compound
The main active ingredient is glibenclamide .
1 tablet contains 1.75, 3.5 or 5 mg of this element. The drugs Maninil 1.75 and Maninil 3.5 also contain the following additional components: methylhydroxyethylcellulose, lactose monohydrate, magnesium stearate, silicon dioxide, starch, red dye.
The medicine Maninil 5 contains the following additional components: talc, lactose monohydrate, gelatin, magnesium stearate, starch, red dye.
Use of the drug Maninil
The drug should be prescribed only by a doctor and always with diet correction. Dosing depends on the results of studies of glucose levels in blood plasma and urine. First and subsequent appointments. Therapy is started, if possible, with minimal doses, especially for patients with an increased tendency to hypoglycemia and body weight ≤50 kg. It is advisable to start therapy by prescribing 1/2–1 tablet of Maninil 3.5 (1.75–3.5 mg of glibenclamide) or 1/2 tablet of Maninil 5 (2.5 mg of glibenclamide) once a day. This dose can be gradually increased at intervals of several days to 1 week until the therapeutic dose is reached. The maximum effective dose is 15 mg/day (3 tablets of Maninil 5) or 10.5 mg of micronized glibenclamide (3 tablets of Maninil 3.5). Transferring the patient from the use of other antidiabetic drugs. Transferring to Maninil 3.5 is carried out very carefully and starts with 1/2–1 tablet of Maninil 3.5 (1.75–3.5 mg of glibenclamide per day). Dose selection. In elderly patients, asthenic patients or those with malnutrition, as well as those with impaired renal or hepatic function, the initial and maintenance dose should be reduced due to the risk of hypoglycemia. In addition, when the patient’s body weight decreases or lifestyle changes, it is necessary to decide on dose adjustment. Combination with other antidiabetic agents. Maninil can be prescribed as monotherapy or in combination with metformin. In some cases, if metformin is intolerant, additional use of drugs from the glitazone group (rosiglitazone, pioglitazone) may be indicated. Maninil can also be combined with oral antidiabetic drugs that do not stimulate the release of endogenous insulin by pancreatic β-cells (guare or acarbose). In case of secondary resistance to glibenclamide (decreased insulin production as a result of depletion of β-cells of the islets of Langerhans), combination therapy with insulin can be used. However, when the secretion of the body's own insulin completely stops, insulin monotherapy is indicated. Method of administration and duration of therapy. A daily dose of up to 2 Maninil tablets is taken without chewing with a sufficient amount of liquid (1 glass of water) 1 time per day before breakfast. With a higher daily dose, it is recommended to divide it into 2 doses in a ratio of 2:1 in the morning and evening. It is very important to take the drug at the same time every time. If you miss a dose of the drug, you should not take a double dose to replace the missed dose. The duration of therapy depends on the course of the disease. During treatment, it is necessary to regularly monitor the metabolic status.
Pharmacodynamics and pharmacokinetics
Glibenclamide stimulates insulin and increases the insulin-secreting effect of glucose .
Under the influence of the drug, the sensitivity of pancreatic cells to insulinotropic glucose-dependent polypeptide increases.
The extrapancreatic effect is achieved by increasing the sensitivity of receptors to insulin.
Maninil in therapeutic doses reduces the risk of developing complications such as nephropathy, retinopathy , cardiopathy , and reduces mortality from diabetes.
The drug has antiarrhythmic and cardioprotective effects, which allows it to be prescribed to diabetics with concomitant coronary artery disease.
Glibenclamide reduces platelet aggregation and prevents vascular complications of diabetes.
The drug is effective for more than 12 hours. In a micronized form, glibenclamide is absorbed more quickly from the gastrointestinal tract, which allows the drug to act more physiologically and gently.
Pharmacological properties of the drug Maninil
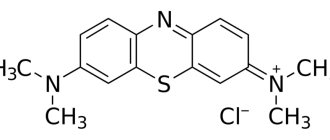
Pharmacodynamics. Glibenclamide - (1-{4-[2-(5-[chloro-2-methoxybenzamido)ethyl]benzenesulfonyl}-3-cycloxyxylurea) is a hypoglycemic agent. Reduces plasma glucose levels in both patients with type II diabetes mellitus and healthy volunteers by increasing insulin secretion by pancreatic β-cells. The hypoglycemic effect of glibenclamide depends on the glucose concentration in the environment surrounding the β-cells of the pancreatic islets of Langerhans. It inhibits the release of glucagon by α-cells of the pancreas and has an extrapancreatic effect, in particular, it increases the sensitivity of insulin receptors to insulin in peripheral tissues, enhances the action of insulin at the post-receptor level and slows down the breakdown of receptors, but the clinical significance of these phenomena has not yet been studied. Pharmacokinetics. After oral administration, it is quickly and almost completely absorbed. Concomitant food intake does not significantly affect the absorption of glibenclamide, but may lead to a decrease in the concentration of glibenclamide in the blood plasma. Binding to plasma albumin is 98%. Cmax in blood plasma after taking 1.75 mg of glibenclamide is achieved after 1–2 hours and is 100 ng/ml. After 8–10 hours, the concentration in the blood plasma decreases, depending on the dose administered, by 5–10 ng/ml. In the liver, glibenclamide is almost completely converted into two main metabolites: 4-trans-hydroxy-glibenclamide and 3-cis-hydroxy-glibenclamide. Both metabolites are completely excreted from the body in equal quantities with urine and bile within 45–72 hours. T1/2 of glibenclamide is 2–5 hours, but can be extended to 8–10 hours. The duration of action, however, does not correspond to T1/2. In patients with impaired liver function, elimination from blood plasma is slow. In case of renal failure, depending on the degree of renal dysfunction, the excretion of metabolites in the urine increases compensatoryly. With moderately severe renal failure (creatinine clearance - 30 ml/min), the total elimination remains unchanged; in severe renal failure, cumulation is possible.
Contraindications
Type 1 diabetes, diabetic precoma , coma , ketoacidosis , hyperosmolar coma , extensive burns, trauma, leukopenia, infectious diseases, pregnancy, microangiopathy, liver, kidney failure, intestinal obstruction.
Prescribed with caution for adrenal insufficiency, alcoholism, febrile syndrome, and thyroid diseases.
Contraindications to the use of the drug Maninil
If insulin therapy is necessary: insulin-dependent diabetes mellitus (type I), metabolic acidosis, hyperglycemic precoma and coma, decompensation of metabolic disorders during infectious diseases and operations, as well as conditions after pancreatic resection, complete secondary resistance to glibenclamide in type II diabetes mellitus. Other contraindications include: severe liver dysfunction, renal failure with creatinine clearance ≤30 ml/min, hypersensitivity to glibenclamide, Ponceau 4R dye or other components of the drug, as well as to other sulfonylureas, sulfonamide derivatives, diuretics and probenecid; During pregnancy and breastfeeding.
Side effects
With an inadequate diet or violation of the dosage regimen, Maninil can lead to hypoglycemia .
Fever, weight gain, allergies, arthralgia, dyspeptic disorders, proteinuria , neurological disorders, cholestasis porphyria cutanea tarda , polyuria, photosensitivity, impaired taste perception, headaches, and fatigue are also noted.
Side effects of the drug Maninil
When assessing side effects, the following frequency of occurrence is taken as a basis: very often (≥10%), often (≤10% and ≥1%), sometimes (≤1% and ≥0.1%), rarely (≤0.1 % and ≥0.01%), very rare (≤0.01% or cases unknown): metabolic: often - weight gain, hypoglycemia, which can become protracted and lead to a life-threatening severe hypoglycemic coma. The reasons for this may be an overdose of the drug, impaired liver and kidney function, alcoholism, irregular diet (especially skipping meals), unusual physical activity, impaired carbohydrate metabolism due to diseases of the thyroid gland, anterior pituitary gland and adrenal cortex. Adrenergic symptoms during hypoglycemia may be absent or mild with slowly developing hypoglycemia, peripheral neuropathy, or concomitant therapy with sympatholytics (mainly beta-adrenergic blockers). Symptoms that are precursors of hypoglycemia: hyperhidrosis, increased heart rate, tremor, a sharp feeling of hunger, anxiety, paresthesia in the mouth, pale skin, headache, drowsiness, dyssomnia, impaired coordination of movements, transient neurological disorders (impaired speech and vision, sensory and motor areas ). More detailed information about the state of hypoglycemia is given in the overdose section. With long-term use, hypofunction of the thyroid gland may develop; from the organ of vision: very rarely - visual impairment and accommodation, especially at the beginning of treatment; from the gastrointestinal tract: sometimes - nausea, feeling of fullness/distension in the stomach, vomiting, pain in the abdomen, diarrhea, belching, metallic taste in the mouth. These changes are transient and do not require discontinuation of the drug; from the hepatobiliary system: very rarely - transient increase in AST and ALT, alkaline phosphatase, drug-induced hepatitis, intrahepatic cholestasis, possibly caused by an allergic reaction of a hyperergic type on the part of hepatocytes. These disorders are reversible after discontinuation of the drug, but can lead to life-threatening liver failure; from the skin and subcutaneous tissue: sometimes - itching, urticarial rash, erythema nodosum , measles or maculopapular exanthema, purpura, photosensitivity. These hypersensitivity reactions are reversible, but very rarely can lead to life-threatening conditions, accompanied by shortness of breath and a significant decrease in blood pressure, up to the development of shock. Very rarely - generalized hypersensitivity reactions, which are accompanied by skin rash, arthralgia, chills, proteinuria and jaundice; allergic vasculitis; from the blood and lymphatic system: rarely - thrombocytopenia; very rarely - leukopenia, erythropenia, granulocytopenia (up to the development of agranulocytosis); in some cases - pancytopenia, hemolytic anemia. The listed changes in the blood picture are reversible, but very rarely can pose a threat to life; other side effects: very rarely - weak diuretic effect, reversible proteinuria, hyponatremia, disulfiram-like reaction, cross-allergy with sulfonamides, sulfonamide derivatives and probenecid. Ponceau 4R dye may cause allergic reactions.
Overdose
Increased sweating, hunger, impaired speech, consciousness, vision, tremors , rapid heartbeat, irritability, insomnia, depression , cerebral edema and other signs of hypoglycemia , coma.
Treatment: take sugar orally. If the patient is unconscious, then administer intravenous bolus of dextrose, glucagon, diazoxide. Every 15 min. monitor blood glucose levels. To prevent recurrent hypoglycemia, it is necessary to give the patient food rich in carbohydrates (easily digestible). For cerebral edema, dexamethasone and mannitol are prescribed.
Overdose of the drug Maninil, symptoms and treatment
Acute and chronic overdose of glibenclamide can cause the development of severe, prolonged and life-threatening hypoglycemia. Hypoglycemia can develop due to skipping meals, increased physical activity, and drug interactions. Symptoms of hypoglycemia: severe feeling of hunger, nausea, vomiting, general weakness, anxiety, hyperhidrosis, tachycardia, tremor, mydriasis, muscle hypertonicity, headache, sleep disturbances, endocrine psychosyndrome (irritability, aggressiveness, depression, depression, impaired concentration, confusion , coordination disorders, primitive automatisms - grimacing, grasping movements, chomping, convulsions, focal symptoms - hemiplegia, aphasia, diplopia, drowsiness, coma, disturbance of the central regulation of breathing and activity of the cardiovascular system). As hypoglycemia progresses, loss of consciousness (hypoglycemic coma) is possible; characterized by wet and cold skin upon palpation, tachycardia, hyperthermia, motor agitation, hyperreflexia, the appearance of a positive Babinski reflex and the development of paresis and convulsions. Treatment. Mild hypoglycemia (without loss of consciousness) can be eliminated by the patient on his own by taking approximately 20 g of glucose, sugar or carbohydrate-rich food. In case of accidental overdose and in the presence of contact with the patient, it is necessary to induce vomiting, perform gastric lavage (in the absence of convulsive readiness), prescribe adsorbents and administer intravenous glucose solution. In case of severe hypoglycemia (with loss of consciousness), it is necessary to immediately catheterize the vein. 40–100 ml of 40% glucose solution is administered intravenously as a bolus, followed by an infusion of 5–10% glucose solution, and if venous catheterization is impossible, 1–2 mg of glucagon is administered intramuscularly or subcutaneously. If the patient does not regain consciousness, the above measures are repeated and, if necessary, intensive therapy is carried out. To prevent relapses of hypoglycemia after restoration of consciousness over the next 24–48 hours, carbohydrates are prescribed orally (20–30 g immediately and every 2–3 hours) or a prolonged intravenous infusion of 5–20% glucose solution is performed. You can administer 1 mg of glucagon IM every 6 hours for 48 hours. Carry out regular monitoring of glycemic levels for at least 48 hours after elimination of a severe hypoglycemic state. If, in the event of a significant overdose (for example, during suicidal attempts), consciousness is not restored, a continuous infusion of 5–10% glucose solution is performed, the desired plasma glucose concentration is approximately 200 mg/dL. After 20 minutes, a re-infusion of 40% glucose solution is possible. If the clinical picture does not change, it is necessary to carry out a differential diagnosis of coma and simultaneously treat cerebral edema (dexamethasone, sorbitol). Glibenclamide is not excreted from the body during hemodialysis.
Interaction
Antifungal drugs, ACE inhibitors, NSAIDs, fibrates, anti-tuberculosis drugs, coumarin anticoagulants salicylates , beta-blockers, anabolic steroids, MAO inhibitors, biguanides, fenfluramine, tetracycline , chloramphenicol , pentoxifylline , cyclophosphamides, acarbose, pyridoxine, di zopyramide, bromocriptine, reserpine , allopurinol , insulin enhance the effect of Maninil.
Adrenergic stimulants, barbiturates, antiepileptic drugs, carbonic anhydrase inhibitors, BMCA, chlorthalidone , thiazide diuretics, furosemide , baclofen , glucagon, terbutaline, asparaginase, danazol , isoniazid , ritodrine, morphine, salbutamol , diazoxide, danazol, ritodrine, glucagon, hormones thyroid gland, rifampicin , chlorpromazine, nicotinic acid, lithium salts, estrogens, oral contraceptives weaken the effective effect of Maninil.
Large doses of ascorbic acid and ammonium chloride increase the reabsorption of the drug, enhancing the effect of glibenclamide.
When taken simultaneously with drugs that inhibit bone marrow hematopoiesis, there is an increased risk of myelosuppression .
Maninil 3.5 mg No. 120 tab.
Maninil International name: Glibenclamide Group affiliation: Hypoglycemic agent for oral use of the 2nd generation sulfonylurea group Description of the active substance (INN): Glibenclamide Dosage form: tablets Pharmacological action: Oral hypoglycemic agent, derivative of the 2nd generation sulfonylurea. It has pancreatic and extrapancreatic effects. Stimulates insulin secretion by lowering the threshold for irritation of pancreatic beta cells by glucose, increases sensitivity to insulin and the degree of its binding to target cells, increases insulin release, enhances the effect of insulin on glucose uptake by muscles and liver, and inhibits lipolysis in adipose tissue. Acts in the second stage of insulin secretion. It has a hypolipidemic effect, reduces the thrombogenic properties of blood. The hypoglycemic effect develops after 2 hours and lasts 12 hours. Indications: Diabetes mellitus type 2 (if diet therapy is ineffective). Combination therapy with insulin for daytime glycemic control. Contraindications: Hypersensitivity, diabetes mellitus type 1 (including in childhood and adolescence), diabetic ketoacidosis, diabetic precoma and coma, hyperosmolar coma, microangiopathy, liver and/or renal failure, extensive burns, trauma, major surgical interventions, intestinal obstruction, gastric paresis, conditions accompanied by impaired absorption of food and the development of hypoglycemia (infectious diseases), leukopenia, pregnancy, lactation. With caution. Feverish syndrome, alcoholism, adrenal insufficiency, thyroid disease (hypothyroidism or thyrotoxicosis). Side effects: Hypoglycemia (if the dosage regimen is violated and the diet is inadequate); weight gain, fever, arthralgia, proteinuria, allergic reactions (skin rash, itching), dyspepsia (nausea, diarrhea, feeling of heaviness in the epigastrium), neurological disorders (paresis, sensitivity disorders), hematopoietic disorders (hypoplastic or hemolytic anemia, leukopenia, agranulocytosis, pancytopenia, eosinophilia, thrombocytopenia), liver dysfunction (cholestasis), porphyria cutanea tarda, changes in taste, polyuria, photosensitivity, headache, fatigue, weakness, dizziness. Overdose. Symptoms: hypoglycemia (hunger, increased sweating, severe weakness, palpitations, tremor, anxiety, headache, dizziness, insomnia, irritability, depression, cerebral edema, impaired speech and vision, impaired consciousness), hypoglycemic coma. Treatment: if the patient is conscious, take sugar orally; if unconscious, inject dextrose intravenously (intravenous bolus - 50% dextrose solution, then infusion of 10% solution), 1-2 mg of glucagon subcutaneously, intramuscularly or IV, diazoxide 30 mg IV over 30 minutes, monitoring glucose concentration every 15 minutes, as well as determining pH, urea nitrogen, creatinine, and electrolytes in the blood. After regaining consciousness, it is necessary to give the patient food rich in easily digestible carbohydrates (to avoid re-development of hypoglycemia). For cerebral edema - mannitol and dexamethasone. Method of administration and dose: The dose depends on age, severity of diabetes, blood glucose concentration on an empty stomach and 2 hours after meals. The average daily dose ranges from 2.5 to 15 mg. Frequency of administration: 1-3 times a day, 20-30 minutes before meals. Doses of more than 15 mg/day do not increase the severity of the hypoglycemic effect. The initial dose in elderly patients is 1 mg/day. When replacing hypoglycemic drugs with a similar type of action, glibenclamide is prescribed according to the scheme given above, and the previous drug is immediately discontinued. When switching from biguanides, the initial daily dose is 2.5 mg; if necessary, the daily dose is increased every 5-6 days by 2.5 mg until compensation is achieved. In the absence of compensation within 4-6 weeks, it is necessary to decide on combination therapy. Special instructions: It is necessary to regularly monitor the blood glucose level on an empty stomach and after meals, the daily curve of glucose levels in the blood and urine. In case of surgical interventions or in case of decompensation of diabetes, the possibility of using insulin preparations must be considered. Patients should be warned about the increased risk of hypoglycemia when taking ethanol (including the possible development of disulfiram-like reactions: abdominal pain, nausea, vomiting, headache), NSAIDs, and during fasting. During treatment, it is not recommended to stay in the sun for a long time. Dose adjustment is necessary in case of physical and emotional stress, or changes in diet. Clinical manifestations of hypoglycemia can be masked when taking beta-blockers, clonidine, reserpine, guanethidine. During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions. Interaction: ACE inhibitors (captopril, enalapril), H2-histamine receptor blockers (cimetidine), antifungal drugs (miconazole, fluconazole), NSAIDs (phenylbutazone, azapropazone, oxyphenbutazone), fibrates (clofibrate, bezafibrate), antituberculosis drugs (ethionamide), salicylates, coumarin anticoagulants, anabolic steroids, beta-blockers, MAO inhibitors, long-acting sulfonamides, cyclophosphamides, biguanides, chloramphenicol, fenfluramine, acarbose, fluoxetine, guanethidine, pentoxifylline, tetracycline, theophylline, tubular secretion blockers, reserpine, bromocriptine, disopyrami d, pyridoxine, insulin and allopurinol enhance the effect. The effect is weakened by barbiturates, corticosteroids, adrenostimulants (epinephrine, clonidine), antiepileptic drugs (phenytoin), BMCC, carbonic anhydrase inhibitors (acetazolamide), thiazide diuretics, chlorthalidone, furosemide, triamterene, asparaginase, baclofen, danazol, diazoxide, isoniazid, morphine, ritodrine, salbutamol, terbutaline, glucagon, rifampicin, thyroid hormones, Li+ salts, in high doses - nicotinic acid, chlorpromazine, oral contraceptives and estrogens. Drugs that acidify urine (ammonium chloride, CaCl2, ascorbic acid in large doses) enhance the effect by reducing the degree of dissociation and increasing the reabsorption of glibenclamide. Drugs that inhibit bone marrow hematopoiesis increase the risk of myelosuppression.
special instructions
It is necessary to regularly monitor blood sugar levels and monitor the daily glucose concentration curve.
When taking ethanol simultaneously, a pronounced hypoglycemic effect, headache, and dyspeptic disorders may be observed.
During the treatment period, prolonged exposure to the sun is not recommended.
When changing diet, emotional and physical stress, a dose adjustment of Maninil is required.
Reduces the speed of reactions when driving vehicles.
MNN: Glibenclamide.
Analogs of Maninila
Level 4 ATC code matches:
Gliclazide
Glidiab
Glyurenorm
Glimepiride
Amyx
Glibenclamide
Amaryl
Diabetes
Analogs include Glibamide and Glibenclamide .
Maninila price, where to buy
The price of Maninil 1.75 is 130 rubles per package of 120 tablets.
The cost of Maninil is 3.5 - 170 rubles for the same packaging.
Maninil 5 will also cost about 130 rubles for 120 tablets.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Maninil 3.5 tablets 3.5 mg 120 pcs. Menarini-Von Heyden/Berlin Hemi
RUB 152 order - Maninil 1.75 tablets 1.75 mg 120 pcs. Berlin-Chemie AG/Menarini Group
121 rub. order
- Maninil 5 tablets 5 mg 120 pcs. Berlin-Chemie AG
120 rub. order
Pharmacy Dialogue
- Maninil (5 mg tablet No. 120)Berlin-Chemie AG/Menarini
116 RUR order
- Maninil (tab. 3.5 mg No. 120) Berlin-Chemie AG/Menarini
RUB 152 order
- Maninil (tab. 1.75 mg No. 120) Berlin-Chemie AG/Menarini
117 RUR order
show more
Pharmacy24
- Maninil 5 mg No. 120 tablets Berlin Chemi AG, Nimechchina
89 UAH.order - Maninil 3.5 mg No. 120 tablets Menarine von Heyden GmbH/Berlin Chemie AG (Menarine Group), Nimecchina/Nimecchina
93 UAH order
PaniPharmacy
- Maninil tab. 3.5 mg No. 120 Germany, Berlin-Chemie
105 UAH order
- Maninil tab. 5mg No. 120 Germany, Berlin-Chemie
94 UAH order
show more