Causes Symptoms Complications Diagnostics Treatment Advantages of treatment at MGC Price of treatment Classification
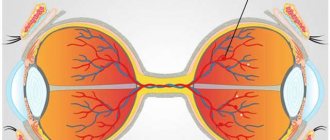
Uveitis is a collective concept that covers inflammatory diseases of various parts of the choroid. The choroid (synonymous with the uveal tract) is represented by the anterior section (includes the iris and ciliary body) and the posterior section (the choroid itself - the choroid). Anatomically, these sections have separate blood supply and innervation, therefore the inflammatory process in the choroid is localized in most cases, although in some cases the entire uveal tract may be affected.
Classification
Uveitis is classified according to duration, predominant damage to one or another structure of the uveal tract, and also depending on the pathogen.
There are four types of uveitis depending on the location of the inflammation.
- Anterior uveitis is inflammation of the anterior part of the choroid, including iritis and iridocyclitis. This is the most common type of uveitis.
- Posterior uveitis (synonymous with choroiditis) is an inflammation of the posterior part of the choroid, in addition to the choroid itself, affecting the retina and optic nerve.
- Peripheral uveitis is a disease that affects the ciliary body, vitreous body, the choroid itself (choroid) and the retina.
- Panuveitis is a combined inflammation of all structures of the vascular tract.
Depending on the severity of the pathological development, uveitis can be acute or chronic.
How is uveitis treated?
For treatment, antibiotics, non-steroidal and steroidal anti-inflammatory drugs are used, both local preparations - in the form of gels, ointments, drops, and systemic action. If the cause of secondary uveitis can be established, its treatment is carried out at the same time.
Self-medication with drugs or folk remedies at home is unacceptable in this case. Advanced forms of the disease can lead to complete blindness and other complications of uveitis. If you suspect that one or more symptoms of your illness may indicate uveitis, consult your doctor immediately: the sooner you begin treatment for acute uveitis, the higher the chance of maintaining your vision and completely getting rid of the disease.
Symptoms
Depending on the location of the inflammatory process, the patient's complaints will be different.
With anterior uveitis, the leading symptoms will be redness of the mucous membrane of the eye, accompanied by lacrimation, photophobia, pain, a narrow pupil (miosis), blurred vision, and increased intraocular pressure.
Symptoms of posterior uveitis are usually mild and manifest themselves in the form of “floaters” before the eyes, the appearance of a veil, decreased vision, pain in the depths of the orbit and changes in the visual fields (if the optic nerve is involved in the pathological development).
With peripheral uveitis, the main manifestations will also be “floaters” in front of the eyes and blurred vision.
Patients with panuveitis may present with complaints characteristic of damage to one or another part of the uveal tract.
Symptoms of uveitis
The clinical picture of ophthalmovascular inflammation is determined by a number of conditions: the nature of the pathogenic factor, the localization of the primary lesion, the speed and intensity of development. Accordingly, the symptoms of uveitis are very diverse.
Thus, more or less typical manifestations of anterior uveitis are subjective sensations of “veil before the eyes” and heaviness in the eyeball; decreased visual acuity and clarity; noticeable redness of the sclera; aching, “pulling” or sharp pain; miosis (constriction of the pupil) with weakened or absent response to light, or, on the contrary, a painful reaction of the eye to bright light; hyperlacrimation (increased lacrimation); surge in IOP (intraocular pressure). The extreme, limiting symptom of uveitis in some cases is complete loss of vision.
Posterior uveitis (choroiditis) is dangerous due to a long period of asymptomatic development, when there are neither visible signs nor subjective painful sensations. A decrease in visual acuity and quality also develops, as a rule, too slowly and gradually for the patient to notice it in the early stages. Seeking help is usually due to obvious “fogging” or the appearance of scotomas (blind spots) in the field of vision.
Treatment of uveitis
The earlier the pathology is detected, and the more accurately the cause of the disease is established, the greater the chances of a positive outcome in the treatment of uveitis. The choice of treatment tactics depends on the characteristics of the disease in a particular patient. To stop the inflammatory process, local and general therapy is used (anti-inflammatory drugs, immunostimulants, pupil dilators, antibiotics, physiotherapy, etc.). A good effect for this disease is provided by the use of hirudotherapy (treatment with leeches), which is also used in our clinic. If intraocular pressure increases, antiglaucomatous drops are prescribed.
Causes of the disease
The cause of uveitis can be the herpes virus, fungal infections, toxoplasmosis, tuberculosis bacteria, as well as other viral, mycotic, parasitic or bacterial attacks;
- allergies;
- systemic diseases of the body (endocrinological, hematological failures);
- autoimmune diseases (for example, rheumatoid uveitis in rheumatoid arthritis);
- injuries;
- surgical interventions;
- genetic predisposition;
- reducing the overall immunity of the body;
If, during the disease, damage to the uveal tract develops first, they speak of primary uveitis. If pathogenic agents enter the eye from another inflammatory process in the body, this is a secondary type of disease.
Advantages of treatment at MGK
One of the most important factors for successful treatment of uveitis is early detection, the most accurate diagnosis and comprehensive treatment. By contacting the Moscow Eye Clinic, you can undergo a comprehensive and completely painless examination in a short period of time, comfortably. Based on the results of the examination, the doctor will select an individual treatment regimen.
Our clinic employs recognized domestic specialists who have extensive practical experience in successfully treating a wide variety of eye diseases. For those patients who require long-term treatment using injections, physiotherapeutic techniques, hirudotherapy, etc. A day hospital is available, which allows treatment under the supervision of experienced doctors. The clinic is open seven days a week, from 9 a.m. to 9 p.m.
Author:
Mironova Irina Sergeevna 5/5 (1 rating)
Honey. portal:
Symptoms and diagnosis
The severity and manifestation of symptoms of ocular uveitis depends on its location (anterior or posterior), the degree of pathogenicity of the pathogen and the general condition of the patient’s body.
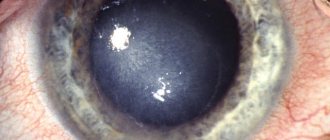
Anterior uveitis in its acute form manifests itself as bright redness, the so-called pericorneal injection - a halo of hyperemia around the cornea. A mixed injection is possible - total redness of the entire eyeball. Soreness increases, vision becomes blurred, the eye waters, it hurts to look at the light. The doctor, examining the patient, notes a constriction of the pupil, effusion, and a cellular suspension in the anterior segment. In most cases, ocular hypertension is observed.
In subacute or exacerbation of chronic uveitis of the eye, the symptoms are less pronounced, smoothed out - there is slight redness of the eye, mild pain, floating opacities in the field of vision.
Frequent complications of anterior uveitis of the eye are adhesions of the pupillary edge of the iris with the lens capsule - posterior synechiae, secondary glaucoma, cataracts, edema of the macular zone of the retina.
When localized predominantly in the posterior parts - posterior uveitis of the eye - symptoms include blurred vision, a large number of floating opacities in the field of vision that change their location when the gaze changes, distortion of the shape and size of objects.
Complications of the posterior forms of localization of uveitis are swelling and lack of blood supply in the center of the retina, impaired blood supply to the retina, its detachment, damage to the optic nerve.
The outcome of severe forms of posterior uveitis or panuveitis is often blindness or low vision, which leads to disability of the patient.
Diagnostics
Diagnostic measures necessarily include not only an examination by an ophthalmologist, but also consultations with related specialists - therapists, rheumatologists, dermatologists, allergists, etc.
In the ophthalmologist’s office, the following must be carried out:
- autorefractokeratometry and vision testing without/with correction;
- tonometry - measurement of intraocular pressure;
- examination of the anterior segment of the eye under a microscope (biomicroscopy). At this stage, signs of anterior uveitis are identified - cell suspension, exudate, precipitates on the endothelium of the cornea, changes in the iris, the presence of adhesions, changes in the vitreous body;
- ophthalmoscopy – examination of the fundus of the eye. The most informative is ophthalmoscopy performed after pupil dilation. In addition, instillation of mydriatics for uveitis of the eye, dilating the pupil, “breaks” the fusion between the iris and the lens, improving the circulation of intraocular fluid and serves as a prevention of ocular hypertension. When examining the fundus, the “interest” of the posterior segment in the inflammatory process is clarified: focal changes in the retina, its edema, ischemia, involvement of the optic nerve head, etc.
If the optical media are opaque, ultrasound is performed. Among additional diagnostic manipulations, if necessary, gonioscopy is performed (determine the presence of exudate, adhesions, newly formed vessels in the corner of the PC), and in transparent optical media - OCT (optical coherence tomography of the retina and optic nerve).
Gonioscopy - examination of the angle of the anterior chamber - in case of uveitis, it can reveal exudate, adhesions, neovascularization of the iris and the angle of the anterior chamber of the eye.
For adequate treatment of uveitis, laboratory diagnostics are extremely important: ELISA (determination of antibodies of classes M, G) to the causative agents of toxoplasmosis, cytomegalovirus, herpes, chlamydia, mycoplasma and other infections. They perform a general and biochemical blood test, a general urine test, etc.
If a tuberculous etiology of the process is suspected, phthisiatricians are involved in the diagnosis and treatment of eye uveitis, and a chest x-ray and Mantoux test are prescribed.
Etiology and development of the disease
The disease uveitis can be caused by any microorganisms that can provoke inflammation.
Moreover, their role is not primary: they act as provocateurs. The main reasons: decreased immunity due to serious diseases and predisposition of the body. The following forms of the disease are distinguished:
- iritis;
- iridocyclitis;
- cyclite;
- choroiditis;
- chorioretinitis.
Varieties of the disease account for from 30 to almost 60% of the inflammatory processes with which patients consult an ophthalmologist. In advanced forms and untimely treatment, the disease can lead to partial or complete loss of vision, which occurs in 25-30% of cases.
The uveal tract of the eye is characterized by separate blood supply to the anterior and posterior sections, a large branching of vessels with a rather slow blood flow. Due to these structural features, microorganisms can linger in the choroid and provoke inflammation.
Features of diagnosing inflammation of the choroid
For uveitis, ophthalmologists prescribe the following types of examination:
- external examination of the eyes (that is, checking the condition of the skin of the eyelids and conjunctiva);
- study of pupil reaction;
- visometry;
- perimetry;
- tonometry
- biomicroscopy;
- gonioscopy:
- ophthalmoscopy (if the optical media are clouded, an ultrasound of the eye is performed);
- angiography of the retinal vascular system;
- optical coherence tomography;
- laser scanning tomography of the retina;
- electroretinography;
- rheoophthalmography;
- paracentesis of the anterior chamber of the eye;
- biopsy, etc.
Correct diagnosis of the origin of uveitis is extremely important; such a study includes virological, bacteriological and immunological blood tests. Sometimes you may need to consult a rheumatologist or phthisiatrician, Mantoux test, chest X-ray, MRI of the brain, as well as other studies.
Consequences and complications
Severe trophic disorders, the action of toxins, epithelial lesions, pupillary fusion, congestion and exudation in the retina can lead to such serious consequences and complications as:
- clouding of the lens or in other words - cataract ;
- secondary glaucoma;
- atrophy of the eyeball;
- neuritis;
- exudative retinal detachment;
- band-shaped corneal degeneration.
Reasons for the development of uveitis
Factors that cause uveitis include:
- various infections (bacterial, viral, fungal, protozoal);
- allergic reactions;
- systemic diseases;
- eye injuries;
- metabolic problems;
- hormonal disorders.
The most extensive group of diseases is infectious uveitis - they account for over 43% of all cases of pathology. Among the infectious agents leading to inflammation, we can name primarily streptococcus, toxoplasma, mycobacterium tuberculosis, treponema pallidum, herpes virus, and cytomegalovirus.
The infection often penetrates the vascular system of the eye with blood transferred from the infectious focus, in the presence of tuberculosis, sinusitis, caries and other diseases.
Allergic uveitis occurs in the presence of high specific sensitivity to certain environmental factors. As is known, an allergic reaction can be triggered by plant pollen, certain foods, chemicals, etc. Inflammation often occurs as a pathological reaction of the body to certain medications.
Inflammation can be caused by various systemic pathologies and syndromes, including rheumatism, psoriasis, sarcoidosis, Reiter's syndrome, etc. Post-traumatic uveitis is observed after penetrating wounds of the eyeball, eye burns, and foreign bodies.
The likelihood of developing uveitis increases in the presence of diabetes mellitus, hormonal problems, reduced immunity, and also during menopause. Uveitis often develops against the background of other diseases of the visual organs (conjunctivitis, keratitis, blepharitis, scleritis, corneal ulcers, retinal detachment, etc.).
Diet for uveitis
Diet to boost immunity
- Efficacy: therapeutic effect after 3 weeks
- Terms: 1-3 months or more
- Cost of products: 1600-1800 rubles. in Week
If uveitis is non-traumatic in nature, then the severity of the course and the speed of development of pathogenesis directly depends on the state immunity . Therefore, to prevent uveitis, in addition to eye hygiene and regular examinations by an ophthalmologist, it is important to have a nutritious diet rich in vitamins (especially A and E) and foods that increase the body’s resistance. It is advisable to include in the diet:
- seafood, including cod and oysters;
- chicken eggs;
- nuts and seeds;
- carrots, apricots, citrus fruits and other orange fruits and vegetables;
- sprouted wheat, spinach and microgreens;
- Blueberries, which are also very good for vision, are rich in vitamin A and antioxidants .
Herpetic uveitis
| Herpetic uveitis accounts for up to 25% of all inflammatory diseases of the iris and ciliary body and most often occurs as keratouveitis (see.
|
Only an ophthalmologist can make a correct diagnosis. In our clinic, you will undergo all the necessary examinations using modern high-precision equipment and will prescribe the necessary treatment.
Causes
Often it is not possible to determine the cause (idiopathic uveitis). Provoking factors can be genetic, immune or infectious diseases, injuries.
It is believed that the cause of this disease after injury is the development of an immune reaction that damages the cells of the uveal tract in response to microbial contamination and the accumulation of decay products of damaged tissues. When the disease is infectious, the immune system begins to destroy not only foreign molecules and antigens, but also its own cells. In cases where uveitis occurs against the background of an autoimmune disease, the cause may be damage to the choroid's own cells by immune complexes, as a result of a hypersensitivity reaction.
Diseases that most often contribute to the occurrence of uveitis include: seronegative arthropathy (ankylosing spondylitis, Reiter's syndrome, psoriatic arthropathy, inflammatory bowel disease (Crohn's disease, ulcerative colitis)), rheumatoid arthritis, systemic lupus erythematosus, Behçet's disease, sarcoidosis, tuberculosis, syphilis, herpes virus, toxoplasmosis, cytomegalovirus, AIDS.
According to Rodrigues A. et al. (1994), idiopathic uveitis predominates among other forms and accounts for about 34%. Seronegative spondyloarthropathy causes the disease in 10.4% of cases, sarcoidosis - in 9.6%, juvenile rheumatoid arthritis - in 5.6%, systemic lupus erythematosus - in 4.8%, Behçet's disease - in 2.5%, AIDS - at 2.4%. According to the same author, anterior uveitis is the most common (51.6%), posterior - in 19.4% of cases.
When identifying symptoms of uveitis in a patient, it is necessary to remember about the “masquerade” syndrome, which imitates the disease. It can be of either a non-tumor nature (with intraocular foreign bodies, retinal detachments, myopic dystrophies, pigment dispersion syndrome, retinal dystrophies, circulatory disorders in the eye, reactions to the administration of medications), or tumor (with such oncological diseases as intraocular lymphomas, leukemia , uveal melanoma, metastases of tumors of other localizations, paraneoplastic syndrome, cancer-associated retinopathy, retinoblastoma).