- Cyst treatment
- Possible complications
- Prevention
Functional cysts are benign formations in the ovary that have a capsule that is filled with either liquid or semi-liquid contents. They increase in size due to stretching of the walls, and not due to tissue proliferation.
Although formations most often regress without medical intervention, no doctor can confidently predict what changes will occur under the influence of various factors.
As they develop, such formations can, in particular, negatively affect a woman’s reproductive function. To avoid serious consequences, it is necessary to monitor the cyst over time in order to take the necessary measures in a timely manner.
What are ovarian cysts?
Ovarian cysts are divided into:
- functional, the formation of which is directly related to the activity of the ovary. Detected in 90% of cases;
- organic, which are essentially tumor-like formations. These cysts, unlike functional ones, do not shrink or resolve on their own over time.
Let's take a closer look at the classification of ovarian cysts, which is based on their structure and method of formation.
Follicular cyst
This is the most common formation. Most often it develops in women of reproductive age. Much less often, follicular cysts are detected in the postmenopausal period (within 5 years after the last menstruation). Their development is due to the fact that the dominant follicle, due to a number of changes in the hormonal profile, did not undergo ovulation. As a result, it remains, increases in size and releases high levels of estradiol, which can disrupt the normal menstrual cycle.
There are cases where follicular cysts were found in newborns. This is due to the hormonal surge during childbirth. In approximately 50% of cases, they disappeared on their own within 1.5 months.
In some cases, treatment of a follicular cyst is required. It will be conservative, medicinal.
Luteal cyst
A corpus luteum cyst is formed in the second half of the menstrual cycle from the corpus luteum that appears after ovulation. This can be facilitated by various factors: changes in the endocrine system, characteristics of the blood supply to the ovary, chronic inflammatory diseases and other disorders. In this case, the corpus luteum, which appears in place of the dominant follicle, develops incorrectly. It increases in size, turning into a cyst.
Paraovarian cyst
It is formed from the tissue of the epididymis and is filled with transparent contents. It grows quite slowly, but over time it can reach large sizes (up to 30 centimeters in diameter). As a rule, it is diagnosed in women of reproductive age, less often it is detected in adolescents. It does not regress on its own, so a paraovarian cyst in some cases requires surgical treatment.
Endometrioid cyst
Hemosiderin, contained in blood cells, gives the cyst a specific color, which is why it is also called chocolate. The defeat can be unilateral or bilateral.
An endometrioid cyst is a manifestation of endometriosis. The formation can be of very different sizes (from 10 to 120 mm in diameter), and can cause an increase in the CA-125 tumor marker. It is diagnosed in women of reproductive age, in some cases in combination with pathologies such as fibroids and endometrial hyperplasia (overgrowth).
Cystadenomas
Also benign formations include cystadenomas; they are serous and mucinous. Mucinous cystadenoma tends to grow rapidly and has mucin-containing mucus inside. Most often it is diagnosed in patients of late reproductive age, as well as after menopause. Malignant transformation occurs in approximately 15% of cases.
Dermoid cyst
Teratomas (dermoid cysts) can be detected at any age in ovarian tissue and carry the rudiments of other tissues. These can be dermoid derivatives (the rudiments of skin, hair) or other tissues. Teratoma can reach 15 centimeters or more in diameter. This is a unilateral formation, which malignizes on average in 2% of cases.
What is a follicular cyst?
This is a bubble ~30-50 mm in size and has thin walls. It occurs in place of a follicle that has not burst: the egg dies, and the follicle degenerates into a cyst. It is important to understand that education has nothing to do with the malignant process, but it is necessary to monitor it over time. In the vast majority of cases, the formation is detected during a routine gynecological examination or during an ultrasound of the pelvic organs.
In many women, the pathology is asymptomatic. If the follicular cyst has grown to a size of 50 mm or more, symptoms may occur.
- Delayed menstruation. If the next menstruation does not occur after 1.5-2 months, the pregnancy test is negative, there is a high probability of developing this pathology.
- Cycle disruption. This includes heavy discharge and prolonged menstruation. Intermenstrual spotting is also possible.
- Pain in the lower abdomen. Aching pains are localized in the lower abdomen or in the area of the projection of the ovary. Discomfort and distension in the lower abdomen are also typical. Why does a follicular cyst hurt? This is due to the growth of the bladder and compression of the nerves, disruption of the blood supply to the tissues.
Only one of the described manifestations may be observed; sometimes the symptoms accompany each other.
Causes of cyst formation
So far, experts cannot say unequivocally why ovarian cysts form. However, it is believed that hormonal imbalances are the basis, which can be triggered by various factors:
- inflammatory diseases (both pelvic organs and other body systems);
- endocrine pathology;
- absence of pregnancies during the reproductive period of life;
- repeated artificial termination of pregnancy;
- menopause, as well as the period preceding its onset (perimenopause);
- taking certain medications.
There is evidence of a certain proportion of hereditary predisposition.
Formations are detected both during reproductive age and after the onset of menopause.
Epidemiology of ovarian cysts
Statistics show that seventy-five percent of ovarian cysts that occur in women of reproductive age are functional, and twenty-five percent of cystic formations are tumors. Functional ovarian cysts develop at any age, but they most often occur between puberty and menopause. Since on the eve of menopause there is increased stimulation of the ovary by gonadotropins, this contributes to the fairly frequent formation of functional cysts. In women who smoke, the risk of developing functional ovarian cysts doubles.
Signs
There may be no symptoms of a functional cyst (or other ovarian cysts) initially. Sometimes women tell their doctor that they:
- heaviness and/or nagging pain appeared in the lower abdomen. The intensity of sensations usually increases during and after sexual intercourse, as well as during physical activity;
- the cycle was disrupted, including intermenstrual bleeding from the genital tract;
- the abdomen has increased in volume (this happens if the cyst has acquired significant size).
Ovarian cysts - symptoms, signs, clinical manifestations, diagnosis and treatment methods
Hello Konstantin Viktorovich.
Elena Pavlova writes to you, (Samara), for the last 2 years I have lived like in a nightmare, I remember my last “favorable visit” to the gynecologist when, after an examination, she said that everything was fine with me and there was no reason to worry, after 6 months At an appointment with another gynecologist, she immediately sent me for an ultrasound. The diagnosis sounded like a death sentence: uterine fibroids of 8 cm, a large ovarian cyst, adhesions and obstruction of the tubes and a bunch of other ailments. And the examinations began, each time there were more and more new sores, each doctor gave me his own diagnosis and it was more and more terrible, all these endless queues in hospitals, tests, tears, despair, mistakes, indifference and indifference of doctors and none of them did not promise me to save my female organs. Then I was 31 years old and had not yet given birth, but no one cared. I did not agree to the operation, continuing to go to doctors, calling all my friends, looking for information on the Internet, in other cities, with the hope that someone would still help me. For all these consultations and examinations, I paid quite a large amount of money. So this time flew by, the cyst increased several times, the fibroid also grew, and 3 more small fibroids were discovered. The doctors at our oncology center didn’t even want to talk about preserving organs, having lost all hope, I opened the Internet for the last time, before the operation, sat there all day, and only late at night I accidentally found a website about the Swiss University Clinic and Konstantin Viktorovich Puchkov. I read the reviews until the morning and didn’t believe that it was all true. I no longer had a choice, because the doctors in my city refused to help me and I wrote a letter to Konstantin Viktorovich, although, to be honest, I did not even hope that I would receive a letter in response. And suddenly OH MIRACLE!!! After 2 days, Konstantin Viktorovich sent me a letter saying that organs can and should be preserved. I went to Moscow with little hope and faith in the best surgeon in the world. Everyone tried to dissuade me from going, the doctors insisted that miracles don’t happen and you’ll just leave all your money there and come back to us for help. At the clinic, I couldn’t believe myself, as if I was in a fairy tale: sweet and polite girls at the reception, kind, attentive, responsive doctors. The entire examination and tests went so quickly and painlessly that I did not expect it; I received competent and clear advice. Konstantin Viktorovich immediately warned that it would be necessary to do 2 operations and reassured me by promising to save the organs, first to remove a huge ovarian cyst, and after a few months to remove the fibroids. I had my first operation in February 2015, and a few days later I was already at home. Having been in the golden hands of a most experienced surgeon and his colleagues, I no longer had any doubt that I would perform the second operation only in a Swiss clinic. I went to the next operation, which took place in December 2015, without fear - with full confidence that Konstantin Viktorovich would save my organs. At that time, I only had 3 small lines left, traces reminiscent of the operation. During the second operation, 11 fibroids were removed, instead of the discovered 4, one of which was 12 cm. Despite the fact that abdominal surgery was performed, the next day I was already moving around, and 4 days later I was going home to Samara.
I would like to thank all the employees of the Swiss University Clinic, and especially Lyubimova Elena Anatolyevna, Agisheva Valeria Vladislavovna for their attentive attitude, careful and very careful examinations, for their kind eyes and understanding, for their clear and competent consultation. Thanks to Leonid Venidiktovich, the anesthesiologist who worked during the operation, the nurse Nastenka, who nursed me after anesthesia, and the other nurses who looked after and helped after the operation. Special thanks to Olga Troitskaya for prompt preparation for the operation.
The Swiss University Clinic employs not just doctors, but DOCTORS with extensive experience and ability, who are not afraid to trust with their lives. The clinic has not just a team - it is one team working clearly and harmoniously.
Dear Konstantin Viktorovich, I express my sincere gratitude and low bow to you for saving my life, for giving me hope for the opportunity to become a mother and I will try to make it come true. For your golden hands, energy, sunny smile, experience, talent, kindness, cheerfulness, for your kind heart. I thank the Lord God that he directed me to your clinic. God bless you. Sorry if I forgot someone or wrote something wrong, for the verbosity.
Sincerely, Elena Pavlova, Samara [email protected]
Diagnostics
Typically, an ovarian cyst is discovered randomly during a routine examination. The doctor prescribes:
- ultrasound examination of the pelvic organs;
- clinical blood test;
- blood test for hCG (to exclude pregnancy);
- smear microscopy;
- analysis to determine the tumor antigen CA-125.
If there is a suspicion of complications, additional diagnostic laparoscopy, puncture of the posterior vaginal vault, computed tomography (CT) or magnetic resonance imaging (MRI) may be required.
Which candles to choose?
Ichthyol suppositories in gynecology for ovarian cysts have an anti-inflammatory and antiseptic effect. The active substance is ichthyol. This substance is black in color and has a pungent odor. It is used rectally after natural bowel cleansing 1-2 times a day, it can also be used vaginally. The positive effect is achieved quickly enough due to good absorption of the substance. Ichthyol suppositories for ovarian cysts have good reviews due to the absence of contraindications and side effects.
Indomethacin for ovarian cysts reduces pain and swelling by blocking enzymes that cause inflammation. Refers to non-steroidal anti-inflammatory drugs. The effectiveness of the drug is achieved at 90%. Taken vaginally 1-2 suppositories per day, quickly absorbed. It is not recommended for patients with diseases of the gastrointestinal tract, liver, allergies, pregnant women and nursing mothers. Side effects include dizziness, drowsiness, abdominal pain, nausea and vomiting.
Diclovit is a non-steroidal anti-inflammatory drug. It is used as an anti-inflammatory drug for the pelvic organs. Administer rectally after defecation or a cleansing enema, 1-2 suppositories per day. It should not be prescribed for allergic reactions, bronchospasms, individual intolerance to the substance, or for pregnant and lactating women. Side effects: migraine, tinnitus, allergic reaction, and in rare cases, swelling of the legs. In case of overdose, confusion, nausea, vomiting, and bleeding may occur. The drug should be used very carefully in combination with other drugs.
In gynecology, longidaza is used for the treatment and prevention of adhesions formed due to the inflammatory process. It has immunomodulatory, antioxidant and slight anti-inflammatory effects. Has good absorption. One suppository is used after a two-day break. It is administered vaginally or rectally, after cleansing the intestines. Contraindicated for patients with cancer, pregnant women, children under 12 years of age, and kidney disease. Side effects manifest themselves in the form of an allergic reaction.
Suppositories with propolis are used as anti-inflammatory, antibacterial, antioxidant, and immunomodulatory agents. Used vaginally or rectally, after cleansing the intestines.
Treatment
In most cases, functional cysts regress on their own within a few months, so dynamic monitoring is required. Ultrasound monitoring will allow you to assess the changes occurring and prevent the development of possible complications.
Based on the results of the examination, the following may be prescribed:
- anti-inflammatory drugs;
- COOK.
If the formation has not disappeared within six months, then we are not talking about a functional, but about a true formation of the ovary. Surgery may be recommended.
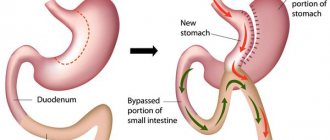
Cystectomy is a laparoscopic operation. Gaining access to the ovary requires only a few small punctures, so it is minimally traumatic.
If there is a suspicion that the tumor is malignant or borderline, the scope of surgical intervention can be expanded by the surgeon.
Cysts during pregnancy
The ability to become pregnant is not impaired during cystic ovarian lesions. Pregnancy promotes the disappearance of cystic formation. During pregnancy, a cyst appears extremely rarely. The formation of follicles stops during this period.
If a cyst is diagnosed when planning a pregnancy, many factors should be taken into account. If attempts to conceive do not succeed, an examination will help determine the type, cause and location of the cystic growth. The normal resorption process takes a couple of months, later the ovulation process improves, the normal menstrual cycle resumes, and the chance of getting pregnant increases. After the operation, 80% of women become pregnant in the first year, 15% in the first months.
Possible complications
Small functional cysts do not provoke dangerous complications and most often, as we have already said, resolve on their own within a few months. True ovarian masses may continue to grow, causing the risk of:
- rupture of the capsule, resulting in the contents pouring into the abdominal cavity;
- torsion of the cyst stalk, which disrupts the blood supply to the ovary itself. As a result, an inflammatory process and tissue necrosis develops. This condition requires immediate hospitalization.
Symptoms
As a rule, the symptoms of an ovarian cyst are not clearly colored and appear only when the course of this pathology is complicated. In this case, the patient may complain:
- for pain in the lower abdomen;
- enlargement of the abdomen and change in its shape;
- urinary disorders and constipation associated with the pressure of an increasing cyst on nearby organs;
- menstrual irregularities with irregular heavy discharge and bleeding in the middle of the cycle.
Prevention
To reduce the risk of developing ovarian cysts, women are advised to:
- undergo regular preventive examinations with an obstetrician-gynecologist and promptly treat diseases of the genitourinary organs;
- adhere to the principles of rational nutrition;
- use contraceptives to avoid abortions; correct endocrine disorders in a timely manner;
- do not use COCs or take medications without a doctor’s prescription.
If a functional cyst is discovered during the examination, it cannot be ignored and the recommendations of the treating obstetrician-gynecologist must be strictly followed.
Causes
Experts attribute most cases of occurrence to hormonal disorders, cell death, and inflammation. Women of mature age sometimes encounter this pathology, and after menopause, it is extremely rare. The process of occurrence is directly related to the menstrual cycle, and its absence significantly reduces the risk. But taking contraceptives, stressful situations, infections, abortions, and early onset of menstruation significantly increase the risk. Cysts are formed due to the following factors:
- Early menarche.
- Bad habits.
- Surgical interventions on the genital organs.
- Hormonal imbalance.
- Irregular menstruation.
- Lack of sexual intercourse for a long time.
- Obesity of various stages.
- Lack of reproductive function.