Hemorrhagic stroke is a rupture of cerebral vessels and hemorrhage in brain tissue. Depending on the localization and extent of the process, the prognosis of the disease is determined. Hemorrhagic stroke occurs less frequently than ischemic stroke, but the prognosis of the disease is more unfavorable.
The Yusupov Hospital treats patients with strokes and provides emergency care with the patient being transported to the intensive care unit. In the hospital, the patient will be examined using innovative equipment and will receive effective treatment using minimally invasive neurosurgery methods, the latest developments in the field of stroke treatment, and modern medications. The hospital provides comfortable rooms, dietary meals, and doctors create an individual treatment and rehabilitation program.
Types of hemorrhagic stroke
The effectiveness of stroke treatment depends on timely medical care. In hemorrhagic stroke, symptoms depend on the location of the injury. There are several types of hemorrhagic stroke:
- Intraventricular stroke - characterized by rupture of blood vessels and breakthrough of blood into the ventricles of the brain. The brain tissue becomes saturated with blood or hematomas form in the ventricles of the brain. Such a stroke most often ends in the death of the patient on the 2nd or 3rd day.
- Parenchymal stroke - hemorrhage occurs in the substance of the brain, a hematoma can form or the nerve tissues of the brain become saturated with blood, as a result of such a stroke a severe neurological deficit is formed.
- Subarachnoid stroke - hemorrhage occurs in the cavity between the arachnoid and pia mater of the brain.
- Mixed hemorrhages - bleeding is accompanied by changes that are characteristic of different types of strokes.
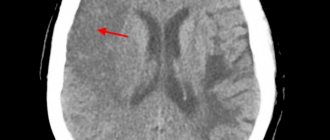
Principles of disease diagnosis
The gold standard for making a diagnosis is computed tomography (CT). In the early period after an attack (1-3 days), this method of neuroimaging is more informative than MRI. Fresh hemorrhagic material, including 98% hemoglobin, appears on CT as a high-density, well-defined, bright inclusion against the background of darker brain tissue. Based on a computed tomogram, the epicenter zone, volume and shape of the formation, the level of damage to the internal capsule, the degree of dislocation of brain structures, and the state of the cerebrospinal fluid system are determined.
With the onset of the subacute phase (after 3 days), the red cells of the hematoma along the periphery are destroyed, in the center the iron-containing protein is oxidized, and the focus becomes lower in density. Therefore, along with CT scan, MRI is mandatory within 3 days and later. In subacute and chronic forms, the MR signal, in contrast to CT, better visualizes a hematoma with derivatives of hemoglobin oxidation (methemoglobin), which passes into the isodense stage. Angiographic examination methods are used in patients with an unknown cause of hemorrhagic stroke. Angiography is primarily performed on young people with normal blood pressure readings.
For adequate management of patients after an attack of intracerebral hemorrhage, an ECG and X-ray of the respiratory organs are required, and tests for electrolytes, PTT and APTT are taken.
Causes
Hemorrhagic stroke is poorly diagnosed, although the causes and mechanism of its development are well studied. Various factors can provoke the development of hemorrhoidal stroke:
- Hypertension, arterial hypertension.
- Vascular aneurysm.
- Long-term use of anticoagulants.
- Diseases of the brain, spinal cord, cardiovascular system, diabetes.
- Congenital vascular defects.
- Blood diseases.
- Systemic diseases.
- Kidney and liver diseases.
- Alcoholism, drug addiction, tobacco addiction.
- Obesity.
- Stress.
- Hard physical labor.
- Hereditary predisposition.
A persistent increase in blood pressure leads to the formation of fibrinoid-hyaline necrosis of the walls of arterial vessels and can cause rupture of the walls of the aneurysm and the development of bleeding. The hematoma compresses the surrounding brain tissue, causing brain swelling. Blood from ruptured vessels can permeate the nerve tissue of the brain or, under pressure, break into the ventricles of the brain, the subarachnoid space.
Prevention
The disease is extremely serious and dangerous. It is much easier to avoid it than to treat it later. Prevention measures include:
Blood pressure control
- proper nutrition;
- monitoring weight changes (especially when you are overweight);
- control of blood pressure, preventing its increase;
- fight against atherosclerotic phenomena;
- getting rid of bad habits - smoking, alcohol;
- If possible, avoid stress and overexertion.
To prevent relapse, restorative and vitamin preparations are prescribed. Constant supervision by a specialist is required.
Symptoms of hemorrhagic stroke
Subarachnoid hemorrhage is accompanied by severe headache, vomiting, convulsions may begin, consciousness is impaired, Terson syndrome is observed, and meningeal symptoms appear. Parenchymal stroke is characterized by unexpectedly occurring severe headache, pallor or redness of the face, asymmetry of facial features, impaired coordination of movement, impaired respiratory function, and agitation. Ventricular stroke, the most severe form of the disease, is characterized by rapid deterioration of the patient's condition; bloody vomiting, loss of consciousness, fever, convulsions, and coma may occur. Ventricular stroke most often leads to the death of the patient. In most cases, hemorrhagic stroke occurs during the daytime, and the patient suddenly loses consciousness.
At the first examination, doctors note a change in complexion, high blood pressure, impaired respiratory function, slow pulse, decreased muscle tone, and tendon reflexes. Such symptoms are characteristic of the first hours after a stroke, then an increase in muscle tone and tendon reflexes occurs, the function of the pelvic organs is disrupted, the condition worsens, and the patient may fall into a coma.
Make an appointment
Puncture-aspiration method
| Puncture removal of hematoma with administration of fibrinolytic |
It is advisable to use the puncture-aspiration method for small lateral and medial hematomas accompanied by severe neurological disorders. The method consists of puncturing the hematoma with a catheter and simultaneously evacuating the liquid part of the hematoma. For precise positioning of the catheter, it is recommended to use neuronavigation. In some cases, drainage is carried out within 24 hours. The puncture-aspiration method with the introduction of fibrinolytics is indicated for lateral and medial supratentorial hemorrhages of medium size (from 30 to 60 ml) and for cerebellar hematomas (15–30 ml) provided the patient’s condition is stable. In this case, the technique is supplemented by fractional administration of fibrinolytic drugs at certain intervals. In the case of isolated ventricular hemorrhages, external ventricular drainage is performed with fractional intraventricular administration using fibrinolytics. According to the Research Institute of Neurosurgery, this method can reduce mortality in massive IVH by up to 40%, while in the natural course of this disease it approaches 100%.
Difference between hemorrhagic stroke and ischemic stroke
Strokes are characterized by the same symptoms, but have different causes of pathology. Hemorrhagic stroke has a more unfavorable prognosis and is characterized by the development of various severe disorders. In ischemic stroke, a favorable prognosis depends on the degree of brain damage. All types of strokes are characterized by the following disorders:
- Loss of speech.
- Paralysis of the body and limbs.
- Impaired sensitivity.
- Visual impairment or complete loss.
- Loss of coordination.
- Partial or complete hearing loss.
- Disorder of the function of the cerebral cortex.
- High blood pressure.
The consequences of a stroke depend on the location and extent of the brain lesion. Hemorrhagic stroke begins acutely, the disease progresses rapidly, and coma may develop within the first minutes or several hours. With hemorrhagic stroke, symptoms appear earlier than with ischemic stroke, they are more pronounced.
Clinical picture
At the first symptoms of a hemorrhagic stroke, it is important to begin treatment immediately. This is an acute condition that does not go away without symptoms. In most cases, the patient experiences a sharp deterioration in health, and loss of consciousness may occur.
The first symptoms of hemorrhagic stroke
The first manifestations of a stroke may differ, depending on the volume of the hematoma and its location. The task of loved ones is to identify them at an early stage and call a medical team for urgent hospitalization of the patient. Experts from the Clinical Brain Institute advise you to familiarize yourself with the main symptoms that may indicate acute cerebrovascular accident:
- tingling sensation of the skin, numbness of part of the face;
- nausea and vomiting;
- headaches, as well as soreness in the eye area and behind the eyes;
- impaired motor coordination;
- rapid pulse;
- paresis and paralysis of muscles in any part of the body, most often the process is one-sided.
These symptoms are typical if the patient remains conscious. Fainting is a common sign of a hemorrhagic stroke, and it is strictly forbidden to try to revive the person. There are several phases of consciousness regression - the prognosis for each of them will also be different:
- stunning - minor changes in which the victim is poorly aware of what is happening and practically does not react to others;
- somnolence - lack of response to external factors, while the eyes remain open, breathing and heartbeat are normal;
- stupor - a condition that resembles sleep, with preservation of the swallowing reflex and the reaction of the pupils to light;
- coma is a complete lack of reaction to what is happening; the patient’s vital activity is supported by special equipment.
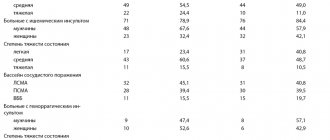
Various disturbances of consciousness are present in almost all patients, say experts from the Clinical Brain Institute. Based on their condition, it is already possible to preliminarily predict their chances of recovery. Thus, if consciousness is maintained, the probability of death remains within 20%, with stunning - up to 30%, with somnolence - up to 55%, with stupor - up to 85%. With the development of coma, the prognosis is questionable - survival rate is no more than 10%.
Signs of the acute phase of stroke
The clinical picture of stroke includes several main syndromes. They are a consequence of acute cerebrovascular accident and occur when neurons die. These syndromes suggest a hemorrhagic stroke, even if the patient is conscious:
- anisocoria - the patient’s pupils are dilated unevenly and have different sizes;
- decreased severity of reflexes, including a slower reaction of the pupils to bright light;
- the appearance of an oculocephalic reflex - if a patient in a coma turns his head to the side, his pupils shift in the opposite direction;
- bulbar syndrome - decreased tone of the chewing, swallowing muscles and tongue, which is manifested by corresponding symptoms;
- pseudobulbar syndrome - a violation of swallowing, chewing and speech while maintaining the tone of the corresponding muscles.
Immediately after a hemorrhagic stroke, it is difficult to predict the likelihood of full recovery. The patient’s condition can only be determined dynamically, so the patient spends the first time under 24-hour medical supervision. The fact is that during the course of the disease there are often several critical periods during which the likelihood of relapse is increased. The first of them occurs on the second to fourth day after the attack, the next one appears 10-12 days later.
Treatment after a stroke
A patient with a hemorrhagic stroke should receive first aid. The patient is placed on the bed, clothes are unbuttoned to make breathing easier, and a window is opened to allow fresh air to enter. The patient's head should be higher than the body level. The patient should measure blood pressure and pulse, monitor breathing in case of loss of consciousness and, if necessary, carry out resuscitation measures. The main task of doctors in case of hemorrhagic stroke is to stop bleeding, maintain respiratory function, the functioning of the cardiovascular system, and relieve cerebral edema.
In case of extensive hemorrhage in the brain, neurosurgical microtechnical operations are used - the hematoma is removed in order to reduce the pressure on the brain tissue and prevent the development of cerebral edema. Surgery for hemorrhagic stroke is performed strictly according to indications. Painkillers are prescribed to reduce headaches. If the cause of a hemorrhagic stroke was an aneurysm, doctors perform an operation and prescribe hemostatic drugs to stop the bleeding. Often, subarachnoid stroke is accompanied by vasoconstriction (secondary vasospasm) and the development of ischemic stroke. In this case, calcium channel blockers are prescribed to prevent narrowing and spasm of blood vessels.
Direct surgical removal of hematoma
| Direct surgical removal of hematoma |
Direct surgical intervention is used for subcortical hematomas of medium and large sizes, for large hematomas of lateral or mixed localization, accompanied by increasing edema and dislocation of the brain, deteriorating condition of the patient, for cerebellar hematomas. The operation consists of removing the hematoma by encephalotomy, aspiration of blood, removing dense clots with fenestrated tweezers and washing the wound with saline solution. After removing the hematoma, it is necessary to examine its walls and perform thorough hemostasis using coagulation and hemostatic agents. Better results can be achieved by using microsurgical techniques, which can significantly reduce the size of the encephalotomy and thereby minimize surgical brain trauma. For large VMH, accompanied by edema and dislocation of the brain, a wide osteoplastic craniectomy is performed with plastic surgery of the dura mater with periosteum or artificial materials. In case of cerebellar hematomas, it is advisable to supplement direct removal of the hematoma with the installation of external ventricular drainage.
Consequences
The consequences of a hemorrhagic stroke can bother the patient for the rest of his life. Depending on the severity of the disorders, recovery occurs; the most severe condition is in patients with extensive hemorrhagic stroke. Depending on which hemisphere of the brain is affected, the consequences of cerebral hemorrhage are observed. Hemorrhagic stroke of the right hemisphere of the brain:
- Partial or complete loss of vision.
- Disorders of urination and defecation.
- Paresis or paralysis of the body, decreased sensitivity of the left half of the body.
- Development of mental disorders.
A stroke to the left hemisphere of the brain causes paralysis on the right side of the body. When hemorrhage occurs in the area of the brain stem or cerebellum, loss of sensitivity occurs, the patient cannot swallow or speak, partial or complete loss of hearing in the right ear occurs, vision is impaired, coordination of movements is impaired, the patient cannot make unilateral or bilateral voluntary movements. Often the consequence of a hemorrhagic stroke is dementia (dementia), which develops gradually.
Right side
If the right side is affected, the most dangerous consequence is damage to the brain stem, in which a person's chances of survival are close to zero. This department is responsible for the functioning of the heart and respiratory system.
Diagnosing a hemorrhagic stroke on the right is quite difficult, since the centers of orientation in space and sensitivity are located in this part. This lesion is determined by speech impairment in right-handed people (in left-handed people the speech center is located in the left hemisphere). In addition, there is a clear relationship: if the functionality of the right half of the brain is impaired, the left side suffers and vice versa.
Rehabilitation of hemorrhagic stroke
Rehabilitation of the patient in the first 6-12 months consists of maintaining his vital functions and restoring lost abilities. During this period, when the patient has lost motor functions, the risk of bedsores and congestion increases. The patient is turned several times a day, the position of the body is changed, hygienic procedures are carried out, massage is carried out, the instructor engages in physical therapy exercises with the patient. During this period of time, the patient’s condition is monitored by several doctors - a therapist, a neurologist, a cardiologist and a psychologist. Rehabilitation measures are aimed at improving the patient’s quality of life and restoring lost functions.
Stroke
Practice shows that the best condition is achieved by patients who recover in specialized stroke departments of multidisciplinary hospitals. This allows, on the one hand, to help at the initial stage and, if possible, prevent disability, on the other hand, to move on to the recovery stage as early as possible.
As part of the Oberig universal clinic, there is a stroke center that helps people with GI recover well. Stroke is a multidisciplinary team consisting of highly qualified specialists: doctors, nurses, speech therapists, occupational therapists, physical therapists, psychologists. The center’s specialists adhere to international protocols that are used in countries with developed healthcare systems: the USA, Canada, Australia, and the European Union.
"Oberig" takes all necessary measures to improve the condition of patients. Rehabilitation team members spend an average of three hours per day with each patient. Physical therapists individually select aids: sticks, carts, orthoses. Before discharge, relatives are given detailed recommendations on how to care for the person at home.
The number of deaths and the frequency of complications in stroke are five times lower than the average in Ukrainian clinics. The center has existed for more than a decade, and during its work it has helped more than two thousand patients regain control over their bodies. Contact the call center and our staff will provide advice regarding your situation.
Forecast
The prognosis for hemorrhagic stroke depends on the severity of brain damage and the time of seeking first aid. If the stroke was not extensive and did not affect the vital centers of the brain, timely assistance was provided - there is a chance to return to normal life. It is impossible to predict the patient’s life expectancy - the prognosis depends on many factors:
- Patient's age.
- Severity of brain damage.
- Concomitant diseases.
According to statistics, more than 30% of patients die within a few weeks after a stroke, more than half of patients die within a year, and more than 60% of patients become disabled. No more than 20% of patients can recover completely within a few years.
Effective rehabilitation programs have been developed and tested at the Yusupov Hospital. The recovery process after a hemorrhagic stroke is unpredictable, lengthy and difficult. You can get advice on the treatment and rehabilitation of a patient by calling the hospital.
Make an appointment