Published: 11/03/2021 10:00:00 Updated: 11/03/2021
Urticaria is an allergic disease, the causes of which in children and adults can be very different. The main symptom of the disease is the appearance of blistering rashes on the skin, which are very itchy and resemble a nettle burn.
According to statistics, 25% of the entire population of the planet has encountered this pathology at least once in their lives, mainly children and women under the age of 40. With constant contact with the allergen, the disease becomes chronic, and in half of all cases it is accompanied by Quincke's edema.
Reasons for the development of urticaria
Hives never develop on their own; there is always a reason for this.
In some cases, identifying it is not difficult, but sometimes it is difficult to do. Most often, urticaria in children appears after using certain medications or eating certain foods. The most allergenic foods for babies are honey, nuts, fish, food additives, spices, sausages, and processed foods. Therefore, they are not recommended for children under 3 years of age.
Also, provoking factors include:
- insect bites;
- the presence of parasites in the body;
- plant pollen;
- mold;
- chemicals, including household chemicals;
- latex;
- ultraviolet radiation;
- vibration.
However, it is not always possible to find out what exactly the patient developed allergic urticaria to. In about a third of all patients with this diagnosis, the causes of the disease, even after numerous tests and analyses, remain unknown.
Diet
Diet is very important to prevent the occurrence of both acute and chronic allergic urticaria and its treatment. To determine what exactly triggered the allergic reaction, either the method of introducing a single product or allergy tests are used.
If it is not possible to identify a specific product, general recommendations should be followed:
- exclude products with a high and moderate degree of allergenic activity: chocolate, citrus fruits, eggs, nuts, fish, red fruits and berries, poultry, mushrooms, spices, vinegar, honey;
- exclude tonic drinks – tea, coffee, alcohol;
- exclude products with dyes and preservatives from the menu.
It is recommended to include water porridge (oatmeal, rice, buckwheat), vegetable soups, baked goods made from soft dough, and fermented milk products into the diet. Food processing helps reduce the allergenicity of food: peeling, heat treatment, freezing.
To speed up the removal of the allergen from the body, you need to drink a sufficient amount of water - up to 2-2.5 liters per day.
Symptoms of urticaria
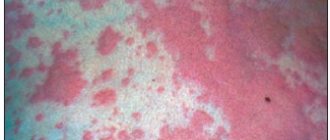
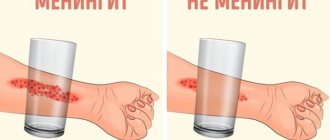
The main manifestation is the appearance on the skin of red or pink spots of various shapes, and blisters, the size of which can reach several centimeters.
A slight swelling may appear, which gradually disappears over the course of a day, rarely two. If the swelling affects the deeper layers of the skin or mucous membranes, angioedema may result - a life-threatening condition that requires immediate medical intervention.
The rash of allergic urticaria is always accompanied by unbearable itching, and some patients describe it as an unbearable burning sensation. Violent scratching of such areas can lead to infection of the epidermis with further complications in the form of pustules and wounds.
Minor manifestations of urticaria include:
- headache;
- elevated temperature;
- sleep disorder;
- anxiety;
- loss of appetite.
According to the nature of the course, allergic diseases are divided into two types.
Acute urticaria is diagnosed most often. Blisters and swelling of the skin in this form appear completely suddenly, sometimes against the background of a person’s excellent health. Most often caused by some external reasons, food. It also happens after using medications, especially when self-medicating. Symptoms go away on their own within a few days to several weeks.
Chronic urticaria is a condition in which symptoms continue to persist for more than 6 weeks after the first rash on the skin. This variant is characterized by a wave-like course, when periods of complete absence of symptoms (recovery) are abruptly replaced by exacerbations with the appearance of a new portion of spots and blisters. This is accompanied by unbearable itching and rapid development of Quincke's edema. The emerging elements of the rash can merge with each other, covering more and more new areas of the skin.
Sometimes periods of complete well-being without symptoms can last for a long time - up to 10 years.
Children's urticaria is an allergic skin disease, which most often develops against the background of an existing exudative diathesis and appears due to food products introduced as complementary foods.
It has been noticed that this type of allergy mainly develops in babies who are bottle-fed or eat foods that are not appropriate for their age.
Price
Allergology-immunology
| Name of service | Price |
| Consultation with an allergist-immunologist, primary | 3 500 ₽ |
Advantages
- The latest, constantly updated equipment
- Interest-free installments for all services
- Online consultations with an ENT doctor
- Visit of an ENT doctor to your home
- Friendly and qualified staff
- 24/7 ENT assistance
Hives are a condition characterized by a reddish, itchy rash on the skin that is caused by an allergic reaction. It is not contagious and is most often caused by a specific allergen, but in some cases the cause is unknown.
An allergic reaction to hives is fraught with serious complications that require urgent medical attention and are life-threatening. Therefore, you should not endure unpleasant attacks, but contact an allergist and find out how to treat urticaria in your particular case.
Complications of urticaria
It is important to know what hives look like and to be able to provide first aid correctly.
This will help prevent the development of severe complications that can lead to death. Often urticaria is accompanied by Quincke's edema, which is also called angioedema. Its development in the larynx area is especially dangerous, as it can compress the trachea and impair breathing.
Another serious complication is anaphylactic shock. This is a life-threatening immediate allergic reaction that occurs when the human body is hypersensitive to a particular allergen. Usually develops upon repeated contact with the allergen and requires immediate medical attention.
Recommendations for prevention
Those who have previously encountered pathology should avoid contact with potential allergens. It is worth keeping a food diary - recording the daily menu and the body's reaction to foods. This way a person will determine what he can and cannot eat, and will prevent the development of allergies and hives.
People with drug allergies are not recommended to take drugs based on acetylsalicylic acid and NSAIDs to prevent urticaria.
Clothing made from natural fabrics is less irritating to the skin and does not provoke the development of an allergic reaction such as hives.
An important role in disease prevention is played by the identification and sanitation of chronic foci of infection, helminthic infestations, and restoration of normal intestinal microflora. It is necessary to adhere to a healthy lifestyle and strengthen the immune system.
People prone to developing allergies need to have antihistamines on hand to help alleviate the condition before visiting a doctor. It is worth discussing their use with your doctor in advance, since some medications are contraindicated for children, pregnant women, and driving.
Article sources:
- Characteristics of patients with chronic urticaria at the stage of outpatient examination. Skorokhodkina O.V., Klyucharova A.R. Practical medicine No. 4, 2015. p. 131-135
- Urticaria: pathogenesis, clinical picture, therapy. Levonchuk E.A. Medical news No. 12, 2015. p. 3-6
- Clinical and laboratory features of the course of urticaria. Prokofieva N. B. Dermatovenereology. Cosmetology. Sexopathology, 2011. p. 30-35
- Modern principles of treatment of acute and chronic urticaria. Skorokhodkina O.V., Klyucharova A.R. Practical medicine No. 7, 2012. p. 45-49
Diagnosis of urticaria
Before starting treatment, it is important to understand what exactly a person has such a strong allergic reaction to.
Only by removing this provoking factor from your usual life can you not be afraid that the symptoms of urticaria will appear again, and this is possible even after proper therapy. Most often, this type of allergy appears to food. It is possible to determine what exactly caused the rash by a blood test: the level of IgE antibodies to a mixture of food allergens is detected. First of all, you need to diagnose the presence of an allergic reaction to:
- nuts;
- vegetables and legumes;
- citrus fruits and fruits;
- seafood;
- cereal and sesame flour;
- fruits and melons;
- baby formula;
- fish;
- meat;
- mushrooms;
- loose leaf tea;
- goat milk.
In addition to food, allergic manifestations can also occur to other substances that surround us almost everywhere in life:
- mold fungi;
- pollen from early flowering trees;
- pollen of late-flowering trees;
- weed pollen;
- epithelium of domestic animals;
- house dust;
- house dust mite;
- poultry feather.
To identify the exact type of allergen, allergy tests are performed on certain foods.
It often happens that rashes appear due to seasonings and herbs used in cooking: paprika, cumin, cloves, basil, ginger, tarragon, thyme, marjoram, dill, bay leaf, black pepper, vanilla. Some types of fish may also be allergenic: cod, halibut, mackerel, and squid meat. But sometimes an allergic reaction in the form of urticaria develops to such familiar products as:
- cucumber;
- apricot;
- cherry;
- tomato;
- plum;
- grape;
- persimmon;
- carrot;
- beet;
- watermelon.
All tests are carried out only by a specialist laboratory technician. You cannot independently determine the presence of an allergy in the form of urticaria to a particular food product or substance. This can be life-threatening, since it is possible to develop not only Quincke's edema, but also anaphylactic shock.
General notes on therapy
Treatment Goals
- regression of rashes;
- no relapses.
Diet.
- In case of a proven food allergy, it is recommended to avoid eating foods that provoke the development of the disease. Eliminating identified allergens from the diet leads to an improvement in the condition of the skin after 24-48 hours.
- In patients with daily or almost daily urticaria, it is recommended that a hypoallergenic diet be included in the extensive evaluation plan. In the case of a pseudo-allergic reaction, improvement with a hypoallergenic diet occurs after 3 weeks.
Pharmacological drugs
.
- Non-sedating 2nd generation H1-histamine blockers are recommended as basic first-line therapy for acute and chronic urticaria.
- The use of 1st generation H1-histamine blockers is currently limited due to their low effectiveness and the risk of side effects (sedation, anticholinergic effects, sleep disorders, etc.) and is indicated only in a number of exceptional cases.
- Treatment of acute urticaria with glucocorticosteroid drugs is not recommended. Indications for the use of systemic glucocorticosteroids are: lack of effect when treated with H1 receptor blockers, delayed urticaria due to pressure, angioedema.
- It is not recommended to use, due to very low evidence of effectiveness: H2-receptor blockers (both monotherapy and in combination with H1-histamine blockers), montelukast, zafirlukast, tranexamic acid, sodium cromoglycate, topical corticosteroids, colchicine, indomethacin, nifedipine.
Indications for hospitalization
to the dermatological hospital: widespread urticaria, accompanied by intense itching and a disturbance in the general condition, as well as lack of effect at the outpatient stage of therapy. to the intensive care unit: concomitant angioedema in the larynx, anaphylactic reactions
Requirements for treatment results
- stopping the appearance of fresh rashes;
- complete resolution of existing rashes;
- absence of subjective manifestations of the disease.
Prevention
Prevention of urticaria involves a thorough analysis of the allergy history before prescribing drug treatment. Particular attention should be paid to the manifestations of atopy in patients with urticaria. For preventive purposes, the use of 2nd generation H1-histamine blockers is recommended [8]. For patients with chronic urticaria, it is important to sanitize foci of chronic infection, treat concomitant pathologies, and also limit the effect of potential allergens.
Acute urticaria
- Eliminate exposure to trigger factors.
- Carry out drug therapy aimed at relieving the symptoms of the disease:
- treatment with H1-histamine receptor blockers;
- if there is no effect, treatment with systemic glucocorticosteroid drugs;
- urgent measures to relieve angioedema.
Chronic urticaria
- Elimination of exposure to factors that cause exacerbation of the disease (if possible).
- Hypoallergenic diet with the exclusion of suspected allergens and/or obligate allergens. When eliminating a food allergen from the diet, the condition improves after 1-2 days. When the rashes disappear, a gradual introduction of excluded or new foods begins, one at a time, one every other day, until new rashes appear. The ineffectiveness of the elimination diet for 1 month indicates the absence of a connection between urticaria and food products and serves as an indication for canceling the elimination diet.
- Drug therapy aimed at reducing symptoms of the disease.
Algorithm for drug treatment of patients with chronic urticaria.
| First line of therapy: | H1-histamine blockers 2nd generation |
| Symptoms persist for 2 weeks | |
| Second line of therapy: | Increasing the dose of 2nd generation H1-histamine blockers by 4 times* |
| Symptoms persist for 1-4 weeks | |
| Third line of therapy: | Omalizumab |
| A short (maximum 10-14 days) course of glucocorticosteroid drugs can be administered at any time. Indication: severity of exacerbation | |
* it is required to justify the prescription in doses exceeding those specified in the instructions for the use of drugs, to invite the patient or his legal representative to sign an informed consent, explaining the benefits and risks of such a prescription, to approve the prescription by a medical commission.
2nd generation H1-histamine blockers are effective in 40-60% of patients with chronic spontaneous (idiopathic) urticaria. If there is no effect from treatment with them for 2 weeks, a 4-fold increase in the dose of drugs is possible. Increasing the dose of H1-histamine receptor blockers allows you to limit the use of glucocorticosteroid drugs and, thus, avoid side effects of therapy and steroid resistance.
Features of the treatment of individual forms of urticaria
- Cold urticaria
. Patients should avoid sudden exposure to cold temperatures. 2nd generation antihistamines (rupatadine) can be used. Systemic glucocorticosteroid drugs are ineffective. - Delayed pressure urticaria
. Pressure on the skin should be avoided. For severe delayed urticaria from pressure, the most effective are systemic glucocorticosteroid drugs, which are prescribed for a short period of time with a gradual reduction in dose. Histamine H1 receptor blockers are usually ineffective. - Solar urticaria
. Antihistamines and ultraviolet light irradiation in gradually increasing doses are effective (tolerance induction). Adequate photoprotection (UVA+UVB) is important. - Urticarial dermographism
. No treatment is required unless the patient consistently responds to minimal trauma. 1st generation H1-histamine receptor blockers are effective. In some cases, the disease is severe and continuous therapy with 2nd generation antihistamines is required. - Cholinergic urticaria
. Patients should avoid intense physical activity. 1st and 2nd generation H1-histamine receptor blockers are used. Belladonna alkaloids/phenobarbital/ergotamine and radobelin/phenobarbital/ergotamine are indicated for the treatment of cholinergic urticaria. - Contact urticaria.
Avoid contact with provoking factors. Antihistamines are effective methods of therapy. Preventive administration of 2nd generation H1 histamine blockers is acceptable in cases of possible contact with trigger factors (for example, insect bites). Topical glucocorticosteroid drugs may be prescribed. For severe manifestations of the disease, systemic glucocorticosteroid drugs are used. - Thermal, aquagenic, vibration urticaria.
Antihistamines are not always effective. - Angioedema
. With the development of angioedema, epinephrine is administered parenterally (intravenously, intramuscularly or subcutaneously, depending on the severity and location of the lesion) and H1-histamine receptor blockers (intravenously or intramuscularly). If this therapy is ineffective and in cases of the development of severe angioedema with a violation of the general condition, systemic glucocorticosteroid drugs are used. In cases of difficulty breathing, aminophylline is used. - Adrenergic urticaria.
Avoid contact with provoking factors, oral propranolol. Nonspecific therapy, including tranquilizers and antihistamines.
Treatment regimens
1. 2nd generation H1-histamine receptor blockers
- Loratadine 10 mg orally 1 time per day until the rash disappears and 4 weeks after the rash disappears
- desloratadine 5 mg orally once a day until the rash disappears and 4 weeks after the rash disappears
- fexofenadine 180 mg orally 1 time per day until the rash disappears and 4 weeks after the rash disappears
- Cetirizine 10 mg orally once daily or 5 mg orally twice daily until the rash disappears and 4 weeks after the rash disappears
- Levocetirizine 5 mg orally once a day until the rash disappears and 4 weeks after the rash disappears
- ebastine 10-20 mg orally 1 time per day (depending on the severity of symptoms) until the rash disappears and 4 weeks after the rash disappears
- Rupatadine 10 mg orally once a day until the rash disappears and 4 weeks after the rash disappears.
2. First generation H1-histamine receptor blockers
- diphenhydramine 25-50 mg orally 4-6 times a day or 20-50 mg intramuscularly 1-2 times a day for 7-10 days
- clemastine 1 mg orally 2 times a day or 2 mg intramuscularly 2 times a day for 7-10 days chloropyramine 25 mg orally 1-2 times a day or 20-40 mg intramuscularly 1-3 times a day for 7-10 days
- cyproheptadine 2-4 mg orally 3-4 times a day for 7-10 days
3. Glucocorticosteroid drugs
- betamethasone 1-2 ml intramuscularly with an interval of 7-10 days, 1-2 injections
- dexamethasone 4-16 mg per day intravenously or intramuscularly until pronounced clinical improvement occurs, with further transition to oral administration (except for the treatment of angioedema)
- dexamethasone 1.5-4.5 mg per day orally until pronounced clinical improvement occurs, with a further gradual dose reduction of 0.125-0.25 mg once a week until complete withdrawal
- prednisolone 30-100 mg per day intravenously or intramuscularly until pronounced clinical improvement occurs, with further transition to oral administration (except for the treatment of angioedema)
- prednisolone 10-30 mg per day orally until pronounced clinical improvement occurs, with a further gradual reduction in dose by 2.5-5 mg once a week until complete withdrawal.
4. Adrenergic agonists
For severe urticaria and/or angioedema (laryngeal edema, exercise-induced anaphylaxis, severe cold allergy), epinephrine, a solution of 0.1% (0.1 to 0.3 ml), is administered subcutaneously or intramuscularly, if necessary, the administration is repeated after 10 -20 minutes up to 3 times.
5. Omalizumab
The drug is indicated for the treatment of chronic idiopathic urticaria, resistant to therapy with H1-histamine receptor blockers, in patients aged 12 years and older. The recommended dose of the drug for chronic idiopathic urticaria is 300 mg subcutaneously every 4 weeks. It is recommended that the attending physician periodically evaluate the need for continued treatment. The effect of omalizumab, as a rule, can be observed already in the first day, with its subsequent increase over a number of weeks. According to clinical studies and real clinical practice, the effectiveness of omalizumab reaches 90%.
Treatment of angioedema (Quincke's edema)
- epinephrine, solution 0.1%: 0.1-0.5 ml intravenously or intramuscularly, or subcutaneously once;
- chloropyramine, or clemastine, or diphenhydramine 1-2 ml intravenously or intramuscularly once;
- prednisolone 60-100 mg intravenously or intramuscularly or dexamethasone 8-16 mg intravenously or intramuscularly until pronounced clinical improvement;
- aminophylline 10 ml of 2.4% solution intravenously, slowly, once.
Related treatments
In the treatment of urticaria, drugs that affect the central nervous system are used as concomitant therapy: anxiolytics (tranquilizers) and antidepressants.
1. Anxiolytics (tranquilizers) for cholinergic urticaria:
- Hydroxyzine 25 mg orally 4 times a day with meals for 7-10 days
- belladonna alkaloids/phenobarbital/ergotamine 1 tablet orally 2-3 times a day for 1 month
- radobelin/phenobarbital/ergotamine 1 tablet orally 3 times a day for at least 1 month.
2. Antidepressants as concomitant therapy for patients with urticaria in the presence of depression and anxiety.
- amitriptyline 25-50 mg orally 1 time per day for at least 1 month.
3. External therapy. To reduce itching and burning, use warm showers and baths, lotions, shaken suspensions with menthol, anesthetics that do not contain glucocorticosteroid drugs.
Open recommendations
- Some experience has been accumulated in the use of cyclosporine A in combination with 2nd generation H1 histamine blockers for chronic urticaria.
- There are few studies showing the effectiveness of plasmapheresis in chronic urticaria of autoimmune origin.
- The latest consensus documents on the treatment of urticaria also recommend leukotriene receptor blockers, 2nd generation H1 histamine blockers in combination with omalizumab, ketotifen, dapsone, sulfasalazine, oxatamide, nifedipine, warfarin, intravenous gammaglobulin, autologous plasma, montelukast. However, this therapy has low-quality evidence, with no efficacy data from high-quality randomized clinical trials (CDs) [26–29, 34–43].
Treatment of pregnant women and during lactation
When managing pregnant and lactating women, you should adhere to rules similar to those when managing children. It is important to avoid the use of any systemic drug during pregnancy, especially in the first trimester, but the most effective treatment should be ensured. There are indications of an increase in histamine levels in pregnant women, which determines the need for the use of antihistamines. Prescription of 2nd generation H1-histamine blockers during pregnancy should only be used if necessary, when the expected benefit to the mother outweighs the possible risk to the fetus. In the first trimester, medications should be avoided.
A low dose of loratadine may be used for a short time. Use of 1st generation H1-blockers immediately before birth may cause respiratory depression and other side effects in newborns.
To date, there is not a single indication in the world of congenital pathology in children born to women who took 2nd generation H1-histamine blockers (cetirizine, loratadine) during pregnancy. It is advisable to prescribe loratadine to pregnant women with urticaria; recommendations for loratadine can be extrapolated to desloratadine. Recent clinical observations have shown that the safest drugs during pregnancy are loratadine, and during lactation, loratadine and cetirizine [45].
Treatment during lactation.
It is necessary to avoid taking medications during breastfeeding. If necessary, loratadine and cetirizine can be used.
Treatment of children
In children, acute urticaria is more often recorded, which can manifest itself as an allergic reaction, for example, to food. The disease usually develops within an hour after eating food and resolves within 24 hours. Chronic urticaria is less common among children than among adults. In childhood, the most commonly reported urticaria are pressure urticaria and cold urticaria, which are often combined with dermographic or cholinergic urticaria. In most cases, the positive effect of therapy is achieved by taking antihistamines and eliminating trigger factors. For children, 1st line of therapy is recommended, similar to that for adults. It is important to consider the age restrictions and age dosages of each of the H1-histamine blockers:
- loratadine: children aged 2 to 12 years with body weight less than 30 kg - 5 mg 1 time per day, children over 12 years old, and also with body weight more than 30 kg - 10 mg 1 time per day;
- Levocetirizine: children aged 2 to 6 years - 2.5 mg per day, children over 6 years - 5 mg per day;
- Cetirizine: children over 6 years of age (weighing more than 30 kg) - 1 tablet 1 time per day.
Desloratadine, fexofenadine, rupatadine are approved for use in children aged 12 years and older. In infants and children under 2 years of age, first generation H1-histamine receptor blockers can be prescribed. In rare cases, the use of systemic glucocorticosteroid drugs is allowed (for 3-5 days ) .
First aid for hives
It is important that you always have allergy medications in your home medicine cabinet, since urticaria in adults, and in children too, can appear at any time.
Allergy medications can be in the form of drops or tablets. Modern remedies do not cause drowsiness and have virtually no side effects. Doctors recommend having in your home medicine cabinet to eliminate urticaria and itching, Fenistil drops, which can be used from childhood, Erius tablets, which have a long-lasting antihistamine effect after administration, Loratadine, which helps cope with Quincke's edema, which often accompanies urticaria.
It is important to take the medicine at the first symptoms, without waiting for the general condition to worsen. If after 20 minutes from the moment of administration there is no improvement, you should call an ambulance.
Methods of treatment with traditional methods
The following methods will help relieve itching, soothe the skin and speed up the healing of blisters.
Honey and horseradish:
- Mix honey and horseradish juice in a 1:1 ratio.
- Take the resulting mixture 1 tsp. 3 times a day.
Mint tincture:
- Pour 20 grams of boiling water over it. mint, leave for several hours.
- Strain and take 3 tbsp. l. in a day.
Mint decoction for lotions:
- Pour 30 gr. fresh nettle leaves 2 tbsp. water.
- Bring to a boil and simmer over low heat for 2 minutes.
- Leave for one hour, strain.
- Soak gauze in the infusion and apply to the sore spot several times a day.
hives in a child photo
Treatment of urticaria
The only way to get rid of the disease is to avoid contact with the allergen, which is previously detected by laboratory tests.
If testing does not reveal a provoking factor, and the urticaria is episodic, then taking antihistamines will quickly eliminate the symptoms. During treatment, it is recommended to follow a diet that, in case of urticaria, will help prevent the recurrence of the disease. The menu should include only hypoallergenic products: lean boiled meat, soups with recycled meat broth or vegetarian. It is better to choose rice, buckwheat, and oatmeal from cereals. Low-fat cottage cheese, natural yogurt, apples, dried fruit compote, excluding raisins, and whole grain bread are recommended.
Citrus fruits, nuts, fish and all seafood, chocolate products, smoked meats, coffee, eggs, honey, and store-bought baked goods should be excluded from the menu during treatment.
Treatment is carried out by a dermatologist and an allergist-immunologist. For topical application, ointments for urticaria are effective; they not only relieve itching, but also eliminate swelling, redness and a burning sensation on the skin. One of the most effective is Dimetinden gel, which must be applied in a thin layer to the affected area of the skin up to 4 times a day.
A course of antihistamines is prescribed in the form of tablets. Your doctor may also prescribe calcium gluconate or calcium chloride for urticaria. They help reduce the symptoms of allergies, but they should only be administered under the supervision of a doctor in the treatment room.
If antihistamines do not provide the desired effect quickly, or for severe forms of hives, corticosteroids are used, which can be applied to the skin or taken in the form of tablets or injections.
Our doctors
Orlova Tatyana Vladimirovna
Doctor - allergist-immunologist, pulmonologist, doctor of the highest category
Experience 38 years
Make an appointment
Shundeva Oksana Veniaminovna
Allergist, doctor of the highest category
Experience 39 years
Make an appointment
How long does it take to cure hives?
Within 4-6 weeks, acute urticaria resolves in almost all patients with this diagnosis.
However, sometimes the acute form can become chronic, and then the disease becomes incurable, with periods of exacerbation and complete remission with the absence of symptoms, which alternate with each other. To deal with this allergic reaction as quickly as possible, it is recommended:
- Immediately consult a doctor at the clinic or call an ambulance.
- Follow a hypoallergenic diet for several months.
- Follow all doctor's orders and recommendations regarding treatment. Do not stop taking allergy medications at the first signs of improvement, but complete the full course.
- Be sure to have modern antihistamines recommended by an allergist in your home medicine cabinet.
Author:
Pugonina Tatyana Alekseevna, Therapist
How to treat urticaria using traditional methods
The question that concerns all patients who develop urticaria is what to do and how to treat it? Whatever the cause of urticaria, treatment must begin with eliminating the cause of its occurrence. A mild form of the disease can be cured using traditional methods.
Advantages of traditional methods:
- Treatment is carried out at home;
- Natural ingredients are used;
- There is no need for large financial expenses.
Disadvantages of traditional methods of treating urticaria :
- A lot of time is spent on preparing products;
- It is dangerous to treat a severe disease with such drugs.