Diabetic foot is a broad concept that refers to the destruction of the skin, bones and nerves in the feet that develops in patients with diabetes and can lead to the death of the limb.
The main cause of diabetic foot syndrome (DFS) is damage to blood vessels by atherosclerotic plaques and mediocalcinosis (hardening of the vessel walls), characteristic of diabetes mellitus. Blood flow is disrupted, ulcers and gangrene develop, and wounds may not heal at all.
In addition, diabetics develop peripheral nerve damage (neuropathy), which reduces the sensitivity of the skin of the legs and the secretion of sweat. Patients with neuropathy do not feel pain from minor injuries and may not notice them until the wounds turn into trophic ulcers.
A dangerous factor for complications in diabetes is severe immunodeficiency. It promotes the unlimited spread of infection through soft tissues and the development of general blood infection - sepsis.
Only a comprehensive impact on all factors of the syndrome can successfully prevent amputation and death of these patients.
How to cure diabetic foot?
The Innovative Vascular Center is a unique medical institution for our country, where modern approaches have been introduced in the diagnosis and treatment of pathology of the lower extremities in diabetes. Our specialists perform microsurgical operations for diabetic gangrene, which allow most patients to save their legs, and also carry out a full medical examination and management of patients with diabetic foot syndrome.
At the Innovative Vascular Center in Moscow, Voronezh and Pskov, a full diagnosis of changes in nervous tissue and blood vessels characteristic of diabetes is carried out. The patient is examined by an endocrinologist, neurologist and vascular surgeon. Diagnostic tests are carried out to determine the state of immunity, the degree of arterial damage is assessed using expert ultrasound diagnostics, and laboratory and microbiological studies are carried out.
Each of our outpatient centers employs a specialist, a podologist, who conducts periodic examinations of the feet of patients with diabetes, since timely diagnosis of problems helps to avoid dangerous complications. If hyperkeratosis develops, only a podiatrist can safely treat the foot and nails.
Every 6 months we prescribe an ultrasound scan of the arteries of the lower extremities and once a year we perform x-rays of the foot bones. This approach makes it possible to prevent the development of problems in patients with diabetes in advance.
Amputation for diabetic feet can be avoided. At the Innovative Vascular Center, high amputations are not performed for purulent complications of the diabetic foot, but are successfully treated by restoring blood flow using endovascular methods (balloon angioplasty and stenting of the arteries of the leg) or microsurgical bypass methods. In the presence of extensive wounds, we use effective local treatment using vacuum technologies and perform reconstructive plastic surgeries of any complexity.
What to do to avoid surgery?
Firstly, if an ulcer appears (any defect in the skin of the foot or leg) and does not heal for several days, you need to start treatment with a qualified specialist at the Diabetic Foot office. Yes, not all doctors are equally helpful, but when treated by a qualified and experienced specialist, healing occurs faster, even with such a dangerous disease as a diabetic ulcer.
- Contrary to popular belief, treating a diabetic ulcer is not just a bandage with ointment, but also:
- Correctly prescribed antibiotics
- Timely suspected bone lesion
- Arterial blood flow disturbances detected and corrected in a timely manner
- Properly applied foot relief devices
- Modern dressing materials
- Normalization of glucose and cholesterol levels
All this, applied in time, allows you to cure a diabetic ulcer without foot surgery.
A separate problem is osteomyelitis (purulent bone lesions).
Previously, it was believed that if a bone is affected by this process, then it is impossible to cure it without surgery, and this bone must be removed (usually as part of a “minor amputation” (within the foot)). But since 2007, international recommendations (IWGDF), and since 2015 – Russian ones, indicate that an alternative to surgical bone removal can be a long (usually about 1.5 month) course of antibiotics. It is also possible to undergo treatment without amputation by removing only the affected part of the bone (called partial bone or joint resection or “virtual amputation”).
Secondly, it is important to identify diabetic ulcers in a timely manner, since in many patients they are painless and are detected in later stages - for example, when a wound infection occurs. To avoid missing any damage, it is important to examine your feet (including the soles of your feet and between your toes) daily or at least several times a week. This often requires the help of relatives.
Thirdly, minor injuries leading to diabetic ulcers can be avoided by following special protective rules. You can find out more about them here.
That is, the development of an ulcer can be prevented, but if it has developed, it should be identified and treated in the early stages.
Take care of your feet!
We wish you to visit the Diabetic Foot office only for a preventive annual examination.
Neuropathy
Neuropathy - damage to sensory nerves occurs in 70% of patients with diabetes. Nerves in the legs are particularly susceptible to damage because poor diet and high sugar levels destroy the myelin sheath. In the neuropathic form, where a diabetic patient loses sensation in the legs, any microtrauma may go unnoticed until serious ulcers develop.
Signs of foot neuropathy:
- Numbness of the skin
- Tingling
- Pain or burning of the skin of the legs (some forms of neuropathy may cause pain)
Gymnastics for feet
A set of such exercises should be performed daily. The main rule for their implementation is to regulate the force load on the affected limbs after consultation with a specialist.
Standard set of exercises:
1. Manipulations on a chair. In a sitting position, you need to straighten your back and fix your leg at an angle of 90 degrees with your toe raised up. Fixing the leg in this position should last 5 seconds, followed by changing the lower limb. Then you need to perform similar manipulations with the lowered toe of the foot.
2. Exercise with paper. An A-4 sheet of paper must be placed on the floor. The patient’s task is to move the paper, alternately changing legs, from side to side. Then the exercise is complicated by chopping the sheet and repeating the described movements.
3. Lifts and squats. Leaning on any surface, you need to carefully rise and fall on your toes. The exercise becomes more complicated by squats with smooth rolls from heels to toes with increasing speed of movement.
4. Rope exercise. The object is placed on the floor with one end, and the other is held tightly in the hands. The rope should be under the foot, but not around it. The point of the exercise is to make forward-returning movements when pulling on an object.
5. Warm up with a ball. The spherical body should not exceed the size of a soccer ball. When performing movements, you need to make sure that your foot does not slip while rolling the object on the floor.
6. Exercise on the mat. In a lying position, you need to raise your legs at an angle of 90 degrees and bring your feet together without excessive zeal. The exercise will not be completed right away, so you should not rush to avoid damaging the ligaments.
Angiopathy
In diabetes, damage to blood vessels often occurs - angiopathy. They become covered with atherosclerotic plaques, which leads to circulatory failure in the foot. It looks a bit like rusty pipes. Very little water comes out of the tap due to rust blocking the inside of the pipes. The same thing happens when blood vessels are clogged. If the vessels in the legs become clogged or completely blocked, the skin and tissues will suffer first from poor circulation. The process of delivering oxygen and nutrients to the limb will be disrupted, which means cell death in the affected area.
- Decreased ability to fight infection
- The ability to heal wounds will decrease.
- Signs of blood vessel damage
- Pain in the lower leg when walking,
- A change in the normal color or temperature of the feet,
- Leg pain at night or while resting.
If nerve damage is combined with poor circulation, the risk doubles. You are more likely to get injured (because you don't feel pain) and the injury will lead to infection or ulceration. Healing will not occur due to poor circulation, which will inevitably lead to gangrene.
Risk factors for developing diabetes include poor diet and glucose control, poor circulation, smoking, and diabetes mellitus of more than 10 years.
The effect of drugs in the treatment of disease
Insulin. Diabetics of the first type are prescribed injections to prevent gangrene, while diabetics of the second are prescribed glucose-lowering medications in the form of Maninil. When diagnosing the initial development of pathology, Difort has proven himself to be excellent.
Painkillers. Elimination of spasm is impossible with the use of many analgesics. Pain syndrome can be effectively blocked only after consultation with an endocrinologist. Self-medication can provoke hyperglycemia.
Antibiotics. If blood sugar levels are elevated, the effect of drugs from this pharmacological group may be blocked. This warning especially applies to people with type 2 diabetes. Penicillin is usually prescribed taking into account 2 weeks of use with a further break until new doctor’s appointments. For severe infections, antibiotics with a wide range of effects on the body will be needed. Semi-synthetic drugs such as Clindamycin may be prescribed.
Medicines for microcirculation. Pentoxifylline is a drug that acts as an angioprotector on the body. The advantages of the drug are a decrease in blood viscosity and additional oxygen supply to the tissues of the lower extremities. Pentoxifylline is contraindicated in patients undergoing breastfeeding and during pregnancy. The drug can be replaced with Latren, Trental and Agapurin.
Medicines for tissue restoration. Solcoseryl is an oily substance that helps block the progression of ulcerative lesions. As a contraindication, the instructions state only one point - individual intolerance to the medication. Before applying Solcoseryl, the wound must be dried using disinfectants. Drugs with a similar effect on the affected areas of the foot are Adgelon, Actovegin, Vitadent and Methyluracil.
Antidepressants. The disease is associated with many inconveniences that can provoke apathy. SSRIs (Duloxetine, Velafax) and tricyclics (Elavil) will help to cope with it.
Vitamin therapy. Diabetes mellitus is a pathology that is accompanied by a lack of B vitamins. A diet in the form of fish, beef liver, dairy products and oats will not in all cases compensate for the loss of this organic compound. Neuromultivita or Milgamma injections can effectively replace the lack of vitamin B.
A new approach to solving the problem. The remedy from Havana in the form of the wound healing agent Heberprot-p is contraindicated only in the case of diagnosing tumors that are actively progressing. Such injections are prescribed in the presence of ischemic ulcers, when there may be a threat of amputation of the affected foot.
Prevention of diabetic foot:
To minimize the risk of developing pathology, the following preventive requirements must be observed:
1. Maintain personal hygiene. In addition to washing your feet daily, you should avoid hot water procedures using sea salt.
2. Daily study of the condition of the feet. This manipulation must be performed in bright light. It is advisable to purchase a special mirror for a more detailed study of the sounded area.
3. Compliance with the rules of wearing shoes. Insoles are not an annoying addition to boots and shoes, but an important part of them. Giving up socks is also dangerous for people diagnosed with unstable blood sugar levels.
4. Proper cutting of nails. You should forget about the beautiful frame of the plate in the form of a semicircle. Nails must be cut at a precise right angle.
5. Timely help to yourself. One ingrown horny plate on the leg can turn into a big problem. If any defect is found, you should contact a specialist.
Classification
Neuropathic form - impaired sensitivity of the feet like stockings or socks, dry skin, small cracks are possible. Nerve damage is a common complication of diabetes mellitus, sensitivity disorders occur in the feet, up to its complete loss, damage to the motor nerves leads to muscle atrophy. In the neuropathic form, some patients do not feel injury, temperature, skin punctures and receive injuries that can lead to infection.
Osteopathic form - destruction of bones and joints leading to foot deformation, the formation of trophic ulcers and skin damage. Poor circulation weakens bones, and can cause the bones and joints in the foot and ankle to deteriorate. Weakness of the ligamentous apparatus leads to multiple dislocations of the bones of the foot and its deformation. Bone destruction and pathological fractures are not accompanied by pain symptoms and can occur unnoticed by the patient, up to perforation of the skin by a bone fragment. In such cases, purulent complications and wet gangrene develop unnoticed.
The ischemic form is a violation of the blood supply to the foot with the formation of trophic ulcers and dry gangrene. It develops when blood flow is blocked due to plaque blocking the arteries. Against the background of ischemia, dry necrosis of the fingers or feet is observed, easily turning into wet gangrene. The most dangerous thing with diabetes is that, in conditions of decreased sensitivity, the patient may not pay attention to the appearance of trophic ulcers and necrosis and progress his disease to diabetic phlegmon.
Diabetic phlegmon and gangrene are severe purulent destruction of the soft tissues and bones of the foot against the background of impaired blood circulation. Cellulitis can develop with preserved vascular patency, and gangrene only with blockage of the arteries of the leg. The causes of phlegmon and gangrene are different, but the result is usually the same - amputation. Only timely specialized surgical care can count on the preservation of the supporting limb. The frequent appearance of purulent and putrefactive infections is associated with impaired immunity, characteristic of patients with diabetes; in the neuropathic form, attention to injuries is reduced, and the infection easily enters the subcutaneous tissue, causing the development of diabetic phlegmon. Phlegmon is a purulent melting of soft tissue. It can be caused by various microbes, but the most dangerous are the causative agents of gas gangrene. Infection in diabetes quickly leads to intoxication and sepsis. With the development of sepsis, the patient's general condition sharply worsens, liver and kidney dysfunctions are noted, and severe pneumonia often develops. In the absence of a timely diagnosis and proper treatment, the prognosis for life is extremely unfavorable.
Also in the classification there is a mixed form of diabetic foot, which gives a variety of symptoms and requires appropriate treatment.
Basic rules for foot care
Diabetic feet need to be cared for daily, following simple rules of prevention:
- careful hygiene, including the interdigital space;
- treatment of keratinized areas with pumice;
- moisturizing dry skin with cream;
- Regularly changing socks. Socks and stockings must be made of natural fabric and selected exactly in size so that folds and gathers do not form and the tissues of the foot and lower leg are not compressed;
- wearing loose, comfortable shoes.
In addition, it is important to carefully trim your nails in a straight line, not to use medicinal products without a doctor’s prescription, to do daily exercises to improve blood flow, and to undergo regular medical examinations.
What not to do:
- walk barefoot even after all ulcers and other injuries have healed;
- be exposed to hypothermia;
- warm your feet by rubbing, steaming and using a heating pad;
- cover the damage with a band-aid without consulting a doctor. You should only use special dressings prescribed by your doctor.
Flow
When the development of diabetic foot begins, diet and control of sugar levels, proper foot care, periodic examination of the feet and timely monitoring by a doctor are extremely important. In this case, complications rarely develop. In European countries where podiatry services are developed, the development of diabetic gangrene is very rare. The number of amputations due to diabetes in Europe has decreased tenfold, but in Russia diabetic gangrene is the main cause of high amputation rates.
Complications
The extreme and most dangerous stage of DFS is the development of gangrene of the foot. Diabetic foot is the leading cause of non-traumatic amputation in peacetime. Every year in Russia 70,000 amputations are performed for diabetic gangrene.
Diabetic gangrene often occurs with an associated anaerobic infection. With this outcome, the damaged tissues die, and the blood and healthy tissues become infected. The disease develops very quickly, often leading to death.
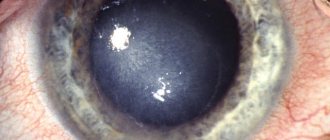
Trophic ulcers are another complication, most often found on the sole or big toe. They can also form on the sides of the foot from poorly fitting shoes. If left untreated, they can lead to serious infections. The classification of complications of diabetes includes trophic changes in the skin of the foot.
Stages of development
The University of Texas classification of diabetic foot syndrome includes 4 stages of development of the purulent-necrotic process:
- 0 – There is no ulcerative defect.
- 1 – There is a superficial ulcer without signs of inflammation.
- 2 – Deep ulcer, the bottom of which is a tendon or joint capsule.
- 3 – Deep ulcer with abscess and osteomyelitis (purulent melting of bone tissue).
- 4 – Deep ulcer, the bottom of which is a bone or joint [6].