03.02.2021
The onset of old age is often accompanied by a deterioration in health; older people suffer from chronic diseases and their exacerbations. One of the most severe conditions that are diagnosed in old people is gangrene of the lower extremities. The disease is characterized by its insidiousness and rapid increase in symptoms, leads to disability of the sick person and can cause death.
Few people know that, in accordance with the current legislation of the Russian Federation, elderly parents have the official right to receive financial assistance from their children. Alimony can be received by pensioners, persons with disabilities who have lost the ability to independently provide for their existence. If the future heir refuses to voluntarily fulfill the obligations assigned to him, the elderly parents can go to court.
What is gangrene
Gangrene is the process of tissue death of body parts or organs with a color change in the area of death from blue to black. The darkening of the tissue is caused by the presence of iron sulfide, which is formed when hemoglobin in the blood is destroyed. This disease can affect not only the limbs, but also the lungs, intestines or gall bladder.
Based on the type of dead tissue, gangrene is divided into dry and wet.
With dry gangrene, which most often affects the extremities, the blood vessels become clogged slowly. This process takes months or even years. The body's protective reaction allows it to independently isolate healthy tissue from damaged tissue (usually the fingers or feet are affected first). The dead tissue dries out, while practically no decay occurs, there is no smell or intoxication of the body. If dry gangrene does not turn into wet gangrene, then there is no direct threat to the patient’s life, but there is a danger of complications. To avoid complications, as well as for cosmetic purposes, blackened necrotic tissue is amputated.
Wet gangrene develops acutely, as a result of rapid blockage of blood vessels, while infection is always present. The root cause of the disease is frostbite, injury, burn or acute arterial insufficiency. The affected tissue is enlarged in volume and filled with hydrogen sulfide, has a corpse-like appearance and smell, and color ranges from greenish to purple. To save the life of an elderly person, surgical removal of the diseased organ is performed. Both limbs and internal organs can be affected.
Gangrene
Dry gangrene
As a rule, dry gangrene develops in cases of gradual disruption of blood supply.
It is more often observed in dehydrated, malnourished patients, as well as in patients with a dry physique. It is usually limited and not prone to progression. In this form of gangrene, tissues wrinkle, dry out, decrease in volume, become denser, mummify, and become black with a bluish tinge or dark brown. In the initial stages of gangrene, the patient experiences severe pain in the limb area. The skin in the affected area first turns pale, then becomes marbled and cold. The pulse in the peripheral arteries is not detected. The limb becomes numb, sensitivity is impaired, but pain persists even during the period of pronounced necrotic changes. Prolonged pain during gangrene is caused by a long period of preservation of nerve cells in the lesions and compression of the nerve trunks due to reactive swelling of tissues located proximally (closer to the center of the body) from the lesion.
Dry gangrene begins in the distal (remote) parts of the limb, and then spreads upward to a place with normal blood circulation. A demarcation shaft is formed at the border of affected and healthy tissues. If the necrotic area is not surgically removed, it gradually breaks away on its own, but this process takes a long time.
At the initial stages, it is very important to prevent the transition of dry gangrene, with its relatively favorable course, into a more dangerous and severe form - wet gangrene. Therefore, before the tissue begins to dry, it is necessary to ensure strict adherence to the rules of asepsis. The affected areas are covered with dry sterile wipes, and regular dressings are performed.
The disintegration of necrotic tissues in dry gangrene is practically not expressed. The small amount of absorbed toxins, the absence of intoxication and the satisfactory general condition of the patient make it possible not to carry out early surgical treatment. Surgery for this form of gangrene is usually performed only after the demarcation shaft has completely formed.
Wet gangrene
Wet gangrene usually develops in conditions of a sudden, acute disruption of the blood supply to the affected area. Overweight, “loose”, pasty patients are more prone to this form of gangrene. In addition, wet gangrene occurs with necrosis of internal organs (lungs, intestines, gall bladder).
With wet gangrene, necrotic tissue does not dry out. Instead, a center of rot is formed. Decay products from this focus are absorbed into the body, causing severe intoxication and seriously affecting the general condition of the patient. Microorganisms multiply intensively in dead tissues. Unlike dry gangrene, with wet necrosis, necrosis quickly spreads to neighboring areas. The demarcation shaft is not formed.
At the initial stages of development of wet gangrene, the skin on the affected area becomes pale, cold, and then acquires a marbled color. Significant swelling occurs. Dark red spots and blisters of exfoliated epidermis appear on the skin, and when opened, bloody contents are released. Upon examination, a bluish venous network is clearly visible. The pulse in the peripheral arteries disappears. Subsequently, the affected area turns black and disintegrates, forming a foul-smelling grayish-green mass.
The condition of a patient with wet gangrene deteriorates sharply. Severe pain, decreased blood pressure, increased heart rate, significant increase in temperature, lethargy, lethargy, and dry mouth are noted.
Due to the deterioration of the general condition and intoxication caused by the absorption of tissue breakdown products, the body's ability to resist infection is sharply reduced. Gangrene spreads quickly, affecting the overlying sections. In the absence of timely specialized care, sepsis develops and death occurs. A particularly severe course of gangrene is observed in patients with diabetes mellitus. This is due to deterioration of microcirculation, metabolic disorders and a decrease in the overall resistance of the body.
To prevent the spread of infection during wet gangrene, removal of the affected tissue (amputation or necrectomy) is performed as early as possible.
Gangrene of internal organs
Clinical signs of gangrene of internal organs depend on the location of the pathological process. In conditions caused by necrosis of the abdominal organs, symptoms of peritonitis are observed: fever, intense abdominal pain, nausea and vomiting that does not bring relief. Upon examination, a sharp pain when pressed is revealed. The muscles of the anterior abdominal wall are tense. Specific symptoms are determined (Shchetkin-Blumberg, Voskresensky, Mendel). A characteristic symptom is a symptom of imaginary well-being - sharp pain at the time of perforation, which then decreases, and after 1-2 hours intensifies again.
With gangrene of the lung, there is a high temperature, heavy sweats, lethargy, increased heart rate and decreased blood pressure. The patient's condition is serious and rapidly deteriorating. When coughing, foul-smelling sputum is released, which, when settled, is divided into three parts: the lower part is a thick crumbly mass (destroyed lung tissue), the middle part is brown liquid mixed with blood and pus, and the upper part is foamy. Multiple moist rales are heard in the lungs.
Causes of gangrene
- Impaired blood supply to tissues (incorrectly applied plaster, which restricts the movement of blood, heavy pressure on the body. For example, in car accidents or under rubble, when a medical tourniquet is applied for a long time to stop bleeding). Basically, in such cases, the limbs are damaged and a dry type of gangrene develops.
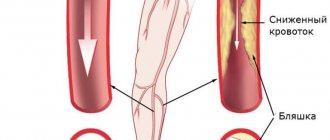
- Diseases of the heart or blood vessels (atherosclerosis, thrombosis and others).
- Bacterial infection (microbes that get into the wound - streptococci, proteus, enterobacteria, etc. can give rise to the disease).
- Frostbite, burns, including chemical burns (in damaged areas, blood supply is disrupted and inflammation begins, which, if infected, can provoke disease).
- Mechanical injuries aggravated by infections.
Prognosis and prevention
The prognosis for this disease depends on the type of gangrene and the degree of damage.
If left untreated, any gangrene can be fatal. However, gas gangrene, Fournier’s gangrene, gangrene of internal organs and wet gangrene are considered the most dangerous due to their rapid development and general intoxication of the body.
Dry gangrene is less likely to be life-threatening, but it also causes a high level of disability in patients. If you seek medical help in a timely manner, you can prevent not only death, but also the loss of a limb or affected organ.
Preventive measures aimed at preventing the development of gangrene can be divided into several groups:
- General strengthening. This includes recommendations for reducing total body weight in case of obesity, diet, quitting smoking and alcohol, and organizing moderate physical activity (fast walking, cycling, swimming). According to research, daily walking in combination with conservative therapy is effective in treating diagnosed gangrene of the feet in the early stages of the disease (when there is already necrotic tissue, but there is no necrosis of entire areas of the foot - one or more toes, etc.).
- Monitoring the course of chronic diseases. If you have atherosclerosis or diabetes mellitus, you should not only monitor your diet, monitoring the level of sugar and lipids of various fractions in the blood, but also undergo regular examinations with your doctor (the doctor, at his discretion, prescribes the necessary tests, uses ultrasound diagnostic methods, etc.).
In addition, you should avoid excessive hypothermia and frostbite of the extremities, try to avoid injury to the skin, scratches, and abrasions. If they occur, treat the wound to prevent infection.
Why does gangrene of the lower extremities begin in old age?
Of all the types of this disease, the most common among older people is gangrene of the lower extremities.
- weakened state in old age;
- prolonged immobilization;
- lack of vitamins;
- smoking, alcoholism;
- somatic diseases;
- metabolic disorders in the body;
- hypothermia of the body.
The causes of gangrene of the lower extremities in older people are very different. A significant proportion of those suffering from this disease are patients with diabetes, since high blood sugar destabilizes the functioning of all organs and systems, including the functioning of blood vessels.
The underlying factor of the disease is poor circulation in older people. Not enough nutrients and oxygen enter the tissue, so the ability to heal wounds deteriorates. Even small wounds, scratches, and cuts become non-healing ulcers.
Causes
Impaired blood supply to tissues is now one of the most common causes of gangrene. In this case, the tissues do not receive enough oxygen and necessary nutrients, which leads to changes in their structure, and subsequently necrosis. The pathological condition can occur with the development of various peripheral arteries, as well as against the background of:
- Diabetes mellitus.
- Atherosclerosis.
- Oncological diseases.
- Diseases of the endocrine system.
Another common cause of gangrene is the activation of pathogenic microorganisms, most often bacteria. Against this background, tissue destruction and death occurs. As a rule, processes occur when the immune system is weakened and various infectious diseases develop. In particular, gas gangrene is caused by the anaerobic pathogen Clostridium.
Factors that provoke tissue necrosis include physical and chemical influences that lead to tissue damage. The pathological condition often occurs due to thermal, radiation or chemical injury.
Symptoms of dry gangrene of the leg in the elderly
- this type often appears in weakened old people, thin and prone to dehydration;
- at first the person feels acute pain in the limb (until the tissue dies), the skin is pale and cold;
- it is not possible to feel the pulse in the arteries of the diseased leg;
- often gangrene begins from the toe of an elderly person and reaches a place with normal blood flow (the lesion is limited to a certain area and does not spread to a healthy neighboring area);
- gradually the tissue dries out, wrinkles and decreases in volume, mummification occurs;
- a sick person cannot move his leg and does not feel it;
- fabric color - from dark brown to bluish-black;
- the line between healthy and necrotic tissue (demarcation) is very pronounced;
- if medical amputation is not done, then sometimes the body independently rejects necrotic tissue;
- the patient feels relatively well, there is practically no intoxication.
Symptoms and complications
Areas affected by gangrene are usually warm and swollen.
The skin may be pale at first, but soon turns red or brown and finally greenish-black. The affected area may become severely scarred and require reconstructive surgery. If significant tissue death occurs, the affected body part may even need to be removed. Sometimes a brown liquid forms under the skin, causing large blisters to grow. If clostridia is the cause of gangrene, gas produced by the bacteria may be seen in these blisters.
Substances produced by bacteria are very toxic to human tissue and kill healthy cells by reducing oxygen levels. If the infection does not stop, these bacterial toxins will soon enter the bloodstream and begin to poison vital organs (so-called toxic shock), causing immediate kidney failure.
Symptoms of wet gangrene
- wet gangrene of the leg usually begins in an overweight, edematous elderly person;
- the skin is initially pale and cold, severe swelling is observed, the venous network is visible, the pulse in the arteries of the leg cannot be felt;
- dark red spots appear on the skin;
- inflammation progresses rapidly, there is no demarcation shaft between healthy and diseased areas;
- the affected tissues do not dry out, but turn black and decompose (there is a strong smell of rotting);
- decomposition products enter the bloodstream and severe intoxication occurs;
- the elderly person’s condition is very serious, he is bothered by intense pain and high fever; pulse is increased, blood pressure is low;
- the patient's refusal to eat and drink;
- spread of infection leads to sepsis and death.
How to properly treat gangrene?
The first thing you need to know is that self-medication can lead to dire consequences, so you should abandon this idea. No need to waste time, make an appointment with a doctor immediately.
An exceptionally experienced specialist will be knowledgeable about how gangrene on the arm can be cured, etc., and will therefore be able to prescribe treatment for you without the need for amputation.
gangrene treatment
To avoid negative consequences, it is necessary to restore normal blood circulation, so doctors prescribe minimally invasive endovascular operations on arteries and vessels to patients with gangrene on the arms and legs. In addition, specialists can resort to necrectomy, which will ensure that there is no need for amputation.
In what cases should you urgently consult a doctor?
There are a number of symptoms, the appearance of which may indicate a predisposition or the onset of gangrene of the leg in an elderly person, and requires contacting a medical institution for consultation and diagnosis of the disease:
- constantly cold feet (even in the summer heat);
- fatigue when walking and pain in the legs;
- cramps in the limbs;
- poor healing of even minor wounds;
- loss of sensation in the affected area;
- change in the skin from pale to bluish or marbled, and then to black (in later stages of the disease);
- the patient's refusal to eat and drink;
- non-healing ulcers.
Under no circumstances should these symptoms be ignored. There is a very fine line between dry and wet gangrene, which develops rapidly and poses a threat to the life of an elderly person, especially if the elderly person has high blood sugar. Immediate consultation with a doctor, prevention and treatment will help prevent the development of a serious illness leading to disability and death.
Diagnostics
Diagnosis of gangrene is not difficult and includes:
- Inspection of the affected area (visual);
- Arterio- or phlebography;
- Ultrasound Doppler examination of blood vessels;
- Rheovasography;
- CT and MRI;
- Duplex scanning with contrast agent;
- General blood analysis;
- Blood chemistry;
- Bacteriological examination of biomaterial taken from the affected area.
A correct diagnosis can be made in all cases.
Treatment
Most often, gangrene appears in an elderly bedridden person. The first thing such a patient needs to do is check the capacity of the blood vessels and organize special care for him.
Beginning ischemic gangrene in the lower limb requires urgent restoration of blood circulation. To limit the affected area and preserve the supporting function of the limb (in more advanced stages), operations are performed on the blood vessels, and then, after restoring blood supply, dead tissue is removed or the affected part of the limb is amputated (depending on the extent of the damage). Untreated dry gangrene in the vast majority of cases is complicated by damage to the heart, lungs, liver or kidneys, which ultimately leads to death.
In the infectious form of this disease, to save the patient's life, amputation is carried out immediately, and tissues and organs damaged by gangrene are treated with penicillin injections.
Results of gangrene treatment in our clinic
The effectiveness of treatment in our clinic can be determined in 95% of saved “hopeless” limbs. Such good results are achieved through the use of modern methods of restoring blood flow and the use of reconstructive plastic surgery technology. More than 80% of our patients arrive after unsuccessful treatment in other vascular surgery clinics, and we are most often able to help them. In 2011, our clinic became and for many years remains a leader in the treatment of patients with damage to the arteries of the leg and foot, performing more than 500 reconstructive vascular operations at this level annually.
Prevention of gangrene in private nursing homes “Longevity”
In the Longevity boarding houses, elderly guests are provided with comprehensive services, including regular examinations by doctors, as well as a set of preventive measures to prevent the development of this serious illness. At the initial stage, the disease can be prevented or the process of necrosis can be stopped in time. Experienced boarding house specialists know how gangrene begins in the elderly, what it looks like, so they can easily detect not only the beginning of gangrene, but also its precursors by the symptoms.
In addition, our guests are provided with:
- full care and supervision for the elderly and sick 24 hours/7 days a week (for bedridden patients - special medical beds with anti-decubitus mattresses);
- 5-6 balanced meals a day (dietary meals are prescribed if necessary);
- comfort in the rooms, choice of accommodation (1, 2, 3-bed rooms);
- individual psychological assistance, organized leisure, walks, interest groups.
The boarding houses are located in quiet and cozy places in Moscow and the Moscow region (in Ramenskoye, Vidnoye, Zelenograd, Belozerki). All houses have their own fenced area with picturesque nature.
Our guests, no matter how severe their illnesses, do not feel lonely and abandoned. Here they always feel support, help and confidence in the future.
How to get treatment
- Make an appointment with a leading specialist in the treatment of critical ischemia and gangrene, Ph.D. Kalitko Igor Mikhailovich, by phone (reception in Moscow on Saturdays).
- To consult directly at the clinic (in Klin) or to obtain information on emergency hospitalization, contact our chief physician Alexey Valerievich Sedov by phone.
- in a special section or use “Correspondence with a Doctor” to get preliminary consultation on documents and guidance on treatment methods and costs.
- You can make an appointment yourself using a special registration form, but the administrator will definitely call you back to confirm the appointment and clarify the reasons for your application.
Sources
- Bondarenko O.N., Ayubova N.L., Galstyan G.R., Dedov I.I. Transcutaneous oximetry in dynamic monitoring of patients with diabetes mellitus and critical ischemia of the lower extremities. Diabetes. 2013;16(1):33-42.
- Mitish V.A., Paskhalova Yu.S., Ushakov A.A., Slepnev S.Yu., Mishurinskaya E.A. The role of disarticulation and guillotine amputation of the leg in the strategy of surgical treatment of ischemic gangrene of the lower limb. Wounds and wound infections. Journal named after prof. B.M. Kostyuchenka. 2020;7(1):26-35.
- Barkhatova N.A., Abdulova Yu.B. Some clinical and laboratory risk factors for death in gangrene of the extremities. //Innovative science. - 2022. - No. 4.