What are varicose veins?
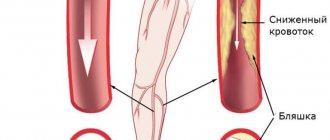
Varicose veins (in common parlance - varicose veins ) are overstretched, irregularly shaped, tortuous blood vessels that have lost their elasticity. They are increased in length and width and look like thick, convoluted blue strands that are visible under the skin. Veins become this way when the venous valves are missing or for some reason cannot perform their functions. If the valves do not work properly, blood flows through the veins in the opposite direction, downwards, accumulating in the lower sections of the veins and bursting their walls. As a result, the veins lose their natural shape, and a pathological chain of various complications begins.
Vessels: what you need to know?
22.10.2019
There are three main types of blood vessels in the human body: arteries , veins , and lymphatic vessels . They all look like a rubber pipe with many branches and different passages. pink arteries the veins are bluish and soft. Blood vessels are yellowish.
Story
Ancient anatomists connected arteries and veins with various organs. In the Middle Ages, scientists misunderstood the system of arteries ; they thought that they were not all connected to each other. This theory was refuted by the Italian physician Jacopo Berengario da Carpi at the end of the 15th century. He noticed that an artery is connected to every artery . In the 16th century, anatomists tried to answer the question of how blood gets from veins to arteries . This was clarified in the second half of the 17th century by William Harvey, who discovered blood circulation.
Under a magnifying glass
The wall of the vessel consists of three layers. Its inner part consists of a lining of flat cells (the so-called endothelium; the entire inner layer has other parts and is called intima). The middle layer consists of round and spirally oriented smooth muscle cells. The outer layer of the vessel is a compound that forms a flexible membrane (adventitia). The adventitia connects blood vessels and nerves to nourish and control vascular . Arteries have a thicker layer of muscle than veins . The capillary wall consists of a single layer of cells - the endothelium. In the veins, the endothelium forms a small pocket, a flap, in certain places, preventing blood flow. Blood vessels have a similar structure to veins .
Comparative anatomy of blood vessels
As is known, humans have a closed blood circulation. For example, mollusks, snails, arthropods and jellyfish have open blood circulation. Their “blood” or hemolymph, if present, is located directly between the organs of the body. Insects are less developed, they have only a simple tubular heart .
Anatomy
Blood vessels extend from the heart to all organs and cells. The aorta originates in the left ventricle, descends into the abdomen and flows into the pelvis, where it divides into two arteries that carry blood to the lower extremities. arteries (emanating from the aorta) also function blood to the head, upper limbs, all internal organs and skin. The arteries branch into smaller ones and eventually become capillaries. Arterial capillaries pass into venous capillaries, which converge further into veins . The superior vena cava carries blood to the heart from the lower extremities, abdomen and torso, and it also carries blood from the head and upper extremities. Blood vessels form blindly between cells flowing into stronger trunks and entering veins .
Functions
Blood vessels are used to transport blood in the body. A person has a so-called closed circulation. This means that blood flows only in blood vessels and does not accidentally “wash” certain organs. Arteries carry blood from the heart . Most of this blood is oxygenated, except for the blood that passes through the pulmonary artery from the right ventricle to the lungs . Veins carry blood to the heart . Except for the blood in the pulmonary veins , which is oxidized and flows into the left ventricle.
In the human body there are two circles of blood connected by the heart . The "small" or pulmonary circulation is where oxygenated blood is drawn through the pulmonary artery from the right ventricle into the lungs , where the pulmonary veins lead to the left ventricle. And the “large” circulation, where oxygenated blood from the left ventricle moves to the right atrium, and from there to other arteries and organs. There the blood loses oxygen and the veins return it to the heart . Blood vessels collect saliva in the intercellular spaces and transport it to the veins .
Published in Cardiology Premium Clinic
How common are varicose veins?
Varicose veins are one of the most common diseases of the vascular system. According to some statistical estimates, from varicose veins . The number of people who have varicose veins increases with age, and women are affected much more often than men. According to statistics, in the age group under 25 years only 8% of women suffer from varicose veins, and in the older age group - 55 years and older - 64% of women are affected by varicose veins.
How can you recognize varicose veins in yourself?
The most common sign of varicose veins is fatigue, dull pain, a feeling of heaviness and fullness in the legs after sitting or standing for a long time. Often these symptoms appear or worsen in the evening. However, it is usually impossible to determine exactly where it hurts. And if these unpleasant symptoms - fatigue, heaviness, pain - go away after resting with your legs elevated, then they are really caused by varicose veins (unless some other cause is reliably identified).
However, do not rush to blame everything on varicose veins, especially if there are no external signs in the form of dilated veins. Some other painful conditions may also exhibit the same symptoms.
Leg cramps
With varicose veins, painful nighttime cramps in the leg muscles can actually occur (in other words, “leg cramps”). Most often, cramps appear in the calf muscles and can sometimes be so painful that the patient wakes up. Moreover, night cramps usually occur after a hard day, when the patient had to stand or sit a lot.
Is varicose veins inherited?
It is now known that varicose veins are hereditary. Scientists even believe that they were able to isolate a separate gene responsible for the development of varicose veins. It is not yet clear whether this gene causes malformations of the venous valves or malformations of the vein walls themselves. But there is no doubt that these studies will help develop a gene therapy technique - perhaps the most promising way to prevent and treat varicose veins. Unfortunately, this is still a matter of the rather distant future, and gene therapy is not yet available to patients with varicose veins.
Varicose veins during pregnancy
Pregnancy does not cause varicose veins, but it is often a trigger for the appearance of varicose veins in those women who are predisposed to it. For example, in people with congenital insufficiency or even absence of venous valves. This fact has already been established quite definitely, because many pregnant women do not develop any varicose veins. Sometimes varicose veins appear only during the fourth, fifth or tenth pregnancy.
And in some women, they appear during pregnancy and disappear immediately after the birth of the child. Pregnancy acts as a triggering factor for varicose veins due to the fact that during pregnancy the content of sex hormones - estrogen and progesterone - in a woman’s blood increases sharply. These hormones, in high concentrations, help soften the venous walls, the veins stretch, and the valves cannot close normally because of this.
Physiology/hemodynamics
Normally, oxygenated blood leaves the left side of the heart through very large arteries. Which then branch into smaller and smaller arteries, then into arterioles and capillaries, which penetrate all organs and tissues of the human body. They are visible only under a microscope. The capillary bed connects the smallest arteries (arterioles) with the smallest veins (venules). Capillaries are very small vessels with very thin walls, thanks to which oxygen and nutrients easily flow from the blood into the tissues of the body. The tissues, in turn, release carbon dioxide and various waste products into the blood, which returns through the veins to the heart (Figure 1).
Picture 1.
Blood from the heart enters the large arteries (indicated in red), then it flows into smaller arteries and arterioles of the upper and lower extremities, as well as other organs and systems of the human body. Then the blood enters a network of tiny vessels - capillaries, which penetrate all human tissues and organs. The blood releases oxygen and various nutrients, and then returns through the veins (highlighted in blue) to the heart.
The venous system of the lower extremities consists of superficial and deep veins. Deep veins are large vessels through which the bulk of the blood moves due to the work of muscles. Superficial veins are smaller vessels that collect blood from the skin and subcutaneous tissue, and, due to the work of venous valves, move it upward, back to the heart. The superficial and deep veins communicate with each other through communicating or perforating veins, which are also equipped with valves. It is due to the operation of the valves that blood moves from the bottom up and from the superficial veins to the deep ones; such one-way movement is the key to the proper functioning of the veins.
Regulation of blood flow through the vessels is carried out by the nervous, endocrine system, as well as local vasoactive substances produced in tissues. This complex regulation allows blood flow to increase or decrease depending on the body's needs, for example, increased blood flow in the muscles during exercise, and decreased at rest. By changing the tone of skin vessels, body temperature is regulated. When it is cold, the blood vessels in the skin constrict, blood moves closer to the center of the body, due to this mechanism the body retains heat. On the contrary, when it is hot, the blood vessels in the skin dilate and the body gives off more heat. Various body injuries and injuries trigger processes that can cause blood flow to increase or decrease, for example, in the area of a skin burn or in a sprained area.
The walls of the veins are very thin and pliable, so the venous system can change its capacity to accommodate different amounts of blood. Blood volume is proportional to the pressure inside the veins. When the amount of blood in the veins decreases or its pressure on the vein walls decreases, the veins collapse like an empty balloon. When the volume of blood or its pressure on the walls of the vein increases, the veins expand, like an inflated balloon. If the pressure in the veins becomes very high, the venous wall stretches, its permeability increases and the vein allows fluid to pass through, which rushes into the tissue. This is how swelling occurs.
To maintain normal blood circulation in the body, the following 4 components are very important:
- Normal functioning of the heart, which, when contracting, works like a pump
- Pressure gradient between areas of low and high venous pressure
- “Muscular-venous pump” - the muscles of the lower extremities contract and work like a pump, pushing blood to the heart
- Normal, non-dilated, completely patent veins, with functioning venous valves
(1) The heart is the main pump of the human circulatory system. Blood moves through the arteries due to rhythmic heart contractions. It is important to understand that venous blood, after returning to the heart, must be pumped to the lungs, where it is enriched with oxygen. If the vein does not perform this function, as happens with heart failure, then venous blood stagnates and edema can appear even with absolutely normal veins.
(2) According to the laws of physics, any liquid moves from a high pressure zone to a lower pressure zone. The pressure difference between different zones is called gradient. There are such zones in the human body, thanks to which blood can move against the force of gravity. For example, the pressure in the veins of the lower extremities is higher than in the veins of the pelvis and abdominal cavity, and in the right parts of the heart it is even lower and may even be negative, which is why venous blood moves towards the heart. With some diseases of the lungs and heart, the pressure in the right parts of the heart may be increased, which can also lead to edema.
(3) “Muscular-venous pump” - like the heart, which pumps blood through the arteries, the muscles of the lower extremities contract to pump blood through the veins. The most important muscles performing the pumping function are the gastrocnemius muscles. There is also a venous network in the foot area; the muscles and ligaments of the foot also act as an additional pump. With each step, the muscles of the foot and lower leg contract rhythmically, pushing blood through the veins towards the heart, overcoming the effects of gravity. If a person leads a sedentary lifestyle and there is not enough activity in his life, the muscular-venous pump ceases to function normally and edema may appear. It can also occur as a result of injury or after a stroke. Sometimes the gait of older people changes, it becomes shuffling, the old people seem to shift from one foot to another. In this case, the muscular-venous pump also stops working and swelling may appear.
(4) Most veins in the human body are equipped with valves that allow blood to flow in only one direction. For the normal functioning of the venous system, the valves must be intact, that is, not damaged, and functioning correctly. As a result of contraction of the leg muscles, a portion of blood moves up through the veins, the valves allow blood to pass upward, and immediately close. They work like the rungs of a ladder, allowing blood to move forward towards the heart.
Figure 2.
The work of the “muscular-venous pump” is similar to a pump that pumps blood from the lower extremities to the heart. Due to the many valves with which the veins of the lower extremities are equipped, blood moves only in one direction: from the more superficial layers to the deep ones and from bottom to top, towards the heart. (a) When muscles contract, blood is forced out of the veins and moves upward. (b) When the muscles relax, the valves close, preventing blood from flowing back.
Each venous valve consists of two thin elastic flaps located opposite each other, opening and closing synchronously. If the vein dilates more than normal, as happens with varicose veins, the valve flaps cannot close and block the lumen of the vein, as a result, the blood moves in the opposite direction - this is called reflux. The flow of blood through a vein can also be disrupted if a blood clot forms that blocks the lumen of the vein. In both cases, venous pressure increases significantly, the vein wall becomes thinner as it stretches, and the liquid part of the blood seeps into the tissue, causing swelling. Edema is one of the main signs (symptoms) of improper functioning of the venous system.
If venous outflow is disrupted for a short time, for example after an air flight or prolonged static exercise, the main manifestation is swelling, which completely disappears overnight. If venous edema persists for a long time, for months, the skin and subcutaneous tissue begin to change, thickening and darkening may appear in the lower leg area, and subsequently infection, erysipelas, and microbial eczema may occur. All this can lead to the formation of long-term non-healing trophic ulcers.
Other causes of varicose veins
Such a widespread prevalence of varicose veins in highly developed Western countries is probably associated with the lifestyle of the population. For example, we spend a lot of time sitting on chairs. From kindergarten until graduation, a person sits for at least 40 hours a week (counting approximately 5 hours during the day in class, 3 hours in the evening doing homework, watching TV, and so on 5 days a week). Now let's multiply these hours by 10 months a year, and so on - up to 17 years. Then - work in some institution where you have to sit even longer. When a person sits in a chair, the veins running along the back of the thighs are compressed, and the calf muscles (the rhythmic contractions of which help move venous blood to the heart) do not work.
Another important factor is nutrition. In Western countries, people prefer a low fiber diet. With such a diet, fecal matter becomes denser, and constipation often occurs. When straining to move hard stool, the abdominal muscles tense and the pressure in the abdominal cavity increases significantly. High pressure spreads to the veins running along the back of the abdominal cavity and to the veins of the legs, which dilate, causing the venous valves to leak.
Anatomy of the veins of the lower extremities
The veins of the lower extremities are divided into superficial and deep.
Superficial veins of the lower limb
The superficial venous system of the lower extremities begins from the venous plexuses of the toes, forming the venous network of the dorsum of the foot and the cutaneous dorsal arch of the foot. From it originate the medial and lateral marginal veins, which pass into the greater and lesser saphenous veins, respectively. The plantar venous network anastomoses with the deep veins of the fingers, metatarsals and the dorsal venous arch of the foot. Also, a large number of anastomoses are located in the area of the medial malleolus.
The great saphenous vein is the longest vein in the body, contains from 5 to 10 pairs of valves, and its normal diameter is 3-5 mm. It originates in front of the medial epicondyle and rises in the subcutaneous tissue behind the medial border of the tibia, bends around the medial femoral condyle behind and passes to the anteromedial surface of the thigh, parallel to the medial border of the sartorius muscle. In the area of the oval window, the great saphenous vein pierces the ethmoidal fascia and flows into the femoral vein. Sometimes the great saphenous vein on the thigh and leg can be represented by two or even three trunks. From 1 to 8 large tributaries flow into the proximal portion of the great saphenous vein, the most constant of which are: the external genital, superficial epigastric, posteromedial, anterolateral veins and the superficial vein surrounding the ilium. Typically, tributaries flow into the main trunk in the area of the fossa ovale or somewhat distally. In addition, muscle veins can flow into the great saphenous vein. The small saphenous vein begins behind the lateral malleolus, then it rises in the subcutaneous tissue, first along the lateral edge of the Achilles tendon, then along the middle of the back surface of the leg. Starting from the middle of the leg, the small saphenous vein is located between the layers of the fascia of the leg (N.I. Pirogov’s canal) accompanied by the medial cutaneous nerve of the calf. That is why varicose veins of the small saphenous vein are much less common than the large saphenous vein. In 25% of cases, the vein in the popliteal fossa pierces the fascia and flows into the popliteal vein. In other cases, the small saphenous vein can rise above the popliteal fossa and flow into the femoral, large saphenous vein, or into the deep vein of the thigh. Therefore, before the operation, the surgeon must know exactly where the small saphenous vein flows into the deep one in order to make a targeted incision directly above the anastomosis. The constant estuarine tributary of the small saphenous vein is the fenopopliteal vein (vein of Giacomini), which flows into the greater saphenous vein. Many cutaneous and saphenous veins flow into the small saphenous vein, most in the lower third of the leg. It is believed that the small saphenous vein drains blood from the lateral and posterior surface of the leg.
Deep veins of the lower limb
The deep veins begin as the plantar digital veins, which become the plantar metatarsal veins, which then drain into the deep plantar arch. From it, blood flows through the lateral and medial plantar veins into the posterior tibial veins. The deep veins of the dorsum of the foot begin with the dorsal metatarsal veins of the foot, which drain into the dorsal venous arch of the foot, from where blood flows into the anterior tibial veins. At the level of the upper third of the leg, the anterior and posterior tibial veins merge to form the popliteal vein, which is located lateral and somewhat posterior to the artery of the same name. In the area of the popliteal fossa, the small saphenous vein and the veins of the knee joint flow into the popliteal vein. Then it rises in the femoral-popliteal canal, now called the femoral vein. The femoral vein is divided into the superficial vein, located distal to the deep vein of the thigh, and the common vein, which is located proximal to it. The deep vein of the thigh usually flows into the femoral vein 6-8 cm below the inguinal fold. As you know, the femoral vein is located medial and posterior to the artery of the same name. Both vessels have a single fascial sheath, while doubling of the trunk of the femoral vein is sometimes observed. In addition, the medial and lateral veins surrounding the femur, as well as muscular branches, flow into the femoral vein. The branches of the femoral vein widely anastomose with each other, with the superficial, pelvic, and obturator veins. Above the inguinal ligament, this vessel receives the epigastric vein, the deep vein surrounding the ilium and passes into the external iliac vein, which merges with the internal iliac vein at the sacroiliac joint. This section of the vein contains valves, in rare cases, folds and even septa, which causes thrombosis to be frequently localized in this area. The external iliac vein does not have many tributaries and collects blood mainly from the lower limb. Numerous parietal and visceral tributaries flow into the internal iliac vein, carrying blood from the pelvic organs and pelvic walls. The paired common iliac vein begins after the confluence of the external and internal iliac veins. The right common iliac vein, somewhat shorter than the left, runs obliquely along the anterior surface of the 5th lumbar vertebra and has no tributaries. The left common iliac vein is slightly longer than the right and often receives the median sacral vein. The ascending lumbar veins flow into both common iliac veins. At the level of the intervertebral disc between the 4th and 5th lumbar vertebrae, the right and left common iliac veins merge to form the inferior vena cava. It is a large vessel without valves, 19-20 cm long and 0.2-0.4 cm in diameter. In the abdominal cavity, the inferior vena cava is located retroperitoneally, to the right of the aorta. The inferior vena cava has parietal and visceral branches, which supply blood from the lower extremities, lower torso, abdominal organs, and pelvis. Perforating (communicating) veins connect the deep veins with the superficial ones. Most of them have valves located suprafascially and thanks to which blood moves from the superficial veins to the deep ones. About 50% of the communicating veins of the foot do not have valves, so blood from the foot can flow from deep veins to superficial ones, and vice versa, depending on the functional load and physiological conditions of outflow. There are direct and indirect perforating veins. Direct ones directly connect the deep and superficial venous networks, indirect ones connect indirectly, that is, they first flow into the muscular vein, which then flows into the deep vein. The vast majority of perforating veins arise from tributaries rather than from the trunk of the great saphenous vein. In 90% of patients, there is incompetence of the perforating veins of the medial surface of the lower third of the leg. On the lower leg, incompetence of the perforating veins of Cockett, which connects the posterior branch of the great saphenous vein (vein of Leonardo) with the deep veins, is most often observed. In the middle and lower thirds of the thigh there are usually 2-4 most permanent perforating veins (Dodd, Gunter), directly connecting the trunk of the great saphenous vein with the femoral vein. With varicose transformation of the small saphenous vein, incompetent communicating veins of the middle, lower third of the leg and in the area of the lateral malleolus are most often observed. In the lateral form of varicose veins, the localization of perforating veins is very diverse.
Varicose veins in older people
Why varicose veins more common in older people, and especially common in women?
1. To answer briefly - because their vascular system wears out with age and, sooner or later, fails. However, there are still many objective reasons why older women suffer from varicose veins more often than younger men and women. Firstly, since women generally live somewhat longer than men, there are correspondingly more elderly women than elderly men, and their veins have been working harder for a longer period of time.
2. Men don't get pregnant. Even if varicose veins that appeared in a woman during pregnancy disappear soon after the birth of the child, these veins were still abnormally enlarged within a few months. And with age, all the muscles of the human body, including the smooth muscles of the vascular walls, become less elastic than in youth. And the veins, which had already expanded once, during pregnancy, in old age again become a little wider than normal.
3. Nowadays, many women over the age of 30 are resorting to hormone replacement therapy, which was originally intended to relieve the unpleasant symptoms of menopause. There is no doubt that hormone replacement therapy helps women look younger, feel better, and generally cope with the menopause years more easily. Doctors' observations also confirm that hormone replacement therapy to some extent reduces the frequency of angina attacks and prevents a decrease in bone strength due to osteoporosis.
However, hormonal supplements at the same time soften the vein walls in the same way as increased levels of estrogen and progesterone during pregnancy. This side effect of hormonal pills is all the more dangerous because the walls of the veins are already becoming weaker - due to natural age-related changes in the muscle layer. So, additional clinical studies are needed to definitively clarify this issue.
What types of vessels are there?
All vessels in the human body can be divided into arteries, veins and capillaries
.
Despite the difference in size, all vessels are constructed approximately the same. The inside of their walls are lined with flat cells - endothelium. With the exception of capillaries, all vessels contain tough and elastic collagen fibers and smooth muscle fibers that can contract and dilate in response to chemical or nerve stimuli. Arteries
carry oxygen-rich blood from the heart to tissues and organs.
This blood is bright red
, which is why all the arteries appear red.
Blood moves through the arteries with great force, which is why their walls are thick and elastic. They are composed of a large amount of collagen, which allows them to withstand blood pressure. The presence of muscle fibers helps turn the intermittent blood supply from the heart into a continuous flow to the tissues. As they move away from the heart, the arteries begin to branch, and their lumen becomes thinner and thinner. The thinnest vessels that deliver blood to every corner of the body are capillaries
.
Unlike arteries, their walls are very thin, so oxygen and nutrients can pass through them into the cells of the body. This same mechanism allows waste products and carbon dioxide to move from cells into the bloodstream. The capillaries through which oxygen-poor blood flows are collected into thicker vessels - veins
.
Due to the lack of oxygen, venous blood is darker
than arterial blood, and the veins themselves appear bluish. Through them, blood flows to the heart and from there to the lungs to be enriched with oxygen. Vein walls are thinner than arterial walls because venous blood does not create as much pressure as arterial blood.
Types of varicose veins
Varicose veins are divided into two main groups:
- The first group includes primary varicose veins, caused by a hereditary predisposition to varicose veins.
- The second group includes varicose veins that appear after damage to the venous walls as a result of injury with the formation of blood clots in the veins or thrombosis.
When a clot or thrombus passes through a vein, the integrity of the venous valves is disrupted and secondary varicose veins are formed.
Varicose veins
Varicose veins are bundles of thin, purple or red veins that appear around the knees or ankles. (Sometimes such vascular “webs” can appear on the face, near the nose.) These vessels cannot be called varicose veins, since, by definition, varicose veins are veins that are increased in length and in diameter. In fact, these are slightly dilated venules (vessels connecting capillaries to the veins themselves), which are located close to the surface of the skin.
Such dilated venules appear due to increased levels of female sex hormones in the blood and are often found in women taking oral contraceptives. But venules can expand even in the presence of varicose veins of larger veins that do not appear externally. However, women with varicose veins often experience symptoms very similar to those of varicose veins.
Treatment of varicose veins
Treatment depends on the severity of the disease. If the disease does not manifest itself too strongly, then conservative treatment is best:
- regular rest with your feet up,
- elastic bandaging (or special elastic stockings),
- physical exercises for leg muscles.
If these measures are not enough, the veins affected by varicose veins must be surgically removed at the Phlebology Center. Or using new, experimental methods - elastic strengthening of the venous walls is carried out surgically. That is, a special elastic plastic cover is placed on the outer surface of the affected veins in places of varicose veins, where incompetent venous valves are located. And finally, to treat dilated venules or varicose veins of small veins remaining after surgery, sclerotherapy - that is, the introduction of sclerosing substances into the areas of dilation, which causes clogging of the pathological vein. Blood returns to the heart through normal venous vessels.
Abstract on biology on the topic “Vessels of the circulatory system: arteries, veins, capillaries” (8th grade).
The topic of the lesson is
“Vessels of the circulatory system: arteries, veins, capillaries.”
In the human body, blood continuously moves through a closed system of blood vessels in a strictly defined direction. This continuous movement of blood is called circulation
. It depends on the work of the heart, which serves as the main engine of blood. The heart pumps blood into the vessels, ensures its movement and return to the heart itself.
Circulatory system
= heart + blood vessels: arteries + veins + capillaries, which penetrate all human organs and tissues.
In humans
, like all representatives of the chordate type,
a closed circulatory system
, i.e. blood moves in our body only through blood vessels and does not spill into organ cavities and body walls.
Structure and functions of blood vessels
.
There are 3 types of blood vessels: arteries, veins and capillaries.
1. Arteries
- These are the vessels through which
blood flows from the heart to the organs.
" arterial walls
contain a lot of muscle cells, they are
very thick, multi-layered and elastic
, which allows them to withstand the pressure of blood pushed out of the heart;
« the inner layer of the walls consists of a single layer of flat epithelial cells;
« the middle layer is formed by smooth muscle tissue. He's fat
and its contraction promotes the movement of blood through the vessels;
« the outer layer of the images is dense connective tissue;
« the diameter of the vessel decreases in the direction from the heart to the organs;
“The speed of blood flow is approximately 0.5 m per second;
“blood pressure 120 mm. Hg Art.;
« blood amount: 17%.
Figure 1 – Features of the structure of arteries
2. Vienna
- These are vessels through which
blood flows from organs to the heart.
“The walls of the veins
are three-layered, less thick and elastic
than the walls of the arteries, but
more extensible;
“ The inner layer of the walls consists of a single layer of flat epithelial cells;
“ The middle layer is formed by smooth muscle tissue.
It is thin and has pocket-like valves
that prevent blood from flowing in the opposite direction;
« the diameter of the vessel increases in the direction from the organs to the heart;
“The speed of blood flow is approximately 0.2 m per second;
“blood pressure 10 mm. Hg Art.;
« blood amount: 67%.
Figure 2 – Features of the structure of veins
3. Capillaries
- these are the smallest vessels,
the walls of which are thin, single-layer, microscopic and formed only by epithelial tissue.
“ The diameter of the vessel is smaller than a hair;
“The speed of blood flow is approximately 0.05 mm per second;
“blood pressure 30 mm. Hg Art.;
« blood amount: 16%;
“they exchange fluids, nutrients and gases between blood and tissues (metabolism);
“The membranes of these cells have numerous holes that facilitate the passage of substances involved in metabolism through the capillary wall.
Figure 3 – Features of the structure of capillaries
Comparative characteristics of blood vessels
| Sign | Arteries | Vienna | Capillaries |
| Vessel function | carry blood from the heart to the organs | carry blood from organs to the heart | exchange of substances, gases between blood and tissues |
| Features of the structure of the walls | thick, multi-layered, elastic | three-layer, less thick and elastic than arteries, more extensible | thin, single-layer, microscopic |
| Availability of valves (no / yes) | No | There is | No |
| Outer layer | layer of dense connective tissue | No | |
| Middle layer of smooth muscle | thick | thin | No |
| Inner layer | consists of a single layer of squamous epithelial cells | ||
| Vessel diameter | decreases away from the heart | increases towards the heart | thinner than a hair |
| Blood flow speed, m, mm/s | 0.5 m per second | 0.2 m per second | 0.05 mm per second |
| Blood pressure, in mm. Hg Art. | 120 mm. Hg Art. | 10 mm. Hg Art. | 30 mm. Hg Art. |
| Amount of blood, in% | 17% | 67% | 16% |
Additional Information:
1. Large arteries are divided into smaller ones - arterioles
, which in turn branch into
microscopic capillaries that
intertwine all tissues.
The capillaries connect into thin venous vessels - venules
, which merge together to form
veins
.
Figure 4 – Blood vessels
2. Since the venous walls, unlike arteries, are not elastic, there is an auxiliary mechanism that promotes the movement of blood from the organs to the heart. Skeletal muscles located next to the veins stimulate blood circulation. When muscles contract, the venous vessels are compressed and push blood through. Blood cannot move in the opposite direction, since the veins have valves that open only in the desired direction. the muscle or venous pump works
Figure 5 – Venous pump
3. At the junction of the smallest arteries into capillaries there are accumulations of muscle cells. Contractions of these cells change the lumen of the vessels, open or stop the flow of blood into the capillaries. Typically, in a person at rest, only 20-30% of the capillaries are open to blood flow. During intense work, additional capillaries open and enter the bloodstream. This mechanism is especially well developed in athletes.
Figure 6 – Muscular regulators of capillary lumen
4. The largest artery of the body is the aorta. Its diameter in an adult is approximately 3-4 cm.
Complications during treatment
The main danger with conservative treatment (elastic stockings, exercise and resting with legs elevated) is its possible ineffectiveness.
Surgical treatment of varicose veins of the lower extremities should currently be performed by experienced vascular surgeons and phlebologists . Often complications and relapses after surgical treatment are caused by the fact that the operation was not performed by a specialist from the phlebology center.
With sclerotherapy, the main nuisance is small dark spots that can remain at the injection sites for several months, or in some cases forever.
Dilated veins after surgical treatment
If varicose veins have been removed, varicose veins will no longer appear in their place. However, sometimes varicose veins are found after surgery - in veins that were not previously affected, or in small veins that were not identified during the preoperative examination. Varicose veins after surgery appear because the blood is forced to find new outflow paths. At the same time, a larger volume of blood is redistributed to the remaining veins than before, and if there were any defects in the valves or walls, then new problems arise. New varicose veins, as a rule, bring cosmetic inconvenience and can be easily eliminated by a phlebologist using modern sclerotherapy techniques.
What is blood pressure?
Blood pressure is the force with which blood presses against the walls of the arteries. It increases when the heart contracts and pumps out blood, and decreases when the heart muscle relaxes. Blood pressure is stronger in the arteries and weaker in the veins. Blood pressure is measured with a special device - tonometer
.
Pressure readings are usually recorded in two numbers. Thus, normal blood pressure for an adult is considered to be 120/80
.
The first number, systolic pressure
, is a measure of the pressure during a heartbeat.
The second is diastolic pressure
- the pressure during relaxation of the heart.
Such dangerous excess weight
Professor Sergei Boytsov, chief specialist in preventive medicine at the Russian Ministry of Health and Social Development, talks about how extra pounds affect the heart and blood vessels.
Pressure is measured in the arteries and expressed in millimeters of mercury. In the capillaries, the pulsation of the heart becomes invisible and the pressure in them drops to approximately 30 mm Hg. Art. A blood pressure reading can tell your doctor how your heart is working. If one or both numbers are higher than normal, this indicates high blood pressure. If it’s lower, it means it’s reduced. High blood pressure indicates that the heart is working too hard: it requires more effort to push blood through the vessels. It also indicates that a person has an increased risk of heart disease.