With age, human articular and cartilaginous tissues lose their former elasticity, lose their functionality and are destroyed. Such changes can be delayed with the help of a number of drugs. Glucosamine chondroitin is a remedy that helps maintain the functionality of cartilage and joints, relieve symptoms of developing diseases of the musculoskeletal system and improve the quality of life of older people.
What are glucosamine and chondroitin?
Let's figure out what monosaccharides such as chondroitin and glucosamine are. There is such a thing as chondroitin sulfate. This substance is an essential component of cartilage tissue, which it produces independently. The compound is part of the synovial fluid that fills the joint capsule. These facts indicate that the full functioning of the joints depends on the presence of chondroitin.
Glucosamine acts as a building base for chondroitin and joint fluid. Its deficiency provokes a deficiency of chondroitin sulfate in cartilage tissues. The consequence of this may be the appearance of pain and crunching in the joints.
Indications for the use of glucosamine with chondroitin
The first, important factor indicating the need to take glucosamine with chondroitin is high physical activity. This can be not only the physical activity of athletes at the stadium or in the gym during training. This also includes groups of people whose daily activities involve constant movement, such as couriers who spend a lot of time on bicycles or loaders who strain their backs.
The second, no less important factor is age. In older people, the rate of synovial fluid production is reduced, and tissue elasticity is not the same as it was in youth. Any, even minor, loads lead to serious problems with the joints, since tissue cells can no longer recover at the required rhythm. People aged 65+ should discuss taking any medications with their local doctor, because there may be restrictions with certain concomitant chronic diseases.
The third factor indicating the need to supplement with chondroitin with glucosamine is the presence of injuries. Any damage to bones and joint tissues will be quickly forgotten, and motor activity will be restored if you help the body by taking chondroprotectors.
What is the difference between glucosamine and chondroitin?
One of the questions that people face before using drugs is what is the difference between glucosamine and chondroitin? These substances have the same structure. It is important to know that glucosamine is an essential component of chondroitin, which complements it and enhances its properties. The combination of these substances makes it possible to improve their absorption, provide effective protection and active restoration of cartilage. Most chondoprotectors are drugs consisting only of these components. There are also products in which chondroitin and glucosamine complement the composition.
Condition of cartilage in OA
Chondroitin sulfates are an important component of the main proteoglycan of the cartilage matrix - aggrecan, and are found in cartilage, skin, tendons, ligaments, arteries, and the cornea of the eye. Tendon proteoglycan components are important for mechanical properties. While collagen fibers allow tendons to resist tensile stress, proteoglycans allow tendons to resist compressive stress. The tightly packed and highly charged sulfate groups of chondroitin sulfate generate electrostatic repulsion, which provides much of the compression resistance of cartilage. Proteoglycan molecules are involved in the assembly of the intercellular matrix. They can form complexes with collagen, adhesive proteins and other proteins, protecting them with carbohydrate components from the action of enzymes. Proteoglycans are involved in regulating the activity of signaling molecules. They form a gel-like environment in which fibrillar and adhesive proteins are immersed. Glycosaminoglycans can bind large amounts of water, giving the extracellular matrix high viscosity (jelly-like properties) [8]. CS has the ability to suppress chondrocyte apoptosis. Cell protection occurs due to inhibition of protein oxidation reactions, lipid peroxidation and suppression of the formation of free radicals [9; 10]. An increase in the synthesis of type II collagen and proteoglycans was found with the administration of cholesterol [11]. A number of studies have shown an increase in the synthesis of hyaluronic acid by synovial membrane cells. In general, this indicated the anabolic properties of cholesterol [11, 12]. In OA, the most pronounced pathomorphological changes occur in the cartilage matrix. Strong and elastic cartilage turns into dry and dull, with a rough surface. The initial stage of OA is characterized by changes in the collagen framework, swelling and disintegration. Subsequently, degradation processes increase with the destruction of proteoglycans by proteases, which leads to thinning and softening of the cartilage in areas of maximum load. In later stages, fragmentation of the cartilage occurs with the formation of vertical cracks in it. Possible calcification of cartilage. When the cartilage cover is thinned, the pressure distribution between the articular surfaces becomes uneven. This leads to local overloads, the appearance of areas of osteosclerosis, subchondral cysts and the formation of osteophytes [13]. The mechanisms of degenerative processes are the same for the intervertebral disc and peripheral joints. Disc degeneration is mediated by impaired formation of proinflammatory mediators secreted by cells of the nucleus pulposus, annulus fibrosus, and macrophages. An increase in the concentration of cytokines in the tissues of the disc protrusion area suggests their likely role in the occurrence of endoneurial edema and demyelination of nerve fibers. By influencing nociceptors, cytokines play an important role in peripheral hyperalgesia and the formation of pain syndrome [14]. The effectiveness of chondroitin sulfate in the treatment of patients with osteoarthritis is the result of a large complex of biological reactions, including anti-inflammatory effects, stimulation of the synthesis of proteoglycans, collagen and hyaluronic acid, as well as a decrease in the catabolic activity of chondrocytes, inhibiting the synthesis of proteolytic enzymes, nitric oxide and other substances. The mechanism of action of chondroitin sulfate is complex, multifaceted and covers almost all key aspects of the pathogenesis of osteoarthritis. Chondroitin sulfate improves trophism and reduces resorption of subchondral bone, determines the viscosity of synovial fluid and the elasticity of cartilage. In addition, it is necessary to note its effect on the metabolism of subchondral bone, hydrophobicity and stimulation of the synthesis of hyaluronic acid, which contributes to the implementation of its main function by cartilage. It has been proven that the biological activity of cholesterol is carried out by influencing NF-kB (one of the main regulators of the inflammatory response), reducing the expression of IL-1β by chondrocytes and synoviocytes, reducing the concentration of pro-inflammatory molecules (CRP, IL-6), and inhibiting the expression of COX-2. [15, 16]
Properties, benefits and role for the human body
Speaking about why glucosamine chondroitin is taken, it is worth turning to the research of scientists. With long-term therapy with drugs that include this compound, pain relief in gonarthrosis in elderly patients is noted. Their quality of life improves as their joints become more functional. The need for non-steroidal anti-inflammatory drugs in this case is reduced (). The properties of glucosamine chondroitin allow the drugs they contain to perform the following functions:
- ensuring the regeneration of failed and damaged tissues;
- support of the process of cellular nutrition;
- prevention of the formation of age spots;
- fight against inflammatory processes in the gastrointestinal tract;
- preservation of tissue structure at the molecular level;
- preventing the appearance of vascular plaques.
Observations by scientists have led to the conclusion that glucosamine chondroitin is effective as a remedy against osteoarthritis. Its mechanism of action is based on triggering the active production of proteoglycans that have a healthy structure. The benefit of glucosamine chondroitin is that it prevents the destruction of cartilage tissue by inhibiting the activity of matrix metalloproteinase. This compound also helps prevent the spread of inflammatory processes ().
What are chondroprotectors?
Chondroprotectors for joints (powders for the treatment of joints) are slow-acting preparations that contain proteins necessary for the construction of articular cartilage, bones and other functional tissues of the musculoskeletal system. Chondroprotective drugs are used in complex therapy of diseases of the musculoskeletal system together with anti-inflammatory and other drugs. However, their main task is the prevention of degenerative changes in joints. Therefore, they are effective before the onset of the disease, as well as in its early stages.
Indications for use and instructions for use
According to the instructions for use, glucosamine chondroitin is prescribed in case of diagnosis of osteoarthritis, tendinitis, osteoarthritis and discosis. It is recommended to use drugs with this compound for people prone to injuries, such as dislocations and fractures. Glucosamine chondroitin should be used by people who engage in weightlifting, powerlifting or bodybuilding. Their body is subject to great physical stress, after which it needs help in recovery.
Popular release forms
Glucosamine chondroitin is available in the form of external and internal use. These can be creams, ointments, capsules, tablets and powders. Products for external use do not always give the expected results and do not act as quickly as drugs that need to be taken. Tablets may be slightly less effective than capsules because some of the active ingredient dissolves on the way to the intestines, causing it to lose its benefit. In addition, the tablet form of the drug can cause intestinal irritation. Capsules are more effective and safe. They do not contain additional components that provoke adverse reactions from the gastrointestinal tract, and deliver the active substance intact to the stomach, through the walls of which it is completely absorbed into the bloodstream. Powders are more convenient to use if it is difficult to swallow tablets or capsules.
How to drink glucosamine chondroitin: norm per day, dosage
Glucosamine chondroitin is a drug with a cumulative effect, which is why the duration of its use can be up to 12 months, depending on the clinical picture. Athletes are recommended to drink 1500 mg of the drug in 2 or 3 doses. The maximum daily dose of glucosamine and chondroitin for humans is 2000 mg. The drug is started to be taken in a small amount equal to 400 mg, increasing the dosage according to the dosage regimen. It is drunk during or after meals, since the effect of the active substance slows down on an empty stomach.
Contraindications and side effects
Do not take the drug if you are hypersensitive, or if you are pregnant or breastfeeding.
Contraindications to the use of glucosamine chondroitin are also:
- minor age;
- blood clotting disorder;
- diagnosing diabetes mellitus;
- presence of asthma or hypotension;
- disruption of vascular function, including thrombus formation.
When talking about whether glucosamine chondroitin is effective, it is worth taking into account the cumulative effect of the drugs. In order for the therapy to bring results, you need to take the drug for at least 6 months. Thorough research helped determine how safe long-term use of the drugs is. It is noted that effective relief of pain and restoration of joint functionality is observed both while taking the drugs without breaks, and when they are used in courses of 3 months with breaks of the same duration. Side effects of glucosamine chondroitin have been observed in isolated cases. These include abdominal pain after discontinuation of use and a papular rash during use (). In some cases, drugs can cause nausea, vomiting and diarrhea.
Treatment of osteoarthritis
Treatment of OA should be comprehensive.
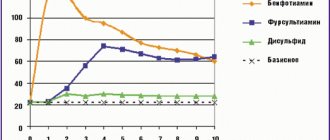
Recommendations for the management of OA, created by EULAR (European League Against Rheumatism) and OARSI (Osteoarthritis Research Society International), include non-pharmacological, pharmacological and surgical therapies [17, 18]. In 2003, the EULAR (European League Against Rheumatism) recommendations introduced a group of drugs called delayed-acting drugs (SYSADOA - symptomatic slow acting drugs for osteoarthritis), which have symptomatic and possible structure-modifying effects [15]. This group of drugs is very attractive in terms of the high safety profile of treatment [19]. None of the clinical studies revealed significant side effects of cholesterol, even with long-term treatment. The metabolism of cholesterol occurs without the participation of the cytochrome P450 system, therefore, the risk of developing adverse events when combined with cholesterol with other drugs is unlikely [16]. This is very significant for patients of older age groups, who have high comorbidity and the need for simultaneous use of a large number of medications. Currently, research is ongoing, and individual evidence of the structure-modifying effect of these drugs is accumulating. The most studied to date are chondroitin sulfate (CS) and glucosamine (G). Chondroitin sulfate has been used in practical medicine for more than 40 years. A feature of oral preparations of chondroitin sulfate is that 90% of low molecular weight derivatives of 10% of native molecules enter the systemic circulation. The bioavailability of cholesterol is determined by molecular weight, degree of sulfation, and the presence of impurities. On average, bioavailability is 10–20% [8, 15]. The maximum concentration of cholesterol in the blood is achieved 3-4 hours after administration, in the synovial fluid - after 4-5 hours. To achieve a sustainable clinical effect, regular use of the drug for 8–12 weeks is recommended. Many clinical studies have noted that the symptom-modifying effect of cholesterol, namely the reduction of pain, occurs much earlier than the structure of cartilage tissue is restored [14]. Nasonov E.L. and co-authors (2015) note the advisability of jointly prescribing slow-acting symptomatic drugs (MDSS) together with fast-acting analgesics (NSAIDs, paracetamol) and assessing their effectiveness no earlier than 1-2 months after the start of treatment, taking into account their ability to reduce the severity of MBS arising against the background of OA. If there is a good therapeutic effect and tolerability, the use of MDSS is possible for a longer period (≥ 6 months). However, if the diagnosis of OA is established, then it is recommended to prescribe a drug from the MDSS group with an assessment of effectiveness 1-2 months after the start of treatment. If pain is relieved or significantly reduced, the course of MDSS can be continued for another 3–6 months [5]. A systematic review by the Cochrane Musculoskeletal Group confirmed the benefits of chondroitin (versus placebo) and demonstrated positive structural changes in the affected joint. Forty-three randomized controlled clinical trials involving more than 9000 patients with OA (primarily knee OA) were selected for analysis. Of the entire sample, 4962 people took chondroitin as monotherapy or in combination with glucosamine, the remaining 4148 patients took placebo or other treatment. The analysis showed that chondroitin significantly reduces pain intensity in the short term. Compared to placebo, the improvement was 8 points on a 100-point scale. In a larger number of patients, compared with placebo, chondroitin reduced the intensity of pain in the knee joint with OA by 20%. This indicator was measured using the pain subscale of the WOMAC MCII (Western Ontario and McMaster Universities Osteoarthritis Index Minimal Clinically Important Improvement). According to the results, 53 out of 100 patients in the chondroitin group achieved a pain reduction of ≥20% and 47 out of 100 in the placebo group. Chondroitin appears to slightly improve quality of life as measured by the Lequesne index (pain + function + disability). The number of points scored in the active therapy group compared to placebo was 2 points lower (better) on a 24-point scale. According to instrumental diagnostic methods, chondroitin slightly slows down the narrowing of the intra-articular space in the affected joint. After treatment, the chondroitin group narrowed the joint space by an average of 0.18 mm less than the placebo group [20].
The evidence base has also accumulated regarding the use of glucosamine sulfate in OA [21, 22]. Glucosamine sulfate is a monosaccharide and a natural component of glycosaminoglycans in the articular matrix and synovial fluid, which has a specific effect on cartilage in OA, stimulates the synthesis of proteoglycans and hyaluronic acid by chondrocytes. It significantly reduces the activity of catabolic enzymes in cartilage, including matrix MMPs, suppresses the synthesis of nitric oxide, and stimulates the synthesis of chondroitinsulfuric acid. The sulfates contained in the molecule of this compound promote the formation of glycosaminoglycans, and the sulfide esters of the side chains of proteoglycans maintain the elasticity of cartilage and retain water in the cartilage matrix. There are different opinions about the effectiveness of individual glucosamine salts.
Some authors believe that only glucosamine sulfate has a symptom-modifying and structure-modifying effect. Other studies highlight that glucosamine hydrochloride and glucosamine sulfate are equally effective [23]. The bioavailability of glucosamine when taken orally is 25%. When taking glucosamine sulfate in therapeutic doses, glucosamine enters both the plasma and synovial fluid, with the concentration of the drug in the synovial fluid being 3.22–18.1 µmol/dL. The half-life of glucosamine is about 15 hours. Currently, cholesterol is available in the form of various dosage forms. One of these drugs is Artradol, which contains lyophilized CS powder for the preparation of a solution for intramuscular injection. The drug is made from high-quality raw materials using modern technologies. It has chondroprotective properties: suppression of the activity of enzymes that cause degradation of articular cartilage, stimulation of the production of proteoglycans by chondrocytes, enhancement of metabolic processes in cartilage and subchondral bone, positive effect on phosphorus-calcium metabolism in cartilage tissue. When administered intramuscularly, the drug accumulates in cartilage tissue, being detected after 15 minutes. in synovial fluid, after 30 minutes. found in significant concentrations in the blood. After 48 hours it reaches maximum concentration in articular cartilage. The properties of artradol are anti-inflammatory and analgesic effects. It reduces the release of inflammatory mediators and pain factors into the synovial fluid, influencing synoviocytes and macrophages of the synovium, suppressing the secretion of leukotriene B4 and prostaglandin E2. When using the drug, the cartilaginous surfaces of the joints are restored, the production of joint fluid is normalized, which leads to improved joint mobility and a reduction in pain.
Indications for prescribing artradol are: primary arthrosis, OA affecting large joints, intervertebral osteochondrosis. It is used intramuscularly, 0.1 g every other day (the contents of the ampoule must be dissolved in 1 ml of water for injection). If well tolerated, the dose can be increased to 0.2 g, starting with the 4th injection. The course of treatment is 25-35 injections. A repeated course is possible after 6 months, which is determined by the doctor. Use with caution if you are prone to bleeding, thrombophlebitis, during pregnancy and lactation.
Artradol indirectly prevents the formation of fibrin thrombi in the synovial and subchondral microvasculature due to its structural similarity to heparin [12, 16, 13].
Among the chondroprotectors, it is worth highlighting the drug "Artracam®", which compares favorably with capsules and tablets in its convenient dosage form - sachet. Sachet "Artracam®" is a powder in single sachets with a high content of glucosamine; it should be used by dissolving it in a glass of water only once a day. Due to the rapidly soluble form and high dosage, the bioavailability of the drug is increased; taking Artracam® begins to affect the course of the disease, helps reduce inflammation and pain, and also improves the production of synovial fluid in the joint. The drug is a domestic development and is produced at a pharmaceutical plant in the Russian Federation, which significantly reduces its cost in contrast to 167 imported capsules and tablets.
The effectiveness, tolerability and safety of the drug "Artradol" has been proven in the treatment of vertebrogenic glenohumeral periarthrosis [24], vertebrogenic cervicobrachialgia [25].
Lapshina S.A. and co-authors showed that combination therapy with the drugs “Artradol” and “Artracam” can be considered as an effective method for relieving pain and inflammation in OA, promoting rapid dose reduction and discontinuation of NSAIDs, including in patients with a serious risk of gastrointestinal and cardiovascular complications [26].
Thus, the interest of doctors of various specialties in slow-acting symptomatic drugs is increasing, taking into account their effectiveness and safety, the range of analgesic, anti-inflammatory, and chondroprotective properties.