Reception is conducted by:
Krivonosov Denis Sergeevich -
cardiologist, candidate of medical sciences
Make an appointment
Svitova Elena Olegovna —
Obstetrician-gynecologist. Functional diagnostics doctor. Ultrasound diagnostics doctor. Doctor of prenatal ultrasound diagnostics.
Make an appointment
Pelvic varicose veins (PVVD) is a chronic vascular pathology characterized by dilation of the pelvic veins. With the disease, the return flow of blood worsens, causing stagnation and poor circulation. Symptoms of pelvic varicose veins in women are nonspecific and are inherent in many gynecological pathologies, so literally a few decades ago the disease could not be diagnosed in time and only the symptoms were stopped, and their root causes were not eliminated.
According to a study conducted in 1999, in approximately 15-20% of cases in patients with vein disease, the reason for visiting a gynecologist was pain in the lower abdomen. However, the diagnosis was correctly made only in 2% of cases. It’s scary to imagine that about 15% of women had their uterus removed as a result of an incorrect diagnosis.
The Profimedica clinic employs professionals with extensive experience. Modern equipment from the world's best manufacturers allows specialists to diagnose and eliminate pathology at the earliest stages.
Causes of development of varicose veins of the pelvis
Today, the main cause of varicose veins is considered to be a history of pregnancy. The situation arises due to the fact that the growing fetus puts pressure on nearby organs and vessels, disrupting blood circulation. A healthy female body after childbirth is able to restore blood circulation on its own and no problems arise. However, under the influence of certain provoking factors, the tone in the vessels is not restored, leading to vascular pathology.
Factors contributing to the occurrence of the disease:
- excessive physical activity;
- sedentary lifestyle;
- diseases of the reproductive system (tumors, polycystic disease, endometriosis, etc.).
It is worth noting that varicose veins of the venous vessels of the pelvis can occur not only during pregnancy. Recently, scientists have been actively discussing the effect of hormonal contraceptives and hormone-containing drugs on the development of venous pathology. This assumption is based on the fact that the disease occurs much more often in women of childbearing age, which means hormones play a major role in this process.
Prices for phlebologist services
0
0 services selected for the amount of 0 rub.
| Total: | from 0 rub. | Sign up |
| Appointment (examination, consultation) with surgeon Globin A.V. (PhD) primary with ultrasound examination of the veins of the lower extremities | from 4000 rub. | Sign up |
| Microsclerotherapy (1 limb) (1 session) surgeon Globin A.V. | from 5400 rub. | Sign up |
| Microsclerotherapy (2 limbs) (1 session) surgeon Globin A.V. | from 7300 rub. | Sign up |
| Microsclerotherapy under ultrasound control or Venolight navigation (1 limb) (1 session) surgeon Globin A.V. | from 6400 rub. | Sign up |
| Microsclerotherapy under ultrasound control or Venolight navigation (2 limbs) (1 session) surgeon Globin A.V. | from 9200 rub. | Sign up |
| Endovenous laser surgery for varicose veins (1 limb) surgeon Globin A.V. | from 48400 rub. | Sign up |
| Endovenous laser surgery for varicose veins. CVI stage 1-2 (2 limbs) surgeon Globin A.V. | from 74600 rub. | Sign up |
| Endovenous laser surgery for varicose veins. CVI stage 3-4 (2 limbs) surgeon Globin A.V. | from 89300 rub. | Sign up |
Symptoms of varicose veins of the pelvis
All women of childbearing age need to be aware of the symptoms of varicose veins. Since the disease has a non-specific clinical picture, contacting a specialist is required when the following signs appear:
- Constant pain in the lower abdomen.
- When pain is relieved with analgesics and antispasmodics, the effect does not last long.
- The pain intensifies during and after sexual intercourse.
- There is a pronounced premenstrual syndrome.
- Painful sensations occur during hypothermia and overheating of the body, as well as during physical exertion and prolonged stay in one position.
In half of the cases with pelvic varicose veins, veins can be visualized in the area of the inner thigh, buttocks, and external genitalia. However, in the initial stages of the disease, this manifestation is absent, and it is quite difficult to independently suspect the pathology.
Medicine distinguishes 3 stages of the disease, depending on its severity. At the first stage, the diameter of the vein expansion is up to 0.5 cm. At the second stage, the expansion reaches 0.6-1 cm. At the third stage – over 1 cm.
Possible complications
Alarming symptoms of varicose veins of the small pelvis cannot be ignored. Without treatment, the disease can cause severe (sometimes fatal) consequences for a woman’s health.
Including:
- chronic inflammation of the genitourinary system;
- thrombosis;
- endocrine disorders;
- thromboembolism;
- severe uterine bleeding;
- infertility;
- thrombophlebitis.
Attention: exacerbation of varicose veins of the small pelvis during pregnancy threatens the life of the fetus.
A woman with vascular pathology has a high risk of premature birth, the birth of a baby with serious weight loss, and defective internal organs. In addition, the woman in labor may experience uncontrolled bleeding, which can be fatal. Most often, patients with varicose veins of the small pelvis undergo a cesarean section.
Diagnostics
Timely detection of the process of vascular dilatation increases the likelihood of its cure and prevention of relapses.
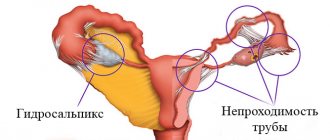
To diagnose pelvic varicose veins, doctors at our clinic use instrumental research methods. One of the most effective ways to detect the disease is ultrasonography. This method is carried out in conjunction with transvaginal and abdominal ultrasound, which allows specialists to obtain the necessary data for diagnosis. During ultrasonography, vascular dilation can be identified by multi-colored spots of irregular shape.
Another research method is laparoscopy. In this case, the presence of pathology is signaled by bluish-colored formations that have a thin, tense wall in the area of the uterine ligament or ovaries.
Recently, a modern diagnostic method – selective oophorography – has been gaining popularity. During the study, a contrast is performed on the patient's blood vessels, thanks to which the doctor is able to see any deviations in their structure.
A CT scan may also be performed. The method helps to see the vessels in the woman’s internal genital organs.
Pronounced discomfort during sexual intercourse and other unpleasant manifestations of the disease contribute to the deterioration of the psychosomatics of patients, which often causes diagnostic errors. The presence of a clear pathognomonic symptom, combined with the absence of signs of pathology of the pelvic organs during a traditional examination and manifestations of clear psychosomatic disorders, often leads specialists to think about the psychoneurological nature of the disease. As a result, instead of treating varicose veins, patients are prescribed consultations with sex therapists and psychotherapists.
Prevention
To minimize the likelihood of developing the disease, women need to follow a number of simple rules:
- stop smoking, alcohol abuse;
- do gymnastics daily, including exercises for the legs and abs;
- get rid of excess weight;
- girls working in the office should do a short warm-up every half hour;
- Healthy food;
- Don't get carried away with strength training.
Take any medications (including oral contraceptives) only as prescribed by a doctor. Women with a genetic predisposition and mothers of many children should contact a phlebologist to select compression garments.
Varicose veins of the small pelvis are a dangerous disease. The sooner you start therapy, the less harm the impaired blood circulation of vital organs will cause to a woman. Despite the fact that the only radical way to get rid of the problem of the disease is surgery, competent conservative treatment in the early stages allows you to achieve sustainable remission.
The medical service provides treatment for varicose veins at a high level. Already at the consultation you will receive a complete diagnosis of the venous system.
Treatment methods for pelvic varicose veins
At the Profimedica clinic, treatment of pelvic varicose veins is carried out in two ways: conservative and surgical.
In order to identify pathology, differential diagnosis is carried out using laparoscopy. The presence of varicose veins is indicated by bluish formations with a thin, tense wall in the area of the ovaries and the broad uterine ligament detected by this method.
Conservative treatment
The first method is used if the patient consults a doctor in the early stages of the disease. Conservative treatment methods include:
- Elimination of factors that provoke the development of pathology (change of sedentary or standing work, increased activity, etc.).
- Avoiding excessive physical activity.
- A balanced diet, including more fresh vegetables and fruits and excluding alcohol, cigarettes, fatty and spicy foods.
- Using a contrast shower to improve blood circulation in the body.
- Carrying out a daily set of exercises (“scissors”, “birch tree”, “bicycle”, etc.).
- The use of special breathing exercises, which are based on breathing using the muscles of the anterior abdominal wall.
- Constantly wearing compression tights.
- Taking medications that accelerate blood flow (phleboprotectors).
Surgery
If the disease was detected already in severe stages, or it was not possible to cure pelvic varicose veins in women using conservative methods, doctors may recommend surgical intervention.
During the operation, the surgeon eliminates the abnormal reflux of blood by passing through the dilated gonadal arteries. When eliminating the disease, as a rule, the method of embolization of ovarian vessels is used. For maximum precision of surgical intervention, all manipulations are carried out under the control of parallel angiography.
In rare cases, open resection or vein clipping techniques during laparotomy may also be used. In this case, the progress of the operation is monitored using an endoscope.
Our doctors
Malakhov Yuri Stanislavovich
Doctor - cardiovascular surgeon, phlebologist, Honored Doctor of the Russian Federation, Doctor of Medical Sciences, doctor of the highest category
Experience 37 years
Make an appointment
Drozdov Sergey Alexandrovich
Cardiovascular surgeon, phlebologist, Doctor of Medical Sciences
Experience 48 years
Make an appointment
Sclerotherapy for vulvar varicose veins - an alternative to phlebectomy?
Gavrilov S.G. , Zolotukhin I.A., Yanina A.M..
Moscow, Russia
Vulvar varicose veins (VV) are a pathognomonic symptom of pelvic varicose veins (PVD). The main methods of treating VV are phlebectomy with or without labiaplasty and scleroobliteration. Until now, there is no clear answer as to which treatment method for VV in VBT should be chosen; information about the possibilities of scleroobliteration of the vulvar veins in VBT is extremely scarce in the literature.
Purpose of the study
— to evaluate the possibilities and effectiveness of phlebectomy and scleroobliteration of the vulvar veins in VBT.
Material and methods.
In the clinic of faculty surgery of the Russian National Research Medical University named after. N.I. Pirogov from 2008 to 2014. 54 patients with VBT and V.V. were treated. A painless form of VVT was detected in 28 patients, a painful form - in 26. Instrumental examination included ultrasound angioscanning of the veins of the lower extremities and pelvis, scintigraphy of the pelvic veins. Patients scheduled for surgery on the ovarian veins underwent computed tomography or selective oophorography and pelvic venography. Combined interventions on the gonadal and vulvar veins were performed in 10 patients. Phlebectomy in the perineum was performed in 32 patients, 4 of them in combination with plastic surgery of the labia minora. Only scleroobliteration of the PV was limited to 12 patients. For scleroobliteration of veins, a 1% solution of ethoxysclerol or 0.5% fiberwein was used, the volume of which and the number of injections were determined individually, depending on the severity of varicose veins.
Results.
Indications for surgery on the ovarian veins were dilation and reflux of blood through them, and the presence of symptoms of pelvic venous congestion (PVP). All patients with VBT and VV underwent direct extraperitoneal resection of the gonadal veins and phlebectomy in the perineum, in 1 case with plastic surgery of the right labia minora due to its hypertrophy. The choice of such treatment tactics is due to the possibility of simultaneous surgical intervention on the pelvic and vulvar veins under general anesthesia and the inappropriateness of dividing the treatment process into two stages. There was no recurrence of VV and no symptoms of TVP for 3 years. Phlebectomy in the perineum was performed in patients with dilation of the pelvic venous plexuses and veins from small (up to 1 cm) incisions on the labia majora or minora, which ensured complete removal of the veins and complete hemostasis. The absolute indication for phlebectomy in the perineum was the presence of hypertrophy of the labia minora, which causes significant inconvenience to patients. Plastic surgery of the labia minora was performed in 4 patients. Relapse V.V. not detected during 3-year follow-up. Phlebectomy in the perineum is a simple and reliable method; its use is justified in patients with VBT with isolated dilatation of the pelvic venous plexuses and V.V. Scleroobliteration V.V. used as an alternative to phlebectomy in order to increase the cosmetic effect of treatment. Typically, no more than 2 injections of sclerosant with a volume of no more than 2 ml were necessary. A repeat session was performed after the symptoms of phlebitis of the vulvar veins subsided. No complications of the method (pelvic vein thrombosis, pulmonary embolism) were identified. Relapse V.V. noted in 2 patients who became pregnant in the near future (after 2 months). The remaining patients showed a persistent therapeutic and high cosmetic effect.
Conclusion.
The first experience of sclerotherapy for vulvar varicose veins showed that this method can be a safe alternative to phlebectomy in the perineum. The insufficiently large volume of accumulated data does not allow us to give unambiguous conclusions about the effectiveness of the method, however, we can already say that scleroobliteration can be successfully used in patients with VBT with isolated expansion of the pelvic venous plexuses without hypertrophy of the labia minora.
* * *
Possibilities of compression therapy for pelvic varicose veins
Gavrilov S.G. , Yanina A.M., Karalkin A.V., Belyaeva E.S..
Moscow, Russia
Conservative treatment of pelvic varicose veins (PVD) is limited to the use of venotonic drugs and non-steroidal anti-inflammatory drugs. Some authors recommend hormonal therapy, the effectiveness of which is questionable and associated with a large number of side effects. There are no indications in the literature on the use of compression therapy for VVT, although its capabilities in the treatment of chronic diseases of the veins of the lower extremities often exceed those when using drug treatment.
Purpose of the study
— to evaluate the possibilities of compression therapy for VBT using abdominal bandages of the 2nd compression class.
Material and methods.
In the clinic of faculty surgery of the Russian National Research Medical University named after. N.I. Pirogov from 2010 to 2014. 27 patients with VBT were treated. All patients had symptoms of pelvic venous congestion (PVP) - chronic pelvic pain (CPP), dyspareunia, hypogastric discomfort. Vulvar varicose veins were found in 7 patients. According to ultrasound angioscanning (USAS) of the pelvic veins, dilation and reflux of blood through the gonadal veins and pelvic venous plexuses were found in 6 women, isolated damage to the pelvic venous plexuses was detected in 21. To assess the degree of TVP, emission computed tomography (ECT) of the pelvic veins was performed according to the original method with calculation of the TVP coefficient (Ktvp). An abdominal bandage (shorts from the waist to the upper third of the thigh) of 2nd compression class was used as a means of compression treatment. The effectiveness of the treatment was assessed through repeated clinical examinations and ECT of the pelvic veins with the calculation of CTVP 14 days after the start of therapy. The main clinical indicator of the effectiveness of treatment was the dynamics of pelvic pain in the studied patients, assessed using the modified McGill scale.
Results.
The study showed that the use of compression abdominal bandages is most effective in patients with VAP with isolated expansion of the pelvic venous plexuses; their CPP decreased within 2 weeks of treatment from 6.4±1.2 to 3.6±0.9 points. The results of ECT of the pelvic veins indicated a decrease in the phenomena of TVP, KTP decreased from 1.93±0.22 to 1.34±0.32. In patients with lesions of the ovarian veins and venous plexuses of the pelvis, no significant clinical effect from the treatment was achieved (CPB before treatment - 7.8±1.6, CPP after treatment - 7.9±1.8) reduction in TVP, according to ECT , pelvic veins before and after treatment were 2.1±0.41 and 2.27±0.54, respectively. A negative point with the use of an abdominal bandage was the lack of compression effect in the perineum, where there is no elastic tissue. This point does not allow compression of the perineal veins, which is especially important in patients with vulvar varicose veins, as well as after scleroobliteration of the vulvar veins. No other negative effects of abdominal compression bandages were noted. Further treatment with their use was continued by 21 patients with isolated dilation of the pelvic venous plexuses. Surgical intervention on the ovarian veins was recommended for 6 patients with symptoms of TVP and dilatation of the gonadal veins. Phlebectomy in the perineum was recommended for 7 patients with vulvar varicose veins.
Conclusion.
Compression treatment of VBT using abdominal bandages (compression class 2 shorts) is an adequate method of conservative treatment of this disease. This treatment is most justified in patients with isolated enlargement of the pelvic venous plexuses. In combination with phlebotropic therapy, compression treatment can be used in patients with VBT who are scheduled for surgery on the pelvic veins.
* * *
Vulvar varicose veins: diagnosis, treatment, prevention
Gavrilov S.G. , Yanina A.M..
Moscow, Russia
Vulvar varicose veins (VV) are dilation of the veins of the external genitalia. This condition is noted in 1/3 of patients with pelvic varicose veins (PVD); during pregnancy, PV occurs in 10-18% of women at different stages and in 6% of them it persists after childbirth. There are different approaches to the diagnosis and treatment of VV; there is no indication of the possibility of preventing its development.
Purpose of the study
— to determine the optimal diagnostic and treatment algorithm for patients with VV, to determine methods for its prevention.
Material and methods.
In the Faculty Surgery Clinic No. 1 of the Russian National Research Medical University named after. N.I. Pirogov from 2000 to 2014. 97 women with V.V. were examined and treated. Of these, 54 patients suffered from VBT, 43 had a pregnancy with a period of 3-7 months. As the main method of examination, we used ultrasound angioscanning (USAS) of the pelvic veins and USAS of the veins of the perineum and lower extremities. These studies were performed in all patients with VBT. Indications for ultrasound examination of intrapelvic veins in pregnant women arose only in the presence of clinical signs of thrombophlebitis of the vulvar veins, thrombosis of the veins of the uterus and parametrium. Patients with VBT with pelvic pain and dilation of the ovarian veins underwent computed tomography or selective oophorography. Direct and endoscopic resection of gonadal veins or their endovascular embolization are used as methods of surgical treatment of VBT. Pregnant women with VV were prescribed conservative treatment. Treatment V.V. in patients with VBT without signs of TVP included phlebectomy in the perineum and scleroobliteration of the vulvar veins.
Results.
Ultrasound ultrasound is the routine method for examining the vulvar veins in all patients. It allows you to verify the diagnosis, carry out differential diagnosis with genital pathology, and confirm/exclude thrombotic lesions of the veins. It is advisable to perform USAS for all patients with VBT, and for pregnant women only if there are complaints of pain in the area of varicose veins, swelling of the perineum, and signs of thrombophlebitis. Ultrasound examination of intrapelvic veins in pregnant women must be carried out according to strict indications, namely: if thrombosis of the pelvic veins is suspected, or the presence of previous operations on the pelvic veins. This is justified by the fact that the statement of the presence of dilated veins of the uterus, parametrium, and gonadal veins in a pregnant woman does not affect the treatment tactics of V.V. Diagnostic and treatment issues in the absence of thrombotic complications should be resolved after childbirth and restoration of the menstrual cycle. Treatment V.V. during pregnancy, it is limited to the prescription of venoactive drugs (MOFF 1000 mg/day), heparin-containing ointments and gels, and the use of thick elastic underwear. Ligation or scleroobliteration of the vulvar veins is indicated only if bleeding from them develops. Removal of the vulvar veins outside of pregnancy is possible either alone or in combination with intervention on the gonadal veins if indicated. Scleroobliteration is also indicated for patients with VV, regardless of damage to the intrapelvic veins. Methods for preventing VVT include regular intake of venotonic drugs by patients with VVT, timely detection of VVT, and surgical interventions on the pelvic veins for VVT. During pregnancy from the second trimester, women with symptoms of chronic phlebopathology are also advised to take venotonic drugs.
Conclusion.
USAS serves as the main method for diagnosing V.V. Invasive radiation diagnostic methods should be used outside of pregnancy, for clear indications. Isolated interventions on the vulvar veins are possible in all patients with VVT, regardless of the prevalence of damage to the intrapelvic veins outside of pregnancy. Taking phlebotropic drugs and timely surgical interventions on the ovarian veins are the main methods of preventing the development of VVs.
* * *
Varicose veins of the vulva during pregnancy
Ivanov E.V., Ivanova O.E..
Tyumen, Russia
Varicose veins of the perineum and vulva, as a variant of pelvic varicose veins, appear in approximately 30% of pregnant women. This leads to significant emotional and physical discomfort, pain and, as a result, a decrease in quality of life. In addition, varicose veins of the vagina and labia can serve as a source of massive bleeding during spontaneous childbirth, so they are always given special attention by obstetricians and gynecologists. However, in recent years, the number of indications for caesarean section has decreased significantly.
Purpose of the study
— determination of the frequency of varicose veins of the vulva during pregnancy, assessment of the risk of bleeding, determination of indications for cesarean section for vulvar varicose veins.
Material and methods.
We studied the primary medical documentation of 200 patients observed for pregnancy at the Medical Center of the TGMA (all patients with varicose veins were examined by a phlebologist), as well as 86 patients referred for consultation with a phlebologist about varicose veins of the vulva during pregnancy from antenatal clinics. The incidence, timing of the appearance of vulvar varicose veins, the presence of concomitant varicose veins of the lower extremities, localization and volume of lesions, the risk of bleeding, recommended and used methods of delivery were assessed. The localization and volume of the lesion were assessed according to our proposed analogue scale: type 1 - single varix on the labia majora or minora (unilateral or bilateral); Type 2 - massive varicose veins of the labia majora and minora without vaginal varicose veins; Type 3 - single varix in the vagina; Type 4 - massive varicose veins of the vagina.
Results.
The incidence of vulvar varicose veins was 26% (52 out of 200 patients). In the examined 138 patients with this pathology, the period of appearance of varicose veins varied from 12 to 26 weeks, but in the majority (86%) it was 18-20 weeks. Early periods of the appearance of varicose veins were observed only during repeated pregnancies. The patients were examined 2 times - when referred for consultation (usually this coincided with the timing of the appearance of varicose veins) and at 36-38 weeks. The exception was 13 patients who contacted a phlebologist for the first time shortly before giving birth. Every second pregnant woman with vulvar varicose veins had concomitant varicose veins of the lower extremities. Single varixes on the labia majora or minora were found in 61 patients. Massive varicose veins of the labia majora and minora without varicose veins of the vagina - in 26. Single varicose veins in the vagina - in 38. Massive varicose veins of the vagina - in only 12 pregnant women. In 1 case, angiomatosis of the vaginal mucosa without varicose syndrome was observed. The risk of bleeding from varicose veins of the vagina and vulva during spontaneous childbirth is directly related to the location and extent of the lesion. All patients of groups 1, 2 and 3 are allowed to give birth independently. We recommended delivery by cesarean section only for patients with massive varicose veins of the vagina. However, 3 of them gave birth on their own; in 1 case there was moderate bleeding that required suturing of the veins.
Conclusion.
The risk of bleeding from varicose veins of the vulva and vagina during spontaneous childbirth is somewhat exaggerated. Caesarean section, previously performed even for minor vulvar varicose veins, in our opinion, should be performed only for massive varicose veins of the vagina.
* * *
Diagnosis of varicose veins of the pelvis in patients with prostate adenoma
Magomedov M.G. , Davudov G.D., Magamedov T.M., Gadzhimirzoev R.G. .
Makhachkala, Russia
In patients with prostate adenoma (PAA), an inflammatory process of the genitourinary system and pelvic varicose veins are often observed. The fundamental element of any inflammatory process is circulatory disorders (increased peripheral resistance, decreased elastotonic properties, arteriolar spasm, phlebostasis, increased vascular permeability, perivasal edema, formation of microthrombi) and pelvic varicose veins. Pelvic varicose veins (PVD) in patients with PVC is a poorly studied vascular pathology. It can manifest itself in the form of varicose veins of the intrapelvic venous plexuses, pelvic phlebitis, phlebothrombosis with venous hypertension in combination with varicose veins of the lower extremities and is often masked by various pathologies of the pelvic organs. At the same time, the lack of information provided by surgeons, urologists, therapists and other specialists about this disease leads to a high percentage of diagnostic errors and incorrect treatment tactics.
Purpose of the study
— to develop a diagnostic algorithm for IVVT in patients with PDA.
Material and methods.
In the urological departments of the Veterans Hospital, Municipal Hospital No. 1 of Makhachkala and the Regional Clinical Center of the Ministry of Health of the Republic of Dagestan, 347 patients with PDA aged 60 years and older were examined. After a clinical examination, the patients were examined jointly by a urologist and a vascular surgeon. Instrumental diagnostics included: ultrasound of the pelvic organs, transabdominal ultrasound angioscanning of the vessels (TAUSAS) of the pelvis, Doppler ultrasound (USDG) of the vessels of the lower extremities. The diagnosis of VVVT was confirmed in 125 patients of varying degrees of severity.
Results.
During the examination, the following diagnostic algorithm was followed. Clinical examination, complaints, anamnesis, international system of summary assessment of symptoms in prostate diseases and the question of quality of life, physical examination and digital rectal examination, urinalysis, determination of creatinine and urea in blood serum, analysis of prostate secretions, determination of prostate specific antigen, ultrasound of the prostate , bladder, kidneys, assessment of residual urine, TAUSAS, ultrasound examination were performed. Currently, preference is given to ultrasound methods - color mapping and spectral Doppler, which we used to study the blood circulation of the prostate gland and surrounding tissues. The following were studied: maximum systolic blood flow velocity (Amax), maximum diastolic blood flow velocity (Amin), pulsatility index (Pi) and peripheral vascular resistance index (Ri). The presence and severity of blood flow, as well as the diameter of the veins and arteries of the prostate gland and surrounding tissues were assessed. Thus, in case of ARV with IPVT, the average maximum blood flow velocities in the veins varied from 0.026 to 0.079 m/s, in the arteries - 0.125-0.170 m/s, the average diameter of the veins ranged from 5 mm and above. Depending on the maximum blood flow velocities in the veins and the diameter of the veins, we distinguish three degrees of severity of VVVT: 1st degree - vein diameter up to 5 mm, A max and A min - 0.054-0.079 m/s. 2nd degree - vein diameter from 6 to 10 mm, A max i, A min - 0.040-0.054 m/s. 3rd degree - vein diameter 10 mm or more, A max i, A min - 0.026-0.040 m/s.
Conclusion.
The variety of clinical manifestations of VVVT in patients with PDA dictates the mandatory use of modern non-invasive instrumental diagnostic methods. The presented algorithm allows us to improve the quality of diagnosis of VVVT, avoid errors in the correct choice of method of preoperative preparation, management of patients in the intra- and postoperative periods in terms of the prevention and treatment of thrombohemorrhagic and thromboembolic complications.
* * *
Foam sclerotherapy in the treatment of varicose veins of the external genitalia
Serazhitdinov A.Sh.
Chelyabinsk, Russia
Purpose of the study
— evaluate the results of foam-form sclerotherapy in the treatment of varicose veins of the external genitalia.
Material and methods.
From October 2005 to February 2014, we performed sclerotherapy for varicose veins of the external genitalia in 16 female patients with varicose veins of the external labia. In all cases, foam sclerotherapy was performed for obliteration of veins of various diameters. In 15 cases there were varicose veins of the left labia. 14 patients underwent 1 session of sclerotherapy, 2 patients received 2 sessions with an interval of 30 and 44 days. The age of the patients ranged from 24 to 48 years. During 1 session, from 2.0 to 4.0 ml of foamed 1% fiberwein solution was administered. The diameter of varicose veins varied from 6 to 12 mm in a vertical position. After sclerotherapy, it is recommended to wear tight “women's underwear” for 7 days. 3 patients with varicose veins more than 10 mm were prescribed preventive dosages of low molecular weight heparin for 3 days.
Results.
We were able to achieve stable obliteration of varicose veins when performing foam sclerotherapy in all cases. The second session of sclerotherapy was performed on two patients due to the large number of varicose veins. All patients noted complaints about discomfort in wearing tight “women's underwear.” In the long-term period, 11 women were interviewed in the period from 24 to 84 months. There are no clinical signs of relapse.
Conclusion.
Assessing the results of sclerotherapy for varicose veins of the labia, we believe that sclerotherapy is an effective method for obliterating varicose veins of the external genitalia.
* * *
Foam-form sclerotherapy in the treatment of varicose veins of the external genitalia
Serazhitdinov A.Sh.
Chelyabinsk, Russia
Purpose of the study
— evaluate the results of foam-form sclerotherapy in the treatment of varicose veins of the external genitalia.
Material and methods.
From October 2005 to February 2014, we performed sclerotherapy for varicose veins of the external genitalia in 16 female patients with varicose veins of the external labia. In all cases, foam-form sclerotherapy was performed for obliteration of veins of various diameters. In 15 cases there were varicose veins of the left labia. 14 patients underwent 1 session of sclerotherapy, 2 patients received 2 sessions with an interval of 30 and 44 days. The age of the patients ranged from 24 to 48 years. During 1 session, from 2.0 to 4.0 ml of foamed 1% fiberwein solution was administered. The diameter of varicose veins varied from 6 to 12 mm in a vertical position. After performing scelerotherapy, it is recommended to wear tight “women's underwear” for 7 days. 3 patients with varicose veins more than 10 mm were prescribed preventive dosages of low molecular weight heparin for 3 days.
Results.
We managed to achieve stable obliteration of varicose veins when performing foam-form sclerotherapy in all cases. The second session of sclerotherapy was performed on two patients due to the large number of varicose veins. All patients noted complaints about discomfort in wearing tight “women's underwear.” In the long-term period, 11 women were interviewed in the period from 24 to 84 months. There are no clinical signs of relapse.
Conclusion.
Assessing the results of sclerotherapy for varicose veins of the labia, we believe that sclerotherapy is an effective method for obliterating varicose veins of the external genitalia.
* * *
Ultrasound duplex scanning in the diagnosis and evaluation of the results of surgical treatment of varicose veins of the small pelvis
Fomina E.E., Ignatiev I.M., Bredikhin R.A..
Kazan, Russia
Purpose of the study
— to determine the possibilities of ultrasound angioscanning in the diagnosis of varicose veins of the small pelvis, to evaluate the results of surgical and endovascular treatment.
Material and methods.
116 women aged 24 to 56 years were examined (average age was 36.2±8.03 years). The 1st (control) group consisted of 30 (25.9%) relatively healthy women; they were examined using duplex angioscanning. The main group consisted of 86 (74.1%) women with symptoms of pelvic venous congestion. All of them underwent duplex scanning, then, according to indications, 55 women underwent pelvic venography (PF), and 17 underwent multislice computed tomography (MSCT). After an instrumental examination, 55 women from this group underwent surgery.
Results.
In the control group, the normal diameters can be considered the size of the arcuate veins up to 0.3 cm, the veins of the pampiniform plexus - 5 cm. In the main group, the average diameters of varicose arcuate veins on the right were 0.37±0.09 cm, on the left - 0.38± 0.07 cm. Unilateral dilatation of the veins of the pampiniform plexus was detected in 8.2%, bilateral - in 91.8%.
Dilated veins of the pampiniform plexus were divided into degrees: 1st degree - 0.5-0.8 cm, 2nd degree - 0.8-1.0 cm, 3rd degree - from 1.0 cm or more. Ultrasound criteria for left renal vein (LRV) stenosis: the average diameter of the LLV between the aorta and the superior mesenteric artery is less than 0.22 cm, the average blood flow velocity is more than 120 cm /
s; ectasia of the left vein in the proximal region more than 0.87 cm; ectasia of the veins of the pampiniform plexus on the left more than 0.88 cm; locating the left ovarian vein from the left renal vein.
Conclusion.
Arcuate veins, veins of the pampiniform plexus and parametric veins are identified in 100% of cases. Ultrasound criteria for the effectiveness of various types of surgical treatment is a significant reduction in the diameters of the veins of the pampiniform plexus.
* * *
Transvaginal ultrasound diagnosis of varicose veins of the pelvis in women with varicose veins of the lower extremities
Shulikovskaya I.V., Chizhova E.A., Tyuryumina E.E.
Irkutsk, Russia
Pelvic varicose veins (PVD) is a little-studied pathology, but with the development of medicine, and in particular ultrasound diagnostics, it has become possible to correctly diagnose this disease.
Purpose of the study
— to assess the incidence of pelvic varicose veins in women suffering from varicose veins of the lower extremities.
Material and methods.
The study included 36 patients with varicose veins of the lower extremities who were admitted to the vascular surgery department of the Irkutsk Regional Clinical Hospital for planned surgical treatment of this pathology. All patients had chronic venous insufficiency of the lower extremities II, III degrees. A thorough history taking was considered an important point in the study. The gluteal areas and perineum were also examined to identify varicose veins. We based our main diagnostics on the results of ultrasound duplex scanning (USDS). The Valsalva maneuver was used as a differential diagnostic criterion between primary and secondary varicose veins. When performing this test, an increase in the diameter of the veins by more than 2 mm was considered a sign of reno-ovarian reflux. There is currently no generally accepted classification of varicose veins of the small pelvis. But according to the results of sonographic studies, three stages of the process are distinguished. The 1st stage of varicose veins is determined when the diameter of the veins is 5-7 mm, covering the upper edge of the left ovary. At stage 2, the diameter of the veins is 8-9 mm, and they cover the entire left ovary. Varicose veins of the uterus and right ovary are identified. At the 3rd stage of the disease, the veins are 10-13 mm and are located below the lower edge of the left ovary with pronounced varicose veins of the uterus, pelvis and right ovary. At this stage, the diameter of the veins of the right ovary approaches the diameter of the left.
Results.
Our study showed that 27 (75%) patients had chronic pain in the lower abdomen, which occurred after prolonged static and dynamic loads and intensified in the second phase of the menstrual cycle. 22 (61.1%) patients had dyspareunia. And only 10 (127.7%) patients had varicose veins of the superficial veins in the perineum and gluteal areas. When performing ultrasound scanning, it turned out that 22 (61.1%) patients had pelvic varicose veins. In 15 (68.2%) patients the 1st stage of the process was identified, in 7 (31.8%) - the 2nd stage. The average diameter of primary varicose ovarian veins was 7.01±0.5 cm.
Conclusion.
Thus, VVBI is a fairly common pathology and requires further research. Focusing only on the clinical manifestations of the disease, one can suspect the disease only in a small percentage of cases. Therefore, ultrasonography acts as an indispensable assistant in making a diagnosis, being a minimally invasive and highly informative method for diagnosing varicose veins of the pelvis.