| Intrauterine infection (IUI) is an infection of a fetus that is still in the womb at any month of gestation. This increases the risk of abnormal development of the baby, mortality and disability. Today, even those mothers who try to lead a healthy lifestyle before conception and during pregnancy may have children with disabilities in physical and mental development. Statistics confirm this. |
- Facts about IUI
- How does an embryo become infected?
- Pathogens of IUI
- Consequences of intrauterine infection
- Risk groups for intrauterine infection
- Symptoms and consequences
- TORCH infections
- Diagnosis of intrauterine infection
During pregnancy, a woman experiences a natural decrease in immunity in absolutely all cases. This is the norm, a necessary process for bearing a child, preventing rejection of the fetus as a foreign organism in principle. Therefore, infections that were dormant before the moment of conception become active. This is dangerous for the fetus, especially in the first 3 months after conception.
Facts about IUI
In less than 10 out of 100 pregnancies, the infection is transmitted to the unborn baby from his mother. And approximately 0.5% of newborns are born with corresponding symptoms. But, if one or another infection is present in the mother’s body, this is not a complete guarantee that the child will also have it.
Some infectious diseases that threaten the development of the embryo are asymptomatic for the mother, without causing much harm to her body. Basically, the fetus becomes infected with the same infection as the mother if she became infected with the disease for the first time.
If a pregnant woman’s disease is detected and treated in time, the risk to the unborn baby is minimal.
How does an embryo become infected?
IUI develops in three ways:
- hematogenous or transplacental, such as viruses, listeriosis, toxoplasmosis, syphilis (infection in the first trimester leads to deformities of the baby and developmental defects; if the embryo is infected in the last 3 months of gestation, the newborn is born with symptoms of an acute form of the disease)
- ascending (this is how herpetic infection, chlamydia, mycoplasmosis can be transmitted; the child becomes infected through the woman’s genital tract, this mainly happens during childbirth. If the infection gets into the amniotic fluid, the child’s gastrointestinal tract, respiratory tract, and skin will be affected)
- descending (the infection reaches the embryo through the fallopian tubes, which happens if the mother develops oophoritis, adnexitis)
What infectious diseases during pregnancy can affect the development of the child?
Intrauterine infections are a group of diseases of the embryo, fetus and newborn that develop as a result of infection in the prenatal period or during childbirth, that is, in the ante- or intranatal period. Infection of the mother during pregnancy often leads to miscarriages and congenital malformations in the newborn. The causative agents of intrauterine infectious diseases can be viruses, bacteria, and sometimes parasites that cause obvious or hidden infections in the mother. Therefore, even at the stage of pregnancy planning, the doctor and the expectant mother need to pay attention to:
- sexually transmitted infections (STIs);
- bacterial infections;
- infections transmitted by protozoan microorganisms, fungi;
- cytomegalovirus infection;
- herpes;
- chlamydia;
- mycoplasma.
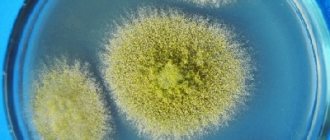
Pathogens of IUI
Most bacteria and viruses can be passed on to the unborn baby, causing serious consequences. Those viruses that provoke acute respiratory viral diseases do not reach the fetus. They can be dangerous for the baby only if the pregnant woman has a high temperature.
A mother can become infected with rubella through airborne droplets. It is not necessary to be close to a sick person; infection is also possible at a distance. In this case, the consequence for the fetus will be fetal rubella syndrome.
Cytomegalovirus is transmitted through body fluids. This is mostly saliva, but may include semen and urine, as well as blood. In a child, the infection may manifest itself with corresponding symptoms after birth, or it may occur in a latent form.
Herpes simplex virus 2 is transmitted mainly through unprotected sexual intercourse. If this happens to a pregnant woman, her child will be born with a congenital form of herpes. Parvovirus B19, like rubella, is transmitted by airborne droplets to a pregnant woman. As a result, the fetus develops dropsy and anemia.
Chickenpox is transmitted not only through the air, but also through household contact. A child receives developmental defects due to intrauterine infection (if the infection occurred in the first trimester). If the infection occurs before childbirth, then there will be a congenital form of this disease, and this is a very dangerous condition.
Listeriosis (a bacterial infection) can develop in a pregnant woman if she eats contaminated cheeses, meats or vegetables. The child eventually develops pneumonia and/or sepsis. Syphilis is transmitted to pregnant women through sexual contact if the partner has been infected. After birth, a child develops this disease with all the ensuing consequences. Tuberculosis, which is also a bacterial infection, is transmitted through the air. The embryo can die in the womb, be born prematurely, with a congenital form of tuberculosis.
Prevention of IUI
It is very important for a woman planning a pregnancy to take all possible measures to exclude the possibility of congenital infections in the newborn. First of all, you need to register with a gynecologist within 12 weeks. It is necessary to listen to the recommendations of specialists and conduct a full examination of the health of the expectant mother, including the following tests:
- flora smear;
- PCR test for the presence of chlamydia, mycoplasma, ureaplasma, herpes simplex virus, cytomegalovirus;
- serological blood test for toxoplasmosis, rubella, HIV, hepatitis and other infections.
It is also necessary to treat existing chronic foci of infection (caries, tonsillitis, genitourinary infectious diseases) and not forget about routine vaccination - vaccinations against measles, rubella, and influenza.
In addition, in order to exclude sexually transmitted infections, it is advisable to have your sexual partner examined, and of course, to avoid casual sexual relations.
“I wish you to give birth to a living, healthy child. So that further in life he only pleases you with his successes, first in his studies, and then further in his work. And for this we must, firstly, be ready and, secondly, we must be fully examined. That is, a woman who decides to become a mother must a priori be healthy.”
Ulukhanova Lala Udzhagovna, Doctor of Medical Sciences, professor, pediatrician, gastroenterologist, infectious disease specialist, nephrologist, pulmonologist in Makhachkala, specialist of the highest qualification category.
Consequences of intrauterine infection
Congenital infection can be acute or chronic. Consequences of acute infection:
- shock
- pneumonia
- severe sepsis
Symptoms of acute intrauterine infection in newborns:
- activity decreasing every day
- long sleep
- poor nutrition
But in most cases there are no symptoms. Long-term consequences of IUI:
- delayed motor development
- mental problems
- visual impairment
- partial or complete deafness
If the infection has penetrated the uterus, the consequences may be:
- stillbirth
- antenatal embryo death
- frozen pregnancy
- miscarriage
If the fetus survives, it will have the following manifestations of IUI:
- Fever
- Skin rashes
- Hydrops fetalis
- Anemia
- Jaundice and enlarged liver
- Pneumonia
- Myocarditis
- Chorioretinitis, cataract
- Micro- and hydrocephalus
Intrauterine infection is dangerous regardless of gestational age. But some pathogens are most dangerous in the first 3 months. A striking example is the rubella virus. Very serious consequences will occur if the mother is infected with chickenpox in the very last week of pregnancy. The consequences can be very different. You can find out about them from your doctor based on the results of ultrasound, tests, gestational age and the detected causative agent of the disease. This means that each case is individual in terms of the course of the disease and in terms of consequences.
What are the dangers of intrauterine infections?
There are so-called persistent infections, i.e. chronic, long-term infections. But they are not always transmitted from mother to child. Therefore, there is no need to worry too much that if the mother has an infectious disease, then it will be 100% transmitted to the fetus. The frequency of transmission of infection to the child in this case is not as high as in the case of primary intrauterine infection.
The greatest threat to the unborn child is posed by a mother who first becomes ill during pregnancy, especially in the first trimester. This period is the most dangerous. Therefore, I would like to urge all women - before planning the birth of a child, get tested for the presence of antibodies to such infections with similar epidemiological signs, such as:
- measles;
- parotitis;
- meningococcal infection;
- rubella;
- chicken pox;
- hepatitis.
Why? Because this is a group of infectious and inflammatory diseases that can be prevented in an expectant mother if she gets a vaccine on time 3 months before conception.
Apart from this, there are also early outcomes of infections. These are: myocarditis, pneumonia, malnutrition, anemia. There are late ones, when intrauterine infection may appear later. It happens that 5-6 years pass, and a child at this age may develop:
- delayed psychomotor development;
- delayed speech development;
- decreased visual acuity;
- hearing loss;
- hydrocephalus;
- microcephaly.
This also needs to be remembered and not forgotten.
Risk groups for intrauterine infection
Women who:
- live in a family with children who go to kindergarten, school, or other institutions
- work in the medical field, having contact with carriers of diseases or sick people
- work in preschool and school children's institutions
- have 2 or more medical abortions
- patients with inflammatory pathologies that occur in a chronic form
- have untimely rupture of amniotic fluid
- have a history of embryonic malformations and antenatal fetal death
- have once given birth to an infected child (one or more)
Symptoms and consequences
The following are signs that indicate an infection in a pregnant woman:
- cough, shortness of breath
- rash
- lymph nodes are painful and enlarged
- heat
- joint pain and swelling
- runny nose, lacrimation, conjunctivitis
- chest pain
But these symptoms in some cases indicate an allergic reaction. If this is so, then there is no risk of intrauterine infection of the baby. In any case, if one or more of the above symptoms appear, you need to go for a face-to-face consultation with a doctor.
CMV (cytomegalovirus)
CMV (cytomegalovirus) belongs to the group of herpes viruses. It is contracted through sexual contact, through close household contacts, and also through blood (if an operation was performed with dirty instruments or a transfusion from a sick donor). If there is a primary infection of a pregnant woman, the virus enters the placenta, and from there to the baby. The child may have no consequences, which is the case in most cases. But 10 out of 100 children who had sick mothers are born with symptoms of IUI.
The consequences of intrauterine infection with CVM can be miscarriages and stillbirths, as well as:
- sensorineural hearing loss
- underweight at birth
- hydrocephalus
- microcephaly
- pneumonia
- hepatosplenomegaly
- psychomotor development delay
- blindness of various degrees
If there is a severe combined lesion, 1/3 of newborns die in the first 2-3 months after birth. Long-term consequences such as mental retardation, blindness and deafness are also very likely. If the infection is mild, the consequences are less serious. Today there is no medicine that would help with the manifestations of cytomegalovirus in recently born children. If a pregnant woman is infected with CVM, the pregnancy is not terminated because the child may not have symptoms. Doctors prescribe treatment for a pregnant woman to minimize the development of complications.
HSV (herpes simplex virus)
Congenital herpes infection develops if the pregnant woman had HSV, especially type 2 (which is sexually transmitted). Symptoms appear in the first month after birth. Mostly, IUI occurs during primary infection of a pregnant woman. The child picks up the infection in most cases during childbirth, when he passes through the birth canal. But the possibility of transmission of the pathogen through the placenta also needs to be taken into account.
Consequences of herpes for a child:
- lethargy, poor appetite
- miscarriage, stillbirth
- characteristic skin rashes
- fever
- bleeding disorder
- jaundice
- brain damage
- eye damage
- pneumonia
Severe congenital herpes is fraught with disability for the child:
- vegetative state
- mental retardation
- cerebral palsy
Rubella
Rubella is very dangerous for the embryo! It causes various deformities. The highest risk occurs during pregnancy before the 16th week. Consequences of IUI caused by this disease:
- microcephaly
- low birth weight
- miscarriage, stillbirth
- heart defects
- deafness (in half of cases IUI)
- cataract
- skin lesion
- pneumonia
- hepatosplenomegaly
- meningitis and encephalitis
Parvovirus B19
This is the causative agent of infectious epithema. In adults it is mostly unnoticed because it occurs latently. If a pregnant woman is infected with it, she may give birth to a stillborn child, and there is a risk of miscarriage or intrauterine infection of the embryo. Children die in 2.5-10 cases out of 100. It is especially dangerous to become infected with it in the 13-28th week of gestation.
Consequences for a child with IUI:
- swelling
- anemia
- brain damage
- peritonitis
- hepatitis
- myocarditis
Chicken pox
If a patient contracts chickenpox, it is very dangerous for the fetus. If a pregnant woman becomes infected and is about to give birth, there is a risk that her child will die. The fetus becomes infected in 25 out of 100 cases, but symptoms do not always appear.
Congenital chickenpox in children has the following symptoms:
- brain damage
- optic nerve atrophy, eye underdevelopment
- underdevelopment of the limbs
- rash, zigzag scars
- pneumonia
Newborns with IUI are not treated with chickenpox because the symptoms do not progress. If the mother became infected 5 days before the day of birth or later, doctors may advise administering immunoglobulin to the newborn, because antibodies were not transferred to him from the mother.
Hepatitis B
The hepatitis B virus is transmitted mainly through unprotected sexual contact with a sick person. It reaches the fetus through the placenta (“baby place”). It is very dangerous for a pregnant woman to become infected from the 4th to the 9th month of gestation. Consequences of IUI:
- hepatitis B with subsequent recovery
- liver cancer
- carriage and chronic form of hepatitis type B
- acute form of hepatitis (liver failure develops, the child dies)
- psychomotor development delay
- lack of oxygen
- light weight
- miscarriage, stillbirth
HIV infection
The human immunodeficiency virus (HIV) attacks specific immune lymphocytes. Infection occurs mainly through sexual contact. The child becomes infected while arriving in the womb, or passing through the infected genital tract of the mother at birth. If you do not treat a child with a congenital form of HIV, he will not survive even two years, because the virus progresses quickly in a weak body. Death occurs from infections that cannot be fatal in healthy children.
To detect HIV in a newborn, PCR is mainly used. In the first 3-6 months after birth, there is no point in doing an antibody test. It is important to detect HIV in those who are expecting a child. They are given antiretroviral drugs for the entire period, that is, mainly zidovudine is given from the 4th week of gestation. They should not breastfeed their newborn. This greatly increases the baby’s chances of health.
Listeriosis
This disease is caused by the bacterium listeria. It can penetrate the embryo through the placenta, which many bacteria cannot. The routes of infection are described above. A pregnant woman may not have any symptoms of the disease. In some cases there are:
- heat
- diarrhea
- vomit
- flu-like symptoms
Consequences of fetal infection:
- multiple purulent foci, rash
- sepsis
- meningitis
- fever
- refusal to eat
- stillbirth, spontaneous abortion
If symptoms appear in the first 7 days after birth, then children die in 60 cases out of 100. Therefore, if a pregnant woman has an accurate diagnosis of listeriosis, she is prescribed ampicillin for 2 weeks. IUI is also treated if the child actually became infected from the mother.
Syphilis
Primary syphilis in pregnant women, which has not been treated, is transmitted in almost 100 cases out of 100. Out of 10 children, 6 die, while others develop a congenital form of the disease. In a sick pregnant woman, a primary ulcer first forms, and then the disease goes into a latent form, exacerbating from time to time.
Infection of the embryo occurs, even if the mother has a latent disease, from the 4th week of gestation. The consequences of IUI are:
- deafness mental retardation
- damage to the eyes, ears, hands, feet, teeth
- cracks in the skin
- rashes on the skin
- anemia, jaundice in a baby
- premature birth or stillbirth
Toxoplasmosis
It is transmitted to humans mainly from cats, but can also be transmitted from other animals. A pregnant woman can become infected when she cleans up after her pet or eats undercooked meat or dirty vegetables. By the time of pregnancy, most women have already had this disease, so it will not be passed on to the child.
During primary infection during pregnancy, in 50 out of 100 cases, the pathogen overcomes the placental barrier, infecting the embryo. Consequences of IUI for a baby:
- hydro-, microcephaly
- eye damage
- jaundice, enlarged liver and spleen
- encephalitis, meningitis, seizures
- stillbirth, miscarriage
- psychomotor development delay
Intrauterine infection is antenatal and/or intrapartum infection of the fetus without the development of an infectious process. Congenital infection is an infectious disease that is detected either prenatally or shortly after birth, but it occurs after antenatal and/or intrapartum infection of the fetus. Intrauterine infection (UI) is a disease in which both infection and the manifestation of clinical manifestations occur in utero. VIs are one of the leading causes of infant death in the early neonatal period and at the same time are considered as an important factor in disability from childhood. Risk factors (markers) of intrauterine infection of the fetus:
- burdened obstetric and gynecological history
- pathological course of the current (previous) pregnancy
- diseases of the genitourinary system
- any infectious diseases of organs and systems
- immunodeficiency states
- repeated blood transfusions (extensive blood transfusion history)
- condition after transplantation (lifelong immunosuppression with activation of endo- and exoinfections)
Infection in the first 2 weeks leads to the development of blastopathies. Outcomes: death of the embryo, formation of systemic organ pathology, which at birth resembles a congenital genetic pathology.
Infection within 2-12 weeks is accompanied by a teratogenic or embryotoxic effect (most often the agents are viruses leading to severe embryopathies or pregnancy ends in miscarriage). When collecting anamnesis, it is important to take into account the presence of miscarriages in the anamnesis.
Infection between 12 weeks and 6 months leads to the formation of early fetopathies (various mesenchymoses). The source of infection is the pregnant mother.
The main routes of transmission: transplacental, ascending, contact.
Etiology: viruses, bacteria, parasites, fungi, more often – mixed infection.
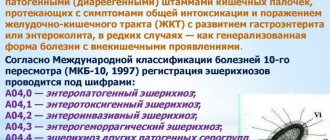
A special position in this group is occupied by infections TORCH complex. In 1971, WHO identified TORCH - a complex, a group of viral and bacterial infections that cause persistent structural changes:
T – Toxoplasmosis, toxoplasmosis; O - Others (other infections, of which are considered absolutely proven: chlamydia, syphilis, hepatitis A and B, gonococcal infection, listeriosis. Probable infections in this group include measles, mumps. Hypothetical infections - influenza A, lymphocytic choriomeningitis, human papillomavirus ); R – Rubella, rubella ; C – Citomegalia, cytomegalovirus infection; H – Herpes Symplex, herpetic infection.
Consequences of intrauterine infection (TORCH group infections)
- Toxoplasma – spontaneous miscarriage, intrauterine fetal death or the birth of a child with congenital toxoplasmosis.
- Rubella – congenital fetal defects (embryopathy, fetopathy), spontaneous abortion, stillbirth, etc.
- Cytomegalovirus infection - most newborns with congenital cytomegalovirus infection never develop symptoms of CMV, some have so-called temporary manifestations that disappear without a trace over time, and in a small number, signs of congenital CMV are pronounced and remain for life (hearing and/or vision loss , mental retardation, lack of coordination, death).
- Genital herpes is the development of early and late fetopathies, ophthalmia and pneumonia in newborns.
The main method of laboratory diagnosis is serological determination of specific immunoglobulins: IgM and IgG.
We recommend diagnosing intrauterine infection in 3 stages:
- Diagnosis in the prenatal period;
- Diagnosis at the time of birth;
- Diagnosis when clinical signs appear.
Diagnostic methods in the prenatal period:
- Direct methods are aimed at isolating the pathogen from chorionic aspirate during chorionic biopsy, amniotic fluid during amniocentesis, and fetal blood during umbilical cord puncture.
- Indirect methods are based on studying the mother’s condition: identifying the causative agent of infection in the mother.
Material for research:
- Saliva, discharge from the nose and pharynx, blood, urine, discharge from the cervix, uterine pharynx.
Determination of the mother's immunological status.
- At the first stage, i.e. a few days after infection, IgM antibodies are formed. Their level increases quite quickly, significantly ahead of the dynamics of class G immunoglobulins (IgG antibodies). The latter reach their maximum titer only 5-8 weeks after infection. By this time, the production of IgM antibodies decreases or stops completely. After recovery or stabilization of the process, only IgG antibodies continue to circulate in the blood in small quantities. With reinfection or exacerbation of the process, the titer of IgG antibodies increases again (several times). These patterns are important to take into account when acute TORCH infection is suspected in women with short terms of pregnancy. In such cases, a mandatory test for IgM antibodies is necessary, since at the beginning of the disease, i.e. during the most dangerous period for the fetus, IgG antibodies can be detected in a very low titer or not detected at all. Screening for TORCH infections is usually included in a comprehensive examination during pregnancy. We recommend testing the blood and cervical canal discharge.
Principles for interpreting the results of studies of TORCH infections The detection of IgG immunoglobulins indicates a low probability of intrauterine infection with pathogens of the TORCH group, and vice versa, their absence indicates a high risk of infection. If indicated, it is also important to establish the timing of infection. To determine the duration of infection, we recommend performing a special test for the avidity of IgG antibodies. Determining the avidity of antibodies to the pathogen makes it possible to isolate the primary infection and differentiate it from the period of reactivation or secondary penetration of the antigen into the body. Avidity refers to the strength of binding between an antibody and an antigen. During the development of the immune response, IgG antibodies gradually increase the strength of binding to the infectious agent, but at the beginning, the connection is quite weak. Such IgGs are called low-avidity. After a few weeks, the antibody is able to bind its target much more strongly. Such antibodies are called high-avidity. Thus, the appearance of low-avidity antibodies indicates a recent infection. The results of the determination are expressed as an avidity index expressed as a percentage:
- <50% – low avidity
- 51-69% - transitional
- >70% - high-avidity protective antibodies
If low-avidity antibodies are detected during pregnancy, confirmatory research methods are prescribed to make a decision. The most reliable is immunoblot - a highly specific and highly sensitive method, the advantages of which are:
- Sensitivity – 97%;
- Specificity – 99%;
- High resolution between negative and positive results;
- More accurate identification of the period of infection.
During the immune response, at different stages, the body produces antibodies to different proteins of the infectious agent, which are determined by immunoblotting. For example, during Toxoplasma infection, IgG antibodies to ROP1 first appear, then to the MAG1 protein, and later to the SAG1 protein. By determining antibodies to each of these proteins, you can obtain important information about the timing of activation of the humoral response with an accuracy of 2-3 weeks. Thus, we recommend conducting the examination in two stages: first, a risk group is identified (serological testing for the presence of IgG and IgM antibodies). Next, we recommend that patients whose blood serum contains IgM be tested for avidity and/or immunoblot testing.
Interpretation of antibody results
| IgG | IgM | Interpretation |
| Yes | No | If the test is taken in the very early stages of pregnancy, the body’s encounter with this pathogen has already taken place and this pathogen does not pose a serious danger to the unborn child. If the test is not taken at the earliest stages, the presence of IgG may be associated with a recent infection, already during pregnancy. In this case, confirmatory testing (IgG avidity) is recommended. |
| No | No | Exposure to this infection during pregnancy can pose a threat to the unborn child. The analysis should be repeated once a month. |
| Yes | Yes | The presence of IgG and IgM may be associated with a recent infection, already during pregnancy. But it also does not exclude infection before pregnancy. In this case, additional examination methods (avidity, immunoblot) are recommended. |
| No | Yes | The presence of IgM may be associated with a recent infection, as early as during pregnancy. But it also does not exclude reactivation of the infection, which is not dangerous during pregnancy. In this case, additional examination methods (immunoblot) are recommended. |
Postnatal diagnosis
Direct definition
- Isolation of the pathogen in aspirate, blood, meconium, urine, and cerebrospinal fluid of a newborn.
- The main principle of diagnostics is the identification of microbes in different materials.
Serodiagnosis
- Infections of the TORCH group, when transmitted intrauterinely, stimulate the early synthesis of class M immunoglobulins (IgM antibodies) in the fetus, which can be used for diagnosis already in the first days of life. When examining newborns, the presence of IgM antibodies in their blood is a clear sign of intrauterine infection, because Antibodies of this class do not penetrate the hematoplacental barrier.
Additional and confirmatory studies: IgG antibody avidity.
Viral hepatitis In the early stages of pregnancy, various fetopathies can occur, and in the second and third trimesters, stillbirths can occur. The frequency of premature births is significant, which is the cause of high perinatal mortality (10-15%). In addition, it should be taken into account that viral hepatitis is more severe in pregnant women than in non-pregnant women (the severity of viral hepatitis usually increases with increasing pregnancy).
Basic methods of laboratory diagnosis of viral hepatitis:
- Serological study of markers - specific antibodies and hepatitis antigens in blood serum.
- PCR – analysis of antigens of hepatitis pathogens.
Sexually transmitted infections
- Gonococcal infection - in 10-15% premature termination of pregnancy and low fetal weight and in 30-50% of ophthalmia of newborns.
- Syphilis - spontaneous abortion and intrauterine fetal death in 30%, late fetopathy (congenital syphilis) in 30-40%.
- Chlamydial infection - premature birth, rupture of membranes of the fetal bladder, postpartum endometritis, ophthalmia and pneumonia of newborns.
- Trichomonas infection - in 20-25% of cases, premature birth.
- Mycoplasma and ureaplasma infection - chorioamnionitis, premature birth, low fetal weight, postpartum endometritis, lung lesions (acute pneumonia, bronchopulmonary dysplasia), systemic lesions, sepsis, meningitis.
- Anogenital warts – laryngeal papillomatosis of newborns.
The main method of laboratory diagnosis of STIs is polymerase chain reaction.
TORCH infections
The following are called torch infections:
- cytomegalovirus
- rubella
- toxoplasmosis
- herpes
- tuberculosis
- syphilis, etc.
They are dangerous if they infect a pregnant woman. Some occur in a hidden or erased form, so they need to be identified by analysis. Therefore, at the stage of planning conception, the couple is tested for TORCH infections. If no antibodies to the rubella pathogen are detected in the expectant mother's body, she is vaccinated. Also, during pregnancy it is better not to come into contact with cats, so as not to become infected with toxcoplasmosis.
Diagnosis of intrauterine infection
Pregnant women undergo a blood test that can detect hepatitis B and C, as well as syphilis. Vaginal smears are regularly taken to check microflora. The PCR method is used, which makes it possible to detect viruses circulating in the blood, if any.
Ultrasound is safe for pregnant women. It does not indicate the presence of infection, but makes it possible to detect defects caused by infection and intrauterine growth retardation. Ultrasound is also a control method when performing cordocentesis. IUI is suspected if an ultrasound reveals the following signs:
- formed developmental defects
- high or low water
- swelling of the placenta, amniotic bands
- intrauterine growth restriction syndrome
- enlargement of the abdomen and expansion of the renal collecting system
- enlargement of the heart, liver and spleen
- multiple calcium deposits in the brain, liver, intestines
- enlargement of the ventricles of the brain
The seroimmunological diagnostic method is based on the determination of immunoglobulins. It is recommended for women from the risk groups listed above. Sometimes methods such as cordocentesis and amniocentesis are necessary. In the first method, blood is taken from the umbilical cord to detect any infection there. Amniocentesis means the examination of amniotic fluid.
If the doctor suspects IUI, a newborn is tested for biological fluids, such as saliva or blood.
Clinical manifestations of intrauterine infection?
If there is an intrauterine infection, the amniotic fluid that is discharged at the birth of a baby is cloudy in color and has an unpleasant odor. They may even be contaminated with meconium (the first discharge from the intestinal tract), which indicates a threatening state of infection of the fetus. Doctors definitely need to pay attention to this. After this, experienced pediatric doctors examine the placenta, its plethora, and whether there are any hemorrhages.
As for the child himself, first of all you need to look at the timing and weight. Pay attention to skin color. Is there a prolonged, prolonged yellowness of the skin or, conversely, pale skin, which may indicate anemia. There may be some skin rashes characteristic of pyoderma, streptoderma. The baby may have congenital pneumonia, congenital myocarditis, congenital meningitis and encephalitis. The liver and spleen are examined for enlargement of these organs. A blood test is also performed, where changes in the clinical picture can also be seen.
If we see the corresponding risk factors, for example, 2 or 3 signs from those listed above, then this child should already be in the “risk group” for intrauterine infections and should be carefully examined.