Compound
One milliliter of a 1% solution for external and intracavitary use includes 10 mg of hydroxymethylquinoxaline dioxide , as well as water for injection in a volume of up to 1 ml.
A milliliter of 0.5 percent solution for local, intravenous and intracavitary use contains 5 mg of hydroxymethylquinoxaline dioxide and water for injection as an excipient (in a volume of up to 1 ml).
A gram of Dioxidin ointment contains 50 mg, as well as excipient substances: polyethylene oxide 400, polyethylene oxide 1500, nipagin, propyl ester of paraoxybenzoic acid.
Dioxidin, 1%, solution for intracavitary administration and external use, 5 ml, 10 pcs.
Ointment
Locally. Apply a thin layer to the affected area once a day. Course - up to 3 weeks.
Solution for infusion and external use, 5 mg/mg
IV,
drip. In severe septic conditions, the drug solution is administered, previously diluted in a 5% dextrose solution or in a 0.9% sodium chloride solution to a concentration of 0.1–0.2%. The highest single dose is 300 mg, the daily dose is 600 mg.
Externally
— deep wounds are packed or irrigated with a solution daily or every other day, depending on the condition of the burn wound and the course of the wound process. The maximum daily dose is 2.5 g. Duration of treatment is up to 3 weeks.
Solution for intracavitary and external use 10 mg/ml
Externally, intracavity.
Dioxidin® is prescribed in a hospital setting.
Dioxidin® 1% solution cannot be used for intravenous administration due to the instability of the solution when stored at low temperatures.
Intracavitary administration.
Depending on its size, 10 to 50 ml of a 1% Dioxidin® solution is injected into the purulent cavity per day. Dioxidin® solution is injected into the cavity through a catheter, drainage tube or syringe. The maximum daily dose for administration into cavities is 70 ml of a 1% solution. The drug is administered into the cavity usually once a day. According to indications, it is possible to administer a daily dose in two doses. If well tolerated, the drug can be administered daily for 3 weeks or more. If necessary, repeat courses are given after 1–1.5 months.
External use.
Use 0.1–1% solutions of Dioxidin®. To obtain 0.1–0.2% solutions, ampoule solutions of the drug are diluted to the desired concentration with a sterile 0.9% sodium chloride solution or water for injection.
To treat superficial infected purulent wounds, apply napkins moistened with a 0.5–1% solution of Dioxidin®. After treatment, deep wounds are loosely tamponed with napkins moistened with a 1% solution of Dioxidin®, and if there is a drainage tube, 20 to 100 ml of a 0.5% solution of the drug is injected into the cavity.
For the treatment of deep purulent wounds with osteomyelitis (wounds of the hand, foot), use 0.5–1% solutions of the drug in the form of baths or carry out a special treatment of the wound with a solution of the drug for 15–20 minutes (injection of the solution into the wound for this period) followed by application dressings with 1% Dioxidin® solution.
Dioxidin® in the form of 0.1–0.5% solutions can be used to prevent and treat infections after surgery. According to indications (patients with osteomyelitis) and if well tolerated, treatment can be carried out daily for 1.5–2 months.
Release form
The drug has the following dosage forms:
- Dioxidin solution 1% for intracavitary and local use;
- Dioxidin solution 0.5% for local, intravenous and intracavitary use;
- Dioxidin ointment 5%.
A one percent solution is available in 10 ml colorless glass ampoules, 10 ampoules in one package; a 0.5% solution is supplied to pharmacies in colorless glass ampoules of 10 and 20 ml; The ointment is packaged in tubes of 25, 30, 50, 60 and 100 grams.
Pharmacodynamics and pharmacokinetics
The mechanism of action of Dioxidin is associated with the damaging effect of hydroxymethylquinoxaline dioxide on the cell walls of microorganisms , which ultimately suppresses their vital activity and leads to their death.
The drug is active against Proteus vulgaris , Friedlander's bacillus , aeruginosa , pathogens of bacterial dysentery from the genus Shigella (Shigella dysenteria, Shigella flexneri, Shigella boydii, Shigella sonnei), salmonella , which is the most common causative agent of acute diarrhea (Salmonella spp.), Escherichia coli (Escherichia coli), staphylococci (Staphylococcus spp.), streptococci (Streptococcus spp.), which are the causative agents of food toxic infections of pathogenic anaerobic bacteria Clostridium perfringens.
Dioxidin is able to act on bacterial strains resistant to other antimicrobial agents (including antibiotics ). In this case, the product does not cause local irritation.
The possibility of development of drug resistance of microflora to the drug cannot be excluded.
When administered into a vein, it has a small therapeutic breadth of action, which in turn presupposes strict adherence to the dosage regimen specified in the instructions.
Treatment of burned areas of the body with the drug, as well as purulent-necrotic wounds , allows you to accelerate the healing process of the wound surface, reparative (restorative) tissue regeneration, as well as their marginal epithelization, and has a beneficial effect on the course of the wound process.
Experimental studies have established that the drug is capable of having teratogenic , mutagenic and embryotoxic effects.
When used as a local remedy, it is partially absorbed from the wound or burned surface treated with it. It is eliminated from the body by the kidneys.
After injection into a vein, the therapeutic concentration of hydroxymethylquinoxaline dioxide in the blood remains for the next 4-6 hours. Plasma concentration after a single injection of the solution reaches a maximum after approximately 1-2 hours.
The active substance quickly and easily penetrates into all tissues and internal organs and is excreted by the kidneys. With repeated administrations it does not accumulate in the body.
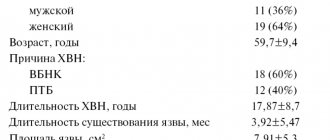
The problem of wound infection has become extremely relevant in recent years. The number of infectious complications from surgical wounds has sharply increased, resulting in severe sepsis caused by gram-negative microorganisms, as well as microorganisms resistant to almost all modern antimicrobial drugs.
Among all surgical patients, wound infection occurs in 35-45%. The number of postoperative purulent-septic infections in 1998 increased to 39% [14].
Simultaneously with the increase in bacterial infections, the frequency of candida and aspergillus fungi increases, most often due to the widespread, irrational use of antibacterial, corticosteroid, cytostatic drugs, as well as the lack of the concept of simultaneous prescribing of antifungal drugs with antibiotics for prophylactic purposes. The problem of intrahospital spread of both aerobic and anaerobic (clostridial and non-clostridial) infections remains relevant.
The reasons for the increase in the frequency and severity of purulent infections in surgery are varied and include the following factors:
— increasing the volume of surgical interventions, especially in high-risk patients;
- widespread use of instrumental examination and treatment methods accompanied by infection of the patient (intravascular and urinary catheters, endoscopic and tracheostomy tubes, endoscopic manipulations, etc.);
- traditional long-term regimens of prescribing certain groups of antibiotics for therapeutic and prophylactic purposes without regular monitoring of the dynamics of resistance of hospital strains to these drugs.
Depending on the pathogens that have invaded and the changes that occur in the wound, nonspecific (purulent, anaerobic, putrefactive) and specific (wound diphtheria, wound scarlet fever) wound infections are distinguished. In addition, a number of infectious diseases that do not have the nature of a wound infection enter the body through a wound, i.e. not accompanied by noticeable disturbances in the wound process. Some of these common infectious diseases are necessarily associated with the invasion of a pathogen into a wound (tetanus, rabies, rat bite disease); in others, the wound is only one of the possible routes of penetration of microbes (syphilis, anthrax). In practice, it is advisable to focus on the distribution of patients with wound infection into groups, taking into account the etiological and clinicopathological features:
- acute purulent diseases of the skin and soft tissues (abscessing boil, carbuncle, hidradenitis, mastitis, etc.);
— purulent post-traumatic wounds of soft tissues (with or without bone damage, with long-term soft tissue crush syndrome);
— postoperative purulent wounds of soft tissues;
— chronic purulent diseases of soft tissues (trophic ulcers of various origins, bedsores, etc.);
- hematogenous, postoperative or post-traumatic osteomyelitis;
- surgical sepsis.
Regardless of the origin of the wound process, the species composition of the wound microflora, the main methods of treatment are surgical and active complex effects on the purulent process, aimed at eliminating the tissue defect, suppressing the growth of microflora vegetating in the wound or preventing suppuration.
Along with timely surgical intervention on a purulent focus, the outcome of the disease is largely determined by adequate systemic and local antibacterial therapy, strictly focused on the data of bacteriological studies.
Only local drug treatment that is carried out strictly in accordance with the pathogenesis of the wound process can be considered reasonable, i.e. taking into account the phase of its flow [15].
Etiology of wound infections
In recent years, under the influence of various factors, primarily the powerful selective action of antibiotics, significant changes have occurred in the etiology of wound infections. Currently, the leading pathogens are:
— staphylococci (S. aureus, S. epidermidis);
- £, B, Y-hemolytic and non-hemolytic streptococci;
— representatives of the family Enterobacteriaceae (E. coli, Citrobacters
spp.,
Klebsiella
spp.,
Enterobacter
spp.,
Serratia
spp.,
Proteus
spp.,
Providencia
spp.);
- non-fermenting gram-negative bacteria (Pseudomonas
spp.,
Acinetobacter
spp.,
Moraxella
spp.,
Flavobacterium, Achromobacter).
The dependence of the species composition of wounds on their origin is clearly visible. So, for example, if in a group with acute purulent diseases staphylococcus in monoculture is detected in 69.5% of cases, then in patients with post-traumatic purulent wounds, chronic purulent diseases of the skin and soft tissues, as well as in patients with purulent wounds and developed sepsis, they are detected immediately several pathogenic microorganisms in 31.5, 48.8, 55.6% of cases, respectively. The rest are representatives of the family Enterobacteriaceae
in monoculture.
In recent years, fungi have begun to emerge from wounds much more often (9.9%), which is apparently due to insufficient attention to this problem and the lack of reliable prevention of fungal invasion (Table 1).
Obligate non-spore-forming anaerobic microorganisms, among which Bacteroides
spp.,
Fusobacterium, Peptococcus
spp.,
Peptostreptococcus
spp.,
F. nucleatum, P. melaninogenicus.
The proportion of pure non-clostridial and mixed aerobic-anaerobic microflora also depends on the location and origin of the purulent wound.
Currently, it is possible to significantly reduce the duration of systemic antibacterial therapy through the active introduction into practice of treating wounds under dressings with modern drugs focused not only on the phase of the wound process, but also on the species composition of wound microorganisms.
This tactic, with timely adequate surgical intervention and treatment with correctly selected drugs for local therapy, allows you to localize the purulent process and avoid generalization of the infectious process.
The use of modern drugs for local treatment of wounds at all stages of complex treatment makes it possible to reduce the time of systemic antimicrobial therapy, avoid the development of side effects, significantly reduce the cost of expensive antibacterial drugs, and avoid the formation of microflora resistance to the systemic antibiotics used.
Currently, several groups of drugs have been developed for local treatment of wounds in phases I and II of the wound process (Table 2).
The main groups of drugs are antiseptics, polyethylene glycol (PEG)-based ointments, modern biologically active dressings, enzyme preparations, and new antiseptics.
Antiseptics
When choosing antiseptics used for both preventive and therapeutic purposes, preference is given to drugs with a universal, broad spectrum of action, active against mixed microflora, and having a microbicidal or microbostatic effect.
Iodophors
In the practice of wound treatment, new complex compounds of iodine with polyvinylpyrrolidone (povidone-iodine, betadine, iodopirone, iodovidone, etc.), which have microbicidal and microbostatic effects, are widely used.
Drugs in this group suppress:
- gram-positive bacteria, including enterococci and mycobacteria;
- gram-negative bacteria, including pseudomonas, acinetobacter, Klebsiella, Proteus;
— bacterial spores, fungi, viruses, including hepatitis B and C viruses, entero- and adenoviruses, as well as anaerobic, spore-forming and asporogenic bacteria.
All pathogens of wound infections do not have either natural or acquired resistance to iodophors.
The activity of the complex with polyvinylpyrrolidone is not affected by the presence of blood, purulent discharge or necrotic tissue [4].
The most widely used in the practice of treating purulent-inflammatory processes are two dosage forms of complex compounds of iodine with polyvinylpyrrolidone - solution and ointment.
Ointments (1% iodopyrone ointment, povidone-iodine ointment) are used to treat purulent wounds with heavy exudation. Solutions (iodopirone, povidone-iodine) are used as antiseptics for prophylactic purposes for treating the surgical field, skin during punctures, closing surgical sutures, as well as for the treatment of wounds, trophic ulcers, bedsores, and diabetic foot syndrome in the absence of a large amount of wound separated.
Dioxidine
Dioxidin is one of two drugs derived from quinoxyline di-N-oxide, developed as a result of fundamental exploratory research in the period from 1960 to 1980 at the All-Union Scientific Research Chemical-Pharmaceutical Institute (currently the Center for the Chemistry of Medicines - TsKhLS VNIHFI , Moscow).
A number of drugs of this class of substances with high antimicrobial activity and a wide antimicrobial spectrum (quindoxine, mequidox, carbadox, temadox, olaquindox) have been developed abroad.
The drug is intended for the treatment of patients with wound infections caused by multidrug-resistant flora, Pseudomonas aeruginosa and non-clostridial anaerobic pathogens. This drug is most active against anaerobic bacteria (Clostridium
spp.,
Bacteroides
spp.,
P. melaninogenicus, Peptococcus
spp.,
Peptostreptococcus
spp., as well as aerobic gram-negative bacteria -
Ps.
aeruginosa, E. coli, Proteus spp.,
Klebsiella
spp.,
Serratia
spp.) [1-3].
It should be noted that strains of Pseudomonas aeruginosa, as well as gram-positive bacteria (staphylococci, streptococci), are more resistant to the drug. That is why, if the clinical situation allows, a 1% dioxidine solution without dilution is used for local treatment.
In the 70-90s, a solution of dioxidine in monotherapy and combination with other antibacterial drugs was considered as the drug of choice for the treatment of patients with sepsis, diffuse and local peritonitis, for the prevention and treatment of purulent-inflammatory processes in the liver and biliary tract, lungs, stomach, kidney allotransplantation, cardiac vascular prosthetics and coronary artery bypass grafting, under conditions of artificial circulation [11-13].
Currently, in Russian clinics for more than 25 years, various dosage forms of dioxidine have been used to treat various forms of purulent infection:
a) for local treatment
— 5% ointment, “Dioksikol” ointment containing 1% dioxidine, dioxidine aerosol (“Dioxisol”), polymer compositions with dioxidine (“Diovin”, “Diotevin”, Anilodiotevin”, “Colladiasob”, “Digispon A”, suture material ;
b) for introduction into cavities, for ultrasonic inhalations
— 1% aqueous solution in ampoules;
c) for intravenous administration
— 0.5% aqueous solution in ampoules.
Intravenous administration of dioxidine is carried out for health reasons. When justifying and determining the indications for the intravenous administration of dioxidine from the “benefit-risk” perspective, it should be taken into account that over the past 15-20 years, highly effective antibacterial agents have been created that have advantages over dioxidine in terms of toxicological properties. Therefore, dioxidin is prescribed intravenously only if other chemotherapeutic agents are ineffective or intolerable, strictly observing the recommended doses for the drug and the duration of each infusion.
Dioxidin is well compatible with other antimicrobial drugs. The clinical capabilities of dioxidin are expanded due to its ability to penetrate the blood-brain barrier, which makes it possible to use it in the treatment of patients with meningitis, brain abscesses and purulent cranial wounds.
Miramistin
The domestic antiseptic Miramistin belongs to quaternary ammonium compounds (cationic surfactants). Preclinical and clinical studies have shown that Miramistin has a pronounced antimicrobial effect against gram-positive and gram-negative, aerobic and anaerobic, spore-forming and asporogenic bacteria in the form of monocultures and microbial associations, including antibiotic-resistant hospital strains. The drug is most effective against hospital strains of staphylococcus and streptococcus. The drug has a detrimental effect on fungi, viruses, and protozoa.
Miramistin has been introduced into clinical practice since the early 90s of the last century. Currently, the drug is widely used in the complex treatment of purulent wounds and accompanying inflammatory complications in the bronchopulmonary system in the form of ultrasonic inhalations and the genitourinary system in the form of bladder instillations [5].
Lavasept
An antiseptic drug, the main active ingredient of which is polyhexanide, considered by experts as the drug of choice for the treatment of contaminated and infected wounds [16]. Polyhexanide belongs to the group of positively charged (cationic) polymers and contains surfactants, which reduce surface tension, which ensures easier removal of microbial biofilms.
Lavasept has a broad-spectrum bactericidal effect, is active against gram-positive and gram-negative bacteria (including Pseudomonas aeruginosa
), fungi, and MRSA.
Prontosan
A particular danger for the patient is a “dormant” infection, the aggressiveness of which is determined by the variability of the microflora, the reactivity of the body, the loss of activity of traditional systemic antibiotics and drugs for local medicinal treatment of wounds. This threat persists to a particular extent if the patient has foreign bodies, implanted devices, in patients with long-term non-healing wounds, trophic ulcers, diabetic foot syndrome, with post-traumatic and postoperative osteomyelitis, chronic post-traumatic and postoperative wounds.
It has been established that microorganisms and fungi, when they remain in a wound for a long time, thanks to the polymers they secrete, form a thin layer - a biofilm. Biofilm formed by bacteria and fungi provides reliable protection for pathogens from ultraviolet radiation, antibiotics, phagocytosis and other factors of the body’s immune system. Microbes in the biofilm can withstand concentrations of antibiotics 100-1000 times more than suppressive planktonic cells. Therapeutic effects on biofilms can be aimed at the mechanisms of initial adhesion of bacteria to the surface, blocking synthesis or destruction of the polymer matrix.
Currently, the attention of researchers on this problem is drawn to the possibility of using various medications that destroy the biofilm formed by bacteria and fungi. One of these drugs is prontosan, which contains polyhexanide, a polymerized biguanide derivative that acts as a local cationic antiseptic. The antimicrobial effect of polyhexanide is due to nonspecific affinity for the cell membranes of the microorganism, which contains a large amount of acidic phospholipids. Polyhexanide acts on bacterial cell membranes and increases their permeability.
Two dosage forms of Prontosan have been introduced into practice - 0.1%, 0.2% solution and gel, which contains 0.1% polyhexanide, 0.1% undecylenic amidopropyl betaine (surfactant), glycerol (humectant), hydroxyethylcellulose ( gelling agent), water.
PEG-based sorbents and ointments
It should be remembered that with abundant purulent exudation, the use of antiseptic solutions for local treatment of wounds in the form of gauze tampons is considered a flawed method, since tampons placed in the wound dry out quickly and do not have the long-term osmotic activity necessary to remove pus. In extreme cases, the wound can be filled with a combined tampon - a silicone tube is placed in the center of the gauze tampon, through which 10-20 ml of antiseptic is injected into the wound with a syringe 3-6 times a day.
For the treatment of superficial infected, purulent and purulent-necrotic wounds of various etiologies in the inflammatory phase, biologically active draining sorbents (anilovine, diovin, anilodiovin, diotevin, anilodyotevin, collasorb, colladiasorb), the main component of which is helevin, are successfully used. Dioxidin is used as an antimicrobial drug. The proteolytic effect of sorbents is due to the introduction of proteolytic enzymes into their composition (terrylitin, collagenase from hydrobionts). The analgesic effect is achieved due to the presence of a local anesthetic, anilocaine, in the composition [11].
Targeted use of biologically active dressings with a differentiated effect on the wound process, taking into account its phase and characteristics of the course, providing for sorption-application therapy in phase I of the wound process using biologically active sorbents or gel dressings with antimicrobial, analgesic and proteolytic effects, followed by wound treatment in phases II and III of the wound process with biologically active stimulating coatings with a specific effect on the processes of regeneration and epithelization.
In recent years, it has become possible to more successfully treat wounds using a new combination drug Baneocin, containing two highly active bactericidal components - bacitracin (a polypeptide antibiotic that inhibits the synthesis of bacterial cell walls) and neomycin (an aminoglycoside that inhibits protein synthesis), between which there is synergy. The results of numerous studies indicate the high activity of baneocin against gram-negative, gram-positive flora, aerobes and anaerobes. The components of the drug exhibit synergism against highly resistant hospital strains of Ps. aeruginosa, E. coli, S. aureus.
Baneocin is characterized by the ability to create high bactericidal concentrations in a purulent focus and not have a systemic effect. Numerous studies have shown that when treating wounds under bandages with Baneocin, complete eradication of pathogenic pathogens and reliable prevention of reinfection of the wound surface by hospital microorganisms is achieved in a short time without the traditional systemic antimicrobial therapy in such cases, prescribed for both therapeutic and prophylactic purposes.
The drug Baneocin is available in two dosage forms, focused on the phases of the wound process. For example, for the treatment of purulent wounds in the first phase of the wound process, Baneocin powder is used, which actively absorbs wound discharge within 5 hours.
For the treatment of wounds in the II phase of the wound process, Baneocin ointment is used, which exhibits a local bactericidal effect necessary to prevent reinfection of granulating wounds with hospital strains. The resulting thin film of the drug protects the thin layer of young epithelium from damaging factors.
The positive properties of two dosage forms of Baneocin - powder and ointment - are successfully implemented both at the outpatient and inpatient stages of complex treatment of patients of different groups:
- with focal skin infections (hidradenitis suppurativa, paronychia, boil, carbuncle);
- with burns, frostbite;
- with trophic ulcers;
- for the prevention of suppuration of household, sports and industrial wounds, abrasions (violations of the integrity of the skin);
— to prevent the development of an infectious process in the area of donor wounds when collecting skin grafts in traumatology, surgery, and cosmetology.
Painless and non-traumatic application, deep penetration into tissue, and good tolerability of Baneocin make it possible to successfully treat patients with trophic ulcers even in cases of aggravated allergic history (intolerance to traditional local drugs) or the identification of highly resistant strains of Ps. aeruginosa
[6].
For the treatment of extensive and deep wounds with a purulent process in the first phase
over the past 25-30 years, PEG-based ointments have been successfully used (levosin, levomekol, 5% dioxidine ointment, dioxykol, 1% iodopyrone ointment, 1% povidone-iodine ointment, 0.5% miramistin ointment, iodometricylene, nitacid, streptonitol , 10% mafenide acetate ointment, streptolaven, stallanin-PEG 3%, oflomelide, etc.). The listed drugs have different osmotic activity for the differentiated treatment of wounds in the first phase of the wound process with copious or moderate amounts of wound discharge (boils, carbuncles, hidradenitis, mastitis, abscesses, phlegmons, suppurating lipomas, atheromas, purulent postoperative and post-traumatic purulent wounds, venous trophic ulcers , “diabetic foot” with a local purulent-necrotic process, etc.
These drugs have a fairly wide spectrum of activity against both aerobic and non-spore-forming anaerobic microorganisms.
Despite many years of intensive use of ointments containing chloramphenicol or dioxidin, their high antimicrobial activity remains against the main causative agents of surgical infection.
If there are gram-negative bacteria in the wound, in particular Pseudomonas aeruginosa, it is recommended to use 10% mafenide acetate ointment, 5% dioxidine ointment, dioxicol ointment, nitacid ointment.
For the treatment of non-sporogenous anaerobic infection in combination with aerobic infection, it is advisable to use the following drugs:
- with nitazol (Streptonitol and Nitacid ointments);
— foaming aerosol Nitazol;
- 5% dioxidine ointment, dioxikol ointment.
When using PEG-based ointments, side effects (clinically significant) are observed in 0.7% of cases, clinically insignificant - in 2.3% of cases. Most often they manifest themselves in the form of local symptoms of drug-induced dermatitis. In cases of intolerance to chloramphenicol, dioxidin, treatment can be carried out with oflomelid ointment or 5% miramistin ointment, which has not only a wide spectrum of antimicrobial activity, but also antiviral and antifungal effects, which is extremely important in the treatment of patients with trophic and long-term non-healing wounds.
Of the new ointments, the domestic drug streptolaven deserves special attention, which includes an enzyme of microbial origin (streptolysin), an antimicrobial drug miramistin and a base balanced in osmotic action that does not cause drying of wound tissue. This is the only ointment in the country with a necrolytic effect and is currently successfully used in the treatment of patients with diabetic foot syndrome, extensive burns, trophic ulcers, and bedsores [9].
The possibilities for successful treatment of patients with purulent wounds, trophic ulcers, bedsores, infected burns have significantly expanded with the advent of the new ointment Stellanin-PEG 3%, containing 1,3-diethylbenzimidazolium triiodide, low molecular weight polyvinylpyrrolidonium, dimexide, polyethylene oxide 400 and 1500. The bactericidal effect of the drug is due to the incoming it contains active iodine [9].
As can be seen from table. 3,
Stellanin-PEG ointment 3% is not inferior in antimicrobial activity to well-known drugs (levomekol, 5% dioxidine ointment).
Stellanin-PEG has high antimicrobial activity against both gram-positive and gram-negative microorganisms, including methicillin-resistant staphylococci (MRSA), E. faecalis, E. faecium,
as well as
E. coli
and
Klebsiella
spp., producing extended-spectrum beta-lactamases, and is also able to suppress the vital activity of fungi
(C. albicans).
In the treatment of wounds and trophic ulcers with severe pain, a high clinical effect is achieved using the new PEG-based ointment oflomelid, which contains lidocaine as an analgesic component and ofloxacin as an antimicrobial component.
Particular severity of the wound process occurs when the patient develops a polyvalent allergy. The solution in such clinical situations is the use of drugs containing silver (Argosulfan ointment - for light wound discharge) or Actisorb Plus dressings (non-woven nylon fiber with activated carbon and silver ions).
For the treatment of wounds with a moderate amount of wound discharge and a slow regeneration process (long-term non-healing wounds, trophic ulcers, diabetic foot syndrome, bedsores, etc.), the use of the original domestic drug 15% Dimephosphone, which has membrane-stabilizing, anti-acidotic, antimicrobial, anti-inflammatory activity, is indicated [10 ].
Treatment of wounds in phase II of the wound process
For the treatment of moderately or slightly exuding purulent wounds in the stage of transition to phase II of the wound process, as well as in the treatment of donor wounds during free skin grafting with autodermograft, the use of biologically active gel dressings Apollo PAK and Apollo PAA, which include iodovidone or miramistin, is indicated. also local anesthetic anilocaine. The hydrogel is based on a copolymer of acrylamide and acrylic acid.
If signs of a regenerative process are detected in the absence of profuse suppuration and mild symptoms of inflammation remain, it is possible to treat wounds under bandages using iodine-containing solutions: 10% Iodopirone, 1% Iodovidone, 1% povidone-iodine, Sulyodopirone.
After the acute purulent process has stopped and symptoms of intoxication have disappeared, confirmed by both clinical and laboratory tests, it is possible to cancel general antibacterial therapy. In these cases, local treatment of wounds at the stage of preparation for final closure with sutures or plastic surgery is carried out under bandages with drugs:
- biologically active stimulating wound coverings with antimicrobial and local anesthetic effects (Digispon-A, Algikol-FA, Kollakhit-FA, Anishispon);
— collagen-containing wound coverings (Gentatsikol);
— wound coverings based on alginates (Algipor, Algimaf);
— wound covering with silver based on collagen and regenerated cellulose (Promogran-Prisma);
— foaming aerosols (dioxysol, gentazol, nitazol);
- ointments with slight osmotic activity (Methyldioxylin, Argosulfan, Fuzimet, Streptonitol, Biopin 5%, 10%; Baneocin);
- oils (Miliacyl, sea buckthorn oil, rosehip oil).
The appearance in hospitals of a new Fuzimet ointment (a combination of fusidine sodium with methyluracil) makes it possible to successfully treat patients with methicillin-resistant S. aureus
(MRSA), without including vancomycin or linezolid in complex therapy [7, 8].
Prevention and treatment of fungal infections during systemic and local antimicrobial therapy of wound infections
Excessive enthusiasm for various antibacterial drugs in the treatment of infectious processes without mandatory simultaneously prescribed antifungal therapy has led to the fact that the problem of deep mycoses in recent years has become extremely urgent and difficult to solve. For example, the mortality rate for candidal pneumonia is 65-70%.
Disseminated candidiasis accounts for up to 10-15% of all nosocomial blood infections. With disseminated candidiasis, fungal infection of the skin is possible with the formation of subcutaneous abscesses, cellulite or individual muscle groups (candidal myositis). Fungal infections of the kidneys and lungs, nervous system, heart, spine, costal and sternoclavicular cartilages, stomach, intestines and bile ducts are extremely difficult to treat.
Candidaemia can be the direct cause of death in 75% of cases, and candidal sepsis as a cause of death can reach 88%.
Diabetes mellitus, antibiotic treatment, the presence of indwelling catheters, and severe neutropenia predispose to colonization of a fungal infection. Disseminated candidiasis is possible as a result of infection during surgical operations, invasive diagnostic procedures (puncture, biopsy, endoscopy), hemodialysis and peritoneal dialysis. Up to 40.2% of medical personnel may be carriers of Candida
spp., with 31.3% of them in association with
S. aureus,
43.7% with coagulase-negative staphylococci, and 25% in monoculture.
Prevalence of oropharyngeal carriage of fungi of the genus Candida
spp. among the medical staff of the general surgery department is 61.5%.
According to a study carried out at the Institute of Surgery named after. A.V. Vishnevsky, frequency of Candida albicans
from various biological media and catheters was detected in 8.6-12% of cases. The most dangerous source of the spread of fungi was a solution of furatsilin, from which fungi were detected in 58.8% of cases.
Traditionally, to prevent fungal infection, along with antibacterial drugs in such cases, ketoconazole or (in case of generalized infection) fluconazole, flucytosine or amphotericin B are prescribed. In case of generalized fungal infection, the duration of etiotropic therapy usually ranges from several weeks to a year.
Timely abandonment of long-term systemic antibacterial therapy, abandonment of traditional antiseptics (furatsilin solution), traditional absolutely ineffective fat-based ointments and active use of drugs such as 1% povidone-iodine solution, solutions of Prontosan, Lavasept (0.1%, 0. 2%) or 0.5% Miramistin ointment allows not only to avoid serious complications of the wound process, but also to successfully combat fungal invasion without resorting to systemic antifungal therapy.
Thus, the pharmaceutical industry currently has the opportunity to produce a fairly complete range of modern, highly effective drugs for successful local medicinal treatment of wounds, trophic ulcers, bedsores of various locations and origins. Timely active introduction of these drugs into the daily practice of practical healthcare can significantly reduce the cost of purchasing systemic expensive foreign drugs (there are no domestic drugs).
However, I would like to draw the attention of leading pharmaceutical manufacturers to the unacceptable cessation of production of such drugs as 5% dioxidine ointment, dioxicol, nitacid, streptonitol, 1% iodopyrone ointment, 0.5% quinifuril ointment, foaming aerosols (dioxysol, gentazol, nitazol, domestic hydrocolloids galagran and galactone, collagen coating with gentamicin gentacycol, wound dressings containing sodium alginate (algipor, algimaf).
The current situation requires an active position of all specialists involved in the treatment of surgical infections. It is extremely important to review the standards of wound treatment using modern drugs, since from the standpoint of evidence-based medicine, such standards can reduce mortality in patients with sepsis to an average of 26.5%, which is of extreme social significance.
Timely equipping of emergency medical teams, teams providing assistance to victims of natural and man-made disasters, military conflicts, outpatient clinic doctors, trauma centers and hospitals, specialized purulent surgery departments with modern drugs for local treatment of wounds will undoubtedly help reduce the development of severe purulent wounds. complications and diseases, will reduce the cost of antibacterial drugs by 2-3 times.
Indications for use
Indications for IV administration of Dioxidin are:
- septic conditions (including conditions developing against the background of burn disease);
- purulent meningitis (purulent-inflammatory damage to the membranes of the brain);
- purulent-inflammatory processes accompanied by symptoms of generalization .
purulent-inflammatory processes occurring in the chest or abdominal cavity , including:
- purulent pleurisy (pleural empyema);
- peritonitis (an inflammatory process affecting the parietal and visceral layers of the peritoneum);
- cystitis (inflammation of the bladder);
- empyema of the gallbladder (acute purulent inflammation of the gallbladder).
Intracavitary injections can also be prescribed for prophylactic purposes to prevent the development of infectious complications after catheterization of the bladder .
Dioxidin is used as an external and local remedy:
- for the treatment of burns , trophic ulcers and wounds (including deep and superficial, of various locations, infected and purulent, difficult and long-term healing);
- for the treatment of wounds that are characterized by the presence of deep purulent cavities (for example, purulent pleurisy , soft tissue abscesses , cellulitis and pelvic abscesses , postoperative wounds on the organs of the urinary and biliary system, purulent mastitis , etc.);
- for the treatment of infectious skin lesions (pyoderma) caused by the activity of streptococci or staphylococci.
What does Dioxidin help with?
A solution for intravenous administration is prescribed for:
- sepsis;
- purulent-inflammatory processes in the brain.
The medicine for intracavitary use is effective for:
- inflammation of the bladder;
- purulent pleurisy;
- purulent processes in the gallbladder.
The product for local and external application can be used for the following problems:
- burns, wounds, ulcers;
- deep purulent cavities.
Contraindications
The use of Dioxidin is contraindicated:
- in case of hypersensitivity to the components of the drug;
- with adrenal insufficiency (including if it is noted in the anamnesis);
- during pregnancy ;
- during lactation ;
- in pediatric practice .
The drug is prescribed with caution to patients with chronic renal failure .
Side effects
Intracavitary administration and administration of Dioxidin into a vein may be accompanied by:
- headache;
- chills;
- dyspeptic disorders , which are expressed in the form of nausea, diarrhea and vomiting ;
- increased body temperature;
- unexpected convulsive muscle twitching ;
- photosensitizing effect (the appearance of pigmented spots on the body when the skin is exposed to ultraviolet rays);
- allergic reactions.
, periwound dermatitis and itching may occur in the area of the body treated with the drug.
Instructions for use of Dioxidin (Method and dosage)
Instructions for use of Dioxidin in ampoules
Dioxidin is administered intravenously by drip. In severe purulent-septic conditions, the solution before administration is pre-diluted with an isotonic solution (5% dextrose solution or 9% NaCl solution) to obtain a concentration of 0.1-0.1%.
The maximum permissible single dose is 0.3 grams, daily dose is 0.6 grams.
In cases where the patient is indicated for external use of Dioxidin, the drug is used for packing deep wounds, as well as irrigating affected areas of the body.
After preliminary cleaning and treatment, deep wounds are recommended to be loosely tamponed with tampons soaked in a 1% solution.
If the patient has a drainage tube, he is advised to administer 20 to 100 ml of a 0.5% solution into the cavity.
Therapy of deep purulent wounds on the hands or feet with osteomyelitis involves the use of Dioxidin solutions (0.5 or 1%, as indicated by the attending physician) in the form of baths.
Special treatment of the wound surface for 15-20 minutes is also allowed: the drug is injected into the wound for the specified time, after which a bandage with a 1% solution of the drug is applied to the affected area of the body.
Treatment of superficial infected purulent wounds involves applying wipes soaked in a 0.5 or 1% solution to the wound surface.
It is recommended to repeat the procedure daily or every other day (the frequency of applications depends on the condition of the wound and the characteristics of the wound process). The highest daily dose is 2.5 grams. Treatment with Dioxidin is usually continued for up to 3 weeks.
For patients with osteomyelitis , as well as if the drug is well tolerated, in some cases treatment can be continued for 1.5-2 months.
If intracavitary administration of the drug is necessary, the patient should inject 10 to 50 ml of a 1% solution into the cavity daily through a catheter or drainage tube. The drug is administered using a syringe, usually once. In some cases, Dioxidin may be administered in 2 doses according to indications.
The course of treatment lasts from 3 weeks. If appropriate, it is repeated after 1-1.5 months.
The highest daily dose for intracavitary administration is 70 ml.
Instructions for use of Dioxidin in the ear
To treat otitis media, it is usually customary to use antibiotics and vasoconstrictor drugs . However, in cases where they are not effective, Dioxidin becomes the drug of choice, a feature of which is its effectiveness against anaerobic bacteria .
Before instilling the medicine, it is recommended to clean the ear canal from wax using a cotton swab soaked in a 3% hydrogen peroxide or special cotton swabs (for convenience, the auricle is slightly pulled back). If the ear is very dirty, leave the tampon with peroxide in it for about 5 minutes.
In case of purulent otitis media , which is often accompanied by perforation of the eardrum and discharge of pus, all purulent contents are first removed from the ear canal before instillation.
For otitis, Dioxidin should be injected simultaneously into the nose and into the ear canal. The solution effectively sanitizes the nasal cavity and stops the inflammatory process in it, and since the nose is connected to the ear by the Eustachian tube, relieving the inflammatory process in the nose has a beneficial effect on the situation as a whole.
The dose and frequency of instillations are selected individually in each specific case and exclusively by the attending physician.
According to the instructions for use, Dioxidin drops are prohibited from being prescribed to patients under 18 years of age. However, in some situations, when it is not possible to achieve an effect using other means, pediatricians prescribe the medicine even to small children.
Instructions for use of Dioxidin in the nose
Prescription of Dioxidna in ampoules into the nose is used when it is necessary to treat certain forms of rhinitis , as well as for sinusitis .
For the treatment of adult patients, the drug should be pre-diluted with NaCl solution, hydrocortisone or water for injection before instillation. Dosage in the nose for an adult - from 2 drops to ⅓ pipette. Dioxdin drops are dripped into the nose 3 to 5 times a day. More precisely, the dose and the required frequency of procedures are determined by the attending physician.
The maximum duration of treatment should not exceed 7 days. If after this period the patient does not show improvement, he requires careful examination and, based on his results, appropriate treatment.
There are no official instructions for the use of Dioxidin in the nose for children. However, if appropriate, doctors also use the drug to treat children. Before instilling Dioxidin into the nose, the solution should be diluted to a concentration of 0.1-0.2%. As in the situation with adults, the doctor selects the treatment regimen individually.
As a rule, Dioxidin is administered to a child's nose 1-2 drops 2 or 3 times a day for 3-5 (maximum 7) days.
Inhalations with Dioxidin for adults
Inhalation therapy is one of the main types of treatment for diseases of the respiratory tract .
To prepare a solution for inhalation, the medicine is diluted with physiological solution in a ratio of 1:4 for a drug with a concentration of 1% and in a ratio of 1:2 for a drug with a concentration of 0.5%.
For one procedure, 3 to 4 ml of the resulting solution is used. The frequency of procedures is 2 times a day.
Dioxidin ointment: instructions for use
The ointment is applied topically. It is recommended to apply a thin layer to the affected area of the body once a day. The course of treatment is up to three weeks.
Dioxidin, 5 mg/ml, solution for infusion and external use, 5 ml, 10 pcs.
Ointment
Locally. Apply a thin layer to the affected area once a day. Course - up to 3 weeks.
Solution for infusion and external use, 5 mg/mg
IV,
drip. In severe septic conditions, the drug solution is administered, previously diluted in a 5% dextrose solution or in a 0.9% sodium chloride solution to a concentration of 0.1–0.2%. The highest single dose is 300 mg, the daily dose is 600 mg.
Externally
— deep wounds are packed or irrigated with a solution daily or every other day, depending on the condition of the burn wound and the course of the wound process. The maximum daily dose is 2.5 g. Duration of treatment is up to 3 weeks.
Solution for intracavitary and external use 10 mg/ml
Externally, intracavity.
Dioxidin® is prescribed in a hospital setting.
Dioxidin® 1% solution cannot be used for intravenous administration due to the instability of the solution when stored at low temperatures.
Intracavitary administration.
Depending on its size, 10 to 50 ml of a 1% Dioxidin® solution is injected into the purulent cavity per day. Dioxidin® solution is injected into the cavity through a catheter, drainage tube or syringe. The maximum daily dose for administration into cavities is 70 ml of a 1% solution. The drug is administered into the cavity usually once a day. According to indications, it is possible to administer a daily dose in two doses. If well tolerated, the drug can be administered daily for 3 weeks or more. If necessary, repeat courses are given after 1–1.5 months.
External use.
Use 0.1–1% solutions of Dioxidin®. To obtain 0.1–0.2% solutions, ampoule solutions of the drug are diluted to the desired concentration with a sterile 0.9% sodium chloride solution or water for injection.
To treat superficial infected purulent wounds, apply napkins moistened with a 0.5–1% solution of Dioxidin®. After treatment, deep wounds are loosely tamponed with napkins moistened with a 1% solution of Dioxidin®, and if there is a drainage tube, 20 to 100 ml of a 0.5% solution of the drug is injected into the cavity.
For the treatment of deep purulent wounds with osteomyelitis (wounds of the hand, foot), use 0.5–1% solutions of the drug in the form of baths or carry out a special treatment of the wound with a solution of the drug for 15–20 minutes (injection of the solution into the wound for this period) followed by application dressings with 1% Dioxidin® solution.
Dioxidin® in the form of 0.1–0.5% solutions can be used to prevent and treat infections after surgery. According to indications (patients with osteomyelitis) and if well tolerated, treatment can be carried out daily for 1.5–2 months.
special instructions
Prescription of Dioxidin is resorted to only in cases where the use of other antimicrobial drugs (including carbapenems , fluoroquinolones , cephalosporins of the II-IV generations ) did not produce the expected effect.
For patients with chronic renal failure, the dosage regimen should be revised towards a lower dose.
When administered intravenously, Dioxidin has a narrow therapeutic range, which requires constant monitoring of compliance with the recommended dosage regimen.
To prevent the development of side effects, treatment with Dioxidin is supplemented with the prescription of antihistamines and calcium supplements . If adverse reactions do occur, the dose is reduced and the patient is prescribed antihistamines .
In some cases, the occurrence of adverse reactions is a reason to discontinue the drug.
If pigment spots appear on the skin, the dose should be reduced, while increasing the duration of its administration (a single dose is administered over one and a half to two hours) and supplementing the therapy with antihistamines.
If crystals appear in ampoules with the drug during storage (usually if the temperature drops below 15°C), it is recommended to dissolve them by heating the ampoules in a water bath (the water should boil) and shaking them periodically until the crystals are completely dissolved.
The solution should be completely transparent. If, after cooling it to 36-38°C, crystals do not form, Dioxidin is considered suitable for use.
During the period of treatment with the drug, care should be taken when driving vehicles, engaging in activities that are potentially hazardous to health and life, as well as performing work that requires a high speed of psychomotor reactions.
Dioxidin injection solution 0.5% 10 ml ampoule 10 pcs
Intravenous administration Intravenous drip (at a rate of 60-80 drops per minute) under the supervision of a physician. A solution of 5 mg/ml is administered, which is pre-diluted in a 5% solution of dextrose (glucose) or in a 0.9% solution of sodium chloride to a concentration of 1-2 mg/ml (0.1 - 0.2%). The daily dose of the drug is administered once or in 3-4 doses during the day (fractional administration). The drug is administered at a rate of 60-80 drops/min for 30 minutes. In severe septic conditions, the maximum single dose is 300 mg (60 ml of a 5 mg/ml solution), the daily dose is 600 mg of hydroxymethylquinoxaline dioxide (that is, 120 ml of a 5 mg/ml solution). For purulent meningitis, the daily dose is 600 mg of hydroxymethylquinoxaline dioxide (that is, 120 ml of a 5 mg/ml solution). For chronic purulent processes in the lungs in the acute stage with signs of generalization, the daily dose is 500-600 mg of hydroxymethylquinoxaline dioxide (that is, 100-120 ml of a 5 mg/ml solution). When treating severe purulent urinary tract infection, the daily dose is 200-400 mg of hydroxymethylquinoxaline dioxide (that is, 40-80 ml of a 5 mg/ml solution). For patients with impaired renal function, the dose of the drug is reduced by 2 times. In elderly patients, a dose reduction may be required if renal function is impaired. In case of precipitation of hydroxymethylquinoxaline dioxide crystals, the crystals are dissolved in ampoules with a solution, heating the ampoules in a boiling water bath while shaking until the crystals are completely dissolved (the solution should become transparent). If, when the ampoules with the drug are cooled to 36-38°C, the crystals do not fall out again, the drug is suitable for use. Local and external use Apply 1-5 mg/ml solutions of hydroxymethylquinoxaline dioxide. To obtain a solution of the required concentration, the drug is diluted with a sterile 0.9% sodium chloride solution or water for injection. To treat superficial purulent wounds, wipes moistened with a solution of the drug are applied to the wound surface, previously cleaned of purulent-necrotic masses. The dressings are changed daily or every other day, depending on the condition of the wound or the course of the wound process. After treatment, deep wounds are loosely tamponed with tampons moistened with a solution of the drug. Dressings are done once a day. The maximum daily dose of hydroxymethylquinoxaline dioxide is 2.5 g (500 ml of 5 mg/ml solution). Duration of treatment is up to 3 weeks. To treat deep purulent wounds with osteomyelitis (wounds of the hand, foot), a solution of the drug is used in the form of baths or a special treatment of the wound with the drug is carried out for 15-20 minutes (injection of the solution into the wound at this time) followed by application of bandages moistened with the solution. For long-term washing of wounds, a solution of hydroxymethylquinoxaline dioxide 1 mg/ml is used (wound drainage with a thin catheter, rinsing with rare drops for 3-4 hours 1-2 times a day, but not more than 400-500 ml of solution per rinse). To prevent infections after surgical interventions, 1-2 mg/ml solutions of the drug are used. According to indications (patients with osteomyelitis) and if well tolerated, treatment can be carried out daily for 1.5-2 months. In case of precipitation of hydroxymethylquinoxaline dioxide crystals, the crystals are dissolved in ampoules with a solution, heating the ampoules in a boiling water bath while shaking until the crystals are completely dissolved (the solution should become transparent). If, when the ampoules with the drug are cooled to 36-38 ° C, the crystals do not fall out again, the drug is suitable for use.
Analogs
Level 4 ATX code matches:
Monural
Nitroxoline
Zyvox
Hexamethylenetetramine
Calcex
Kirin
5-NOK
Bacteriophage Klebsiella Pneumonia
Bacteriophage Proteus
Bacteriophage Coli
Bacteriophage Pseudomonas aeruginosa
Bacteriophage Salmonella
Bacteriophage Coliproteus
Bacteriophage Streptococcal
Bacteriophage Klebsiella Polyvalent Purified
Bacteriophage Staphylococcal
Linezolid
Fosfomycin
Analogues of Dioxidin are the drugs 5-NOK , Galenophyllipt , Hexamethylenetetramine , Zyvox , Kirin , Kubitsin , Monural , Nitroxoline , Ristomycin sulfate , Sangviritrin , Urophosphabol , Fosfomycin , Linezolid-Teva , Zenix , Amizolid , Dioxicol , Quinoxidin .
Dioxidin for children
The drug is not intended for the treatment of children and adolescents under 18 years of age. This contraindication is mainly due to the possible toxic effect of hydroxymethylquinoxaline dioxide .
However, in certain situations, when the expected benefit to the child outweighs the potential risks, the doctor may neglect this limitation. If Dioxidin is prescribed, treatment should be carried out in a hospital setting or under the constant supervision of the attending physician.
In pediatrics, Dioxidin solution is most often used to treat ENT diseases , mainly purulent forms of rhinitis or sinusitis . It is considered most appropriate to use a medicine with a concentration of the active substance of 0.5%.
In addition, the solution and ointment can be used to treat wound surfaces. A solution with a concentration of 0.5% is prescribed if the patient has deep lesions.
However, Dioxidin with such a dosage of the active substance should not be used for a long time. Therefore, as the condition of the wound improves, they switch to a 0.1% solution or ointment.
Dioxidin for a runny nose
The drug is not available in the form of nasal drops, therefore, before dripping Dioxidin into the child’s nose, the contents of the ampoule are diluted with a hypertonic solution to obtain a solution with a concentration of hydroxymethylquinoxaline dioxide of 0.1-0.2%.
It is recommended to administer nasal drops for children three times a day, one or two in each nostril, best after instilling vasoconstrictor drugs that reduce tissue swelling and facilitate nasal breathing. When carrying out the instillation procedure, the patient should tilt his head back so that the medicine penetrates as deeply as possible into the nasal passages.
It should be remembered that after opening the ampoule with the medicine, the solution is considered suitable for use within 24 hours. The maximum permissible duration of treatment for a runny nose is 1 week. However, most pediatricians recommend limiting it to 3-4 days.
In parallel with treatment with Dioxidin, it is recommended to use traditional methods of treating a runny nose (warm the nasal passages and rinse them with weak saline solutions) and monitor the air humidity in the room.
Dioxidine in the ear
Dioxidin instillation into the ear is indicated for severe forms of acute inflammation of the middle ear , in cases where antibiotics do not give the desired effect.
Before using the solution, it is recommended to thoroughly clean the ear from wax with a cotton swab.
The solution in ampoules is instilled into the ear twice a day. Moreover, for otitis media, the procedures are also supplemented with nasal drops.
The drug is not ototoxic and does not affect the auditory nerve.
Dioxidin for sinusitis
Dioxidine in ampoules is often used in the treatment of infectious processes localized in the paranasal sinuses. For sinusitis, the solution is used in the form of inhalations or as nasal drops. Drops are administered two or three into each nasal passage. The procedures are repeated 2 times a day.
To treat sinusitis, complex drops can also be used, which are prepared using solutions of dioxidine, adrenaline and hydrocortisone . Complex drops are administered one into each nasal passage 4-5 times during the day.
Compound drops are prepared according to a prescription prescribed by a doctor in a pharmacy or at home.
Dioxidin for inhalation
Reviews indicate that prescribing inhalations to children using Dioxidin solution can effectively treat persistent cough . In addition, the use of the medicine helps disinfect the nasal passages and paranasal sinuses, provokes the death of pathogens in the bronchi and pharynx , and also eliminates nasal congestion and prevents the separation of purulent secretions.
It is recommended to do inhalations with Dioxidin for children using a nebulizer. As a rule, this method is used for persistent bronchitis , which cannot be treated with other antibacterial drugs .
For inhalation, a 0.5% solution is prescribed. Before the procedure, it should be diluted with a hypertonic solution in a ratio of 1:2. The duration of inhalation is from 3 to 4 minutes. The frequency of procedures is 2 times a day.
Dioxidin for gargling
The advisability of using a solution for gargling is due to the ability of hydroxymethylquinoxaline dioxide to eliminate infection , clean the infected surface and accelerate the regeneration of the mucous membrane .
These features of the drug contribute to the healing process in case of purulent bacterial infections provoked by microflora sensitive to Dioxidin in case of ineffectiveness of other prescribed antibacterial agents or if they are poorly tolerated by the patient.
Rinsing with the solution is prescribed for pharyngitis , sore throat , tonsillitis , and only in severe cases when other drugs do not help.
To prepare a solution for rinsing, the contents of one ampoule of a one percent solution of Dioxidin are diluted in a glass of warm drinking water, water for injection or isotonic NaCl solution.
A small amount of liquid is taken into the mouth and, throwing the head back, gargle for a few seconds. After this, the solution is spat out, and rinsing is continued until the solution is completely used. The procedure is repeated three times a day.
The course of treatment with rinsing with Dioxidin solution is 5 days (unless otherwise recommended by the attending physician).
How to use Dioxidin for gargling
The active substance of the drug can kill infections in the throat and takes part in the restoration of the mucous membrane. The solution is used to rinse the mouth for diseases such as sore throat and pharyngitis. It is necessary to mix the contents of the ampoule with 200 ml of purified water. After this, you can gargle for a few seconds. The solution must be used completely. 3-4 procedures can be performed per day. The duration of the therapeutic course is up to 5 days. Only a specialist can extend the appointment or prescribe a repeat course after examination.
Reviews about Dioksidin
Reviews about Dioxidin are quite contradictory. Most patients to whom it was prescribed describe the drug as a very effective remedy, especially for diseases accompanied by a purulent-septic process .
Negative reviews are due to the fact that the drug is quite toxic (its therapeutic dose is only slightly less than the toxic one), and its use is often accompanied by unwanted side effects.
Reviews of the ointment allow us to conclude that Dioxidin in this dosage form does not cause irritation to the skin, stimulates tissue healing and generally has a beneficial effect on the wound process, however, with prolonged use, microorganisms develop resistance to the drug.
Dioxidin is used primarily as a reserve agent, that is, its help is resorted to only in extreme cases.
The instructions clearly indicate that the drug is intended exclusively for the treatment of adult patients, but it is often used to treat otolaryngological diseases in children.
Despite the fact that Dioxidin does not have an evidence base that would confirm the safety of its use in pediatrics, nasal drops, according to reviews left on the Internet, are a fairly effective remedy for such forms of pathological runny nose as, for example, purulent rhinitis .
Meanwhile, Dioxidin is not included in the standards for the treatment of ENT diseases , and there is no official data on its use as nasal drops. Thus, when prescribing this drug to a child, both the doctor and parents (if they agree with the prescribed treatment regimen) act at their own peril and risk.
It should be noted that until now, the use of the medicine has not been associated with any complications or negative consequences for the child’s body.
Dioxidine price, where to buy
The price of Dioxidin differs depending on the form of release of the drug. For example, the average price of Dioxidin in ampoules with a concentration of hydroxymethylquinoxaline dioxide 0.5% (this form is used for preparing nasal drops) is 547 rubles.
The cost of packaging ampoules with a 1% solution is from 477 to 795 rubles (depending on the manufacturer and the number of ampoules in the package). Ointment for external use can be purchased for approximately 385 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Dioxidin solution for intracavity.
intro., places and adv. approx. 0.01 g/ml 10 ml 10 pcs Grotex LLC 584 rub. order - Dioxidin ointment 5% 30g Biosynthesis OJSC
430 rub. order
Pharmacy Dialogue
- Dioxidin ointment (tube 5% 30g) Biosynthesis OJSC
422 rub. order
- Dioxidin (amp. 1% 10ml No. 10) Valenta Pharmaceuticals OJSC
550 rub. order
- Dioxidin (solution d.inf. and nar. approx. 5 mg/ml 10 ml No. 10) Grotex LLC
RUR 525 order
- Dioxidin (amp. 0.5% 10ml No. 10)Novosibkhimpharm OJSC
RUB 249 order
show more
Pharmacy24
- Dioxidin 1% 10 ml No. 10 solution
193 UAH. order
PaniPharmacy
- Dioxidin ampoule Dioxidin solution d/in. 1% amp. 10ml No. 10 Ukraine, Farmak OJSC
219 UAH. order
show more