- General information
- Historical facts
- Effect on the body
- How to recognize a drug addict
- Tests for Phenazepam
- How long does it stay in the body?
- How long do drug addicts live?
- Analogs
- How to speed up elimination at home
- Detoxification in hospital
- Perdose
- How to recognize and what to do
- Rehabilitation
- Coding
- Why you can’t undergo rehabilitation at home or on an outpatient basis
- Resocialization and work with codependents
- How to quit on your own
Attention! Drug use causes irreparable harm to health and poses a danger to life!
General information
The drug phenazepam is a typical tranquilizer. It is used to normalize sleep, combat anxiety, and relieve convulsive syndrome in epilepsy. Fenozepam is available in injection form or in tablets. All central effects of the drug are achieved through stimulation of benzodiazepine receptors.
The effect of the drug extends to the reticular formation, nonspecific centers of the thalamus and the amygdala complex. The muscle relaxant effect is based on the ability to block spinal reflexes. The tranquilizer is well absorbed through the gastrointestinal tract, after which it is metabolized in the liver and excreted by the kidneys.
Phenazepam is available without a prescription. Doctors sometimes prescribe it to improve sleep, relieve anxiety during performances or in extreme situations. The first aid kit always contains Phenazepam in injection form to relieve seizures in epilepsy or damage to the central nervous system.
All drugs from the benzoidazepine group cause sleep lasting up to 6-8 hours. But the longer the sleep, the stronger the drowsiness, fatigue and depression will be during the next day after taking the drug.
Taken from: Pharmacology, tenth edition by D.A. Kharkevich
The drug is not considered a drug, but addiction can develop from it. In addition, with each subsequent dose, to achieve the desired effect, it is necessary to increase the dose. If you increase the dosage without consulting a doctor, this will lead to acute drug poisoning with possible death.
Autonomic symptoms and nostalgia for neuroses
Summary
The article contains data on the connection of autonomic symptoms, stress and mental disorders with the activity of various types of neurons. It is shown why patients with vegetative symptoms turn not to psychiatrists, but to internists. Currently, it is difficult for internists to treat vegetative symptoms, which are classified as mental disorders. Effective tranquilizers require a special prescription form, and antidepressants require consultation with a psychiatrist. Many internists remember the time of neuroses, when they could treat vegetative symptoms themselves. Perhaps it is time to allow internists to diagnose and treat mental disorders with autonomic symptoms. Pending reforms, tofisopam (Grandaxin) can be used to treat autonomic symptoms.
Summary
The article contains data on the connection of autonomic symptoms, stress and mental disorders with the activity of different neurons. It is shown why patients with vegetative symptoms do not apply to psychiatrists, but to internists. Currently it is difficult for internists to treat vegetative symptoms. They are referred to as mental disorders. Effective tranquilizers require a special form of recipes. Consultation with psychiatrists is required to prescribe antidepressants. Many internists remember the time of neurosis, when they themselves could treat the vegetative symptoms. Perhaps it is time to allow internists to diagnose and treat mental disorders with vegetative symptoms. Pending reforms for the treatment of vegetative symptoms, you can use tofizopam (Grandaxin).
Severe vegetative symptoms1 have long been considered as manifestations of neuroses (hypochondriacal, hysterical, anxious, etc.) (1). This diagnosis was quite acceptable to the patients. It indicated a neural origin of their symptoms and was not associated with mental disorders (diseases such as schizophrenia). In other words, the diagnosis was closer not to “psychiatry”, but to “neurology” (neuropathology) - a medical specialty whose representatives traditionally treated patients in regular clinics or clinical hospitals. As a result, patients could seek help in their “familiar” healthcare institutions, avoiding contact with psychiatric services.
In addition, if a patient was frightened by even such a diagnosis as “neurosis,” he could easily be “ennobled.” For vegetative symptoms, almost all therapeutic specialties had their own terms - syndromes (2):
- hyperventilation (pulmonology),
- vegetative dystonia (neurology),
- neurocirculatory dystonia and da Costa (cardiology)
- irritable bowel (gastroenterology),
- psychogenic pain in the head, neck, back (neurology), etc.
This situation suited everyone for a long time. To the point that “neuroses” began to disappear from domestic psychiatry, as patients with vegetative symptoms increasingly sought help from psychiatric institutions. The very admission of such a patient to a psychiatric hospital was often considered as a sign of the extreme severity of the condition and the inability to remain within the framework of “conventional” medicine. Based on this, the condition of such a patient was often qualified not as “neurosis”, but as “schizophrenia,” albeit poorly progressive or sluggish (3-4).
The current situation began to change after the complete disappearance of “neuroses” from the International Classification of Diseases, 10th revision (ICD-10) (2). Autonomic symptoms, according to the new classification, have become a diagnostic sign of other mental disorders. All of them were included in the heading “neurotic, stress-related and somatoform disorders” (NSSD). These diagnoses were new and could not cause unpleasant associations for anyone. However, their names (for example, panic disorder, social phobias, agorophobia, etc.) were already difficult to associate with “nerves.” On the contrary, they directly indicated that the patient suffered from a mental disorder.
At the same time, the “therapeutic” synonyms for neuroses listed above began to be viewed as outdated and incorrect. Deprived of “convenient” and “euphonious” diagnoses, patients with vegetative symptoms became “strangers” to clinics and clinical hospitals, although they continued to seek help there. Patients of the NSSSR could not “find a new home” in domestic psychiatry. After all, “new” diagnoses, similar to previous “neuroses,” are established extremely rarely (5).
At the same time, it became more difficult for physicians of therapeutic specialties to treat vegetative symptoms with the help of psychotropic drugs in clinics and clinical hospitals. During the times of “neuroses” and their synonyms, tranquilizers could be freely prescribed. Their “calming” name was consistent with the ideas of doctors and patients about the “nervous” origin of vegetative symptoms. This practice has not encountered any opposition from health care organizers. However, then the main tranquilizers, called benzodiazepines after the chemical structure of their molecules, began to be blamed for the frequent formation of drug dependence (6). In Russia, unlike other countries of the world, these drugs were on the list of drugs subject to subject-quantitative registration (7). For a long time, most benzodiazepines have to be prescribed on a special prescription form, and this has affected the frequency of prescriptions. Benzodiazepines are prescribed less and less outside of psychiatry.
The situation could be saved by antidepressants, which are often used abroad to treat NSSSR, the direct heirs of “neuroses” (8). However, this did not happen in our country for several reasons. Thus, in the instructions for antidepressants, their indications are formulated in accordance with ICD-10 (9). Meanwhile, it was already noted above that in this classification, vegetative symptoms are considered as manifestations of mental disorders. As a result, each prescription of antidepressants turns out to be tantamount to establishing a “psychiatric” diagnosis, indicating that the patient has a mental disorder.
In addition, many domestic health experts have long argued that any psychotropic drugs can only be prescribed by a psychiatrist (10). As a result, treatment of autonomic symptoms required consultation with this specialist. But this had to be agreed upon with the patient in advance. He had to explain why he needed a consultation with a psychiatrist and the prescription of an antidepressant for vegetative symptoms. And this despite the fact that the very name of such drugs indicates that they should be used for depression - a fairly severe mental disorder that has its own diagnostic criteria.
Recommendations for the use of certain antipsychotics have added further confusion to the situation (11). Here, quite logical questions could be asked not only by patients, but also by doctors of therapeutic specialties who identified vegetative symptoms. For example, why should “neuroses” (even former ones) be treated in the same way as psychoses? How to explain to patients that medications used for schizophrenia help their condition? How to combine antipsychotics with patient monitoring in a clinic?
The sharp reduction in the arsenal of drugs aimed at treating vegetative symptoms observed outside psychiatry contributed to a kind of idealization of bygone “neuroses.” Doctors of therapeutic specialties recalled with genuine warmth that in the past they themselves could provide assistance to such patients, at least with the help of benzodiazepine tranquilizers. However, lost diagnoses cannot be returned. And in the new International Classification of Diseases, 11th revision (ICD-11), “neuroses” are again absent (12). Perhaps the time has come to allow internal medicine physicians to independently diagnose and treat numerous mental disorders that include autonomic symptoms.
However, such a prospect still seems too vague. To implement it, it is necessary to resolve many issues related to the creation of national recommendations, development and implementation of relevant orders. It is necessary to assess how well the presented approach will comply with the existing legislative framework, for example, the law on mental health care (13), etc.
It is much easier to find and use the still available opportunities for the treatment of vegetative symptoms in clinics and clinical hospitals. First of all, this possibility is associated with the use of two benzodiazepine tranquilizers: bromodihydrochlorophenylbenzodiazepine (Phenazepam) and tofisopam (Grandaxin). Both drugs are prescribed on “regular” prescriptions, although the first of them has the ability to cause drug dependence when taken long-term in large doses (more than 4 mg/day) (14). Accordingly, the prescription of bromodihydrochlorophenylbenzodiazepine and tofisopam (15) is not associated with subject-quantitative accounting and should not cause any particular difficulties for physicians of therapeutic specialties. In addition, both drugs retained the same formulations of indications, allowing them to be prescribed for autonomic symptoms (autonomic dysfunction, autonomic lability, autonomic disorders, cardialgia). As a result, the reasons for prescribing bromodihydrochlorophenylbenzodiazepine (Phenazepam) and tofisopam (Grandaxin) should be quite clear to patients.
When prescribing, you need to take into account the severity of side effects and various restrictions when taking the drugs in question. They are presented in table. 1.
Table 1. Comparison of bromodihydrochlorophenylbenzodiazepine (Phenazepam) and tofisopam (Grandaxin) in terms of tolerability (14,15).
| Phenazepam | Grandaxin | |
| Side effects from the central nervous system and peripheral nervous system | - at the beginning of treatment (especially in elderly patients) - drowsiness, fatigue, dizziness, decreased ability to concentrate, ataxia, disorientation, gait instability, slowed mental and motor reactions, confusion; - rarely - headache, euphoria, depression, tremor, memory loss, impaired coordination of movements (especially at high doses), depressed mood, dystonic extrapyramidal reactions (uncontrolled movements, including the pelvis), asthenia, muscle weakness, dysarthria, epileptic seizures (in patients with epilepsy); - extremely rarely - paradoxical reactions (aggressive outbursts, psychomotor agitation, fear, suicidal tendencies, muscle spasms, hallucinations, agitation, irritability, anxiety, insomnia). | - headache, insomnia, increased irritability, and agitation may occur. - sometimes there is confusion, and convulsive seizures may occur in patients with epilepsy. |
| Impact on the ability to drive vehicles and operate machinery | During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions. | Grandaxin does not have a significant effect on attention and the ability to concentrate |
Bromodihydrochlorophenylbenzodiazepine (Phenazepam) is less well tolerated. When using it, you have to observe certain precautions related to driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions. Therefore, for the treatment of vegetative symptoms in clinics and clinical hospitals, it is best for physicians of therapeutic specialties to use tofisopam.
But is it possible to treat vegetative symptoms with tofizopam “as before”, without focusing the patient’s attention on the fact that he has a mental disorder? The answer to this question lies in the data on the mechanisms of their formation. It is believed that the symptoms of NSSSR resemble changes that occur in the human or animal body during a normal (adaptive) reaction to stress. This response is formed with the participation of different neuronal systems (16). But two of them, GABAergic2 (GA) and serotonin (S), appear to be of decisive importance. The role of the first of them under normal conditions is to ensure rapid inhibition of any neurons (dopamine - D, norepinephrine - N, acetylcholine - A, histamine - GI, glutamate - GL, etc.). The activity of the second is rather associated with the selective inhibition of those neurons that exhibit increased activity and stand out from the general “symphony” of the vital activity of the nervous system (17).
Under the influence of stress, the activity of the GA and C systems decreases (Table 2).
Table 2. Mechanisms of formation of various manifestations of stress and NSSSR (16,17).
| neuronal activity | manifestations | |
| stress | NSSSR | |
| ↓GA,S + ↑D,N,A,GI,GL | anxiety | anxiety, phobias associated with a wide range of situations |
| fading | stupor, chronic feeling of “numbness” and emotional dullness, “stupefaction” | |
| undirected movements | agitation, psychomotor agitation | |
| flight or fight | avoidant or aggressive behavior | |
| ↓GA,S + ↑D,N | activation of thinking | fear of death, loss of self-control, or madness |
| ↓GA,C + ↑A | memory activation | intrusive memories, dreams or nightmares |
| ↓GA,S + ↑GI | increased level of wakefulness | sleep disorders (insomnia) |
| ↓HA,S + ↑H | increased blood pressure, heart rate, respiratory rate | panic attacks: 1) cardiac with palpitations, pain in the heart, pulsation of blood vessels, dizziness; 2) hyperventilation with rapid breathing, shortness of breath, feeling of lack of air, panic attacks |
| ↓GA,S + ↑GI,D,A | increased secretion of gastric juice, increased peristalsis of the gastrointestinal tract | epigastric discomfort, nausea, retching or defecation |
| ↓GA,S + ↑GL,N | increased muscle tone | motor tension with fussiness, tension headaches, tremors, inability to relax |
At the same time, a variety of neurons are disinhibited. Their rapid and simultaneous activation is accompanied by the development of anxiety. In addition, any purposeful activity is blocked. So, for a short time, a victim of stress may freeze and begin to rush around senselessly. But then the decline in the activity of some systems (↓GA, S) and the disinhibition of others (↑D, N, A, GI, GL) begins to work to overcome the stressful situation. The victim of stress may try to escape or fight. This is also facilitated by an increase in the activity of GI neurons, which are responsible for the level of wakefulness. Increasing the “tone” of D-, N-, and A-neurons, which are “responsible” for abstract thinking, the speed of thought processes and memory (respectively), allows you to more intensively and quickly think about the degree and nature of the threat, drawing on accumulated life experience for this.
Adaptation to stress is also achieved by changing the state of the autonomic nervous system, which regulates the functions of muscles and internal organs. For example, the H-system increases blood pressure (BP), the number of heart contractions (HR) and their strength, as well as the number (number) of respiratory movements (RR). Accordingly, an increase in the activity of H-neurons leads to an increase in blood pressure, heart rate and respiratory rate. The GL and H systems control the tone of the striated muscles, and with additional activation of these nerve cells, the muscles contract faster and more intensely. GI neurons influence the level of gastric juice secretion. As a result, when the activity of these neurons increases, the digestion process in the stomach accelerates. The functions of the D- and A-systems include the control of intestinal motility. Accordingly, high activity of D- and A-neurons accelerates the process of passage of food through the gastrointestinal tract.
The adaptive significance of the described “vegetative” processes is quite clear. An organism exposed to stress prepares for active actions (for example, flight or fight), which will require the mobilization of additional forces. In this situation, it is necessary to increase the flow of oxygen to various organs, including muscles (H-neurons). It is necessary to speed up the digestion of food and/or quickly empty the intestines (GI-, A-, D-neurons) in order to relieve the body experiencing stress from the “extra” load.
Manifestations of NSSSR seem to continue the symptoms of a normal reaction to stress, but there are also differences. For example, the activity of neurons during an ordinary reaction to stress changes only in connection with a real traumatic situation. Moreover, such changes are limited in time. As stress is managed, the normal functioning of these systems is gradually restored3. Meanwhile, the relationship between a stressful situation and the development of NSSSD is characteristic of only three disorders (acute stress reaction, post-traumatic stress disorder and adjustment disorder (2)). All other NSSSRs occur spontaneously or in situations that are not dangerous (2). In this case, disturbances in neuronal activity can last for quite a long time. The so-called undulating course with periods of improvement and deterioration of the condition.
However, perhaps it is the similarity of NSSSR with manifestations of normal stress that makes patients doubt that their complaints belong to a mental disorder, especially if they are bothered by autonomic symptoms associated with changes in muscle tone, blood pressure levels, heart rate, respiratory rate, gastrointestinal motility tract, etc. Therefore, patients are reluctant to agree to a consultation with a psychiatrist and prefer to seek help from doctors of therapeutic specialties. If doctors prescribe tofisopam (Grandaxin) to patients, they will have the right to count on effective treatment not only of vegetative symptoms, but also of other (“mental”) manifestations of NSSSR. This drug, like many other benzodiazepine tranquilizers, increases the activity of the GA system due to its effect on the so-called. GABAA receptors (16). And since the decrease in the “tone” of this system (along with the serotonin system) plays a key role in the pathogenesis of NSSSR, tofisopam will act on all their symptoms.
As for the advantages in tolerability of the drug in comparison with other benzodiazepine tranquilizers (for example, bromodihydrochlorophenylbenzodiazepine - Phenazepam), this is explained by the drug’s effect on a limited number of GABAA receptors located in the basal structures of the brain (18). In addition, tofisopam has its own binding site on these receptors, which is different from those used by “conventional” benzodiazepines (19). As a result, the drug does not cause excessive inhibition of the central nervous system, which is especially important when treating patients in therapeutic practice (15).
Of course, a complete arsenal of psychotropic drugs for the treatment of vegetative symptoms cannot consist only of tofisopam. The presented data on the mechanisms of formation of these disorders make it possible to understand why in this situation some benzodiazepine tranquilizers, antidepressants and antipsychotics are successfully used abroad. The former activate the main inhibitory GA system, and the latter (with the exception of agomelatine) act in a similar way on the C system. As for antipsychotics, many of them are capable of inhibiting D-, N-, GI-, and A-neurons. However, the question of using all these drugs in the treatment of vegetative symptoms in therapeutic practice is seriously complicated for the reasons stated at the beginning of the article.
Bibliography.
- List of ICD-9 codes: Section V. https://ru.wikipedia.org/wiki/List_ICD-9_codes:_Section_V
- Mental disorders and behavioral disorders (F00 - F99) Class V ICD-10, adapted for use in the Russian Federation Moscow 1998 https://psychiatr.ru/download/1320?view=1&name=ICD-10+adapted+for+RF+ 1998.pdf
- Smulevich A. B. Low-progressive schizophrenia and borderline states, M., 1987.
- Smulevich A. B. Special forms of schizophrenia. Sluggish schizophrenia. In the book. Endogenous mental illnesses. Ed. A.S. Tiganova. https://ncpz.ru/lib/54/book/29/chapter/9
- Kalinina E.V. Characteristics of patients diagnosed with a mental disorder for the first time in their lives in the Chuvash Republic (clinical, epidemiological and socio-demographic aspects). Diss. ...cand. honey. Sci. Moscow, 2006.
- Long-term use of benzodiazepines: Definitions, prevalence and usage patterns—a systematic review of register-based studies. Kurko TA, Saastamoinen LK, Tähkäpää S, Tuulio-Henriksson A, Taiminen T, Tiihonen J, Airaksinen MS, Hietala J. Eur Psychiatry. 2015 Nov;30(8):1037-47. doi: 10.1016/j.eurpsy.2015.09.003.
- List of Medicines subject to PCU. https://www.ecopharmacia.ru/publ/organizacija_i_ehkonomika_farmacii/uchet_i_otchetnost_apteki/novyj_perechen_ predmetno_kolichestvennogo_ucheta_perechen_pku/11-1-0-852
- Drobizhev M.Yu., Kikta S.V., Machilskaya O.V. Cardiac psychiatry. Translation problems. Cardiovascular therapy and prevention. 2016; 15 (4): 88-98.
- Recommendations of the World Federation of Societies of Biological Psychiatry (WFSBP) on the pharmacotherapy of anxiety, obsessive-compulsive and post-traumatic disorders. https://psychiatr.ru/download/2041?view=1&name=stpr_2011_03.pdf
- Krasnov V.N., Bobrov A.E., Dovzhenko T.V., Starostina E.G., Kuznetsova M.V. Problems, prerequisites and necessary measures to improve the interaction of psychiatric (psychotherapeutic) services with primary care doctors. Mental health. 2011; 63 (8): 3-12.
- Teraligen - official instructions for use. https://medi.ru/instrukciya/teralidzhen_4065/
- 06 Mental and behavioral disorders. https://icd11.ru/psihicheskie-rasstroistva-mkb11/
- Law of the Russian Federation dated 07/02/1992 N 3185-1 (as amended on 07/19/2018) “On psychiatric care and guarantees of citizens’ rights during its provision” https://www.consultant.ru/document/cons_doc_LAW_4205/
- Phenazepam tablets - official instructions for use. https://medi.ru/instrukciya/fenazepam-tabletki_9485/
- Grandaxin - official* instructions for use. https://medi.ru/instrukciya/grandaksin_940/
- Stahl SM Stahl's essential psychopharmacology: neuroscientific basis and practical application. – 3rd ed. Cambridge University Press, 2008. – 1117P.
- Drobizhev M.Yu., Kikta S.V., Machilskaya O.V. Cardiac psychiatry. Translation problems. Cardiovascular therapy and prevention. 2016; 15 (4): 88-98.
- Horváth EJ, Horváth K, Hámori T, Fekete MI, Sólyom S, Palkovits M. Anxiolytic 2,3-benzodiazepines, their specific binding to the basal ganglia. Prog Neurobiol. 2000 Mar;60(4):309-42.
- Rundfeldt C1, Socala K, Wlaz P. The atypical anxiolytic drug, tofisopam, selectively blocks phosphodiesterase isoenzymes and is active in the mouse model of negative symptoms of psychosis. J Neural Transm. 2010 Nov;117(11):1319-25.
M.Yu. Drobizhev, Doctor of Medical Sciences, Head of the Educational Department of the Educational Center of the Association of Medical and Pharmaceutical Universities of Russia
Contact Information -
E.Yu. Antokhin, Candidate of Medical Sciences, Associate Professor, Head of the Department of Clinical Psychology and Psychotherapy of the Orenburg State Medical University of the Russian Ministry of Health.
R.I. Palaeva is an assistant at the Department of Clinical Psychology and Psychotherapy at the Orenburg State Medical University of the Russian Ministry of Health.
S. V. Kikta, Candidate of Medical Sciences, Head. Department of the Federal State Budgetary Institution "Polyclinic No. 3" of the Administration of the President of the Russian Federation, Moscow
1 See below
2GABA – gamma-aminobutyric acid
3 A description of these processes is beyond the scope of this article.
Historical facts
The drug was invented in the 1970s. The developers who received the state order for the new medicine were the scientific directors of the departments of pharmacology from the Odessa Institute of Physics and Chemistry. After successful research and launch of the drug on the market, the group of voters received the USSR State Prize.
The peak use of the drug came at the end of the 80s, when facts of abuse of barbiturates were published and proven. Phenazepam and its analogues have become alternative drugs with similar effects but fewer adverse reactions.
Content:
- Description of the drug 1.1. Contraindications
- Phenazepam after binge drinking: features of use in alcoholism 2.1. Dosing features 2.2. Possible adverse reactions
- Why you can’t take Phenazepam for sleep after a binge without consulting a doctor
Phenazepam belongs to the group of benzodiazepine tranquilizers, which have been widely used in psychiatry, neurology and other areas of medicine for more than 70 years. In narcology, this drug is one of the main ones in the complex treatment of not only alcoholism and drug addiction, but also other forms of addiction, accompanied by increased anxiety, sleep disorders, and neuroses. But along with its pronounced therapeutic effectiveness, Phenazepam, like other benzodiazepines, if taken uncontrolled, can cause the development of drug dependence. That is why the dosage, regimen and duration of use of Phenazepam after a binge for insomnia should be selected only by a doctor.
Effect on the body
After the drug binds to benzodiazepine receptors and the reticular formation, the patient becomes calm and anxiety is eliminated. Then drowsiness appears, smoothly turning into sleep. In addition, the effect of the drug on limbic structures, reflex connections and the thalamus leads to the fact that the drug has the following effects:
- reduces feelings of fear;
- relieves irritability;
- increases emotional lability;
- reduces the manifestation of phobias;
- relieves alcohol and drug withdrawal syndrome;
- relieves muscle spasms;
- prevents nervous tics.
But you should be careful when using Phenazepam. It has a pronounced toxic effect on the liver and heart. If this tranquilizer is abused, the following disorders may occur:
- increased drowsiness, feeling tired;
- nausea and vomiting;
- dizziness;
- fast fatiguability;
- hematopoietic disorders (leukopenia, thrombopenia);
- urinary retention or incontinence;
- epileptic seizures;
- visual impairment;
- depression;
- constipation or diarrhea;
- increased activity of liver enzymes, jaundice;
- dysmenorrhea;
- hallucinations.
To achieve a narcotic effect, Phenazepam is not used in isolation. More often it is combined with other drugs to enhance the result. When the pharmaceutical dose is increased by 2-4 times, the patient's condition becomes the same as with alcohol intoxication or an overdose of barbiturates. But the negative effects and disruption of internal organs are tens of times stronger.
At the moment, benzodiazepanes are the most adequate means to combat insomnia, which is caused by emotional tension, stress, anxiety and worry.
Taken from: Pharmacology, tenth edition by D.A. Kharkevich
What are the consequences of using Phenazepam with alcohol?
Phenazepam can be used as a complex treatment for alcoholism to relieve withdrawal symptoms. A prerequisite for successful treatment is complete abstinence from drinking alcohol. If a person does not follow the doctor’s recommendations and continues to drink alcohol, the following consequences are possible:
- confusion;
- slowing down the respiratory rate;
- development of bradycardia;
- dyspnea;
- feeling of lack of air;
- decreased blood pressure;
- pronounced tremor;
- drowsiness;
- speech disorders;
- lack of coordination of movements;
- very tired.
In the presence of concomitant pathologies and due to an overdose of Phenazepam, the joint use of alcoholic beverages can lead to death.
Alcohol consumption also increases the likelihood and severity of side effects:
- memory and intelligence impairment;
- psychomotor agitation;
- attacks of anger and aggression, increased irritability;
- hallucinations;
- suicidal thoughts;
- severe insomnia;
- severe headaches;
- uncontrollable vomiting;
- liver damage;
- damage to the urinary system.
How to recognize a drug addict
As with any addiction, a drug addict can be in two states: the effects of the drug and the state of withdrawal. In the first case, the patient will be sleepy, lethargic, and answer questions slowly. A person can sleep for a long time. Drug addicts under the influence of Phenazepam react inadequately to external stimuli, they have an increased pain threshold, impaired breathing and a slow heartbeat.
The picture resembles intoxication with alcohol, but there is no smell or bottles of alcohol. But near such a drug addict you can find various packages of medicines and empty packages of pills.
In the case of withdrawal, the opposite is true. The peculiarity of taking tranquilizers is that they cannot be abruptly stopped. If a drug addict runs out of a new dose of medication, he will suffer from insomnia and his general condition will be anxious. Nervous tics will appear, the addict will move into the aggressive phase. When searching for a dose, such a person can deceive those closest to him, sometimes even hit them.
It is difficult to reliably recognize that a person is dependent on tranquilizers. Therefore, the best way to determine drug addiction is testing. Only in this way can you either confirm or eliminate your suspicions.
Release form of Phenazepam
The drug is available in the form of tablets and injections for intramuscular and intravenous administration.
The drug was recognized as dangerous and began to be sold by prescription only recently, so it can still be found in home medicine cabinets as a remedy for insomnia. For practically healthy people (with anxiety, sleep problems, nervous tension, lower back pain) it is no longer prescribed, choosing drugs with a milder effect. Phenazepam is now used only for severe mental disorders and for the relief of seizures during epileptic seizures.
Tests for Phenazepam
You can check for the presence of benzodiazepines in the body using a conventional rapid test. The cost of these tests is from 40 to 100 rubles. Urine is tested at home; blood testing is carried out only in laboratories.
Please note that the effect of phenazepam is similar to other narcotic substances, therefore, in parallel with the test for benzodiazepines, a rapid test is carried out using a tablet for 10 drugs. This allows you to quickly check traces of narcotic substances and, if necessary, request laboratory confirmation.
Laboratory confirmation must be done if a person committed an offense under the influence of a drug. The results of rapid tests have no legal force.
To study biomaterials of a drug addict, methods of enzyme immunoassay, gas chromatography-mass spectrometry or gas-liquid spectrometry are used. These methods are written down in the relevant decrees, and can be used in court as a confirmed diagnostic method.
Phenazepam is quickly eliminated from the body through the kidneys, so it is important to know how much time has passed since the last use of the drug.
Please note that there is no specific test for Phenazepam. There is a test for benzodiazepines. If the patient took any drug from the benzodiazepine group (including Phenazepam), the result will be positive.
Comparison of ease of use of Phenazepam and Tranquesipam
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Phenazepam is approximately the same as Tranquesipam. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-13 10:31:30
How long does it stay in the body?
The rate of elimination from the body depends on the ability of the liver to process the components of the drug. On average, tranquilizers are eliminated in 3-5 days. But the exact period depends on both the period of use and the age of the addict.
It is necessary to consider whether it was taken together with other drugs or alcohol. All this slows down the functioning of internal organs and leads to a slower elimination of the drug from the body.
Phenazepam is excreted through the kidneys, so the best method is to test your urine. Metabolites of the drug can be found in urine within 3-4 days. In the blood - 12-18 hours. There are no other data on hair or saliva testing for Phenazepam.
Get help now
Do any of your relatives or friends have an addiction? Have you tried in every possible way to help, but as a result the person still returned to his past life?
You are not the first to encounter this problem, and we can help you.
We guarantee anonymity, we will persuade you to undergo treatment, and we will help you choose a center.
Call us
8
or
Call me
Good news
A new antipsychotic for the maintenance treatment of schizophrenia from the Janssen company, part of the Johnson & Johnson pharmaceutical division, Trevicta, has been registered in Russia. It has a long-lasting effect and can be used only 4 times a year, that is, every three months, which is much better than monthly injections of long-standing antipsychotics.
Trevicta is now an antipsychotic with the longest dosing interval registered in our country. It maintains its optimal concentration of paliperidone in the patient’s blood for a long time, which is why it requires such rare use.
Prescribe three months of Trevicta to patients with a stable condition after treatment with other drugs. It helps reduce the risk of relapse due to its prolonged action, has a low risk of side effects, and does not create withdrawal syndrome if treatment is abruptly stopped. This makes it possible for a patient with schizophrenia to socialize and maintain his constant normal state.
How long do drug addicts live?
Life expectancy with tranquilizer abuse reaches 3-4 years. But the higher the dose and the more often it is taken, the fewer years the addict has to live. In pharmaceutical doses, the drug does not affect internal organs and the nervous system. If you systematically exceed the permissible limit, irreversible changes will occur in the cerebral cortex. Liver cirrhosis with chronic liver failure may develop.
Phenazepam damages the kidneys, causing chronic kidney disease (CKD or kidney failure). When decompensation occurs in the functioning of the kidneys and liver, a person dies, even if assistance is started.
Analogs
In terms of their effect on the body, barbiturates are analogues of benzodiazepines. They act similarly on the central nervous system and have the same effect on internal organs.
In terms of chemical composition, all drugs from the benzodiazepine group are analogues of Phenazepam, for example:
- Fezanef;
- Phenorelaxan;
- Elzepam;
- Gidazepam;
- Clobazam;
- Lorazepam.
Among drugs, opiates cause similar effects. They also inhibit processes in the central nervous system, but the mechanism for the development of these effects is different.
How to speed up elimination at home
Breeding at home can be hazardous to health. During the rapid release of the drug and its metabolites, rebound syndrome may occur. This means that all inhibitory effects that the drug had will be suppressed by antagonistic mediators. That is, if Phenazepam relaxes the muscles, then if it is abruptly discontinued, cramps may begin. The same applies to sleep and other functions that are affected by tranquilizers.
It is better to limit withdrawal at home to 3-4 procedures and carry it out only in case of an overdose caused by a desire to get drug intoxicated or during a suicide attempt. In other cases, if there are no symptoms of overdose, there is no need to accelerate the elimination of the drug.
Algorithm of actions:
- Rinse the stomach. You can do this by drinking plenty of water, up to two liters of water, and then mechanically induce vomiting (press the root of the tongue with two fingers). This procedure must be repeated 2-3 times. They are effective in the first hour and a half after taking the tablets.
- Take sorbents. It is recommended to take one tablet of activated carbon per 10 kilograms of body weight. You can do more, there will be no harm from the sorbents.
- Drink plenty of fluids to speed up kidney function. This technique is called forced diuresis. Due to heavy drinking, the fluid that is excreted by the kidneys will “pull back” some of the drug metabolites.
If after these procedures lethargy remains and the person is inhibited, you can brew him strong coffee. Caffeine stimulates the nervous system and “unblocks” some of the nerve synapses that inhibit the reaction.
It is better to speed up the elimination of the drug in a hospital setting. Then it is possible to monitor the patient’s general condition and carry out specific therapy with antidotes. In addition, in cases of life-threatening symptoms, emergency medical care can be provided.
Detoxification in hospital
In the hospital, first of all, gastric lavage is performed using a siphon. In this way, you can cleanse the entire stomach without artificially stimulating the vomiting center. After gastric lavage, sorbents (activated carbon, Smecta, white carbon) may be prescribed.
Instead of drinking plenty of fluids in the hospital, infusion therapy with 5% glucose and saline is carried out. This helps remove drug toxins from the liver and kidneys. This way, cleansing occurs faster and symptoms of poisoning or overdose disappear.
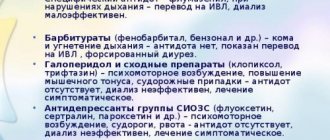
The next step is to prescribe specific antidotes to benzodiazepines. These are the following:
- Mesocarb;
- Flumazenil.
Both drugs must be calculated correctly. If the dosage is incorrect, it can only make things worse.
If possible, in a hospital or special rehabilitation clinics, the blood is purified using an “artificial kidney” device, and the patient is sent for hemodialysis. All methods are based on hardware blood purification; they are relevant for detoxification. Although there is evidence that in case of an overdose of Phenazepam, hemodialysis is ineffective.
It has been established that among all drugs from the benzoidazepine group, Phenazepam is one of the best anxiolytics.
Taken from the scientific article: “The effectiveness of phenazepam as part of complex therapy in patients with anxiety-depressive syndromes.” Authors: M.E. Statsenko, O.E. Sporova, O.A. Talker.
Overdose
An overdose of Phenazepam most often occurs for three reasons: an overdose when increasing the dose on your own, when trying to get drug intoxicated, and when attempting suicide.
An overdose always occurs. This is due to the fact that with each subsequent dose of the drug, receptor insensitivity to its active substances occurs. This process is called the development of tolerance. That is, with each subsequent reception the severity of the effects is less, and they end faster.
If help is not provided in time, a person may die from respiratory failure or cardiac arrest.
How to recognize and what to do
In case of an overdose of any drug from the group of tranquilizers, the following symptoms will immediately appear:
- depression and confusion;
- decreased blood pressure;
- slowing and stopping of the heart;
- slowing and stopping breathing;
- nystagmus;
- convulsions or tremors of the limbs;
- decreased response to tendon reflexes.
With such symptoms, a coma develops, and the person dies without treatment. The main help is gastric lavage, taking sorbents and intravenous administration of a specific antidote: flumazenil.
If necessary, artificial respiration and chest compressions must be performed before the ambulance arrives. You need to press on the chest at intervals of 2 times in 1 second. You need to inhale air into the person’s mouth or nose every 30 presses.
Rehabilitation
Considering that physical dependence on Phenazepam practically does not develop, the main task of rehabilitation is the psychological restoration of the individual, programming a new style of behavior, the patient’s adaptation to society and working with codependent people.
In complex addiction therapy, the location where rehabilitation is carried out plays a role. As a rule, at home or with friends, any attempts to quit end with taking the same drugs or other drugs with a similar effect.
Antidepressive therapy is sometimes added to the rehabilitation complex. With the right dosage, this is a good technique that allows you to get rid of the consequences of depletion of your own mediators.
Coding
Coding doesn't work with dependencies. More than 1000 studies have shown that this method has no evidence base and its use is not rational. Therefore, we can conclude that specialists engage in coding solely for personal gain. The best method of treatment is the correct rehabilitation complex. Coding, hypnosis and similar methods do not work.
Why not at home or on an outpatient basis?
With abrupt withdrawal of Phenazepam, rebound syndrome occurs. This means that without the drug, all the processes that were inhibited by the drug will become 3-4 times more intense. This leads to convulsions and even loss of consciousness. Therefore, you need to quit gradually, under the control of tests and after consultation with a specialist.
In an outpatient setting, it is very difficult to monitor whether the patient is complying with the rehabilitation program. At home, there are no barriers or incentives that force you to stop using drugs. In addition, home conditions mean constant contact with possible active drug addicts. If communication is not stopped, the person will not leave on his own.
Another disadvantage of home rehabilitation is the presence of constant conflicts with family members. Conflict situations become reasons for relapse or even switching to harder drugs.
The only option for outpatient treatment is when a person has been using for 1-2 months and the dependence is mild.
Working with codependents and resocialization
Resocialization is a person’s path to a new social life. Without restoration of the social role, a breakdown may occur. Addicted addicts need constant communication, work for distraction and emotional return from friends, colleagues, and family members. This way a person will realize that he has something to live for and limit himself from drugs.
If this is not done, after a short period of time a breakdown may occur due to melancholy or depression. These are frequent cases, and they are dangerous because after the next breakdown it becomes increasingly difficult to achieve remission in addiction.
In order to minimize disruptions, they work with codependent people, that is, loved ones and family members. During such work, codependent people learn how to correctly shape their behavior and how to help the patient quit drug use forever.
Only close people have constant contact with the addict. They should play the role of psychologists with whom the patient can share his experiences without keeping anything to himself. This minimizes the risk of disruption and restores harmonious relationships between family members. Therefore, without working with codependents, rehabilitation is considered incomplete.
How to quit on your own
You really have to want it. If I quit, then immediately without such excuses: starting Monday, tomorrow, the last time, I’ll quit. In the case of drugs, the reservations do not apply. You need to be prepared for withdrawal, during which there will be a strong desire to use the drug, and without use, depression and even suicidal thoughts may appear.
It is necessary to limit contact with anyone who is an active drug addict, even if they are taking other substances or medications. Such people are a constant temptation to relapse. You cannot change one drug for another because you will end up dependent on two drugs.
It is necessary to monitor health indicators, liver and kidney function. Your attending physician will tell you about the regularity of liver tests and creatinine clearance. In any case, treating addiction on your own is difficult and dangerous. If possible, it is always better to consult with specialists in the field of addiction.
Phenazepam addiction
Dependence on Phenazepam occurs after just a couple of weeks of regular use. If the doctor prescribed this drug, then there are serious reasons for this. It must be taken strictly according to the instructions, following all the rules. Under no circumstances should you take pills for several courses in a row.
Alas, even if all the rules are followed, it cannot be guaranteed that a person will not develop an addiction. If you notice that without the pills you have become nervous, the usual dosage no longer helps, and you want to increase the dose - you should tell your doctor to change your medications.