Pharmacological properties of the drug Oxybutynin
It has a direct antispasmodic effect on the smooth muscles of the detrusor bladder, and also has an M-anticholinergic effect. In patients with neurogenic bladder dysfunction, oxybutynin increases bladder volume, reduces spontaneous contractions of the detrusor muscle and reduces the urge to urinate. The maximum concentration of oxybutynin in blood plasma is observed 45 minutes after oral administration. The concentration in blood plasma is proportional to the dose taken. The half-life is about 2 hours.
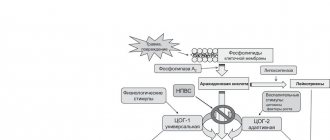
Evaluation of the effectiveness of the drug oxybutynin in children with overactive bladder
Up to 90% of urinary disorders occur due to the so-called. functional forms caused by dysfunction of the central nervous system and disturbances in the sensitivity of the receptor apparatus. In this case, there is a violation of bioenergetics and detrusor ischemia. The most common type of neurogenic bladder dysfunction (NDBD) in children is hyperreflex. It is with detrusor hyperreflexia that pronounced urodynamic disorders are observed, caused by intravesical hypertension and detrusor hypoxia, and, as a consequence, vesicoureteral reflux (VUR) and recurrent urinary tract infection occur [1,2,3,4]. Urodynamic disorders also form a characteristic clinical picture in hyperreflexive bladder in children - imperative urination syndrome, pollakiuria, urgency, imperative urinary incontinence in combination with enuresis. In recent years, the International Continence Society (ICS) has coined a new term for urinary urgency: overactive bladder (OAB). Urodynamic definition of OAB: hyperactive detrusor, which means involuntary contractions of the detrusor - an increase in detrusor pressure during cystometry of more than 5 cm of water. Art. [5]. Successful treatment of OAB helps not only to eliminate the symptoms of urgent urination (i.e., improves the quality of life of patients), but also to stop the recurrence of urinary tract infections in 70–80% of cases of VUR. Treatment of OAB in children includes behavioral therapy, medication, biofeedback, and physical therapy. Among medications, anticholinergic drugs are the first line of treatment. Atropine itself is practically not used in modern neurourology due to side effects on the smooth muscles of almost all organs and systems. Currently, oxybutynin, tolderodine and trospium chloride are the most widely used [6,7,8,9,10,11]. The main mechanism of their action is the interruption of efferent nerve impulses to the bladder at the level of postganglionic parasympathetic receptors. Multicenter studies in adult patients have shown their comparable clinical effectiveness, but with long courses of treatment (6–12 months), tolderodine and trospium chloride have a lower incidence of side effects. As studies in recent years have shown, it is possible to solve the problem of side effects of oxybutynin by using starting doses (not 5, but 2.5 mg) with subsequent titration if necessary, while maintaining high effectiveness of treatment [12]. There are very few publications on the use of tolderodine and trospium chloride in the treatment of LUTD in children, both in domestic and foreign literature. The “gold standard” in pediatric neurourology for the treatment of OAB currently remains the drug oxybutynin (Driptan). Oxybutynin is a drug with a mixed mechanism of action: in addition to anticholinergic activity, it has antispasmodic and local anesthetic effects. In OAB, the disturbance of bioenergetics and hypoxia of the detrusor against the background of intravesical hypertension is of no small importance, which reduces the sensitivity of M-cholinergic receptors and explains the effects of atropine resistance and even paradoxical effects in response to the prescription of atropinization in children with an overactive detrusor. Previously, pharmacocystometry with atropine was used to predict the “behavior” of the bladder in response to blockade of M-cholinergic receptors. Based on the pharmacokinetics of oxybutynin (Cmax is reached after 45 minutes), it seems appropriate to predict the effectiveness of treatment with M-anticholinergics based on the results of a non-invasive study - pharmacouroflowmetry with oxybutynin. Our own 3-year experience has proven the equivalence of the diagnostic significance of pharmacouroflowmetry with oxybutynin and pharmacocystometry with atropine. In case of severe intravesical hypertension, to increase the sensitivity of M-cholinergic receptors to anticholinergic drugs, metabolic and antihypoxic therapy is indicated before the appointment of M-cholinergic drugs [13] or, in the future, combined treatment with M-cholinergic drugs and α1-blockers [14,15]. Therefore, pharmacouroflowmetry with oxybutynin, performed over time in such cases, will serve as a criterion for the “readiness” of the detrusor for treatment with mediator agents. Thus, correct selection of patients makes it possible to increase the effectiveness of treatment with M-anticholinergic blockers, including oxybutynin. The purpose of this work was to study the effectiveness of the drug oxybutynin in children with LUTD of the hyperreflex type. Materials and methods Under our supervision at the nephrology department of the Izmailovsky Children's City Clinical Hospital there were 56 children aged 5 to 15 years with hyperreflex NDMP (45 girls and 11 boys). The average age of the children was 9 years. All children underwent a standard nephrological examination, incl. X-ray. The urological examination included a clinical assessment of bladder function using a urinary urgency assessment table, registration of urination rhythm, and determination of residual urine by ultrasound. The table for assessing imperative urination syndrome in children included the degree of severity in points of imperative urge to urinate, imperative urinary incontinence, enuresis, pollakiuria, nocturia, a decrease in the average effective volume of the bladder, the presence and severity of leukocyturia [16]. The total score of the table varies from 0 to 45. In this range, there are three degrees of severity of imperative urination syndrome: mild (1–10 points), moderate (11–20 points) and severe (more than 21 points). The study of the functional state of the lower urinary tract was carried out using the domestic urodynamic system SURD-01 “Relief-M” (uroflowmetry (UF), cystometry, urethral profilometry). All urodynamic studies were performed in the absence of an active inflammatory process in the urinary system. In 39 (70%) children, the course of NDMP was complicated by pyelonephritis, the average duration of which was 4.1 years. At the same time, in only two children the clinical picture of urinary tract urinary tract debuted simultaneously with the onset of pyelonephritis and persisted after achieving sanitation of the urinary tract. In the remaining children, manifestations of NDMP were noted from an early age. In 8 (14%) children, grade II–III VUR was diagnosed, various anomalies of the kidney structure were detected in 38 (68%), metabolic disorders (oxaluria, uraturia) - in 17 (30%) children. In addition, every third child had combined pelvic organ disorders. In addition to NDMP, 16 (29%) children had functional constipation (of which 3 were complicated by encopresis), and 2 (4%) had encopresis with regular bowel movements. When analyzing the symptoms of urinary disorders using the table for assessing bladder function, we found that the average score was 16.8. At the same time, 13 patients had moderate urodynamic disturbances, 30 had moderate disturbances, and 13 patients had severe disturbances. The following symptoms were noted: pollakiuria in 18 (32%), urgency in 10 (18%), enuresis in 41 (73%), urge urinary incontinence in 34 (61%). Combined urinary disorders, when there was daytime and nighttime urinary incontinence, were noted by us in 25 (45%) patients. In order to predict the effectiveness of oxybutynin therapy, all children underwent pharmacouroflowmetry: 40 minutes before the study, the patient took 5 mg of oxybutynin, after which urination was recorded (from 2 to 5 voids). The test was considered positive when the effective capacity of the bladder increased and the volumetric flow rate of urination normalized (CC coefficient); with rapid urination - with a decrease in the maximum and/or average speed of urination (Fig. 1, 2). The main course of treatment included oxybutynin (Driptan) at a dose of 2.5–5 mg 2–3 times a day, as well as picamilon, B vitamins, and lemontar. The general course of treatment was 4 weeks. If the response to oxybutynin was positive during pharmacouroflowmetry, combination treatment was prescribed immediately (34 patients). Due to severe intravesical hypertension (specific intravesical pressure - SVP - during cystometry exceeded 20-30 cm water column) and the lack of a significant positive effect when using Driptan during uroflowmetry in 22 children, metabolic therapy in combination with thermal procedures on the bladder area preceded the prescription of oxybutynin. Pharmacouroflowmetry with oxybutynin was repeated 10–14 days from the start of metabolic therapy. An improvement in urodynamics compared to baseline results was noted and treatment with Driptan was started. Results were assessed after 10 days, 6 and 12 months. Results and discussion After treatment, all patients showed positive dynamics in the clinical picture: the average score for urinary disorders by the 10th day was 4.7, after 6 months - 4.4, after a year - 4.6. Thus, the reduction in symptoms persisted for a long time and averaged 12.2 points (p <0.01) (Fig. 3). First of all, we noted positive changes in relation to the symptoms of OAB during the day; enuresis was more resistant to therapy (Table 1). Thus, on the 10th day of treatment, pollakiuria stopped in 15 (83%), and after 6–12 months in 16 children, in the remaining two it became less pronounced. A normal urge to micturate was established by the 10th day of treatment in 8 out of 10 children (80%), and after 6 months, rare imperative urges persisted in only one patient. Daytime urinary incontinence disappeared on the 10th day of treatment with oxybutynin in 26 (76%), and during follow-up it was not observed in 30 (87%) patients. During treatment, bedwetting stopped in 22 (54%), in 17 (41%) the frequency of manifestations decreased by 2-3 times, and only in 2 (5%) children did enuresis persist every night. It should be noted that in 8 of 22 children, “dry nights” were observed from 3 weeks to 2 months, followed by resumption of enuresis, although its frequency decreased significantly (5–10 times) compared to the period before treatment with oxybutynin. During urodynamic examination, positive dynamics were noted in all patients. The average effective capacity of the bladder increased significantly (p<0.01) - by 45% after 10 days and by 71% after a year (Fig. 4) and the number of micturitions per day decreased - by 27% after 10 days and by 35% after year (Fig. 5). Before the start of therapy, 30 children had intravesical hypertension with fluctuations in air pressure from 14 to 104 cm H2O. (normally – 6–10 cm of water column). The average air pressure was 41 cm water column. After treatment with oxybutynin (after 6–12 months), in 10 children the tone of the bladder was normalized; in the rest, the average UVP decreased by 2 times (p<0.01) - to 19.7 cm water column. (Fig. 6). In addition, all children stopped recurrent urinary tract infections or their frequency significantly decreased. In 6 out of 8 (75%) VUR was relieved; in two children, reflux persisted, but its intensity decreased. There were no significant side effects during treatment with oxybutynin, so in no case did treatment have to be interrupted. Conclusion The drug oxybutynin (Driptan), having an anticholinergic and antispasmodic effect, is an effective treatment for overactive bladder in children. To achieve a better effect, in some cases it is advisable to combine the use of oxybutynin with metabolic therapy. In case of severe intravesical hypertension, this therapy should precede the administration of oxybutynin to increase the sensitivity of M-cholinergic receptors. In order to predict the effect of treatment and monitor treatment over time, it is advisable to conduct pharmacouroflowmetry with oxybutynin. To achieve stable relief of enuresis in children with OAB, repeated courses of treatment with oxybutynin are indicated at intervals of 2 months or the prescription of oxybutynin for 10 days a month for 3 months.
Literature
1. Pugachev A.G. Romikh V.V. Alferov S.N. Clinical features of functional urination disorders in childhood. Attending physician, No. 9, 2004, p. 32–35. 2. Bauer S., Koff SA, Jayanthi VR Voiding dysfunction children and non-neurogenic. Lun.: Walsh PS et al., ed. Campbell's Urology. 8thed. Philadelphia Penna: WB Saunders Co; 2002: 2231–2283. 3. Vega–PJM, Pascual LA High–pressure bladder: an underlying factor mediating renal damage in the absence of reflux? B.J.U. Iht, 2001, 4, 87(6), p 581–584. 4. Castro J., Soares E., Casimiro A., Nogueria G. Bladder malfunction, urinary infection and vesicoureteral reflux in children./ Acta Med Port 1998, 7, 11(7), p 635–642. 5. Abrams P., Cardozo L., Fall M. et all. The Standardization of Terminology of lower urinary tract function; Report from the Standardization Sub–committee of the International Continence Society. Neurology and Urodynamics. 2002; 21: 167–178. 6. E. B. Mazo, G. G. Krivoborodov. Drug treatment of overactive bladder. RMJ, 2004, vol. 12, no. 8, p. 134–142. 7. Pushkar D.Yu. Overactive bladder in women. – M: MEDpress-inform, 2003.–160 p. 8. Appell RA, Diokho A., Antoci J. et all. One-year, prospective, open-label trial of controlled-release oxybutinin for overactive bladder in a community-based population [abstract]. Neuruorol Urodyn. 2000; 19:526. 9. Vasilyeva Zh.B., Danilov V.V., Danilova T.I.. The effectiveness of the drug spasmex in children with neurogenic bladder dysfunction./ Urology (Vladivostok), 2004, No. 6, p. 17–21. 10. Scott A., MacDiarmid. Overactive bladder: Improving the efficacy of anticholinergics by dose escalation. Current Urology Reports. 2003; 4:446–451. 11. Pushkar D.Yu., Shchaveleva O.B. Spazmex in the treatment of patients with overactive bladder. Urology, No. 4, 2003, p. 46–49. 12. Bemelmans BLN, Kiemeney LALM, Debruyne FMJ Low-dose oxibutinin for the treatment of urge incontinence: Good efficacy and few side effects. Eur. Urol., 2000; 37:709–713. 13. Danilov V.V., Danilova T.I. Atropine test. Methodology, assessment and prognosis of the use of M-anticholinergics in children with neurogenic bladder dysfunction of the hyperreflex type. Vladivostok, 1999, 19 p. 14. Athanascopoulos A., Gyfopoulos K., Giannitsas et al. Combination treatment with an blocker plus an anticholinergic for bladder outlet obstruction: a prospective, randomized, controlled study. J. Urol. 2003; 169:2253–2256. 15. Caine MP, Wu SD, Austin PF, Herdon CDA and Rink RC Alpha blocker therapy for children with dysfunction voiding and urinary retention./ J. Urol. At 2003, Vol 170, p 1514–1517. 16. Vishnevsky E.L., Laurent O.B., Vishnevsky A.E. Clinical assessment of urinary disorders. M., Tera, 2001, pp. 48–56.
Special instructions for the use of the drug Oxybutynin
It should be used with caution in weakened elderly patients and in patients with neurocirculatory dystonia, severe liver and kidney diseases. With the use of oxybutynin, it is sometimes possible to increase the severity of symptoms of hyperthyroidism, ischemic heart disease, congestive heart failure, arrhythmias, tachycardia and prostatic hypertrophy. As with any anticholinergic drug, caution should be exercised when prescribing oxybutynin to patients with a hiatal hernia accompanied by reflux esophagitis. The safety of using oxybutynin during pregnancy has not been established. Should not be prescribed during breastfeeding. The use of oxybutynin may be accompanied by drowsiness and decreased visual acuity, which must be taken into account when driving vehicles and working with potentially dangerous mechanisms.
Oxybutynin
International name of the medicinal substance:
Oxybutynin The list of drugs containing the active substance Oxybutynin is given after the description.
Pharmacological action:
Antispasmodic, eliminates spasms and reduces the tone of smooth muscles: gastrointestinal tract, biliary tract, uterus, relaxes the detrusor (direct spasmomyolytic and m-anticholinergic action).
Increases bladder capacity, reduces the frequency of detrusor contractions, and inhibits the urge to urinate. Well tolerated with long-term use. Pharmacokinetics:
TCmax after oral administration - 45 minutes. The concentration is proportional to the dose applied. T1/2 - 2 hours, in elderly patients - longer.
Indications:
Neurogenic bladder (including detrusor hyperreflexia in multiple sclerosis or spina bifida);
urinary incontinence (idiopathic nature); nocturnal enuresis (in children over 5 years old). Contraindications:
Hypersensitivity, open- and closed-angle glaucoma, gastrointestinal obstruction, paralytic intestinal obstruction, intestinal atony, dilation of the colon (including toxic, complicated by ulcerative colitis), ulcerative colitis, myasthenia gravis, obstructive uropathy, bleeding, childhood (up to 5 years), pregnancy, lactation period. With caution.
Renal/liver failure, thyrotoxicosis, ischemic heart disease, heart failure, arrhythmias, arterial hypertension, prostatic hyperplasia, hiatal hernia, diarrhea accompanying incomplete intestinal obstruction (especially in patients with ileo- or colostomy), old age. Side effects:
Dyspepsia (nausea, vomiting, constipation, flatulence), dry mouth, urinary disorders (including urinary retention), decreased gastric and intestinal motility, drowsiness or insomnia, weakness, dizziness, anxiety, hallucinations, tachycardia, decreased production of tear fluid, visual impairment (mydriasis, paralysis of accommodation, amblyopia), increased intraocular pressure, decreased sweating, decreased potency, allergic reactions. Overdose.
Symptoms: central nervous system excitement (anxiety, tremor, irritability, convulsions, delirium, hallucinations), fever, nausea, vomiting, tachycardia, decreased or increased blood pressure, respiratory failure, paralysis, coma. Treatment: gastric lavage, prescribe activated charcoal and saline laxative drugs, breathing should be maintained; To reduce the severity of symptoms of anticholinergic intoxication, anticholinesterase drugs (physostigmine) are used. For hyperpyrexia - cold compresses (including ice), alcohol rubdowns. Interaction:
Increased side effects are observed when combined with drugs that have an anticholinergic effect.
Ethanol and sedatives increase dizziness and drowsiness. Special instructions:
It must be borne in mind that high ambient temperatures more often provoke the occurrence of fever (decreased sweating) while taking the drug.
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions. Preparations containing the active ingredient Oxybutynin:
Driptan, Novitropan, Oxybutin, Cistrin
The information provided in this section is intended for medical and pharmaceutical professionals and should not be used for self-medication. The information is provided for informational purposes only and cannot be considered official.
Overdose of the drug Oxybutynin, symptoms and treatment
Symptoms of overdose vary from increased severity of common side effects to disorders of the central nervous system (anxiety, psychomotor agitation, rarely psychosis) and the cardiovascular system (autonomic reactions, decreased blood pressure), in exceptional cases - to respiratory failure, paralysis and coma. Treatment: gastric lavage, slow intravenous administration of 1–2 mg of physostigmine (if necessary, repeated, up to 5 mg). With the development of hyperthermia, symptomatic treatment (cool wraps, local hypothermia). In cases of severe agitation, 10 mg of diazepam is administered intravenously; in case of tachycardia, propranolol is administered intravenously. If urinary retention occurs, bladder catheterization is performed. In case of development of a curare-like effect and paralysis of the respiratory muscles, use mechanical ventilation.
List of pharmacies where you can buy Oxybutynin:
- Moscow
- Saint Petersburg