Ibuprofen Medisorb capsules 200 mg No. 10 contour. cells pack
Side effects
The frequency of side effects was assessed as follows: very often (>1/10); often(>1/100.1/1000.1/10000,<1/1000); very rare (<1/10000), frequency unknown (the incidence of side effects cannot be estimated based on available data). Infectious and parasitic diseases: very rarely - worsening inflammation due to infection (for example, the development of necrotizing fasciitis), symptoms of aseptic meningitis with stiff neck, headache, nausea, vomiting, fever or confusion, especially in patients with autoimmune diseases (SLE, systemic connective tissue diseases).
Disorders of the blood and lymphatic system: very rarely - disorders of hematopoiesis (anemia, leukopenia, thrombocytopenia, pancytopenia, agranulocytosis).
Immune system disorders: uncommon - hypersensitivity reactions: nonspecific allergic reactions and anaphylactic reactions, reactions from the respiratory tract (bronchial asthma, including its exacerbation, bronchospasm, shortness of breath, dyspnea), skin reactions (itching, urticaria, purpura, edema Quincke, exfoliative and bullous dermatoses, including toxic epidermal necrolysis (Lyell's syndrome), Stevens-Johnson syndrome, erythema multiforme), allergic rhinitis, eosinophilia; very rarely - severe hypersensitivity reactions, manifested as swelling of the face, tongue and larynx, shortness of breath, tachycardia, arterial hypotension (anaphylaxis, Quincke's edema or severe anaphylactic shock).
Mental disorders: infrequently – psychomotor agitation, irritability, very rarely – neurosis, depression.
Nervous system disorders: uncommon – headache, dizziness, insomnia. Visual disturbances: infrequently - visual disturbances.
Hearing and labyrinthine disorders: rarely – “tinnitus”.
Cardiac disorders: very rarely - tachycardia, heart failure, myocardial infarction. Vascular disorders: arterial hypertension.
Gastrointestinal disorders: often - heartburn, abdominal pain, nausea, vomiting, flatulence, diarrhea, constipation, minor gastrointestinal bleeding, which can lead to the development of anemia; uncommon – peptic ulcer with possible complications (bleeding, perforation), ulcerative stomatitis, exacerbation of colitis and Crohn’s disease, gastritis; very rarely - esophagitis, pancreatitis, development of intestinal membrane strictures.
Disorders of the liver and biliary tract: very rarely - liver dysfunction, hepatotoxicity (especially with long-term use), liver failure, acute hepatitis.
Renal and urinary tract disorders: very rarely - development of edema, especially in patients with arterial hypertension or renal failure, nephrotic syndrome, interstitial nephritis, which may be accompanied by acute renal failure, damage to renal tissue (papillary necrosis).
Laboratory and instrumental data: infrequently – decrease in hemoglobin and hematocrit, increase in bleeding time, decrease in plasma glucose levels, decrease and increase in serum creatinine concentration, increase in the activity of “liver” transaminases, very rarely – increase in the level of uric acid in the blood. The risk of developing ulcerations of the gastrointestinal mucosa, bleeding (gastrointestinal, gingival, uterine, hemorrhoidal), visual impairment (impaired color vision, scotoma, amblyopia) increases with long-term use in large doses.
Ibuprofen Medisorb
The risk of side effects can be minimized if the drug is taken in a short course, at the minimum effective dose required to eliminate symptoms.
Side effects are predominantly dose-dependent.
The following adverse reactions were observed with short-term use of ibuprofen in doses not exceeding 1200 mg/day (6 capsules). When treating chronic conditions and with long-term use, other adverse reactions may occur.
The incidence of adverse reactions was assessed based on the following criteria: very often (≥1/10), often (from ≥1/100 to <1/10), infrequently (from ≥1/1000 to <1/100), rarely ( from ≥1/10000 to <1/1000), very rare (<1/10000), frequency unknown (the incidence of side effects cannot be estimated based on available data).
Disorders of the blood and lymphatic system: very rarely - disorder of hematopoiesis (anemia, leukopenia, aplastic anemia, hemolytic anemia, thrombocytopenia, pancytopenia, agranulocytosis). The first symptoms of such disorders are fever, sore throat, superficial oral ulcers, flu-like symptoms, severe weakness, nosebleeds and subcutaneous hemorrhages, bleeding and bruising of unknown etiology.
Immune system disorders: infrequently - hypersensitivity reactions - nonspecific allergic reactions and anaphylactic reactions, reactions from the respiratory tract (bronchial asthma, including its exacerbation, bronchospasm, shortness of breath, dyspnea), skin reactions (itching, urticaria, purpura , Quincke's edema, exfoliative and bullous dermatoses, including toxic epidermal necrolysis (Lyell's syndrome), Stevens-Johnson syndrome, erythema multiforme), allergic rhinitis, eosinophilia; very rarely - severe hypersensitivity reactions, incl. swelling of the face, tongue and larynx, shortness of breath, arterial hypotension (anaphylaxis, Quincke's edema or severe anaphylactic shock).
Nervous system disorders: infrequently - headache; very rarely - aseptic meningitis.
Cardiac disorders: frequency unknown - heart failure, with long-term use there is an increased risk of thrombotic complications (for example, myocardial infarction).
Vascular disorders: frequency unknown - peripheral edema, increased blood pressure.
Disorders of the respiratory system, chest and mediastinal organs: frequency unknown - bronchial asthma, bronchospasm, shortness of breath.
Gastrointestinal disorders: uncommon - abdominal pain, nausea, dyspepsia (including heartburn, bloating); rarely - diarrhea, flatulence, constipation, vomiting; very rarely - peptic ulcer, perforation or gastrointestinal bleeding, melena, hematemesis, in some cases fatal, especially in elderly patients, ulcerative stomatitis, gastritis; frequency unknown - exacerbation of colitis and Crohn's disease.
Disorders of the liver and biliary tract: very rarely - liver dysfunction (especially with long-term use), hepatitis and jaundice.
Disorders of the kidneys and urinary tract: very rarely - acute renal failure (compensated and decompensated), especially with long-term use, in combination with an increase in the concentration of urea in the blood plasma and the appearance of edema, hematuria and proteinuria, nephritic syndrome, nephrotic syndrome, papillary necrosis, interstitial nephritis, cystitis.
General disorders and reactions at the injection site: very rarely - swelling, incl. peripheral.
Laboratory and instrumental data: infrequently - decrease in hemoglobin and hematocrit, increase in bleeding time, decrease in plasma glucose levels, decrease in creatinine clearance, increase in plasma creatinine concentration, increase in the activity of “liver” transaminases.
It is important to report suspected adverse reactions to ensure ongoing monitoring of the benefit-risk relationship of the drug. If you experience any adverse reactions, contact your doctor, pharmacist, or manufacturer.
Healthcare professionals are encouraged to report any suspected adverse drug reactions through national adverse reaction reporting systems.
Ibuprofen Medisorb capsules 200 mg No. 10
Compound
One capsule contains: active ingredient: ibuprofen – 200 mg;
excipients: croscarmellose sodium; talc; magnesium stearate; Aerosil (colloidal silicon dioxide) composition of hard gelatin capsules No. 1: gelatin, titanium dioxide, yellow iron oxide, indigo carmine.
Description
Hard gelatin capsules No. 1 are white with green caps, containing white or white powder with a yellowish tint.
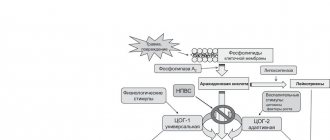
Pharmacodynamics
The mechanism of action of ibuprofen, a derivative of propionic acid from the group of non-steroidal anti-inflammatory drugs (NSAIDs), is due to inhibition of the synthesis of prostaglandins - mediators of pain, inflammation and hyperthermic reaction. Indiscriminately blocks cyclooxygenase I (COX-1) and cyclooxygenase II (COX-2), as a result of which it inhibits the synthesis of prostaglandins. It has a rapid, targeted effect against pain (analgesic), anti-inflammatory and antipyretic effect. In addition, ibuprofen reversibly inhibits platelet aggregation.
Pharmacokinetics
Quickly and almost completely absorbed from the gastrointestinal tract (GIT). Taking the drug with food may increase the time to reach maximum concentration (TCmax). After taking 2 capsules of the drug on an empty stomach, ibuprofen is detected in the blood plasma after 10 minutes, the maximum concentration (Cmax) of ibuprofen in the blood plasma is reached after 30-40 minutes. Communication with blood plasma proteins is more than 90%. Slowly penetrates into the joint cavity, lingers in the synovial fluid, creating higher concentrations in it than in the blood plasma. Metabolized in the liver. After absorption, approximately 60% of the pharmacologically inactive R form of ibuprofen is slowly transformed into the active S form. The half-life (T1/2) of ibuprofen is 2 hours. It is excreted by the kidneys (no more than 1% unchanged) and, to a lesser extent, with bile. In elderly patients, there were no significant differences in the pharmacokinetic profile of the drug compared to younger patients. In limited studies, ibuprofen has been found in breast milk at very low concentrations.
Indications
Headache, toothache, migraine, painful menstruation, neuralgia, back pain, joint pain, muscle and rheumatic pain, fever with flu and colds.
Contraindications
- hypersensitivity to ibuprofen or any of the components included in the drug;
- complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid (ASA) or other NSAIDs (including a history);
- erosive and ulcerative diseases of the gastrointestinal tract (including gastric and duodenal ulcers, Crohn's disease, ulcerative colitis) or ulcerative bleeding in the active phase or in history (two or more confirmed episodes of peptic ulcer or ulcerative bleeding);
- a history of bleeding or perforation of a gastrointestinal ulcer caused by the use of NSAIDs;
- severe heart failure (class IV according to the New York Heart Association (NYHA) classification);
- severe liver failure or active liver disease;
- severe renal failure (creatinine clearance <30 ml/min), confirmed hyperkalemia;
- decompensated heart failure, the period after coronary artery bypass grafting;
- cerebrovascular or other bleeding;
- hemophilia and other bleeding disorders (including hypocoagulation), hemorrhagic diathesis;
- pregnancy (III trimester);
- children's age up to 12 years.
With caution: if you have the conditions listed in this section, you should consult your doctor before using the drug.
Concomitant use of other NSAIDs, a history of a single episode of gastric and duodenal ulcers or gastrointestinal ulcerative bleeding; gastritis, enteritis, colitis, the presence of Helicobacter pylori infection, ulcerative colitis; bronchial asthma or allergic diseases in the acute stage or in history - bronchospasm may develop; systemic lupus erythematosus or mixed connective tissue disease (Sharpe's syndrome) - increased risk of aseptic meningitis; chicken pox; renal failure, including dehydration (creatinine clearance less than 30-60 ml/min), nephrotic syndrome, liver failure, liver cirrhosis with portal hypertension, hyperbilirubinemia, arterial hypertension and/or heart failure, cerebrovascular diseases, blood diseases of unknown etiology ( leukopenia and anemia), severe somatic diseases, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial disease, smoking, frequent alcohol consumption, concomitant use of medications that may increase the risk of ulcers or bleeding, in particular oral glucocorticosteroids (including prednisone ), anticoagulants (including warfarin), selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline) or antiplatelet agents (including ASA, clopidogrel), pregnancy I-II trimester, breastfeeding period, old age . Use during pregnancy and breastfeeding
The use of the drug is contraindicated in the third trimester of pregnancy. You should avoid using the drug in the first and second trimesters of pregnancy; if you need to take the drug, you should consult your doctor. There is evidence that ibuprofen can pass into breast milk in small quantities without any adverse effects on the health of the nursing infant, so there is usually no need to stop breastfeeding when taken for a short period of time. If long-term use of the drug is necessary, you should consult a doctor to decide whether to stop breastfeeding for the period of use of the drug.
Directions for use and doses
For oral administration. For short term use only.
Adults and children over 12 years old: 1 capsule (200 mg), without chewing, 3-4 times a day. The capsule should be taken with water. The interval between taking tablets should be 6-8 hours. To achieve a faster therapeutic effect in adults, the single dose can be increased to 2 capsules (400 mg) up to 3 times a day.
The maximum daily dose is 1200 mg. The maximum daily dose for children 12-17 years old is 1000 mg.
If symptoms persist or worsen, consult your doctor.
Side effect
The risk of side effects can be minimized if the drug is taken in a short course, at the minimum effective dose required to eliminate symptoms. Elderly people experience an increased incidence of adverse reactions with NSAID use, especially gastrointestinal bleeding and perforation, in some cases fatal. Side effects are predominantly dose-dependent. The following adverse reactions were observed with short-term use of ibuprofen in doses not exceeding 1200 mg/day (6 tablets). When treating chronic conditions and with long-term use, other adverse reactions may occur. The frequency of adverse reactions listed below is given in accordance with the following classification: very common (≥ 10%), common (≥ 1% but < 10%), uncommon (≥ 0.1% but < 1%), rare ( ≥ 0.01% but < 0.1%), very rare (< 0.01%), frequency unknown - frequency cannot be estimated from available data.
- Disorders of the blood and lymphatic system: very rare - hematopoietic disorders (anemia, leukopenia, aplastic anemia, hemolytic anemia, thrombocytopenia, pancytopenia, agranulocytosis). The first symptoms of such disorders are fever, sore throat, superficial oral ulcers, flu-like symptoms, severe weakness, nosebleeds and subcutaneous hemorrhages, bleeding and bruising of unknown etiology.
- Immune system disorders: infrequent - hypersensitivity reactions - nonspecific allergic reactions and anaphylactic reactions, reactions from the respiratory tract (bronchial asthma, including its exacerbation, bronchospasm, shortness of breath, dyspnea), skin reactions (itching, urticaria, purpura, edema Quincke, exfoliative and bullous dermatoses, including toxic epidermal necrolysis (Lyell's syndrome), Stevens-Johnson syndrome, erythema multiforme), allergic rhinitis, eosinophilia. Very rare: severe hypersensitivity reactions, including swelling of the face, tongue and larynx, shortness of breath, tachycardia, hypotension (anaphylaxis, angioedema or severe anaphylactic shock).
- Gastrointestinal disorders: uncommon - abdominal pain, nausea, dyspepsia (including heartburn, bloating). Rare: diarrhea, flatulence, constipation, vomiting. Very rare: peptic ulcer, perforation or gastrointestinal bleeding, melena, hematemesis, in some cases fatal, especially in elderly patients, ulcerative stomatitis, gastritis. Frequency unknown: exacerbation of colitis and Crohn's disease.
- Disorders of the liver and biliary tract: very rare - liver dysfunction (especially with long-term use), increased activity of liver transaminases, hepatitis and jaundice.
- Renal and urinary tract disorders: very rare - acute renal failure (compensated and decompensated), especially with long-term use, in combination with an increase in the concentration of urea in the blood plasma and the appearance of edema, hematuria and proteinuria, nephritic syndrome, nephrotic syndrome, papillary necrosis, interstitial nephritis, cystitis.
- Nervous system disorders: uncommon - headache. Very rare: aseptic meningitis.
- Disorders of the cardiovascular system: frequency unknown - heart failure, peripheral edema, with long-term use there is an increased risk of thrombotic complications (for example, myocardial infarction), increased blood pressure.
- Disorders of the respiratory system and mediastinal organs: frequency unknown - bronchial asthma, bronchospasm, shortness of breath.
- Laboratory parameters: - hematocrit or hemoglobin (may decrease); - bleeding time (may increase); - plasma glucose concentration (may decrease); - creatinine clearance (may decrease); - plasma concentration of creatinine (may increase); - activity of “liver” transaminases (may increase).
If any of the side effects indicated in the instructions get worse, or you notice any other side effects not listed in the instructions, tell your doctor.
Overdose
Do not exceed the indicated dose. If you have exceeded the dose, consult your doctor or the nearest medical facility immediately. Take the drug package with you. Symptoms: abdominal pain, nausea, vomiting, lethargy, drowsiness, depression, headache, tinnitus, metabolic acidosis, coma, acute renal failure, decreased blood pressure, bradycardia, tachycardia, atrial fibrillation, respiratory arrest. Treatment: gastric lavage (only within an hour after administration), activated charcoal, alkaline drinking, forced diuresis, symptomatic therapy (correction of acid-base status, blood pressure).
Drug interactions
The simultaneous use of ibuprofen with the following drugs should be avoided:
- Acetylsalicylic acid: with the exception of low doses of acetylsalicylic acid (no more than 75 mg per day) prescribed by a doctor, since combined use may increase the risk of side effects. With simultaneous use, ibuprofen reduces the anti-inflammatory and antiplatelet effect of acetylsalicylic acid (an increase in the incidence of acute coronary insufficiency in patients receiving small doses of acetylsalicylic acid as an antiplatelet agent is possible after starting ibuprofen).
- Other NSAIDs, in particular selective COX-2 inhibitors: the simultaneous use of two or more drugs from the NSAID group should be avoided due to a possible increased risk of side effects.
Use with caution simultaneously with the following medications:
- Anticoagulants and thrombolytic drugs: NSAIDs may enhance the effect of anticoagulants, in particular warfarin and thrombolytic drugs.
- Antihypertensives (angiotensin-converting enzyme (ACE) inhibitors and angiotensin II antagonists) and diuretics: NSAIDs may reduce the effectiveness of drugs in these groups. In some patients with impaired renal function (eg, dehydrated patients or elderly patients with impaired renal function), coadministration of ACE inhibitors or angiotensin II antagonists and cyclooxygenase inhibitors may lead to a deterioration of renal function, including the development of acute renal failure. (usually reversible). These interactions should be considered in patients taking coxibs concomitantly with ACE inhibitors or angiotensin II antagonists. In this regard, the combined use of the above drugs should be prescribed with caution, especially in elderly patients. Patients should be prevented from dehydration and consideration should be given to monitoring renal function upon initiation of this combination treatment and periodically thereafter. Diuretics and ACE inhibitors may increase the nephrotoxicity of NSAIDs.
- Glucocorticosteroids: increased risk of gastrointestinal ulceration and gastrointestinal bleeding.
- Antiplatelet agents and selective serotonin reuptake inhibitors: increased risk of gastrointestinal bleeding.
- Cardiac glycosides: simultaneous administration of NSAIDs and cardiac glycosides can lead to worsening heart failure, a decrease in glomerular filtration rate and an increase in the concentration of cardiac glycosides in the blood plasma.
- Lithium preparations: there is evidence of the likelihood of an increase in the concentration of lithium in the blood plasma during the use of NSAIDs.
- Methotrexate: there is evidence of the likelihood of an increase in the concentration of methotrexate in the blood plasma during the use of NSAIDs.
- Cyclosporine: increased risk of nephrotoxicity when NSAIDs are administered concomitantly with cyclosporine.
- Mifepristone: NSAIDs should be started no earlier than 8 to 12 days after taking mifepristone, as NSAIDs may reduce the effectiveness of mifepristone.
- Tacrolimus: Concomitant administration of NTTVP and tacrolimus may increase the risk of nephrotoxicity.
- Zidovudine: Concomitant use of NSAIDs and zidovudine may result in increased hematotoxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive patients with hemophilia who received concomitant treatment with zidovudine and ibuprofen.
- Quinolone antibiotics: In patients receiving concomitant treatment with NSAIDs and quinolone antibiotics, the risk of seizures may be increased.
- Myelotoxic drugs: increased hematotoxicity.
- Cefamandole, cefoperazone, cefotetan, valproic acid, plicamycin: increased incidence of hypoprothrombinemia.
- Drugs that block tubular secretion: decreased excretion and increased plasma concentrations of ibuprofen.
- Inducers of microsomal oxidation (phenytoin, ethanol, barbiturates, rifampicin, phenylbutazone, tricyclic antidepressants): increased production of hydroxylated active metabolites, increased risk of developing severe intoxications.
- Microsomal oxidation inhibitors: reducing the risk of hepatotoxicity.
- Oral hypoglycemic drugs and insulin, sulfonylurea derivatives: increased effect of drugs.
- Antacids and cholestyramine: decreased absorption.
- Uricosuric drugs: decreased effectiveness of drugs.
- Estrogens, ethanol: increased risk of side effects.
- Caffeine: increased analgesic effect.
special instructions
It is recommended to take the drug for the shortest possible course and in the minimum effective dose necessary to eliminate symptoms. If you need to take the drug for more than 10 days, you should consult a doctor. In patients with bronchial asthma or an allergic disease in the acute stage, as well as in patients with a history of bronchial asthma/allergic disease, the drug may provoke bronchospasm. Use of the drug in patients with systemic lupus erythematosus or mixed connective tissue disease is associated with an increased risk of developing aseptic meningitis. During long-term treatment, monitoring of the peripheral blood picture and the functional state of the liver and kidneys is necessary. When symptoms of gastropathy appear, careful monitoring is indicated, including esophagogastroduodenoscopy, a complete blood count (hemoglobin determination), and a stool test for occult blood. If it is necessary to determine 17-ketosteroids, the drug should be discontinued 48 hours before the study. During the treatment period, ethanol intake is not recommended. Patients with renal failure should consult a doctor before using the drug, as there is a risk of deterioration in the functional state of the kidneys. Patients with hypertension, including a history of hypertension and/or chronic heart failure, should consult a physician before using the drug, as the drug may cause fluid retention, increased blood pressure and edema. In patients with uncontrolled hypertension, NYHA class II-III congestive heart failure, coronary artery disease, peripheral arterial disease and/or cerebrovascular disease, ibuprofen should be prescribed only after a careful benefit-risk assessment, and high doses of ibuprofen (≥2400) should be avoided mg/day). The use of NSAIDs in patients with chickenpox may be associated with an increased risk of developing severe purulent complications of infectious and inflammatory diseases of the skin and subcutaneous fat (for example, necrotizing fasciitis). In this regard, it is recommended to avoid using the drug for chickenpox. Information for women planning pregnancy: ibuprofen suppresses cyclooxygenase and prostaglandin synthesis, affects ovulation, disrupting female reproductive function (reversible after discontinuation of treatment).
Impact on the ability to drive vehicles and machinery
Patients who experience dizziness, drowsiness, lethargy, or blurred vision while taking ibuprofen should avoid driving or operating machinery.
Release form
Capsules 200 mg. There are 10 capsules in a package.
Storage conditions
Store in a place protected from light, at a temperature not exceeding 25°C. Keep out of the reach of children.
Best before date
3 years. Do not use after the expiration date stated on the package.
Vacation conditions
Over the counter.