Next Uno Express caps 200 mg N20 (OTISI)
Inducers of microsomal oxidation (phenytoin, ethanol, barbiturates, rifampicin, phenylbutazone, tricyclic antidepressants) increase the production of hydroxylated active metabolites of ibuprofen, increasing the risk of severe hepatotoxic reactions. Microsomal oxidation inhibitors reduce the risk of hepatotoxicity from ibuprofen. Ibuprofen reduces the antihypertensive effect of antihypertensive drugs (ACE inhibitors, slow calcium channel blockers, etc.), the natriuretic and diuretic effectiveness of furosemide and hydrochlorothiazide; reduces the effectiveness of uricosuric drugs, enhances the ulcerogenic effect of glucocorticosteroids, colchicine, ethanol; enhances the effect of oral hypoglycemic agents and insulin; increases the blood concentration of digoxin, lithium and methotrexate. Ibuprofen enhances the undesirable effects of estrogens when used together. Antacids and cholestyramine reduce the absorption of ibuprofen. Caffeine enhances the analgesic effect of ibuprofen. When administered simultaneously, ibuprofen reduces the anti-inflammatory and antiplatelet effect of acetylsalicylic acid (an increase in the incidence of acute coronary insufficiency in patients receiving small doses of acetylsalicylic acid as an antiplatelet agent is possible after starting ibuprofen). When prescribed with anticoagulant and thrombolytic drugs (alteplase, streptokinase, urokinase), the risk of bleeding simultaneously increases. With the combined use of ibuprofen and cefamandole, cefoperazone, cefotetan, valproic acid, the incidence of hypoprothrombinemia increases. Myelotoxic drugs increase the manifestations of hematotoxicity of the drug. Cyclosporine and gold preparations enhance the effect of ibuprofen on the synthesis of prostaglandins in the kidneys, which is manifested by increased nephrotoxicity. Ibuprofen increases the plasma concentration of cyclosporine and the likelihood of developing its hepatotoxic effects. Drugs that block tubular secretion reduce excretion and increase plasma concentrations of ibuprofen. Ibuprofen may reduce the effectiveness of mifepristone, so ibuprofen should be started no earlier than 8-12 days after taking mifepristone. Concomitant administration of ibuprofen and tacrolimus may increase the risk of nephrotoxicity. Concomitant use of ibuprofen and zidovudine may lead to increased hematological toxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive patients with hemophilia who received concomitant treatment with zidovudine and ibuprofen. In patients receiving concomitant treatment with ibuprofen and quinolone antibiotics, the risk of seizures may increase.
Next Uno Express
Trade name: Next Uno Express
International name: Ibuprofen&, (Ibuprofen)
Pharmacological group: NSAID (non-steroidal anti-inflammatory drug)
Pharmacological group for ATC: M01AE01. Ibuprofen
Compound:
1 capsule contains:
Active ingredient: ibuprofen - 200,000 mg.
Excipients: alpha-tocopherol acetate - 0.372 mg, povidone 17 PF - 30,000 mg, macrogol 600 - 414,628 mg.
The composition of the gelatin capsule shell: gelatin, sorbitol non-crystallizing solution, glycerol, methyl parahydroxybenzoate, purified water, charming red dye E-129.
Description:
Soft gelatin capsules, oval, with a seam, transparent, red.
The contents of the capsules are a colorless or pink-tinged transparent liquid.
Pharmacodynamics:
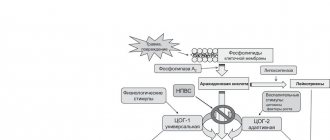
The mechanism of action of ibuprofen, a derivative of propionic acid from the group of non-steroidal anti-inflammatory drugs (NSAIDs), is due to inhibition of the synthesis of prostaglandins - mediators of pain, inflammation and hyperthermic reaction. Indiscriminately blocks cyclooxygenase 1 (COX-1) and cyclooxygenase 2 (COX-2), as a result of which it inhibits the synthesis of prostaglandins. It has a rapid, targeted effect against pain (analgesic), antipyretic and anti-inflammatory effects. Ibuprofen inversely inhibits platelet aggregation.
Pharmacokinetics:
Ibuprofen is absorbed from the digestive tract by approximately 80%. Absorption is slightly reduced when taking the drug after meals. Time to reach maximum concentration (TCmax) when taken on an empty stomach - 45 minutes, when taken after meals - 1.5-2 hours, in synovial fluid - 2-3 hours.
Ibuprofen is 90% bound to blood proteins, mainly albumin.
Subject to presystemic and postsystemic metabolism in the liver. After absorption, approximately 60% of the pharmacologically inactive R form of ibuprofen is slowly transformed into the active S form. The CYP2C9 isoenzyme takes part in the metabolism of the drug. It has two-phase elimination kinetics with a half-life (T1/2) of 2-2.5 hours. It is excreted by the kidneys (no more than 1% unchanged) and, to a lesser extent, with bile.
Indications for use:
Used for headaches, migraines, toothaches, painful menstruation, neuralgia, back pain, muscle and rheumatic pain, feverish conditions such as influenza and colds.
Intended for symptomatic therapy, reducing pain and inflammation at the time of use, does not affect the progression of the disease.
Contraindications:
- hypersensitivity to ibuprofen and other components of the drug,
- erosive and ulcerative diseases of the gastrointestinal tract (including peptic ulcer of the stomach and duodenum in the acute stage, ulcerative colitis, peptic ulcer, Crohn's disease),
- complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other NSAIDs (including a history),
- blood clotting disorders (including hemophilia, prolongation of bleeding time, bleeding tendency, hemorrhagic diathesis),
- children under 12 years of age,
- pregnancy III trimester, breastfeeding period,
- active gastrointestinal bleeding,
- intracranial hemorrhage,
- a history of bleeding or perforation of a gastrointestinal ulcer caused by the use of NSAIDs,
- severe heart failure,
- severe renal failure (creatinine clearance less than 30 ml/min),
- progressive kidney diseases,
- severe liver failure or active liver disease,
— condition after coronary artery bypass surgery,
- confirmed hyperkalemia,
- fructose intolerance.
Carefully:
The drug is used with caution in liver cirrhosis with portal hypertension, hyperbilirubinemia, gastric ulcer and duodenal ulcer (history), gastritis, enteritis, colitis, hepatic porphyria, liver and/or renal failure, nephrotic syndrome, chronic heart failure, arterial hypertension, blood coagulation disorders, blood diseases of unknown etiology (leukopenia and anemia), old age, pregnancy (I-II trimester), ischemic heart disease, cerebrovascular diseases, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial diseases, smoking, chronic renal failure (CK 30-60 ml/min), the presence of Helicobacter pylory infection, long-term use of NSAIDs, frequent alcohol consumption, severe somatic diseases, systemic lupus erythematosus or other autoimmune connective tissue diseases (increased risk of developing aseptic meningitis), simultaneous use of oral corticosteroids (including including prednisolone), anticoagulants (incl. warfarin), antiplatelet agents (including clopidogrel), selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline).
Dosage regimen:
Next Uno Express is prescribed to adults and children over 12 years of age orally after meals, 200 mg (1 capsule) 3-4 times a day. The capsules should be taken with a glass of water.
To achieve a rapid therapeutic effect, the dose can be increased to 400 mg (2 capsules) 3 times a day. When a therapeutic effect is achieved, the daily dose of the drug is reduced to 600-800 mg.
The maximum daily dose for adults is 1200 mg (do not take more than 6 capsules in 24 hours).
The maximum daily dose for children 12-18 years old is 800 mg.
Take a repeat dose no earlier than after 4 hours.
If, after using the drug for 5 days, pain or elevated body temperature persists or intensifies within 3 days, you should stop taking it and consult your doctor.
Side effects:
When using the drug Next Uno Express for 2-3 days, practically no side effects are observed.
In case of long-term use, the following side effects may occur:
- from the gastrointestinal tract (GIT): NSAID gastropathy (abdominal pain, heartburn, diarrhea, flatulence, pain and discomfort in the epigastric region), ulceration of the mucous membrane of the gastrointestinal tract (in some cases complicated by perforation and bleeding), irritation , dry mouth or pain in the mouth, ulceration of the gum mucosa, aphthous stomatitis, pancreatitis, constipation, indigestion, nausea, loss of appetite, vomiting, hepatitis,
- from the respiratory system: shortness of breath, bronchospasm, exacerbation of bronchial asthma,
- hearing impairment: hearing loss, ringing or tinnitus,
- from the central and peripheral nervous system: insomnia, anxiety, nervousness and irritability, psychomotor agitation, depression, confusion, hallucinations, rarely - aseptic meningitis (more often in patients with autoimmune diseases), headache, dizziness, drowsiness:
- from the cardiovascular system: development or worsening of heart failure, tachycardia, increased blood pressure,
- from the urinary system: acute renal failure, allergic nephritis, nephrotic syndrome (edema), polyuria, cystitis,
- from the hematopoietic organs: hemolytic anemia, aplastic anemia, thrombocytopenia and thrombocytopenic purpura, agranulocytosis, leukopenia, pancytopenia,
- from the organs of vision: reversible toxic amblyopia, blurred vision or double vision, dryness and irritation of the eyes, swelling of the conjunctiva and eyelids (allergic origin), scotoma, color vision disorders,
- allergic reactions: skin rash (usually erythematous, urticaria), skin itching, angioedema, anaphylactoid reactions, anaphylactic shock, bronchospasm, fever, erythema multiforme exudative (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell's syndrome), eosinophilia, allergic rhinitis,
- other: increased sweating.
The risk of developing ulcerations of the mucous membrane of the gastrointestinal tract, bleeding (gastrointestinal, gingival, uterine, hemorrhoidal), visual impairment (impaired color vision, scotoma, amblyopia) increases with long-term use in large doses.
If side effects occur, you should stop taking the drug and consult a doctor.
Laboratory indicators.
- bleeding time (may increase),
- serum glucose concentration (may decrease),
- creatinine clearance (may decrease),
- hematocrit or hemoglobin (may decrease),
- serum creatinine concentration (may increase),
- activity of “liver” transaminases (may increase).
Overdose:
Symptoms: abdominal pain, nausea, vomiting, lethargy, drowsiness, depression, headache, tinnitus, metabolic acidosis, coma, acute renal failure, decreased blood pressure, bradycardia, tachycardia, atrial fibrillation, respiratory arrest.
Treatment: gastric lavage (only within an hour after administration), activated charcoal, alkaline drinking, forced diuresis, symptomatic therapy.
Interaction:
Inducers of microsomal oxidation (phenytoin, ethanol, barbiturates, rifampicin, phenylbutazone, tricyclic antidepressants) increase the production of hydroxylated active metabolites of ibuprofen, increasing the risk of severe hepatotoxic reactions.
Microsomal oxidation inhibitors reduce the risk of hepatotoxicity from ibuprofen.
Ibuprofen reduces the antihypertensive effect of antihypertensive drugs (ACE inhibitors, blockers of “slow” calcium channels, etc.), the natriuretic and diuretic effectiveness of furosemide and hydrochlorothiazide, reduces the effectiveness of uricosuric drugs, enhances the ulcerogenic effect of glucocorticosteroids, colchicine, ethanol, enhances the effect of oral hypoglycemic agents and insulin , increases the blood concentration of digoxin, lithium and methotrexate.
Ibuprofen enhances the undesirable effects of estrogens when used together.
Antacids and cholestyramine reduce the absorption of ibuprofen.
Caffeine enhances the analgesic effect of ibuprofen.
When administered simultaneously, ibuprofen reduces the anti-inflammatory and antiplatelet effect of acetylsalicylic acid (an increase in the incidence of acute coronary insufficiency in patients receiving small doses of acetylsalicylic acid as an antiplatelet agent is possible after starting ibuprofen).
When prescribed with anticoagulant and thrombolytic drugs (alteplase, streptokinase, urokinase), the risk of bleeding simultaneously increases.
With the combined use of ibuprofen and cefamandole, cefoperazone, cefotetan, valproic acid, the incidence of hypoprothrombinemia increases.
Myelotoxic drugs increase the manifestations of hematotoxicity of the drug.
Cyclosporine and gold preparations enhance the effect of ibuprofen on the synthesis of prostaglandins in the kidneys, which is manifested by increased nephrotoxicity. Ibuprofen increases the plasma concentration of cyclosporine and the likelihood of developing its hepatotoxic effects.
Drugs that block tubular secretion reduce excretion and increase plasma concentrations of ibuprofen.
Ibuprofen may reduce the infectivity of mifepristone, so ibuprofen should be started no earlier than 8 to 12 days after taking mifepristone.
Concomitant administration of ibuprofen and tacrolimus may increase the risk of nephrotoxicity.
Concomitant use of ibuprofen and zidovudine may lead to increased hematological toxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive patients with hemophilia who received concomitant treatment with zidovudine and ibuprofen.
In patients receiving concomitant treatment with ibuprofen and quinolone antibiotics, the risk of seizures may increase.
Special instructions:
During treatment, monitoring of the peripheral blood picture and the functional state of the liver and kidneys is necessary.
When symptoms of gastropathy appear, careful monitoring is indicated, including esophagogastroduodenoscopy, a blood test to determine hemoglobin, hematocrit, and a stool test for occult blood.
To prevent the development of NSAID gastropathy, it is recommended to combine it with prostaglandin E drugs (misoprostol).
If it is necessary to determine 17-ketosteroids, the drug should be discontinued 48 hours before the study.
Before starting therapy, patients with a history of arterial hypertension and/or heart failure should exercise caution and consult a specialist, as fluid retention, arterial hypertension and edema associated with NSAIDs have been noted in such patients.
Long-term use may increase the risk of acute coronary artery disease or stroke.
In patients with bronchial asthma or a history of allergic diseases, the drug may cause an attack or bronchospasm.
During the treatment period, ethanol intake is not recommended.
Ibuprofen has an antiplatelet effect (weaker than acetylsalicylic acid), which requires caution when prescribed to patients with bleeding disorders and those taking anticoagulants.
It is recommended to take the drug for the shortest possible course and in the minimum effective dose necessary to eliminate symptoms. Drugs that inhibit cyclooxygenase and prostaglandin synthesis can affect ovulation, disrupting female reproductive function (reversible after discontinuation of treatment).
USE IN PREGNANCY AND BREASTFEEDING
Animal studies have not found any adverse effects of ibuprofen on the fetus. Due to the lack of sufficient well-controlled observations in humans, the drug should be used in the first and second trimesters of pregnancy only in cases of urgent need, if the potential benefit to the mother outweighs the potential risk to the fetus and child.
Ibuprofen inhibits the contraction of the uterine muscles. The effect of ibuprofen on the fetus can cause premature closure of the ductus botellus, which can lead to the development of pulmonary hypertension in the newborn. Ibuprofen should not be used during the late (third trimester) of pregnancy.
Ibuprofen was not excreted in breast milk. However, due to the limited scope of these studies and the possible adverse effect of inhibition of prostaglandin synthesis in the newborn, it is not recommended to use the drug during breastfeeding.
INFLUENCE ON THE ABILITY TO DRIVE VEHICLES AND MECHANISMS
During the treatment period, it is necessary to refrain from those activities that require increased attention and speed of mental and motor reactions.
Best before date:
2 years. Do not use after the expiration date stated on the packaging.
Storage conditions:
In a place protected from light at a temperature not exceeding 25 degrees C.
Keep out of the reach of children.
Instruction update date 12/20/2016
The instructions were approved on October 11, 2016