Orencia solution for injection 125 mg/ml 1,007 ml No. 4
Dosage forms lyophilisate for injection 250 mg solution for injection 125 mg/ml 1.007 ml International nonproprietary name? Abatacept Composition Orencia solution for injection 125 mg/ml 1.007 ml Active substance: abatacept. Excipients: sucrose, poloxamer, sodium dihydrogen phosphate monohydrate - 0.288 mg, anhydrous sodium hydrogen phosphate, water for injection. Group? Immunosuppressive drugs (immunosuppressants) Manufacturers Bristol-Myers Squibb Holdings Pharma Ltd. (United States of America) Indications for use Orencia solution for injection 125 mg/ml 1.007 ml Abatacept is indicated for reducing symptoms, enhancing clinical response, suppressing the progression of structural damage and improving functional activity in adult patients with moderate to severe active rheumatoid arthritis. Abatacept can be used as monotherapy or in combination with basic anti-inflammatory drugs. Method of administration and dosage Orencia solution for injection 125 mg/ml 1.007 ml The drug is administered subcutaneously once a week in a dose of 125 mg (1 filled syringe) regardless of body weight, after administration of a loading dose of the drug Orencia®, lyophilisate for preparing a solution for infusion or without prior loading dose. Prescription for patients who have not previously used the drug Orencia®: Without a loading dose. The drug is administered once a week subcutaneously at a dose of 125 mg (1 filled syringe) regardless of body weight; With a loading dose. If it is necessary to administer a loading dose of the drug, the patient is given intravenous administration of the drug Orencia® in accordance with the instructions for use of the drug Orencia®, lyophilisate for preparing a solution for infusion, then the first subcutaneous administration of the drug is performed during the day. Transferring a patient from intravenous to subcutaneous Orencia: When switching a patient from intravenous to subcutaneous Orencia, the first subcutaneous injection is given instead of the next scheduled infusion of Orencia. The drug for subcutaneous administration is not intended for intravenous injection or infusion. The drug is administered by medical personnel. If the patient is able to administer the injections independently, medical personnel must ensure that the patient is properly trained in this procedure and clearly follows the instructions for performing a subcutaneous injection of the drug. The drug is examined before administration. The solution should be clear or slightly opalescent, colorless to light yellow; If there are particles or a change in color of the solution, the syringe with the solution should not be used. It is necessary to inject the entire volume of the drug in a syringe, changing the injection site with each injection. Do not inject the drug into areas with delicate or rough skin, if there is damage or redness of the skin. Missing a dose If the patient misses the date of the next injection of Orencia® subcutaneous for up to 3 days, he should have an injection of the drug immediately and continue to adhere to the original weekly schedule of drug administrations. If, when a dose is missed, more than 3 days have passed from the expected date of administration, the patient should consult a doctor for instructions on the further administration schedule, which should be clarified depending on the patient’s condition and stage of the disease. No dose adjustment is required in elderly patients. Guide to using pre-filled syringe and auto-retractable syringe. Check the expiration date before using prefilled syringes and retractable needle syringes. Remove prefilled syringes from the refrigerator. Keep the syringes at room temperature for 30-60 minutes. Find a place for the syringe (a clean, flat surface). Inspect the syringes without removing the needle cap. Leave syringes at room temperature for 30-60 minutes before injection. At this time, do not remove the cap from the needle. Do not accelerate the warming of the syringe in any way, for example, by placing it in a microwave oven or in hot water. Inspect the solution through the window of the cylinder. The solution in the syringe should be transparent, pale yellow. Do not use the syringe if the solution is opaque, has a different color, or contains undissolved particles. Make sure the solution level is between the black lines on the syringe barrel. Do not administer the drug if the solution level is outside these two indicator lines. If there is an air bubble in the syringe, there is no need to remove it. Prepare supporting materials. Wash your hands thoroughly with warm water and soap. Contraindications Orencia solution for injection 125 mg/ml 1.007 ml Hypersensitivity to abatacept and/or any of the auxiliary components of the drug. Combined use with tumor necrosis factor blockers. Pregnancy (no studies have been conducted). Lactation period. Age up to 6 years. Severe uncontrolled infections (sepsis, opportunistic infections), active infections (including tuberculosis) until control is established. Combined use with azathioprine, gold drugs and anakinra. CAUTION Abatacept should be used with caution in patients with recurrent infections; conditions predisposing to infections (diabetes mellitus), hepatitis; in elderly patients. Abatacept should be discontinued if a severe infectious disease develops. USE IN PREGNANCY AND BREASTFEEDING Due to the lack of clinical studies involving pregnant women, the drug should not be used during pregnancy. Abatacept may cross the placental barrier, which in turn may increase the risk of infections in the newborn. The safety of live vaccines in neonates exposed to abatacept in utero has not been established. The use of live vaccines in these newborns is not recommended within 10 weeks of the last dose administered to the mother. It is not known whether the drug passes into breast milk, so you should not breastfeed while using the drug. Pharmacological action Immunosuppressive agent. Pharmacodynamics Abatacept is a soluble protein consisting of the extracellular domain of cytotoxic T-lymphocyte antigen-4 (CTLA-4) associated with a modified Fc fragment of human immunoglobulin GI (IgG I). Abatacept is a recombinant protein with a molecular weight of about 92 kDa, which is produced by genetic engineering in isolated mammalian cell cultures. Abatacept selectively modulates a key co-stimulatory signal required for full activation of cluster of differentiation 28 (CD 28)-expressing T cells. In patients with rheumatoid arthritis (RA), T lymphocytes are found in the synovial fluid. Activated T lymphocytes play an important role in the pathogenesis of rheumatoid arthritis and other autoimmune diseases. For complete activation of T-lymphocytes, 2 signals from antigen-presenting cells are required: the first is for recognition of a specific antigen by T-cell receptors (signal I); the second (nonspecific) costimulatory signal involves the binding of CD80 and CD86 molecules on the surface of antigen-presenting cells to the CD28 receptor on the surface of T lymphocytes (signal 2). Abatacept specifically binds to CD80 and CD86, selectively inhibiting this pathway. It has been established that abatacept has a greater effect on the response of unactivated (naive) T-lymphocytes than memory T-lymphocytes. Abatacept has been shown to reduce T cell-dependent antibody production and inflammation in in vitro studies and animal models. In vitro, abatacept reduces T-lymphocyte activation, as evidenced by a decrease in proliferation and cytokine production in human lymphocytes (TNF-alpha, interferon-γ and interleukin-2). In rats with collagen-induced arthritis, abatacept suppresses inflammation, reduces the formation of anti-collagen antibodies and antigen-specific production of interferon-γ. Pharmacokinetics. The pharmacokinetics of abatacept following subcutaneous administration follows a linear relationship. The average minimum and maximum equilibrium concentrations were established 85 days after the start of treatment and were 32.5 μg/ml (6.6-113.8 μg/ml) and 48.1 μg/ml (9.8-132.4 μg/ml). ml) respectively. The bioavailability of abatacept when administered subcutaneously is 78.6% of its bioavailability when administered intravenously. Average values of systemic clearance (0.28 ml/h/kg), volume of distribution (0.11 d/kg), terminal half-life (14.3 days). comparable for subcutaneous and intravenous administration. It was found that higher clearance of abatacept is observed in patients with high body weight. The age and gender of patients (when adjusted for body weight) did not affect the clearance of abatacept. The simultaneous administration of methotrexate, anti-inflammatory drugs, glucocorticosteroids and tumor necrosis factor blockers did not affect the clearance of abatacept. Studies have not been conducted to evaluate the metabolism and elimination of abatacept in humans. Due to its spatial structure and hydrophilicity, abatacept is not metabolized in the liver by enzymes of the cytochrome P450 system. Given the large molecular weight of abatacept, it is expected that abatacept is not excreted in the urine. Pharmacokinetics in special categories of patients No studies have been conducted to evaluate the effect of renal and hepatic dysfunction on the pharmacokinetics of abatacept. Side effects Orencia injection solution 125 mg/ml 1.007 ml Frequent adverse drug reactions (ADRs) when using abatacept in clinical studies where the drug or placebo was used with other types of RA therapy. ADRs are presented by organs and systems: very common (>10%); Headache, nausea and upper respiratory tract infections (including sinusitis) were common (>1% and 0.1% and 0.01% and 5%) in patients treated with Orencia®. Serious infections that are at least likely to be related to the drug have been reported in 1.5% of adult patients. The type and incidence of serious infections were similar to those in the placebo group. The profile of adverse reactions in adult patients and children is the same. In rare cases, the following types of malignant neoplasms have been observed in patients treated with Orencia®: non-melanoma skin neoplasms, solid tumors (lung cancer), hematological neoplasms (lymphoma). The incidence of malignant tumors in patients with rheumatoid arthritis did not increase when using Orencia®. In 5.2% of patients with the administration of Orencia® (within 1 hour after the start of the infusion), acute reactions to the drug were observed, the most common being dizziness (1.5%). Other acute reactions to the administration of the drug were observed in 0.1-1.0% of patients: decreased blood pressure, tachycardia, bronchospasm, shortness of breath, myalgia, nausea, erythema, hot flashes, urticaria, hypersensitivity reactions, itching, tightness in the throat, chest discomfort, chills, infusion site bruising, infusion site pain, infusion site swelling, infusion reactions, rash. Anaphylactic reactions with the administration of the drug Orencia® were observed rarely, and hypersensitivity reactions were infrequent. Other reactions potentially associated with hypersensitivity, such as decreased blood pressure, urticaria, and respiratory distress occurring within 24 hours of the start of the infusion, were also observed infrequently. When using the drug Orencia® in patients with chronic obstructive pulmonary disease (COPD), adverse events were observed more often than in the placebo group, incl. serious - exacerbation of COPD and bronchitis. Respiratory disorders (including shortness of breath and exacerbation of COPD) were observed in 5.9% of patients. In 4.8% of patients receiving Orencia® for up to 8 years, the formation of antibodies to abatacept was observed, which persisted after discontinuation of the drug (> 42 days from the last dose). However, no dependence was found on the severity of the clinical effect and the development of side effects on the presence of antibodies to abatacept in the blood plasma. Data from post-marketing studies. During post-marketing studies, it was found that systemic reactions to infusion administration of the drug were similar to those identified during clinical trials of Orencia®, with the exception of one case of fatal anaphylaxis. Adverse drug reactions with subcutaneous administration of Orencia® included itching, tightness in the throat, and shortness of breath. Overdose Doses up to 50 mg/kg when administered intravenously did not cause obvious toxic effects. In case of overdose, medical supervision and, if necessary, symptomatic treatment are recommended. Overdose symptoms are not described. Interaction Orencia solution for injection 125 mg/ml 1.007 ml When using abatacept together with tumor necrosis factor blockers, the risk of serious infections increases, so the use of this combination is not recommended. When transferring a patient from treatment with a tumor necrosis factor blocker to abatacept therapy, the patient's condition should be monitored due to the possible development of infection. The drug can be used in conjunction with basic anti-inflammatory drugs: methotrexate, glucocorticosteroids, salicylates, NSAIDs, as well as less commonly used anti-inflammatory drugs: chloroquine/hydroxychloroquine, sulfasalazine and leflunomide. There was no change in the clearance of abatacept when combined with methotrexate, NSAIDs, glucocorticosteroids and TNF-a inhibitors. There is insufficient information about the safety and effectiveness of the combination of abatacept with azathioprine, gold drugs and anakinra, so combined use with these drugs is not recommended. Abatacept has not been studied in combination with drugs that cause a decrease in lymphocyte counts. With this combination, it is possible to potentiate the effect of abatacept on the immune system. Special instructions Hypersensitivity reactions Hypersensitivity reactions can occur during treatment with any injectable protein drug. Such reactions were observed with the use of Orencia® during clinical studies. After the first administration of the drug, there is a possibility of developing anaphylaxis or anaphylactoid reactions, including life-threatening ones. During post-marketing studies, a case of fatal anaphylaxis was reported after the first infusion of Orencia®. In clinical studies, cases of anaphylaxis were rare and hypersensitivity reactions were uncommon. If an anaphylactic or other serious allergic reaction occurs, discontinue use of the drug (both intravenous and subcutaneous forms) without subsequent resumption and immediately begin appropriate treatment for the adverse reaction. Infections When using the drug, cases of serious infections, including sepsis and pneumonia, including fatal ones, have been reported, more often in patients using concomitant therapy with immunosuppressants. If during treatment a new infectious disease is identified in a patient, the patient should be closely monitored, and if a new serious infection develops, the drug should be discontinued. The safety of the drug in patients with latent tuberculosis has not been studied. When prescribing the drug, it is necessary to conduct a diagnosis to detect tuberculosis. Before prescribing abatacept, patients with latent tuberculosis should receive standard anti-tuberculosis therapy. When prescribing antirheumatic drugs, reactivation of the hepatitis B virus may occur, therefore, before starting treatment with abatacept, carriage of this pathogen should be excluded. The use of the drug in patients with viral hepatitis has not been studied. Effect on the development of malignant neoplasms The potential role of Oresnia® in the development of malignant neoplasms has not been established. When using the drug Orencia® in patients with rheumatoid arthritis, there was no increase in the incidence of malignant neoplasms. Effect on the immune system. Drugs that affect the immune response, including Orencia®, may affect the effectiveness of vaccinations and the body's ability to resist infections and the development of malignant tumors. Because medications that affect the immune system, including abatacept, may reduce the effectiveness of vaccinations, live vaccines should not be used during treatment with abatacept and for 3 months after its discontinuation. There is no evidence of secondary infection of patients receiving abatacept from patients receiving live vaccines. It is possible to use inactivated vaccines during treatment with the drug. There was no significant influence of the drug on the effectiveness of vaccine prevention with the help of a 23-band pneumococcal vaccine, in most patients an adequate immune response (an increase in the antibodies titer) was observed after this vaccination. Also, during the treatment with Orencia®, it is possible to vaccinate a trivalent vaccine from the seasonal influenza virus-the immune reaction in most patients was expressed in at least a 4-fold increase in antibodies. Due to the fact that the risk of developing serious infections and malignant neoplasms in patients over 65 years old as a whole than in young people, caution should be observed in the prescription of abatactation for elderly patients. The impact on the ability to drive vehicles and work with mechanisms should refrain from driving vehicles and classes of other potentially dangerous types of activities that require increased concentration of attention and speed of psychomotor reactions, if the drug causes dizziness, visual impairment and other side effects that can affect these abilities . Storage conditions are stored in the inaccessible for children, a place protected from light at a temperature of 2 to 8 ° C. Do not freeze!
Orencia® (Orenсia)
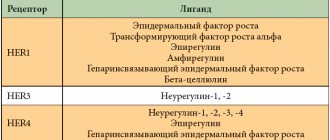
Blocker of co-stimulation of T-lymphocytes. It is a soluble hybrid protein molecule consisting of the extracellular domain of human CTLA4 (cytotoxic T-lymphocyte-associated antigen 4) linked to a modified Fc (CH2 and CH3 regions) fragment of human IgG1. Abatacept is produced by recombinant DNA technology in Chinese hamster ovary cells. The approximate molecular weight of abatacept is 92 kilodaltons.
Abatacept is a co-stimulation modulator of the interaction of CD80 and CD86 on antigen-presenting cells (APCs) with CD28 on T lymphocytes.
Abatacept modulates a key costimulatory signal that is required for full activation of T lymphocytes expressing CD28. T lymphocytes are found in the synovium of patients with rheumatoid arthritis. Activated T-lymphocytes are part of the pathogenesis of rheumatoid arthritis and other rheumatic diseases. For complete activation of T-lymphocytes, 2 signals are required, which are realized with the participation of APCs: identification of a specific antigen by T-cell receptors (1 signal); a costimulatory signal, which is provided through the interaction of the CD28 receptor on T lymphocytes and CD80/CD86 on APCs. Abatacept specifically binds to CD80/CD86, inhibiting this costimulatory pathway, which blocks T cell activation.
Abatacept has been shown to suppress T-cell-dependent antibody responses and inflammation in in vitro studies and animal models. In vitro, abatacept suppresses the activation of T lymphocytes, which is reflected by a decrease in proliferation and cytokine production. Abatacept reduces the production of antigen-specific TNFα, interferon gamma and IL 2 by T lymphocytes. In a model of collagen arthritis (in rats), abatacept suppresses inflammation, reduces the production of anticollagen and antigen-specific production of interferon gamma.
In clinical studies, abatacept at doses of approximately 10 mg/kg has been shown to inhibit T-lymphocyte activation, reduce the production of macrophages, fibroblast-like synovocytes and B cells, and suppress the acute phase of inflammatory reactivation. A decrease in serum levels of soluble IL 2 receptor, a marker of T-lymphocyte activation, was observed; IL 6, a product of activation of macrophages and fibroblast-like synoviocytes; rheumatoid factor, antibodies produced by plasma cells; C-reactive protein, a marker of the acute phase of inflammation reactivation. In addition, a decrease in serum levels of matrix metalloproteinase-3, which causes cartilage destruction and tissue structural changes, was observed. A decrease in serum TNFα levels was also observed.
Orencia®
Hypersensitivity reactions
Hypersensitivity reactions may occur during treatment with any injectable protein drug. Such reactions were observed with the use of Orencia® during clinical studies. After the first administration of the drug, there is a possibility of developing anaphylaxis or anaphylactoid reactions, including life-threatening ones. During post-marketing studies, a case of fatal anaphylaxis was reported after the first infusion of Orencia®. If an anaphylactic or other serious allergic reaction occurs, use of Orencia® (both lyophilisate for infusion and subcutaneous solution) should be discontinued without further resumption and appropriate treatment for the adverse reaction should be initiated immediately.
Infections
When using the drug, there have been cases of serious infections, including sepsis and pneumonia, including fatal ones, more often in patients using concomitant therapy with immunosuppressants. If during treatment a new infectious disease is identified in a patient, the patient should be closely monitored, and if a new serious infection develops, the drug should be discontinued. The safety of the drug in patients with latent tuberculosis has not been studied. Before prescribing abatacept, patients with latent tuberculosis should receive standard anti-tuberculosis therapy.
When prescribing antirheumatic drugs, reactivation of the hepatitis B virus may occur, therefore, before starting treatment with abatacept, carriage of this pathogen should be excluded. The use of the drug in patients with viral hepatitis has not been studied.
Influence or development of malignant neoplasms
The potential role of Orencia® in the development of malignant neoplasms has not been established. The incidence of malignancies during clinical trials of the infusion form of the drug was similar for patients receiving Orencia® and patients receiving placebo.
Effect on the immune system
Drugs that affect the immune response, including Orencia®. may affect the effectiveness of vaccinations, the body’s ability to resist infections and the development of malignant tumors.
Because medications that affect the immune system, including abatacept, may reduce the effectiveness of vaccinations, live vaccines should not be used during treatment with abatacept and for 3 months after its discontinuation. It is possible to use inactivated vaccines during treatment with the drug. When prescribed to children, it is recommended to complete the mandatory vaccination plan before starting to use the drug.
There was no significant effect of the drug on the effectiveness of vaccination using the 23-valent pneumococcal vaccine; most patients had an adequate immune response (increase in antibody titer) after this vaccination. Also, during treatment with Orencia®, vaccination with a trivalent vaccine against the seasonal influenza virus is possible - the immune reaction in most patients was expressed in at least a 4-fold increase in the level of antibodies.
Determination of blood glucose concentration
On the day of drug administration, it is possible to obtain false-positive results for determining blood glucose using tests due to a reaction with maltose contained in the drug. To determine glucose concentration, methods that exclude reaction with maltose should be used.