Pertuzumab is an innovative treatment for HER2-positive breast cancer (BC) that has not responded to trastuzumab.
Before the advent of targeted therapy, HER2-positive breast cancer would have been the most unfavorable tumor variant in terms of treatment and survival prognosis. The situation changed dramatically with the development and introduction into practice of monoclonal antibodies against this receptor. Today it is considered one of the most favorable and promising types of breast cancer in terms of treatment. However, not all patients with this type of tumor fully respond to trastuzumab-containing therapy. Some had primary resistance, when the tumor was resistant to treatment in the first line of therapy. Other patients developed secondary resistance over time. Therefore, the search for treatment methods continued, and one of the options was the use of a combination of trastuzumab, pertuzumab and docetaxel.
Pharmacological action of pertuzumab
The active ingredient pertuzumab is a humanized monoclonal antibody that binds to the extracellular domain of the HER-2 receptor and blocks its connection to other receptors. Let's figure out how it works.
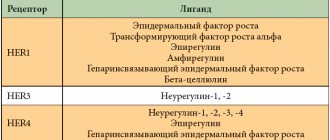
There is a family of epidermal growth factor receptors that trigger a cascade of reactions that ensure cell growth and reproduction. If the number of these receptors is significantly higher than normal, as happens in cancer cells, they begin to divide and multiply uncontrollably. This family includes 4 receptors:
- HER-1.
- HER-2.
- HER-3.
- HER-4.
All of them, except HER-2, begin to work after binding to ligands. The activity of receptors is manifested only when they are associated with other receptors of their family. This state is called dimerization. These can be homodimers, when two identical receptors bind, for example HER-2/HER-2, or heterodimers, when dissimilar receptors bind, for example HER-2/HER-3.
The extracellular part of HER-2 has 4 parts (subdomains), each of which has its own functions. Trastuzumab blocks the action of the fourth part, and pertuzumab blocks the second part, which is responsible for dimerization with other receptors. It is believed that it is the formation of the HER-2/HER-3 dimer that leads to resistance to trastuzumab. To complete the antitumor effect, it is necessary that 2 subdomains be blocked simultaneously, so 2 targeted drugs are prescribed simultaneously - trastuzumab and pertuzumab.
Compound
Pertuzumab is available as a concentrate, which must be dissolved before infusion.
The concentrate has the appearance of a transparent, opalescent, colorless liquid. A slightly brownish color is acceptable. 1 ml of concentrate contains 30 mg of active substance, one bottle contains 420 mg.
The drug is packaged in colorless transparent glass bottles of 14 ml. Each bottle is packed in a cardboard box.
L-histidine, acetic acid, sucrose, polysorbate and deionized water are used as excipients.
Pharmacokinetics
The pharmacokinetics of pertuzumab were studied only after intravenous administration. In this case, different dosages were used in patients with different types of tumors. The results showed that there were no pharmacokinetic differences between early and late stage breast cancer.
Suction
The drug is administered intravenously. Other routes of administration have not been studied.
Distribution
Pertuzumab is distributed in plasma and extracellular fluid.
Metabolism
There have been no separate studies of the metabolism of pertuzumab. It is assumed that, like all monoclonal antibodies, it undergoes catabolic processes - oxidation or breakdown to simpler substances.
Removal
The half-life is 17.2-18.0 days. Clearance 0.235 l/day.
Special cases
No changes were found in the pharmacokinetics of pertuzumab depending on gender and ethnicity.
Slight changes in pertuzumab clearance were observed based on true body weight (body weight excluding fat tissue) and serum albumin levels. But dosage adjustments were not required when these indicators changed.
The pharmacokinetics of pertuzumab in the elderly have not been studied. But population observation data indicate that there are no significant differences.
There have been no separate studies examining the pharmacokinetics of pertuzumab in patients with renal failure. There is population data that renal failure, including severe renal failure, does not affect the pharmacokinetics of the drug. However, so far they cannot be called convincing. No studies have been conducted in liver failure.
The independent data monitoring committee (IDMC) recommended disclosure of randomization treatment codes based on superiority of the drug based on the primary efficacy endpoint; results also indicate a strong trend toward improved overall survival
It is planned to submit an application for registration of a new indication
Positive results from the head-to-head phase III comparative study DESTINY-Breast03 showed that trastuzumab deruxtecan
, an anti-HER2 antibody-drug conjugate (ADC) marketed by Daiichi Sankyo Company Limited, is more effective than trastuzumab emtansine (T-DM1).
During a planned interim analysis, the independent data monitoring committee (IDMC) confirmed that the DESTINY-Breast03 trial met its primary endpoint and observed a statistically and clinically significant increase in progression-free survival (PFS) in patients with HER2-positive, unresectable and/or metastatic breast cancer previously treated with trastuzumab and taxanes.
In the DESTINY-Breast03 study, in patients treated with trastuzumab deruxtecan,
There was also a strong trend toward improved overall survival (OS) compared with T-DM1, although OS data are immature.
The safety profile of trastuzumab deruxtecan
was consistent with previous clinical studies, with no new safety signals identified and no treatment-related incidents of grade 4 or 5 interstitial lung disease.
Executive Vice President and Head of Oncology Research and Development Susan Galbraith Fr.
Ken Takeshita, Chief Research and Development Officer, said: “DESTINY-Breast03 is the first international, head-to-head, phase III study evaluating trastuzumab deruxtecan.
relative to the active control drug, confirming the possibility of using the study drug as a new standard of care for patients with HER2-positive metastatic breast cancer who have received prior therapy with trastuzumab and taxanes. We believe that this advanced and purpose-designed ADC drug delivers on the promise of changing the standard of care for HER2-positive metastatic breast cancer, and our goal is to move to earlier lines of therapy for HER2-positive breast cancer and many other types of HER2-expressing breast cancer. tumors as part of our extensive clinical research program."
The study data will be presented at an upcoming medical conference and submitted for registration of a new drug indication.
Trastuzumab deruxtecan
approved for the treatment of adult patients with unresectable or metastatic HER2-positive breast cancer who have received two or more prior lines of therapy containing anti-HER2 targeted agents for metastatic disease in the United States, Japan, the EU and certain other countries, based on results of the DESTINY-Breast01 study.
Trastuzumab deruxtecan
is being further evaluated in a comprehensive clinical development program for efficacy and safety in a variety of cancers where HER2 receptors are the target of therapy, including breast, gastric, lung and colorectal cancer.
HER2 positive breast cancer
Breast cancer remains the most common malignancy and is considered one of the leading causes of cancer mortality in women worldwide1. In 2022, breast cancer was diagnosed in more than two million patients worldwide and caused nearly 685,000 deaths1. Approximately one in five patients diagnosed with breast cancer is HER2 positive2.
The HER2 receptor is a cell growth-promoting tyrosine kinase receptor that is expressed on the cell surface of many tumors, including breast, gastric, lung and colorectal cancer3. Overexpression of the HER2 receptor can occur as a result of amplification of the HER2 gene and is often associated with aggressive disease and poor prognosis in breast cancer4.
Despite prior therapy with trastuzumab and taxanes, patients with HER2-positive metastatic breast cancer often experience disease progression5. More effective treatment options are needed to further delay progression and improve overall survival5–7.
Study DESTINY-Breast03
DESTINY-Breast03 is an international, head-to-head, comparative, randomized, open registration phase III study to evaluate the efficacy and safety of trastuzumab deruxtecan.
(5.4 mg/kg) compared with T-DM1 in patients with HER2-positive unresectable and/or metastatic breast cancer previously treated with trastuzumab and taxanes. The primary efficacy endpoint in the DESTINY-Breast03 study was PFS based on an independent, blinded central assessment. Secondary efficacy endpoints include OS, objective response rate, duration of response, clinical benefit, investigator-assessed PFS, and safety.
The DESTINY-Breast03 study enrolled approximately 500 patients at multiple sites in Asia, Europe, North America, Oceania and South America. For more information about the study, visit ClinicalTrials.gov.
Trastuzumab deruxtecan
Trastuzumab deruxtecan
is an ADC based on an anti-HER2 monoclonal antibody.
Developed using proprietary exatecan derivative (DXd) ADC technology, trastuzumab deruxtecan
is the flagship ADC drug in the oncology drug portfolio and its research is the most advanced ADC research program on the platform.
Trastuzumab deruxtecan
consists of an anti-HER2 receptor monoclonal antibody linked to the exatecan-derived topoisomerase I inhibitor drug substance via a stable cleavable tetrapeptide linker.
Trastuzumab deruxtecan
(5.4 mg/kg) is approved in Canada, the EU, Israel, Japan and the USA for the treatment of adult patients with unresectable or metastatic HER2-positive breast cancer who have received two or more prior lines of therapy containing anti-HER2 targeted agents, according to regarding the metastatic form of the disease, based on the results of the DESTINY-Breast01 study.
Trastuzumab deruxtecan
(6.4 mg/kg) is also approved in Israel, Japan and the United States for the treatment of adult patients with locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma previously treated with trastuzumab, based on results from the DESTINY-Gastric01 trial.
Development program for the drug trastuzumab deruxtecan
An international clinical development program is currently underway to evaluate the efficacy and safety of monotherapy with trastuzumab deruxtecan.
in a variety of tumors where HER2 receptors are the target of therapy, including breast, gastric, lung and colorectal cancer. Studies are also being conducted to evaluate the use of the drug in combination with other anticancer therapies, in particular immunotherapy.
According to the 2022 Cancer Therapeutics Clinical Advances Report, trastuzumab deruxtecan
cited as one of two significant advances in the ASCO Clinical Oncology Advances of the Year: Advances in Treatment of Gastrointestinal Tumors Based on Tumor Molecular Profile, based on the results of the DESTINY-CRC01 and DESTINY-Gastric01 studies, as well as one of the year's advances in targeted therapy therapy for non-small cell lung cancer (NSCLC) based on interim results obtained in the group of patients with a HER2 mutation in the DESTINY-Lung01 trial.
In May 2022, the drug trastuzumab deruxtecan
was granted breakthrough therapy designation for patients with metastatic non-small cell lung cancer with a HER2 gene mutation and progression during or after treatment with platinum-based drugs.
Cooperation with
and Daiichi Sankyo entered into an international agreement on the joint development and launch of the drug trastuzumab deruxtecan
(anti-HER2 monoclonal antibody ADC) in March 2019, and datopotamab deruxtecan (DS-1062; anti-TROP2 monoclonal antibody ADC) in July 2022 (except in Japan, where exclusive rights are held).
is responsible for the production and supply of trastuzumab deruxtecan
and datopotamab deruxtecan.
About working in breast cancer
With increased knowledge in the biology of breast cancer, I am ready to challenge and rethink the current clinical concept of classification and treatment of breast cancer in order to improve the effectiveness of patient care. The company has a bold goal to eliminate breast cancer as a cause of death.
The portfolio includes a wide range of approved and promising drugs in development with different mechanisms of action in the biologically diverse microenvironment of breast cancer cells. is committed to further improving treatment outcomes for hormone-positive breast cancer with the foundational drugs Faslodex
(fulvestrant) and
Zoladex
(goserelin), as well as an innovative oral selective estrogen receptor suppressor (SERD) drug and a potential new drug AZD9833.
PARP inhibitor drug Lynparza®
(olaparib) is used for targeted therapy of patients with metastatic breast cancer and the presence of a germline mutation in the
BRCA
.
and MSD (Merck & Co., Inc. in the United States and Canada) are continuing to study Lynparza in patients with metastatic breast cancer and the presence of a germline mutation in the BRCA
and are exploring new treatment options for patients in the early stages of the disease.
Based on the first approval of the drug trastuzumab deruxtecan,
an anti-HER2 receptor-based ADC in patients previously treated for HER2-positive metastatic breast cancer, and Daiichi Sankyo is exploring the potential of this drug in earlier lines of therapy and in newly diagnosed breast cancer .
In search of life-saving treatment options for patients with triple negative breast cancer (an aggressive form of breast cancer), is exploring immunotherapy with Imfinzi (
durvalumab) in combination with other anticancer drugs, including
Lynparza®
and
trastuzumab deruxtecan
, exploring the potential of using an AKT kinase inhibitor, capivasertib, in combination with chemotherapy, and is collaborating with to study the potential of the anti-TROP2 ADC drug datopotamab deruxtecan.
About working in the field of oncology
is revolutionizing oncology, striving to develop drugs that can cure various malignant tumors, using scientific advances to understand the nature of malignant tumors in all their versatility to create, develop and introduce revolutionary drugs for patients. The company's interests are focused on some of the most challenging tumor types. It is through continuous innovation that we have created one of the most diverse product lines in the industry that can drive changes in clinical practice and improve treatment outcomes. is committed to rethinking cancer treatment and eliminating cancer as a cause of death.
ABOUT
AstraZeneca (LSE/STO/Nasdaq: AZN)
is an international science-based biopharmaceutical company focused on the research, development and commercialization of prescription drugs primarily in the therapeutic areas of oncology, cardiology, nephrology and metabolism, respiratory and autoimmune diseases. , based in Cambridge (UK), is represented in more than 100 countries, and its innovative products are used by millions of patients around the world. Follow company news on the website astrazeneca.ru and Twitter @AstraZeneca.
List of sources
1. Sung H, et al
.
Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin
. 2021; 10.3322/caac.21660.
2. Ahn S, et al
.
HER2 status in breast cancer: changes in guidelines and complicating factors for interpretation. J Pathol Transl Med
. 2020; 54(1): 34-44.
3. Iqbal N, et al
.
Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Mol Biol Int
. 2014;852748.
4. Pillai R, et al
.
HER2 mutations in lung adenocarcinomas: A report from the Lung Cancer Mutation Consortium. Cancer
. 2017;1;123(21):4099-4105.
5. Barok M, et al
.
Trastuzumab emtansine: mechanism of action and drug resistance. Breast Cancer Res
. 2014; 16(2):209.
6. Moonsey L, et al
.
Changing Natural History of HER2-Positive Breast Cancer Metastatic to the Brain in the Era of New Targeted Therapies. Clin Breast Cancer
. 2018; 18(1):29-37.
7. Martinez-S Saez O, et al
.
Current and Future Management of HER2-Positive Metastatic Breast Cancer. JCO Oncol Pract
. 2022. 10.1200/OP.21.00172.
Indications for use
Pertuzumab is used to treat HER-2 positive breast cancer. Validated research methods for the level of expression of this receptor are first required. These methods include immunohistochemical analysis (IHC) and in situ hybridization, in particular fluorescent hybridization (FISH). The criterion for prescribing targeted therapy is an IHC score of 3 or gene amplification according to FISH.
The combination of trastuzumab, pertuzumab and docetaxel is prescribed in the following cases:
- Treatment of breast cancer with distant metastases.
- Locally recurrent breast cancer tumors.
- Inoperable breast cancer.
The condition for prescribing this regimen is the absence of a previous history of targeted treatment and chemotherapy. A combination of pertuzumab, trastuzumab and cytostatics (not taxanes) is prescribed for the treatment of breast cancer without distant metastases in the following cases:
- Preoperative therapy for early locally advanced HER2+ breast cancer.
- Postoperative treatment of early HER2+ breast cancer, when the tumor exceeds 2 cm in size or has already given regional metastases.
Dosage regimen
Pertuzumab should be used both in hospital and outpatient settings. It is administered exclusively intravenously. Jet or bolus administration is strictly prohibited.
To prepare the finished drug, an isotonic NaCl solution is used. The use of dextrose for dissolution is not recommended as it leads to chemical and physical instability.
The drug is diluted under aseptic conditions. Considering that it does not contain antimicrobial preservatives, it is necessary to carefully observe sterile conditions. After dilution, 14 ml of the prepared concentrated solution is taken and injected into an infusion bag with an isotonic NaCl solution (its volume should be 250 ml). It is allowed to use infusion bags based on polyvinyl chloride, polyethylene or polyolefin.
To ensure even mixing, the infusion bag is carefully inverted several times. After this, the resulting solution is checked for the formation of impurities or color changes. The prepared solution must be used immediately. In extreme cases, it can be stored for 24 hours in a refrigerator. In this case, it is necessary to make sure that the preparation of the solution was carried out according to all the rules of asepsis and sterility. Responsibility for the quality of the solution lies with the specialist who prepared it.
Also, pertuzumab should not be mixed with other drugs. With complex use, sequential administration of drugs is necessary.
During the first administration, a loading dose of 840 mg of pertuzumab is given. The duration of the infusion should be one hour. The drug is then administered every three weeks in a maintenance dosage. If subsequent administrations are well tolerated, the infusion time can be reduced. The shortest possible time is 30 minutes. After the procedure is completed, the patient remains under observation for 30-60 minutes.
Features of use in complex therapy
Trastuzumab
Targeted drugs are used sequentially. The sequence can be any.
During the initial administration of trastuzumab, a loading dose of 8 mg/kg is given. Administration is carried out in the form of intradrop infusion over one and a half hours. The maintenance dose is 6 mg/kg and is applied once every three weeks via a 30-90 minute dropper. The time is determined by the tolerability of the drug in a particular patient.
The second option for using trastuzumab is to administer a fixed dose, which is 600 mg, regardless of the patient’s body weight. The administration regimen is the same - once every three weeks in the form of intradroplet 30-90 minute infusions. No loading dose is required.
Treatment with taxanes (docetaxel)
Taxanes are administered after targeted drugs. The dosage for the first administration is 75 mg/m2. After this, infusions are carried out at intervals of 3 weeks. If all is well, the dosage is increased to 100 mg/m2 (if the treatment regimen does not involve the use of carboplatin).
Features of stage 4 breast cancer treatment
targeted therapy with trastuzumab and pertuzumab together with docetaxel is used. In this case, docetaxel is used in the first 6 cycles of therapy, if there are no signs of tumor progression or intolerance phenomena. The need for its further use is determined by the doctor. If docetaxel is discontinued, treatment is continued with targeted agents only.
Features of the use of pertuzumab with paclitaxel
When using paclitaxel and pertuzumab in combination, the dosage of the first drug should be 80 mg/m2. It is administered intravenously by infusion weekly.
Features of adjuvant targeted therapy with pertuzumab and trastuzumab
Patients who received the combination treatment preoperatively can continue to take targeted therapy for up to a year after surgery. The condition for discontinuation of treatment is loss of effectiveness, as evidenced by tumor progression, or the development of severe complications.
If treatment was carried out as part of postoperative therapy, it is also carried out for a year (maximum 18 cycles), or until the effect ceases or severe complications develop.
Omission in the use of drugs
If the time between infusions is less than 6 weeks, maintenance dosages should be administered as soon as possible.
If more than 6 weeks have passed, therapy is started again with the introduction of loading doses - 840 mg of pertuzumab in the form of an hour-long dropper and 8 mg/kg of trastuzumab in the form of an hour and a half dropper. Then treatment is continued according to the maintenance regimen.
Trastuzumab
Because the half-life of trastuzumab is approximately 28-38 days, the drug may remain in the blood for up to 27 weeks after completion of therapy. Patients receiving anthracyclines after completing treatment with trastuzumab may have an increased risk of cardiac dysfunction. If possible, clinicians should avoid prescribing anthracycline-based chemotherapy for 27 weeks after completion of trastuzumab therapy. When using anthracycline drugs, careful monitoring of cardiac function should be performed.
The need for routine cardiac evaluation should be assessed in patients with suspected cardiovascular disease. All patients should have cardiac function monitored during treatment (eg, every 12 weeks).
As a result of monitoring, it is possible to identify patients who have developed cardiac dysfunction.
In patients with asymptomatic cardiac dysfunction, more frequent monitoring (eg, every 6 to 8 weeks) may be beneficial. With prolonged deterioration in left ventricular function that does not manifest itself symptomatically, it is advisable to consider discontinuation of the drug if there is no clinical benefit from its use. The safety of continuing or restarting trastuzumab therapy in patients who develop cardiac dysfunction has not been studied.
If the left ventricular ejection fraction decreases by > 10 units from the initial value and below the value of 50%, treatment should be suspended. Re-evaluation of left ventricular ejection fraction should be performed in approximately 3 weeks. If left ventricular ejection fraction does not improve or continues to decrease, or if symptoms of chronic heart failure occur, discontinuation of trastuzumab treatment should be considered unless the benefits to the individual patient outweigh the risks. All these patients should be referred to a cardiologist for evaluation and monitored.
If symptomatic heart failure develops during trastuzumab therapy, appropriate standard medical therapy for chronic heart failure should be administered. Most patients with chronic heart failure or asymptomatic cardiac dysfunction in pivotal studies showed improvement with standard drug therapy: angiotensin-converting enzyme inhibitors or angiotensin receptor blockers and beta-blockers. When there was clinical benefit from trastuzumab, the majority of patients with cardiac adverse reactions continued therapy without experiencing additional clinically significant cardiac reactions.
It is not recommended to use trastuzumab in combination with anthracyclines for the treatment of metastatic breast cancer.
The risk of developing cardiac dysfunction in patients with metastatic breast cancer is increased with prior anthracycline therapy, but is lower compared with concomitant use of anthracyclines and trastuzumab.
Patients with early stages of breast cancer should have a cardiac evaluation before starting treatment, every 3 months during therapy, and every 6 months thereafter for 24 months after the last dose of the drug. Longer-term monitoring is recommended after treatment with trastuzumab in combination with an anthracycline, with annual examinations for 5 years after the last dose of trastuzumab or beyond if there is a persistent decrease in left ventricular ejection fraction.
Treatment with trastuzumab is not recommended for patients in the early stages of breast cancer (adjuvant and neoadjuvant therapy) with: a history of myocardial infarction; angina pectoris requiring treatment; chronic heart failure (NYHA functional class II-IV) in history or currently; left ventricular ejection fraction below 55%; other cardiomyopathies; arrhythmias requiring treatment; clinically significant heart defects; poorly controlled arterial hypertension, with the exception of arterial hypertension amenable to standard drug therapy; and hemodynamically significant pericardial effusion, since the effectiveness and safety of the drug in such patients have not been studied.
It is not recommended to use trastuzumab in combination with anthracyclines as part of adjuvant therapy. In patients with early-stage breast cancer receiving trastuzumab (intravenously) after anthracycline-based chemotherapy, there was an increased incidence of symptomatic and asymptomatic adverse cardiac events compared with those receiving chemotherapy with docetaxel and carboplatin (regimens that do not contain anthracycline drugs). row). However, the difference was greater in cases of concomitant use of trastuzumab and taxanes than in cases of sequential use.
Regardless of the regimen used, the majority of symptomatic cardiac events occurred in the first 18 months of treatment. A prolonged increase in the cumulative incidence of symptomatic cardiac events or events associated with decreased left ventricular ejection fraction was observed in 2.37% of patients receiving trastuzumab with taxanes after anthracycline therapy, compared with 1% of patients in the comparator groups (anthracycline and cyclophosphamide group , then taxanes, and in the group of therapy with taxanes, carboplatin and trastuzumab).
Identified risk factors for the development of adverse cardiac events during adjuvant trastuzumab therapy are: age > 50 years, low baseline left ventricular ejection fraction (<55%) before and after initiation of paclitaxel treatment, decrease in left ventricular ejection fraction by 10-15 units, previous or concomitant use of antihypertensive drugs.
The risk of cardiac dysfunction in patients receiving trastuzumab after completion of adjuvant chemotherapy was associated with a higher total anthracycline dose before initiation of trastuzumab and a body mass index >25 kg/m2.
For patients with early-stage breast cancer who may be eligible for neoadjuvant-adjuvant therapy, the use of trastuzumab with anthracyclines is recommended only if they have not previously received chemotherapy and only when using low-dose anthracycline regimens (maximum total dose of doxorubicin 180 mg/day). m2 or epirubicin 360 mg/m2).
In patients who have received a full course of low-dose anthracyclines and trastuzumab as part of neoadjuvant therapy, additional cytotoxic chemotherapy after surgery is not recommended. In all other cases, the decision about the need for additional cytotoxic chemotherapy is made based on individual factors.
Experience with the use of trastuzumab in combination with low-dose anthracycline regimens is limited to two studies. When trastuzumab was used in conjunction with neoadjuvant chemotherapy, which included three to four cycles of neoadjuvant anthracycline therapy (total dose of doxorubicin 180 mg/m2 or epirubicin 300 mg/m2), the incidence of symptomatic cardiac dysfunction was low (1.7%).
Clinical experience in patients over 65 years of age is limited.
Premedication may be used to reduce the risk of reactions to administration.
Although no serious administration-related reactions (including dyspnea, hypotension, wheezing, bronchospasm, tachycardia, decreased hemoglobin oxygen saturation, and respiratory distress syndrome) have been reported for trastuzumab subcutaneous dosage form, care must be taken to caution as these events have been observed with the administration of intravenous trastuzumab.
Analgesics, antipyretics such as paracetamol, or antihistamines such as diphenhydramine may be taken. Serious reactions associated with intravenous trastuzumab were successfully treated with beta-agonists, glucocorticosteroids, and oxygen inhalation. In rare cases, these reactions have been associated with a fatal outcome. The risk of fatal injection-related reactions is greater in patients with dyspnea at rest due to pulmonary metastases or underlying medical conditions, and such patients should not receive trastuzumab therapy.
Caution should be exercised when using trastuzumab in the subcutaneous dosage form, as severe pulmonary events, sometimes accompanied by death, have been reported with the use of trastuzumab in the intravenous dosage form in the post-marketing period. These phenomena can occur both during the administration of the drug and delayed. In addition, cases of interstitial lung disease, including pulmonary infiltrates, acute respiratory distress syndrome, pneumonia, pneumonitis, pleural effusion, acute pulmonary edema and respiratory failure, have been observed. Risk factors associated with interstitial lung disease include prior or concomitant therapy with other antineoplastic drugs known to be associated with interstitial lung disease (taxanes, gemcitabine, vinorelbine, and radiation therapy). The risk of severe pulmonary reactions is higher in patients with pulmonary metastases, comorbidities, and dyspnea at rest, and such patients should not receive trastuzumab. Caution should be exercised, especially in patients receiving concomitant taxane therapy, due to the potential for pneumonitis.
Needles and syringes cannot be reused. Used needles and syringes are placed in a puncture-proof container (capacity). Disposal of trastuzumab and consumables should be in accordance with local regulations.
Studies have not been conducted to study the effect of the drug on the ability to drive a car and operate machinery. If reactions associated with the administration of the drug occur, patients should not drive or operate machinery until symptoms are completely resolved.
Dose adjustment
Reducing the dosage of targeted drugs is not recommended. If toxic complications develop, treatment is stopped and resumed after the patient’s condition normalizes. If there is a need to discontinue trastuzumab, pertuzumab is also discontinued.
If bone marrow suppression develops during chemotherapy, treatment is continued, but it is necessary to monitor the development of complications that are associated with myelosuppression and neutropenia in particular (infectious complications).
If infusion reactions develop, reduce the rate of drug administration or temporarily stop the procedure.
If anaphylaxis develops, treatment is immediately stopped and the question of its cancellation is raised.
Side effects
Because pertuzumab is used only in combination with other drugs, it is difficult to determine the effect of each individual drug on the development of a particular complication. Nevertheless, there were some.
The most common complications that developed in more than 30% of patients:
- Diarrhea.
- Hair loss.
- Nausea.
- Prostration.
- Vomit.
- Decrease in the number of leukocytes.
- Severe neutropenia with fever was observed in 10% of patients. There were even deaths recorded.
Very common complications that occurred in more than 1/10 cases:
- Anemia.
- Infusion reactions.
- Loss of appetite, distortion of taste perception.
- Insomnia.
- Headache, dizziness.
- Paresthesia and peripheral neuropathies.
- Tearing.
- Bleeding (mostly nasal).
- Cough.
- Dyspnea.
- Stomatitis.
- Constipation.
- Rash.
- Skin itching.
- Nail damage.
- Vaginitis.
- Rhinitis.
- Edema.
- Pain in various locations, including muscles and joints.
Frequent complications that developed in less than 1/10 cases and more than 1/100 cases:
- Hypersensitivity reactions.
- Impaired left ventricular function.
- Paronychia.
- URT (upper respiratory tract) infections.
- Chills.
Uncommon complications that occurred in less than 1/100 and more than 1/1000 cases:
- Congestive heart failure.
- Development of pleural effusion.
- Development of interstitial lung disease.
Rare complications that occurred in less than 1/1000 cases:
- Anaphylactic shock.
- Cytokine release syndrome.
- Tumor lysis syndrome.
Trastuzumab
Infusion-related reactions: During the first infusion, chills, fever, nausea, vomiting, pain, tremors, headaches, cough, dizziness, shortness of breath, hypertonicity, skin rash and weakness often occur; rarely - decreased blood pressure, wheezing in the lungs, bronchospasm, tachycardia, decreased oxygen saturation, respiratory distress syndrome.
From the body as a whole: often - abdominal pain, weakness, chest pain, fever, chills, headaches, peripheral edema, inflammation of the mucous membranes, weight gain, lymphangiectatic edema, influenza-like syndrome; rarely - back pain, infections, neck pain, malaise, weight loss; in some cases - sepsis; the possibility of developing coma has been reported.
From the digestive system: often - diarrhea (27%), nausea, vomiting, constipation, stomatitis, abdominal pain, hepatotoxicity, dyspepsia; Possible pancreatitis, liver failure, jaundice.
From the musculoskeletal system: often - arthralgia, myalgia, pain in the extremities, ossalgia, muscle cramps.
From the skin and its appendages: often - rash, erythema, alopecia, disorder of the nail structure; rarely - itching, sweating, dry skin, acne, maculopapular rash; Dermatitis and urticaria are possible.
From the cardiovascular system: rarely - vasodilation, supraventricular tachycardia, decreased blood pressure, heart failure, cardiomyopathy, palpitations; in some cases - decreased ejection fraction, pericardial effusion, bradycardia, cerebrovascular disorders, cardiogenic shock, pericarditis, arterial hypertension.
From the hematopoietic system: rarely - leukopenia, thrombocytopenia; in some cases - neutropenia, febrile neutropenia, leukemia; a decrease in prothrombin levels is possible.
From the central nervous system and peripheral nervous system: often - paresthesia, hypoesthesia, headache, anorexia; rarely - anxiety, depression, dizziness, drowsiness, lethargy, insomnia, muscle hypertonicity, peripheral neuropathy; in some cases - ataxia, tremor, paresis; meningitis, cerebral edema, and thinking disorders are possible.
From the respiratory system: frequent - cough, shortness of breath, pain in the throat and larynx, nosebleeds, nasal discharge, nasopharyngitis; rarely - suffocation, pharyngitis, rhinitis, sinusitis, impaired pulmonary function, decreased oxygen saturation, pleural effusion; very rarely - bronchospasm, respiratory distress syndrome, acute pulmonary edema, respiratory failure; possible hypoxia, laryngeal edema, pulmonary infiltrates, pneumonia, pneumonitis, pneumofibrosis.
From the urinary system: rarely - urinary tract infections; glomerulonephropathy and renal failure are possible.
From the senses: increased lacrimation, conjunctivitis, deafness.
Allergic reactions: rarely - anaphylaxis, angioedema and anaphylactic shock.
Contraindications for use
- Intolerance to the treatment regimen.
- The need to discontinue trastuzumab.
- LVEF is below 50% (left ventricular ejection fraction).
- A history of congestive heart failure.
- Arterial hypertension that is not controlled by recommended treatment regimens.
- Recovery after myocardial infarction.
- Arrhythmias requiring drug correction while taking pertuzumab.
- Liver failure.
- Pregnancy and breastfeeding.
- Age before adulthood.
Treatment with anthracyclines in a cumulative dosage exceeding 360 mg/m2.
Trastuzumab
Infusion-related reactions:
During the first infusion, chills, fever, nausea, vomiting, pain, tremors, headaches, cough, dizziness, shortness of breath, hypertension, skin rash and weakness often occur; rarely - decreased blood pressure, wheezing in the lungs, bronchospasm, tachycardia, decreased oxygen saturation, respiratory distress syndrome.
From the body as a whole:
often - abdominal pain, weakness, chest pain, fever, chills, headaches, peripheral edema, inflammation of the mucous membranes, weight gain, lymphangiectatic edema, influenza-like syndrome; rarely - back pain, infections, neck pain, malaise, weight loss; in some cases - sepsis; the possibility of developing coma has been reported.
From the digestive system:
often - diarrhea (27%), nausea, vomiting, constipation, stomatitis, abdominal pain, hepatotoxicity, dyspepsia; Possible pancreatitis, liver failure, jaundice.
From the musculoskeletal system:
often - arthralgia, myalgia, pain in the limbs, ossalgia, muscle cramps.
From the skin and its appendages:
often - rash, erythema, alopecia, abnormal nail structure; rarely - itching, sweating, dry skin, acne, maculopapular rash; Dermatitis and urticaria are possible.
From the cardiovascular system:
rarely - vasodilation, supraventricular tachycardia, decreased blood pressure, heart failure, cardiomyopathy, palpitations; in some cases - decreased ejection fraction, pericardial effusion, bradycardia, cerebrovascular disorders, cardiogenic shock, pericarditis, arterial hypertension.
From the hematopoietic system:
rarely - leukopenia, thrombocytopenia; in some cases - neutropenia, febrile neutropenia, leukemia; a decrease in prothrombin levels is possible.
From the central nervous system and peripheral nervous system:
often - paresthesia, hypoesthesia, headache, anorexia; rarely - anxiety, depression, dizziness, drowsiness, lethargy, insomnia, muscle hypertonicity, peripheral neuropathy; in some cases - ataxia, tremor, paresis; meningitis, cerebral edema, and thinking disorders are possible.
From the respiratory system:
frequent - cough, shortness of breath, pain in the throat and larynx, nosebleeds, nasal discharge, nasopharyngitis; rarely - suffocation, pharyngitis, rhinitis, sinusitis, impaired pulmonary function, decreased oxygen saturation, pleural effusion; very rarely - bronchospasm, respiratory distress syndrome, acute pulmonary edema, respiratory failure; possible hypoxia, laryngeal edema, pulmonary infiltrates, pneumonia, pneumonitis, pneumofibrosis.
From the urinary system:
rarely - urinary tract infections; glomerulonephropathy and renal failure are possible.
From the senses:
increased lacrimation, conjunctivitis, deafness.
Allergic reactions:
rarely - anaphylaxis, angioedema and anaphylactic shock.
Use during pregnancy and lactation
The use of pertuzumab in pregnant patients is prohibited, as there is a risk of developing kidney disease, oligohydramnios, and even fetal death (data obtained from animal studies). If treatment is necessary for a nursing mother, it is recommended to stop breastfeeding.
Also, women who take this drug must use reliable contraception for the entire treatment period and for 6 months after it.
The effect of the drug on human fertility has not been studied, but according to animal studies, no effect on the reproductive system was observed.
special instructions
The drug is used only after laboratory confirmation of HER-2 overexpression.
The patient's medical documents must indicate the trade name of the drug and its serial number.
The infusion should be administered with access to an emergency kit and a physician experienced in chemotherapy treatment.
Caution is required when using pertuzumab in patients with impaired LVEF. Before starting therapy, they undergo a study of LVEF function, and then regularly monitor it. If the condition worsens, treatment is canceled until stabilization.
Infusion reactions
This group of reactions included increased body temperature, chills, loss of strength, vomiting, and headache. If such reactions develop, it is necessary to reduce the rate of administration of the drug and even interrupt it, if necessary. The patient is monitored until symptoms resolve. If the drugs are well tolerated, the patient should be under the supervision of medical staff throughout the entire infusion and for an hour (in the case of the first administration of the drug) or half an hour (for repeated bites).
If severe infusion reactions develop, the issue of discontinuing this type of antitumor treatment is considered.
Hypersensitivity reactions and anaphylaxis
Cases of death following an anaphylactic reaction to pertuzumab have been observed. In this regard, the drug is administered only if an emergency first aid kit is available. If anaphylaxis develops, assistance must be provided immediately. Further treatment with pertuzumab is contraindicated.
Febrile neutropenia
Febrile neutropenia may occur in patients receiving targeted therapy with docetaxel. The highest risks are during the first 3 courses. Most often, this complication developed in patients against the background of diarrhea and mucositis. In this regard, symptomatic treatment of these phenomena is recommended.
Description of the drug TRASTUZUMAB
Infusion-related reactions:
During the first infusion, chills, fever, nausea, vomiting, pain, tremors, headaches, cough, dizziness, shortness of breath, hypertension, skin rash and weakness often occur;
- rarely - decreased blood pressure, wheezing in the lungs, bronchospasm, tachycardia, decreased oxygen saturation, respiratory distress syndrome.
- rarely - back pain, infections, neck pain, malaise, weight loss;
- in some cases - sepsis;
- the possibility of developing coma has been reported.
- Possible pancreatitis, liver failure, jaundice.
- rarely - itching, sweating, dry skin, acne, maculopapular rash;
- Dermatitis and urticaria are possible.
- in some cases - decreased ejection fraction, pericardial effusion, bradycardia, cerebrovascular disorders, cardiogenic shock, pericarditis, arterial hypertension.
- in some cases - neutropenia, febrile neutropenia, leukemia;
- a decrease in prothrombin levels is possible.
- rarely - anxiety, depression, dizziness, drowsiness, lethargy, insomnia, muscle hypertonicity, peripheral neuropathy;
- in some cases - ataxia, tremor, paresis;
- meningitis, cerebral edema, and thinking disorders are possible.
- rarely - suffocation, pharyngitis, rhinitis, sinusitis, impaired pulmonary function, decreased oxygen saturation, pleural effusion;
- very rarely - bronchospasm, respiratory distress syndrome, acute pulmonary edema, respiratory failure;
- possible hypoxia, laryngeal edema, pulmonary infiltrates, pneumonia, pneumonitis, pneumofibrosis.
- glomerulonephropathy and renal failure are possible.
From the body as a whole:
often - abdominal pain, weakness, chest pain, fever, chills, headaches, peripheral edema, inflammation of the mucous membranes, weight gain, lymphangiectatic edema, influenza-like syndrome;
From the digestive system:
often - diarrhea (27%), nausea, vomiting, constipation, stomatitis, abdominal pain, hepatotoxicity, dyspepsia;
From the musculoskeletal system:
often - arthralgia, myalgia, pain in the limbs, ossalgia, muscle cramps.
From the skin and its appendages:
often - rash, erythema, alopecia, abnormal nail structure;
From the cardiovascular system:
rarely - vasodilation, supraventricular tachycardia, decreased blood pressure, heart failure, cardiomyopathy, palpitations;
From the hematopoietic system:
rarely - leukopenia, thrombocytopenia;
From the central nervous system and peripheral nervous system:
often - paresthesia, hypoesthesia, headache, anorexia;
From the respiratory system:
frequent - cough, shortness of breath, pain in the throat and larynx, nosebleeds, nasal discharge, nasopharyngitis;
From the urinary system:
rarely - urinary tract infections;
From the senses:
increased lacrimation, conjunctivitis, deafness.
Allergic reactions:
rarely - anaphylaxis, angioedema and anaphylactic shock.