Pharmacological properties of the drug Urotol
Pharmacodynamics. Tolterodine is a competitive antagonist of cholinergic muscarinic receptors localized in the bladder and salivary glands. Blocking these receptors causes a decrease in the contractile function of the bladder and a decrease in salivation. Animal studies have demonstrated selectivity of tolterodine for bladder receptors compared to salivary gland receptors. A significant effect of tolterodine on bladder function has been demonstrated in healthy volunteers. After using 6.4 mg of the drug, incomplete emptying of the bladder, an increase in the amount of residual urine and a decrease in detrusor pressure were noted. After oral administration, tolterodine is metabolized in the liver to form a 5-hydroxymethyl derivative, which is the main pharmacologically active metabolite. This metabolite has pharmacological properties similar to tolterodine and, in individuals with active metabolism, contributes to a significant increase in the effect of the drug. The maximum therapeutic effect of tolterodine develops after 4 weeks of use. Both tolterodine and its 5-hydroxymethyl derivative are highly specific for M-cholinergic receptors and do not have a significant effect on other types of receptors. Pharmacokinetics. Tolterodine is rapidly absorbed after oral administration. Its concentration in blood serum reaches its maximum level 1–3 hours after application. The maximum serum concentration increases in proportion to the dose in the range of 1–4 mg. Tolterodine is primarily metabolized by the polymorphic enzyme CYP 2D6, which causes the formation of a pharmacologically active 5-hydroxymethyl metabolite. The systemic clearance of tolterodine in persons with increased metabolism is about 30 l/h, and the final half-life is 2–3 hours. In persons with reduced metabolism (low CYP 2D6 activity), tolterodine undergoes dealkylation by CYP 3A isoenzymes, resulting in the formation of N-dealkylated tolterodine . This metabolite has no pharmacological activity. Reduced clearance and prolongation of the half-life (about 10 hours) of the parent substance in persons with reduced metabolism causes an increase in the concentration of tolterodine in the blood (approximately 7 times) against the background of concentrations of the 5-hydroxymethyl metabolite that cannot be determined. As a result, the exposure (AUC value) of unbound tolterodine in individuals with reduced metabolism of the drug is close to the sum of exposures of unbound tolterodine and its 5-hydroxymethyl metabolite in patients with high CYP 2D6 activity at the same dosage. The safety, tolerability and clinical effect of the drug are the same regardless of the phenotype. Equilibrium concentration in blood plasma is achieved within 2 days. The absolute bioavailability of tolterodine is 65% in poor metabolizers (low CYP 2D6 activity) and 17% in advanced metabolizers (most patients). Concomitant ingestion of food does not affect the exposure of unbound tolterodine and its active 5-hydroxymethyl metabolite in hypermetabolizers, although tolterodine levels are increased when taken with food. There are also no clinically significant changes observed in individuals with low metabolism of the drug. Tolterodine and its 5-hydroxymethyl metabolite bind predominantly to the orosomucoid. Their unbound fractions are 3.7 and 36%, respectively. The volume of distribution of tolterodine is 113 L. After using labeled [14C] tolterodine, about 77% of the radioactivity is excreted in the urine, and 17% in the feces. Less than 1% of the dose is excreted unchanged, and about 4% is excreted as the 5-hydroxymethyl metabolite. The carboxylated metabolite and its corresponding dealkylated metabolite account for about 51 and 29% of the amount excreted in the urine, respectively. Exposure to unbound tolterodine and the 5-hydroxymethyl metabolite increases approximately 2-fold in patients with liver cirrhosis.
Use of the drug Urotol
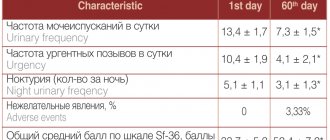
The recommended dose is 2 mg 2 times a day, with the exception of patients with impaired liver and kidney function (glomerular filtration rate ≤30 ml/min), for whom a dose of 1 mg 2 times a day is recommended. If side effects occur, the dose should also be reduced to 1 mg 2 times a day. The course of treatment is 6 months. After 6 months, the need for further treatment should be assessed. The drug is used regardless of food intake. The tablet should be swallowed whole, without chewing, with a sufficient amount of neutral liquid.
Colposuspension according to Birch
It consists of suspending the tissues surrounding the urethra to the strong structures of the anterior abdominal wall - the inguinal ligaments (Cooper). The operation is performed via abdominal access (through the abdomen). Surgical approach: either open or laparoscopic. For a long time, this operation was considered! "gold standard" in the treatment of stress urinary incontinence in women.
With the advent of operations to install a synthetic midurethral sling, Birch colposuspension lost its position.
Its long-term effectiveness “in capable hands” is up to 70-80 percent. The main disadvantages of this technique are: the need for anesthesia with artificial ventilation and the strong dependence of the results on the qualifications of the surgeon.
Side effects of the drug Urotol
Tolterodine may cause mild to moderate M-anticholinergic effects, such as dry skin and mucous membranes, dyspepsia and decreased lacrimation. Immune system: allergic reactions. Mental disorders: increased excitability, impaired consciousness, hallucinations. Nervous system: paresthesia, dizziness, drowsiness. Sense organs: xerophthalmia, visual impairment, including impaired accommodation. Cardiovascular system: tachycardia. Digestive tract: dyspepsia, constipation, abdominal pain, flatulence, vomiting. Kidneys and urinary tract: urinary retention. General manifestations: increased fatigue, headache, chest pain, peripheral edema. Other: very rarely - anaphylactic reactions with angioedema and heart failure. The use of other drugs in this group is sometimes accompanied by palpitation and arrhythmia.
Special instructions for the use of the drug Urotol
Caution should be exercised when using tolterodine: in patients with significant obstruction of the urinary outflow tract due to the risk of urinary retention; for obstructive gastrointestinal diseases (pyloric stenosis); for kidney diseases; liver diseases (the dose should not exceed 1 mg 2 times a day); neuropathy; strangulated hernia; risk of deterioration of gastrointestinal motility; in patients with risk factors for prolongation of the QT (hypokalemia, bradycardia, simultaneous use of drugs that prolong the QT ) and heart diseases, such as coronary artery disease, arrhythmia, chronic heart failure. Before starting treatment with the drug, the presence of organic causes of frequent and imperative urge to urinate should be excluded. The drug can cause accommodation disturbances and slow down the reaction rate, therefore, when using the drug, it is undesirable to engage in activities that require a high speed of psychomotor reactions and quick decision-making (driving vehicles, servicing machines and mechanisms, working at heights, etc.).
Introduction of volume-forming preparations (gels) into the submucosal layer of the urethra
The essence of this technique comes down to the formation of peculiar “pillows” under the urethral mucosa (as with the Mantoux test on the skin of the forearm). As a result of the introduction of the gel at several points, the lumen of the urethra narrows, and the prerequisites are created for better urinary retention. This method of treating stress urinary incontinence, especially in older women, is captivating with its “simplicity” - it is performed under local anesthesia, the operation lasts only 5-10 minutes. The operation is usually performed using a cystoscope through the lumen of the urethra. There are techniques that do not even require a cystoscope.
Unfortunately, despite the considerable cost, the effectiveness of this operation is significantly inferior to surgical treatment.
Repeated injections of the drug are often required. It is also not entirely clear how “harmless” the gels used are for the urethra and paraurethral tissues, especially with repeated administrations. However, there are a number of clinical situations where the introduction of gels is indeed preferable.
Interactions of the drug Urotol
Concomitant treatment with active CYP3A4 inhibitors such as macrolide antibiotics (erythromycin and clarithromycin), azole antifungals (ketoconazole, itraconazole and miconazole), and antiprotease agents is not recommended as these drugs may increase plasma concentrations of tolterodine and the risk of overdose. Concomitant treatment with other drugs that have anticholinergic properties may increase the therapeutic effect and undesirable effects of the drug. On the contrary, with the simultaneous use of M-cholinomimetics, the severity of the therapeutic effect of tolterodine may decrease. The effects of prokinetic agents like metoclopramide and cisapride may be reduced by tolterodine. Pharmacokinetic interactions with other drugs metabolized by cytochrome P450 2D6 (CYP 2D6) or CYP 3A4 are possible. However, concomitant treatment with fluoxetine (a strong CYP2D6 inhibitor metabolized to norfluoxetine, which is a CYP3A4 inhibitor) resulted in only a modest increase in total exposure to unbound tolterodine and its equivalent 5-hydroxymethyl metabolite. It does not cause a clinically significant interaction. Clinical studies have demonstrated the absence of interaction of the drug with warfarin and combined oral contraceptives containing ethinyl estradiol/levonorgestrel. A clinical study did not reveal the ability of tolterodine to inhibit the activity of CYP 2D6, 2C19, 3A4 or 1A2.
Overdose of the drug Urotol, symptoms and treatment
The maximum dose of the drug that the volunteers received was 12.8 mg of tolterodine hydrotartrate once. The most pronounced reactions noted in them were disturbance of accommodation and painful urge to urinate. In case of tolterodine overdose, the stomach should be lavaged and activated charcoal should be prescribed. Possible symptomatic treatment for overdose is presented in the table:
Symptoms | Events |
| Severe central anticholinergic effects (eg hallucinations, extreme agitation) | Physostigmine |
| Convulsions, severe agitation | Benzodiazepines |
| Breathing problems | Artificial respiration |
| Tachycardia | β-adrenergic blockers |
| Urinary retention | Bladder catheterization |
| Midriaz | Use pilocarpine eye drops and/or place the patient in a dark room |
Treatment at the VMT MI Clinic. N.I. Pirogov St. Petersburg State University
North-West Center for Pelviperineology (NWTCPP), founded in 2011 on the basis of the Department of Urology of the Clinic of High Medical Technologies named after. N.I. Pirogov St. Petersburg State University, specializes in modern low-traumatic methods of treating stress urinary incontinence (SUI), painful bladder syndrome (interstitial cystitis), overactive bladder (OAB), its leader is Doctor of Medical Sciences, urologist Dmitry Dmitrievich Shkarupa.
Today we have no doubt that the ability to adjust the sling is the cornerstone that was missing to build a clear and effective system for performing sling operations.
Every year, our Center performs more than 600 implantations of an adjustable sling, which has become the standard of care for SUI. The use of this approach made it possible to almost completely eliminate obstructive complications and increase the real (!) effectiveness of the operation to 90%, even in complicated patients.
We consider tracking long-term treatment results to be the most important element of our work. More than 80% of our patients are regularly examined by the Center’s specialists in the late postoperative period. This allows you to see a real picture of the effectiveness and safety of the treatment.
COST OF TREATMENT FOR URINARY INCONTINENCE:
Most patients receive care free of charge as part of compulsory health insurance (compulsory medical insurance).
It is also possible to pay for treatment in cash. The price depends on the volume and complexity of the operation. On average: from 60,000 to 80,000 rubles
(The price includes: surgery, anesthesia, hospital stay, mesh implant and other expenses).
Bibliography
- AskMayoExpert. Female urinary incontinence and voiding dysfunction (adult). Rochester, Minn.: Mayo Foundation for Medical Education and Research. 2016.
- What is urinary incontinence? Urology Care Foundation. https://www.urologyhealth.org/urologic-conditions/urinary-incontinence. Accessed March 18, 2022.
- McAninch JW, et al., eds. Urinary incontinence. In: Smith and Tanagho's General Urology. 18th ed. New York, NY: McGraw-Hill; 2013. https://accessmedicine.mhmedical.com/content.aspx?bookid=508§ionid=41088107. Accessed March 18, 2022.
- South-Paul JE, et al. Urinary incontinence. In: Current Diagnosis & Treatment in Family Medicine. 4th ed. New York, NY: The McGraw-Hill Companies; 2015. https://accessmedicine.mhmedical.com. Accessed March 18, 2022.
- Lukacz ES. Evaluation of women with urinary incontinence https://www.uptodate.com/home. Accessed March 18, 2017.
- Bladder control problems in women (urinary incontinence). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-women. Accessed March 18, 2022.
- AskMayoExpert. Male urinary incontinence. Rochester, Minn.: Mayo Foundation for Medical Education and Research. 2016.
- Bladder control problems in men (urinary incontinence). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-men. Accessed March 18, 2022.
- Gameiro SF, et al. Electrical stimulation with non-implanted electrodes for overactive bladder in adults. Cochrane Database of Systematic Reviews. https://onlinelibrary.wiley.com/doi/10.1002/14651858.CD010098.pub4/full. Accessed March 18, 2022.
- Jelovsek JE. Surgical management of stress urinary incontinence in women: Choosing a primary surgical procedure. https://www.uptodate.com/home. Accessed March 18, 2022.
- Frawley J, et al. Complementary and conventional health-care utilization among young Australian women with urinary incontinence. Urology. 2017;99:92.
- Mo Q, et al. Acupuncture for adults with overactive bladder: A systematic review protocol. BMJ Open. 2015;5:1.
- Solberg M. A pilot study on the use of acupuncture or pelvic floor muscle training for mixed urinary incontinence. Acupuncture Medicine. 2016;34:7.
- Vinchurkar AS, et al. Integrating yoga therapy in the management of urinary incontinence: A case report. Journal of Evidence-Based Complementary & Alternative Medicine. 2015;20:154.
- Brown A.Y. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Jan. 24, 2022.
- Ziegelmann MJ, et al. The impact of prior urethral sling on artificial urinary sphincter outcomes. Canadian Urological Association Journal. 2016;10:405.
- Linder BJ, et al. Autologous transobturator urethral sling placement for female stress urinary incontinence: Short-term outcomes. Urology. 2016;93:55.
- Lukacz ES. Treatment of urinary incontinence in women. https://www.uptodate.com/home. Accessed May 9, 2022.
- American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins - Gynecology and the American Urogynecologic Society. ACOG Practice Bulletin No. 155: Urinary Incontinence in Women. Obstetrics & Gynecology. 2015;126:e66.