Phenylketonuria
(PKU) is a hereditary disorder of the metabolism of amino acids, primarily phenylalanine (PA), which is part of proteins. The substance is involved in protein folding and stabilization of protein structures.
The first symptoms: frequent regurgitation, vomiting, eczema, convulsions, and the smell of mold emanating from the urine and skin. The child may be lethargic or, conversely, hyperactive. He lags behind in psychomotor development, there are signs of mental retardation. The diagnosis can be made in the maternity hospital. All children with phenylketonuria certainly receive the status of “disabled child.”
Treatment of the disease involves following a special low-protein diet that does not contain foods with FA.
Definition of disease
Phenylketonuria is a congenital, genetic pathology that involves impaired hydroxylation of phenylalanine. It is characterized by the accumulation of amino acids and the products of its metabolism in the body, which leads to severe damage to the central nervous system. The disease was first described by the Norwegian doctor I. A. Felling in 1934.
While studying the disease, experts found that a single phenylalanine hydroxylase gene is responsible for the presence of the disease. The first successful treatment was developed and carried out in 1950 in England.
There is no clinic in the neonatal period. The pathology manifests itself in the first six months of a child’s life. Subsequent accumulation of the substance leads to severe developmental disorders. Therefore, it is extremely important to identify the defect immediately after birth and prevent the consumption of foods containing phenylalanine. Later adherence to the diet will not eliminate the resulting disorders, but will not allow the development of new ones.
The pathology is equally common among both sexes. No racial characteristics were identified. A large number of patients are in countries such as China, Türkiye, and Ireland. On average, in Russia every 7 thousandth child is born with phenylketonuria.
Medicines
Photo: saratov24.tv
Sapropterin dihydrochloride
Dosage form: tablets. Available in a dosage of 100 mg (76.8 mg of sapropterin).
Be sure to drink the resulting solution no later than 15 minutes after preparation.
The dose of the drug is calculated based on the patient’s body weight.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Causes of phenylketonuria
There are three types of genetic disorder, the first is considered classic, since it is diagnosed in more than 90% of cases. The second and third are a rarer form of pathology. Symptoms are similar in all types, the disease leads to mental retardation. In the classic form of phenylketonuria, this can be avoided by diet therapy, but atypical variants, unfortunately, cannot be corrected.
- Classic phenylketonuria (type I) is a low production of phenylalanine hydroxylase (PAH), which leads to the accumulation of phenylalanine and its breakdown products in natural body fluids. The pathology is caused by a mutated RAS gene.
- Phenylketonuria type II is a deficiency of dihydropteridine reductase, which prevents the conversion of phenylalanine to tyrosine. Pathology due to mutation of the QDPR gene.
- Phenylketonuria type III is a deficiency of 6-pyruvoyltetrahydropterin synthase, necessary for the synthesis of tetrahydrobiopterin. The pathology is caused by a mutated PTS gene.
All forms of the disease are inherited in an autosomal recessive manner. This means that the genetic defect can be inherited from one of the parents. The gender of the parent and child does not play a role.
Inheritance of autosomal recessive phenylketonutia
If the expectant mother becomes ill with phenylketonuria, the risk of the child inheriting the disease depends on the genotype of the expectant father. If the child's father is not a carrier of the abnormal gene, the child will be born healthy (but will be a carrier). On the other hand, if the child's father carries the PKU gene, the chance of having an affected child is 50%.
It is also very important for pregnant women to follow a diet - too high levels of phenylalanine can lead to defects in the child (heart defects, limb defects or mental retardation).
Classification
Phenylketonuria currently does not have a generally accepted worldwide classification. There is ongoing debate over this issue, as well as research into the disease. A little earlier, before deciphering genes, it was believed that the degree of damage to intellectual abilities depended on the degree of enzyme activity. Therefore, the current qualification is considered outdated. It also does not take into account other symptomatic factors.
When diagnosing they put:
- Type I (PAH deficiency) - FA concentration is more than 20 mg/dl.
- The average form of PKU is FA from 8.1 to 20 mg/dl.
- Mild form of HPA level - FA from 2.1 to 8.0 mg/dl.
At levels up to 8.0 mg/dL, phenylketonuria is considered benign. It does not require special treatment, but observation is necessary for the first year of the child’s life. The condition is monitored by a pediatrician, neurologist, and geneticist.
There is also another form of phenylketonuria that does not require correction. This is a transient form of HPA during the neonatal period. Occurs, as a rule, with prematurity, which is due to the functional immaturity of the body. Transient phenylketonuria is a temporary increase in FA levels that can rise to critical values. In this case, there is no clinical manifestations or the manifestations are very minor. After a few months, biochemical parameters returned to normal.
Pathogenesis
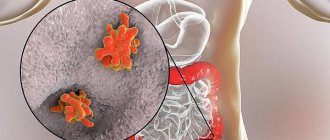
The mechanism of the origin and development of phenylketonuria is associated with a violation of the metabolism of an organic compound - the amino acid phenylalanine. The metabolic block prevents the conversion of phenylalanine to tyrosine. The amino acid not only is not converted, but accumulates in the form of toxic metabolites:
- phenyllactic acid;
- phenylpyruvic acid;
- phenylacetic acid;
- phenylethylamine and so on.
The accumulation of phenyl substances has a toxic effect on the central nervous system. At the moment, the mechanism has not yet been fully studied; doctors do not know the pathogenesis of brain dysfunction.
There are suggestions that damage to the nervous system is the result of a number of factors. Among them are both the direct toxic effects of phenylalanine and disruption of the metabolism of proteins, lipoproteins and glycoproteins, failure of homonal metabolism and membrane transport of amino acids. All this together is important for the maturation and proper functioning of the central nervous system.
Symptoms
Type I The first signs in a child appear between the ages of 2 months and six months.
- Apathy or, conversely, increased irritability.
- Lack of interest in the environment, people, objects, settings.
- Frequent regurgitation.
- Allergic dermatitis.
- Violation of muscle tone.
- Low pressure.
- Cramps.
- Sometimes microcephaly (small size of the skull relative to other parts of the body) and hydrocephalus (excess fluid surrounding the brain) develop.
Characteristic symptoms include hypopigmentation of the skin, hair, and iris. Urine has a specific musty smell or is also called a “mouse” smell. Epileptic seizures are observed in half of the patients and are often the first pronounced clinical symptom. The attack is characterized by “salaam” convulsions, reminiscent of nodding. They occur frequently and do not respond well to anticonvulsant treatment.
If PA concentrations are not adjusted, the disease progresses. As a rule, the IQ level in such children does not exceed 20, with the norm being 85. Mental retardation is so severe that there are no emotional reactions, psychopathy and schizophrenia-like disorders are observed.
Type II The first symptoms appear in the first year of life.
- Increased excitability.
- Developmental delay.
- Profuse drooling.
- Reduced blood pressure.
- Frequent increase in body temperature.
- Tendon hyperreflexia (increased reflexes) or spastic tetraparesis (weakness of all four limbs).
- Myoclonic epilepsy (generalized seizures, predominantly occurring upon awakening).
- Microcephaly.
A distinctive feature of the second type is the death of neurons, disruption of folate metabolism, as well as calcification in various parts of the brain. The disease progresses rapidly and can lead to the death of a child within 2 to 3 years.
III type. Symptoms of pyruvoyltetrahydropterin synthetase deficiency are similar to those of Parkinson's disease:
- Postural instability and gait difficulties. It is difficult or impossible to maintain a certain position of the whole body or limbs.
- Hypokinesia (low motor activity, limited tempo and range of movements).
- Hypersalivation (increased salivation).
- Swallowing disorders.
- Oculogyric crisis (symmetrical deviation of both eyes, usually directed upward).
In 80% of cases, this type of disease is accompanied by a decrease in the amount of biogenic amines in the cerebrospinal fluid. Treatment is complicated by the fact that an early decrease in FA concentration can cause serious pathological changes. Failure to comply with diet therapy will lead to slower speech development, low intelligence, and memory problems.
Diagnostics
Phenylketonuria can be detected in the first days after birth before any symptoms appear. To determine the concentration of phenylamine in the blood, carry out:
- microbiological test;
- chromatography;
- fluorimetry;
- mass spectrometry.
In all cases, the biological material is dry spots of capillary blood from the baby.
Recently, testing for phenylketonuria has been included in the neonatal screening program. It is carried out on all newborns; the study is especially important for premature babies. The diagnostic criterion is an increased concentration of phenylalanine at a rate of 0 - 2 mg/dl. An elevated level requires further diagnostic testing. It will be necessary to establish the very fact of the presence of phenylketonuria and identify its cause.
- If the screening test shows high PA level results, the following may additionally be prescribed:
- Phenylalanine load diagnostics to identify the nosological form of the disease.
- Molecular genetic analysis to determine the form: classical, type II or III.
- Sequencing of the RAS gene, if molecular genetic diagnostics gave a negative result for the PAH gene.
- Analysis for pterins in urine to exclude pterin-dependent forms.
Differential diagnosis of phenylketonuria is carried out with such pathologies as liver dysfunction, galactosemia and other diseases.
Treatment
Symptomatic therapy for any form of phenylketonuria is ineffective. There is only one way to prevent the negative consequences of the disease - diet therapy. High-protein foods and phenylalanine-containing foods are excluded from the diet. The missing amount of protein is replenished with specialized therapeutic nutrition, with the lowest possible content of the amino acid FA or completely devoid of it. It should be taken into account that the effectiveness of therapy directly depends on the time the correction began and the pathological changes that have already occurred.
The goal of therapeutic nutrition in the classic form of the disease is to prevent the development of disorders of the central nervous system, physical and mental development. A mild form of HFA allows for an expansion of the diet under the strict supervision of a doctor over the child’s condition and biochemical parameters. Prohibited: meat, fish, nuts, chocolate and legumes, all types of eggs, cottage cheese and cheeses. You should also avoid foods that contain the artificial sweetener aspartame.
The criterion for the effectiveness of treatment is the level of FA in the blood.
Folk remedies
Photo: vestiregion.ru
Diet therapy is a treatment method that comes from traditional medicine. Through trial and error, it was found that excluding foods containing high amounts of protein from the diet of children with certain symptoms alleviated their condition. To alleviate some neurological symptoms (irritability, anxiety), it is possible to use decoctions of chamomile, mint, lemon balm, and hawthorn.
The disease in question requires constant monitoring of patients by specialists . It is recommended not to neglect the recommendations of your doctor.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Prognosis and prevention
Carrying out mass screening in maternity hospitals allows for timely identification of genetic abnormalities. Start following diet therapy in a timely manner and, as a result, prevent serious consequences. Otherwise, the prognosis for mental development is unfavorable.
Classic PKU has a favorable prognosis if it is diagnosed in the first weeks of a child’s life and all doctors’ requirements are met. Such children go to regular schools, are able to obtain higher education and lead a normal life.
When preparing for pregnancy, a couple should undergo preliminary genetic testing for the presence of mutations in the RAS gene. If one of the parents has a defective gene, the chance of having a child with PKU is 1:4 and 100% if both parents are sick.
Women with established phenylketonuria should follow a strict diet during pregnancy and breastfeeding. High concentrations of the amino acid in the blood and amniotic fluid have a serious teratogenic effect on the fetus.
During pregnancy
Women with phenylketonuria who have been successfully treated with diet should be extremely careful about their condition while carrying a child, because even with genetically normal fetal development, there is a high risk of disorders due to the increased level of phenylalanine and its metabolites in the mother’s bloodstream as a serious teratogenic factor with neurotropic toxicity. Therefore, before conceiving, such patients are advised to return to a strict diet and stick to it throughout the pregnancy.
A special diet should limit intake to 15-20 mg/kg of phenylalanine per day, while ensuring that essential amino acid .