Published: 07/30/2021 12:45:00 Updated: 07/30/2021
Gilbert's syndrome is the most common form of hereditary pigmentary hepatosis, characterized by impaired bilirubin metabolism due to a genetic defect in microsomal liver enzymes. Often the disease is asymptomatic for many years, but under the influence of provoking factors intermittent jaundice, dyspeptic and asthenovegetative disorders can occur.
Diagnosis requires collecting a family history, laboratory and instrumental studies. In the treatment of Gilbert's syndrome, medications of different groups are used.
Gilbert's syndrome according to the ICD corresponds to code E80.4. Men suffer from this disease four times more often than women. In general, the prevalence of pathology in European and Asian countries does not exceed 5%.
Reasons for appearance
Normally, in humans, during the breakdown of red blood cells, a substance toxic to the body is formed - indirect bilirubin.
It is neutralized by liver cells, which ensure its binding to glucuronic acid and conversion into water-soluble direct bilirubin. Subsequently, this compound is excreted through the organs of the biliary system with feces and urine. The cause of congenital Gilbert's syndrome is a genetic mutation of the microsomal enzyme UDP-glucuronyltransferase, which is responsible for the binding of glucuronic acid to indirect bilirubin. The second mechanism for the development of the disease is considered to be a violation of the uptake of bilirubin by microsomes of the vascular pole of the liver cell and its transport by glutathione-S-transferase. Thus, the concentration of toxic metabolic products in the blood serum increases. As a result, unconjugated bilirubin accumulates in tissues, turning them yellow. Inheritance of the pathology occurs according to an autosomal dominant pattern.
Predisposing factors that provoke clinical manifestations of the disease include:
- unbalanced diet, strict diet or fasting;
- loss of body fluids, dehydration;
- stress, physical fatigue;
- menstrual bleeding;
- infectious processes;
- operations;
- taking alcohol and certain medications.
Frequently asked questions
Why is Gilbert's syndrome dangerous?
Gilbert's syndrome itself does not pose a risk to health and well-being. However, with an increase in the level of free bilirubin, bile secretion may gradually decrease and cholelithiasis, cholecystitis or duodenitis may develop.
Why can't you sunbathe if you have Gilbert's syndrome?
Due to the negative effect of solar ultraviolet radiation on liver function, sunbathing with Gilbert's syndrome is undesirable either in the open sun or in a solarium. There is no direct prohibition, but prolonged sun exposure can activate an increase in unconjugated bilirubin. Therefore, it is advisable to go to the beach for a short time (no more than half an hour) and do this only in the morning or evening hours.
How is Gilbert's syndrome transmitted?
This is a genetic pathology with an autosomal dominant type of inheritance, i.e. if one of the parents has the disease, the child gets the disease in 50% of cases.
Symptoms of Gilbert's syndrome
The first manifestations of Gilbert's syndrome in children begin in adolescence, after 11-12 years, which is associated with the inhibitory effect of sex hormones on the utilization of bilirubin.
However, the onset of the disease can occur much later, up to 30 years. The disease has a wave-like course, that is, it appears only during an exacerbation; in other periods, symptoms of Gilbert's syndrome are completely absent. The following signs are most characteristic of the pathology in question:
- Intermittent jaundice. Localization and severity can vary - from a change in color of only the sclera of the eyeballs to bright yellowness of the skin and mucous membranes throughout the body. The appearance of jaundice is always sudden, occurs after exposure to provoking factors and disappears spontaneously.
- Xanthelasma of the eyelids. Single or multiple yellowish plaques that rise above the skin.
- A feeling of heaviness in the right hypochondrium, a feeling of discomfort in the abdominal cavity. These symptoms are associated with an enlarged liver and spleen, the development of cholecystitis, biliary dyskinesia, and cholelithiasis.
- Asthenovegetative disorders. Due to intoxication of the body, rapid fatigue and depression, sleep disturbances, and excessive sweating appear.
- Dyspeptic manifestations. Loss of appetite, bitter taste in the mouth, nausea, belching, bloating and excess gas, stool disorders.
About 30% of people with Gilbert's syndrome are asymptomatic. Long periods of remission complicate the diagnosis of the pathology, which is why many patients do not know about it.
Gilbert's disease: treatment
Gilbert's syndrome is not a reason to prescribe any specific treatment. A nutritious, high-calorie diet with sufficient fat content is recommended. Drinking alcohol is prohibited, emotional and physical stress, and taking medications that can induce jaundice should be avoided. With frequent episodes of hyperbilirubinemia, phenobarbital is used to treat patients with Gilbert's syndrome, which is prescribed at 0.05-0.1 g 2-3 times a day for 1-2 weeks. Typically, after 7-10 days, the level of bilirubin in the blood decreases to normal.
Diagnosis of Gilbert's syndrome
Making a diagnosis includes an analysis of existing complaints and clinical manifestations of the disease, clarification of the presence of episodes of jaundice and pathology of the hepato-biliary system in close relatives, and the use of laboratory and instrumental research methods.
Differential diagnosis of Gilbert's syndrome is carried out with viral and chronic hepatitis, mechanical and hemolytic jaundice, Crigler-Nayyar syndrome, Dabin-Johnson syndrome and Rotor syndrome, primary shunt hyperbilirubinemia, congenital cirrhosis of the liver, bile duct atresia. The main distinguishing feature of this disorder is an increase in the fraction of unconjugated bilirubin in the blood serum, not associated with hemolysis of erythrocytes, and a hereditary burden.
The standard list of tests when examining for Gilbert's syndrome includes:
- General clinical blood test. In some cases, there is an increase in hemoglobin levels or a decrease in the number of platelets.
- Blood chemistry. The main symptom of the disease is an increase in the concentration of total bilirubin to 34.2–85.5 µmol/l due to its indirect fraction. The values of other liver blood enzymes, such as AST, ALAT, GGTP, alkaline phosphatase, are usually within normal limits. Dysproteinemia and increased total protein concentrations may be present.
- Analysis of urine. Creatinine determination is carried out.
- Determination of markers for viral hepatitis in blood serum. In Gilbert's syndrome, the presence of Ig G to HBcAg, hepatitis A and C is uncharacteristic.
- Coprogram. A stool test for stercobilin for the pathology in question has a negative result. In difficult cases, functional laboratory tests are indicated. A decrease in bilirubin level while taking phenobarbital and its increase by 1.5-2 times after fasting, a low-calorie diet or intravenous administration of nicotinic acid confirms the diagnosis.
If indicated, DNA defects are also determined using the polymerase chain reaction method.
Research in Gilbert's syndrome reveals genetic polymorphism in the DNA fragment encoding the UDPGT enzyme. Of the instrumental methods, ultrasound examination of the abdominal organs is most often performed to exclude other liver pathologies and cholelithiasis. In children, you can use a method for determining the hepatosplenic index using ultrasound data.
Additionally, duodenal intubation and thin layer chromatography are possible. Percutaneous puncture of the liver with subsequent morphological assessment of the obtained biomaterial is performed if the patient is suspected of having chronic hepatitis or cirrhosis of the liver.
Gilbert's syndrome. Current views, outcomes and therapy
00:00
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– In our section “Hepatology”, Professor Reizis Anna Romanovna. Gilbert's syndrome.
Usually it raises a lot of questions.
"Gilbert's syndrome. Current views, outcomes and therapy.”
Ara Romanovna Reizis , professor, doctor of medical sciences:
- Dear Colleagues.
There are diseases that run through a person’s entire life – from childhood and adolescence to the most advanced years. On this path, doctors of various specialties, a very wide range of doctors, come to the attention of doctors. It is important that this wider community is aware of the new developments in our understanding of this disease.
Such diseases include Gilbert's syndrome (GS). More than a century has passed since Augustine Gilbert described this syndrome in 1901. During this time, many new things have emerged in our understanding of this disease. It is in the aspect of this new thing that I would like to present this pathology today.
From our college days we remember what it is. Gilbert's syndrome is a hereditary disorder of bilirubin metabolism, which consists of insufficiency of its glucuronidation (mandatory for its entry into the biliary tract) and, in connection with this, the development of benign unconjugated hyperbilirubinemia.
We also know the set of clinical and laboratory criteria that have always been the basis for our diagnosis. It is known that it is detected mainly in adolescents during prepubertal and pubertal age. Most often in the family we have some evidence of a hereditary family predisposition to this syndrome.
As a rule, the intensity of jaundice is low. Maximum – subicteric skin and icteric sclera. The appearance or intensification of jaundice is often associated with intercurrent diseases or with fasting, physical or psycho-emotional stress. And also with the use of a number of medications. Especially the so-called aglucones, sulfamides, the group of salicylates. We will talk about this a little further in more detail.
Most often, hepatomegaly is absent or insignificant. In laboratory tests, bilirubin increases by 2-5 (rarely more) times due to the predominantly free fraction. With normal transaminase activity and the absence of markers of viral hepatitis and evidence of hemolytic anemia.
This set of clinical and laboratory data was enough for us to diagnose this syndrome.
03:24
Recently, the situation has changed in the sense that we have the opportunity of objective genetic analysis, which confirms or does not confirm this diagnosis.
The genetic face of SG has become known, which lies in the fact that a mutation occurs in the promoter region of the encoding enzyme glucuronyl transferase. It consists of a tyrosine-arginine dinucleotide insertion. This insertion is repeated a varying number of times. Depending on this, we have either the classic version of SG or its variations (alleles).
The possibility of objective confirmation of this diagnosis and its objective formulation has in many ways radically changed our ideas about this syndrome. Changed some myths that have been quite persistent throughout the century that we are familiar with this syndrome.
The first is the prevalence of GS. It was considered to be a fairly rare disease. With the help of a genetic diagnosis, it became obvious that this is a fairly common disease. Between 7% and 10% of the world suffers from GS. This is every tenth. This is an unusual frequency for an inherited disease.
In the African population up to 36%. In our population (European and Asian) 2-5%. In our country and in our population, this diagnosis is becoming more frequent.
(Slide show).
Data from our clinic, where we encounter GS as an object of differential diagnosis of viral hepatitis. Over 20 years, we have (from the 1990s to the present) an increase in the frequency of this diagnosis by more than 4 times.
The second myth, which is becoming a thing of the past with the possibility of genetic diagnosis of GS. It is a myth that GS is, first of all, jaundice. This is a completely unnecessary symptom for GS. This is just the tip, the visible part of the iceberg. The majority of patients with GS do not have jaundice or manifest it in some special life situations. This is not a mandatory symptom at all, which is also very important.
07:10
The third myth with which we must part in our time. The myth is that GS is a completely harmless disease. We are accustomed to the fact that this is the case. It does not lead to fibrosis or transition to cirrhosis of the liver. As such, it does not require our attention.
In fact, it has recently become clear that it makes a very serious contribution to the development and incidence of cholelithiasis (GSD) in the world. In particular, a number of studies speak about this quite extensively.
A genetic study in 2009, where about two hundred patients with cholelithiasis and about 150 patients without it were genetically examined for GS. It turned out with high confidence that among those who have GS, cholelithiasis is significantly more common.
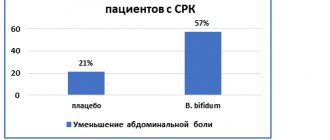
In 2010, an even larger study appeared. This is a meta-analysis of a number of studies. It covers about three thousand patients with cholelithiasis and about one and a half thousand patients without it. It turned out that patients with genetically confirmed GS have a full risk of cholelithiasis. Mainly men have this weld.
Women generally suffer from cholelithiasis more often due to hormonal conditions, estrogens, and so on. Men fall into this category, mainly if they have SG. The increase in cholelithiasis in men with GS occurs by 21%.
Another new direction, a completely new aspect in our modern ideas about lifesaving. This fact is that the study of the characteristics of drug metabolism against the background of GS formed the basis for the emergence of a completely new direction in pharmacology. The so-called pharmacogenetics, which are of great importance for the development of drugs and their practical use.
Many drugs, the so-called aglucones, must also combine with glucuronic acid, like bilirubin, in order to be excreted from the body and generally go through their metabolic path in the body. The same enzyme is loaded - glucuronyl transferase.
Accordingly, bilirubin is displaced from its connection with glucuronic acid. Its excretion into the bile canaliculi is disrupted, resulting in jaundice.
10:57
When developing and testing a number of drugs on a large contingent of patients, pharmacologists were faced with the fact that a number of patients exhibited severe jaundice. This could be interpreted as true hepatotoxicity of the drug, which sometimes cast a shadow on very important and promising drugs that are essential for the corresponding category of patients.
A 2011 paper shows how, in a trial of Tocilizumab, a promising drug used for rheumatoid arthritis, two patients had high bilirubin levels. When these patients were examined, it turned out that both of these patients (and only them of all those participating in the trial) had a genotype characteristic of GS.
This removed this drug from suspicion in terms of true hepatotoxicity.
But the number of relevant publications is increasing. Here is another indication of this. With a disease such as acromegaly, resistance to somatostatin is now common. The new drug that was tested showed a high degree and high incidence of jaundice. It turned out that all these patients had GS.
An example much closer to us is the antiviral therapy of chronic hepatitis C with interferons with Ribavirin. It's the same picture. Two patients showed a 17-fold increase in bilirubin levels. But it turned out that these two patients had GS. O led to the normalization of bilirubin. No additional shadow was cast on Ribavirin.
Until now, we have been talking mainly about data from world literature. I would like to provide my own data for 20 years of the children’s clinic. During this time, we observed 181 children and adolescents with GS. It turned out that a very high percentage of these patients (more than half of them) had biliary dyskinesia with and without sludge syndrome, and developed cholelithiasis, despite the fact that these were children.
But we received especially important and interesting information when we divided our patients into two groups, into two decades: 1992–2000 and 2001–2010. These decades were different in that at the first stage they did not receive Ursodeoxycholic acid drugs. Or we received it according to indications when we already had a developed picture of damage to the biliary tract.
In these patients, only 11.8% of children had a normal state of the biliary tract. 76.5% had biliary dyskinesia, almost half of them with sludge syndrome. Almost 12% of children have already developed cholelithiasis.
15:40
In the second stage (second decade) there are 105 patients. Already from the first steps, as soon as the diagnosis of GS was made, preventive courses of Ursodeoxycholic acid (UDCA) were carried out twice a year in the form of the drug Ursosan, with which we have been working for many years.
Results. In almost 65% of cases, these patients have a normal condition of the biliary tract. The number of patients with cholelithiasis decreased by 4.5 times (to 2.8%).
This suggests that GS still deserves our attention and some therapeutic influence. It is aimed at reducing the total level of bilirubin, as indirect, free to reduce general intoxication (since indirect bilirubin is toxic to the nervous system). As well as reducing direct conjugated bilirubin to prevent damage to the biliary tract.
What do we have for this today? In terms of reducing the level of indirect bilirubin, the drug Phenobarbital is still used. It is known that it has some ability to increase the activity of glucuranyl transferases. Thanks to this, the level of indirect hyperbilirubinemia is reduced to some extent and intoxication and the effect on the central nervous system (CNS) are reduced.
In order to reduce or prevent damage to the biliary tract, we consider it correct to use UDCA (Ursosan, in particular). According to our data, it significantly reduces or even prevents complications from the biliary tract, including cholelithiasis.
18:17
(Slide show).
There is an arrow here from UDCA to a decrease in the effect on the central nervous system. We came across some interesting data from experimental studies so far. They say that UDCA can reduce the sensitivity of nerve cells to the damaging effects of indirect bilirubin.
Cultures of rat nerve cells (astrocytes and neurons) were incubated with indirect bilirubin or with indirect bilirubin in the presence of UDCA. In the case of mono incubation, there was a 4- to 7-fold increase in apoptosis in these cells.
When they were incubated with indirect bilirubin in the presence of UDCA, there was significant protection (60%). Reduction in apoptosis level less than 7%.
Thus, the treatment of GS today, as it seems to us, should contain. As for dietary restrictions, they can only be associated with possible folate and be of this nature. They shouldn’t be strict enough, but they are part of a healthy lifestyle.
As for the second point - the sparing regime - it is very important. Patients should be well aware of this. Physical and psycho-emotional overstrain is extremely unfavorable and will directly lead to yellowing.
A very important point is medication sparing - minimizing medicinal effects in all areas. First of all, this applies to glucocorticosteroids, which are direct aglucones. Salicylates - the whole group. Sulfonamides. “Diacarb”, quite often used. “Menthol” (“Mentholum”) and a number of other drugs.
In general, the banner of a patient with GS should read: “Minimize drug exposure.”
As for drug therapy for the syndrome itself, Phenobarbital in an age-specific dosage is used only in cases of high bilirubin elevation (above five or more norms). For a lower level of bilirubin rise, use Valocordin, which contains phenobarbital in small quantities. For children or adolescents, 1 drop per year of life, 20 - 30 drops for adults 3 times a day.
As for UDCA, 10 – 12 mg per kilogram per day. Preventive courses of 3 months (spring-autumn) are useful annually and, as I have shown in our experience, are quite effective in preventing damage to the biliary tract and cholelithiasis.
Indicated when direct bilirubin increases until it normalizes. If biliary dyskinesia occurs with sludge syndrome before eliminating it and 1-2 months after to maintain the result.
22:24
Thus, GS is a hereditary disorder of bilirubin metabolism, the timely recognition and correction of which is essential, both for the patient and for the population as a whole.
The modern stage of development of medicine, which has made it possible to objectively confirm the diagnosis of GS using genetic methods, puts its diagnosis at a new level.
The benign nature of the syndrome, consisting in the absence of fibrosis and outcome in cirrhosis of the liver, does not exclude such adverse consequences as diseases of the biliary tract, including cholelithiasis.
Last thing. To prevent and treat these adverse effects, it is advisable to use UDCA, in particular Ursosan.
Thank you for attention.
Treatment of Gilbert's syndrome
The mere presence of Gilbert's syndrome in children and adults is not an indication for drug treatment.
To prevent exacerbation of the disease and the development of complications, general measures are important: limiting participation in strenuous sports, prolonged exposure to the sun, consumption of alcoholic beverages and hepatotoxic drugs. Such patients need to eat right, avoid prolonged fasting, as well as foods containing indigestible fats - fatty meats, fried and spicy foods, canned foods. During an exacerbation of the clinical manifestations of the disease, plenty of fluids and a gentle diet corresponding to table No. 5 are prescribed. Conservative therapy during this period is aimed at reducing the formation and accelerating the removal from the body of excess amounts of unconjugated hemoglobin and includes:
- taking microsomal enzyme inducers (phenobarbital, zixorine);
- taking activated carbon;
- phototherapy.
For the prevention of cholecystitis and cholelithiasis in Gilbert's syndrome, the use of choleretic herbs, hepatoprotectors (ursosan, ursofalk), essential phospholipids, choleretics (cholagol, allochol, holosas) and B vitamins is recommended.
Causes
The cause is a genetic disorder, and provoking factors include:
- Infections, colds.
- Emotional and physical stress.
- Vomit.
- Errors in diet and fasting.
- Drinking alcoholic beverages.
- Drug loads ( ampicillin , chloramphenicol , glucocorticoids, vitamin K , caffeine , paracetamol , rifampicin , anabolic steroids, androgens , salicylates ).
- Various operations.
- Trauma.
- Excessive influence of insolation.
- Premenstrual syndrome.
- Poor sleep, lack of sleep.
Prognosis and prevention
The prognosis of the disease at any age is favorable.
Hyperbilirubinemia in Gilbert's syndrome persists for life, but is benign in nature, is not accompanied by progressive changes in the liver and does not affect life expectancy. Source of statistical data: Visual pediatric gastroenterology and hepatology: textbook. allowance — Kildiyarova R. R., Lobanov Yu. F. 2013. — 124 p. : ill. (Chapter 6. Liver diseases (vmede.org).
Author:
Pugonina Tatyana Alekseevna, Therapist
Prevention
Parents who have had a child with this disease should definitely consult and be examined by a geneticist before planning their next pregnancy. This also applies to married couples planning to have children if their relatives are diagnosed with this syndrome.
To prevent exacerbations, it is important for the patient to:
- Compliance with the diet and quality of nutrition.
- Dietary food within table No. 5.
- Moderate physical activity without overload.
- Compliance with the work and rest regime.
- Hardening and a healthy lifestyle.
- Sanitation of chronic foci of infection.
- Treatment of pathology of the biliary tract.
- Rational use of medications. This primarily concerns the intake of glucocorticoids, anabolic steroids, Rifampicin , Streptomycin , Cimetidine , Levomycetin , Ampicillin , caffeine , paracetamol , diacarb .
- Consumption of alcoholic beverages is prohibited.
- Conducting preventive courses of ursodeoxycholic acid for biliary sludge .
Treatment of pathology
Treatment of Gilbert's syndrome involves reducing physical and psycho-emotional stress, diet therapy and drug support. To lower the level of bilirubin in the bloodstream, a comprehensive therapeutic approach is required.
The doctor recommends not going to the gym, giving up alcohol, limiting time spent in the open sun, and also stops taking hepatotoxic drugs.
The athlete must strictly control the load, otherwise progression of the disease cannot be avoided. It is regularly required to undergo preventive examinations to analyze the activity of the pathological process. Even during remission, sports activities should be carried out in a gentle manner.
Another contraindication for young men with Gilbert's disease is military service. According to the order of the Ministry of Defense, the place and conditions for its holding are separately specified for conscripts. The army and sports can be present in a man’s life, but in a strictly limited volume and with a specially selected regime.
Medication
To reduce the amount of pigment in the bloodstream, you must take the following medications:
- enzyme inducers, such as phenobarbital, zixorin, whose action is aimed at reducing the amount of bilirubin;
- sorbents (atoxyl, polysorb) necessary to accelerate the excretion of pigment in feces.
For preventive purposes, to prevent exacerbation of pathology, the following are recommended:
- hepatoprotectors (Essentiale, Karsil) to protect liver cells;
- choleretics (allochol) stimulate the formation of bile;
- cholekinetics (holosas) have a choleretic effect and facilitate outflow;
- B vitamins
Of the physiotherapeutic procedures, preference is given to phototherapy, which helps reduce the yellowness of the skin. Another possible method of influencing pathology is unconventional treatment. The folk approach involves taking decoctions based on choleretic plants, as well as using herbal baths. The recipe may include rose hips, corn silk, milk thistle, calendula and immortelle.
Diet for Gilbert's syndrome
In case of exacerbation of the disease, a diet is prescribed that corresponds to table No. 5. Meals should be fractional (up to six times a day), in small portions. Every day you should drink at least one and a half liters of liquid (non-acidic compotes, herbal tea, rosehip decoction).
The prohibited list of foods includes fatty, fried foods, hot spices, legumes, sorrel, coffee, soda, baked goods and chocolate. Daily calorie content should not exceed 2800 kcal. Vegetable fats, low-fat fish, milk and vegetables (pumpkin, potatoes, carrots) are recommended.
Dishes must be pureed and served warm.
Example of table menu No. 5:
| Eating | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Breakfast | protein omelette, porridge (rice), optional with milk, with 5 g of butter, weak tea with a slice of lemon | meat cutlets with milk sauce, fresh salad (apples/carrots, grate), weak coffee with milk | low-fat cottage cheese with 60 gr. sour cream, light tea, oatmeal with milk | tea with milk, pasta, ground beef | light coffee with milk, homemade cottage cheese, buckwheat without milk | weak tea, meat cutlets, buckwheat (boil) | light tea, rice, a piece of herring soaked in milk |
| Lunch | cottage cheese casserole | apple | baked apple | lazy dumplings | apple | carrot puree, apple jam | rosehip decoction |
| Dinner | vegetable soup (mash vegetables), soufflé (boiled meat), carrots (stew), compote | potato soup, berry jelly, piece of boiled fish | piece of boiled chicken, side dish (boiled rice), vegetable soup, compote of ground dried fruits | cabbage rolls, a glass of jelly, vegetable soup (grind potatoes) | pasta, borscht in water, jelly, soufflé (boiled meat) | compote, curd pudding, milk soup with noodles | pasta, soup (cereals, vegetables), milk sauce, steamed meat cutlets, compote |
| Afternoon snack | tea with cookies | rosehip decoction with cookies | fruits | kefir | tea with jelly cookies | cookies, kefir | |
| Dinner | vermicelli with cheese, still mineral water | buckwheat, still mineral water | steamed fish cutlet, mashed potatoes, rosehip broth, milk sauce | tea, cheese, rice milk porridge with 6 gr. oils | piece of boiled fish, mashed potatoes, fresh vegetable salad, mineral water | semolina porridge with milk, mineral water | steamed protein omelette, mineral water, cheesecakes |
Is homeopathy effective?
Treatment for Gilbert's disease may include homeopathy. Hepel is often prescribed. The drug has a hepatoprotective effect, protects liver cells from the aggressive effects of environmental factors.
In addition, homeopathy has choleretic, anti-inflammatory and antispasmodic effects. The drug is produced in tablet form for sublingual absorption (under the tongue). It is prescribed to restore liver function in cases of cholestasis, cholecystitis, cholelithiasis and hepatitis.
Contraindications include individual intolerance to the components of the drug. The tablet should be dissolved three times a day half an hour before meals.
Forecast
The disease is incurable, but if medical recommendations are followed, the pathology does not bother the person and does not reduce the quality of life. Dietary nutrition and avoidance of alcohol allow you to control the activity of the pathological process and prevent the development of complications. In addition, do not forget about regular preventive examinations.
If medical recommendations are followed, the pathology does not bother the person and does not reduce the quality of life. If you ignore the advice of a specialist and do not pay attention to the symptoms of the disease, in the near future you should expect the appearance of clinical signs of hepatitis or cholelithiasis.
What is bilirubin?
Bilirubin is the main blood indicator if we are talking about Gilbert's syndrome. It's time to talk about what it is. It is a pigment that is the end product of heme metabolism. Heme is part of hemoglobin (Hb), a protein responsible for transporting oxygen in the blood. The largest amount of hemoglobin is found in red blood cells. The latter circulate in the blood for 120 days, after which they are destroyed in the spleen. Hemoglobin is broken down into heme and globin (a protein compound). The body can reuse the protein, but the heme is recycled. At the same time, it undergoes enzymatic transformation first into biliverdin (green pigment), and then into bilirubin (orange pigment). Next, the resulting bilirubin is transported in combination with albumin (blood transport protein) to the liver.
Bilirubin is a toxic fat-soluble substance in high concentrations that can accumulate in tissues, so the body disposes of it as waste. To reduce toxicity and remove this compound from the body, it must first be neutralized. For this procedure, the liver contains an enzyme that can convert fat-soluble bilirubin (indirect, unconjugated) into water-soluble (direct, conjugated). The latter is included in the composition of bile and leaves the body through the gastrointestinal tract.
Figure 2. Metabolism of bilirubin. Image: Sakurra/Depositphotos