It is necessary to distinguish physiological anovulation from pathological.
- Physiological is considered a violation of the maturation and release of the egg from the follicle during puberty, during pregnancy, lactation and menopause. In addition, ovulation does not occur 1-2 cycles a year, since the ovaries need rest.
- Pathological anovulation occurs with various diseases and hormonal disorders. The dominant follicle does not develop or burst, as it should normally, but regresses and turns into a cyst. The egg does not enter the abdominal cavity, therefore, fertilization and pregnancy are impossible.
Causes
Only a specialist can identify the causes of anovulation after a thorough examination, these include:
- pathologies of the hypothalamic-pituitary system (dysfunction, pituitary tumors, vascular disorders), often accompanied by hyperprolactinemia, hyperandrogenism;
- gynecological diseases (inflammation of the appendages, polycystic disease, endometriosis);
- diseases of the endocrine glands (thyroid);
- obesity;
- uncontrolled use of hormonal drugs, including contraceptives;
- stress;
- liver diseases, in which the synthesis of transport proteins and hormone metabolism are disrupted;
- vitamin deficiencies;
- anorexia;
- intoxication;
- genetic developmental pathologies;
- early menopause
Anovulation is only a sign of the disease, so adequate treatment is possible after determining its cause.
What can be the prognosis after treatment of anovulatory cycles?
It is very important to correctly develop a course of treatment for anovulatory cycles. After completing it fully, about 40% of women suffering from the disease can successfully conceive, bear and give birth to a child.
A woman should be very careful and careful about her health. Self-care should be accompanied by good nutrition, rational distribution of working time and rest periods. Every woman should make regular visits to a gynecologist to check the health of her genitals, take care of protection from fungi, and avoid infection with toxins.
Symptoms
During anovulation, women usually turn to a gynecologist if they cannot get pregnant for a long time, but they can suspect that ovulation is not happening based on a number of signs.
The symptoms of anovulation are as follows:
- the menstrual cycle is disrupted, the quality of menstruation has changed, the interval between them has changed, or they are completely absent;
- discharge does not change throughout the cycle, although normally it thins out after ovulation;
- the condition of the skin and hair has worsened;
- there is no rise in rectal temperature indicating ovulation;
- negative ovulation test.
With such signs, you need to visit a gynecologist.
Symptoms and diagnostic methods
Typical pathogenesis of the anovulatory cycle
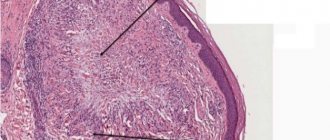
In the ovaries, during the anovulatory cycle, periods of development and degradation of the follicle vary in duration and characteristics. The anovulatory cycle is characterized by an oversaturation of the action of estrogen, which must fall under the influence of the gestagenic hormone progesterone, which does not happen during the anovulatory cycle. In very rare situations, the anovulatory cycle is comparable to hypoestrogenism.
The development of the level of estrogenic influence affects the endometrium of various types.
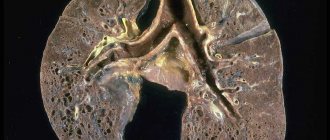
Atresia of the follicle becomes the cause of hormonal imbalance, and this already becomes the reason for the development of the anovulatory cycle and the cause of such menstrual bleeding. During each anovulatory cycle, the endometrium begins to exhibit functional failures, and the anovulatory cycle will therefore be accompanied by hemorrhages, extravasations, and necrosis. The uppermost layers of the endometrium are quite unstable and often disintegrate, which causes bleeding, but in the absence of independent endometrial rejection, the development of bleeding is accompanied by diapedesis of red blood cells. At times, hyperestrogenism does not decrease and the excretion of estrogen in the urine remains quite stable throughout the current anovulatory cycle.
When menstrual function matures in puberty, the cause of the anovulatory cycle may be the lack of the required ratio of luteinizing and luteotropic hormones, the synthesizing reactions of which become most active by the age of 16.
The gynecology of the female body develops in inverse proportion during menopause:
- cyclic secretion is disrupted;
- there is an increase in gonadotropic influence.
Such unsystematic alternations of full menstrual and anovulatory cycles with fading reproductive function are accompanied by changes in the nature of menstruation and the duration of the cycle itself.
Diagnostics
In case of infertility, diagnosing anovulation is the first step to make the correct diagnosis and begin treatment.
Laboratory and instrumental research methods are used:
- blood chemistry;
- analysis of hormone concentrations;
- Ultrasound control and examination of the reproductive organs, thyroid and mammary glands.
If it is necessary to examine the hypothalamic-pituitary system, computed tomography or magnetic resonance imaging is prescribed.
Signs that ovulation has not occurred
The main sign of anovulation is the absence of menstruation. The remaining symptoms are less noticeable, but they can be easily calculated if you know how the normal process proceeds.
Signs of normal ovulation, observed between 7-14 days after the last menstrual period:
- Changes in the nature and amount of vaginal discharge during the entire cycle - from liquid transparent to viscous, milky color.
- Soreness, tension of the mammary glands.
- Pulling sensations in the area of the ovaries, lower abdomen.
- Jumps in basal temperature.
- Increased libido.
More information about ways to determine ovulation is written in our article “What is ovulation.”
Treatment
In some cases, even if anovulation is detected, no special treatment is required; it is enough to avoid stress, eat normally, lose weight, and the menstrual cycle is restored. If hormonal imbalances are detected, the cause must be clarified; treatment by specialized specialists - an endocrinologist, a neurosurgeon (pituitary tumors) may be necessary.
Treatment of anovulation associated with diseases of the reproductive organs can be carried out with medications. Depending on the pathology, anti-inflammatory and antibacterial drugs are used. To correct hormonal levels, progesterone preparations and estrogens are used. An effective method of treating infertility during anovulation is ovarian stimulation. It is carried out according to an individually selected scheme.
For polycystic ovary syndrome, uterine fibroids, and endometriosis, minimally invasive surgery (hysteroscopy or laparoscopy) may be required. For example, laparoscopic dissection of the ovarian membrane or wedge resection allows a woman to become pregnant in more than 50% of cases.
If there is no effect, there is still a chance to get pregnant if you turn to assisted reproductive technologies. For anovulation, IVF is one of the methods of infertility treatment.
1.General information
The short word “anovulation” in a longer translation would mean “the absence of the normal process of maturation of the egg and its migration along the fallopian tube to the uterus for potential fertilization.” Indeed, anovulatory is a menstrual cycle in which bleeding is not preceded by the maturation of the hormonally active corpus luteum, i.e. Conception is impossible in any phase of the cycle. However, menstruation itself in such cases is most often irregular or absent altogether.
If the anovulatory cycle is one-time or extremely rare, and the reasons for this are quite specific and understandable, such a phenomenon is not considered pathological by modern gynecology. However, if a woman of reproductive age has anovulatory most or all menstrual cycles, this is clearly a pathology that requires consultation, examination and medical intervention.
A must read! Help with treatment and hospitalization!
Doctors' opinion
Uncoordinated work of the pituitary gland, hypothalamus and ovaries leads to an imbalance of sex hormones. The consequence is often the appearance of anovulation - a failure in the process of maturation and release of the egg from the follicle. In case of such suspicions, it is useful to regularly measure basal temperature to monitor possible pathology. This is an easy way to identify violations and take timely action.
Anovulation therapy must be carried out under the supervision of a doctor. Additional measures in the form of herbal medicine and other folk methods are allowed, but after consultation with specialists.
How to correctly diagnose anovulation?
When a woman has not had her period for a long time or her cycle is very unstable and has large gaps, anovulation can be diagnosed very quickly. It is enough to undergo a short examination. The gynecologist will prescribe:
- progesterone test;
- gynecological ultrasound;
- folliculometry.
If the progesterone test does not give a clear result and the ultrasound does not show ovarian pathologies, additional studies are carried out:
- smear for a group of infections;
- comprehensive pelvic ultrasound;
- Ultrasound of the ovaries;
- Ultrasound of the corpus luteum;
- Ultrasound of the thyroid gland, since it also produces hormones that can affect reproductive function;
- a set of hormone tests: sex hormones, thyroid hormones and pituitary hormones are examined.
MENSTRUAL CYCLE
In the follicular phase of the menstrual cycle, under the influence of FSH of the pituitary gland, the growth of several follicles begins, but usually one follicle (maturation and function of the follicle is also promoted by LH), which is called dominant .
As the follicles mature, their cells produce female hormones - estrogens, which lead to the proliferation of the mucous layer of the uterus - the endometrium.
Proliferation is the active division of cells leading to thickening of the endometrium. Gradually, other follicles, the growth of which in a given cycle began along with the dominant one, undergo atresia and reverse development. The larger the dominant follicle reaches, the more estrogen its cells produce. When the amount of estrogen reaches a sufficient level for ovulation, a sharp release of luteinizing hormone (LH) occurs into the blood, after which the follicle ruptures within about 24-48 hours - ovulation. In place of the ruptured dominant follicle, a corpus luteum is formed, which functions for an average of 14 days, secreting progesterone. Progesterone gives rise to the second phase of the menstrual cycle - luteinizing.
In parallel with the process occurring in the ovaries, the secretory phase begins in the uterus. During it, the endometrium profusely grows with vessels and glands. The egg, along with the follicular fluid, enters the abdominal cavity, and subsequently into the fallopian tube. If the egg and sperm meet, fertilization occurs in the cavity of the fallopian tube. If this process does not take place, then the unfertilized egg quickly loses its viability (after 12–24 hours) and is destroyed .
If pregnancy does not occur, LH and FSH levels gradually decrease towards the end of the second phase. The endometrium undergoes necrotic changes (vessels shrink, no nutrition occurs), and then it is rejected, menstruation occurs.
The period of development of the dominant follicle can vary both among different women and within the same woman, in different phases of the cycle. Below are three pictures - how different authors schematically presented the physiology of the menstrual cycle.
Diagnosis of ovulation.
The presence of chronic ovulatory dysfunction is indicated by the absence of ovulation in 2 out of 3 cycles. Therefore, all methods for determining ovulation must be used in 2-3 menstrual cycles.
To diagnose ovulation (pictured below), you can use different methods:
- use of test strips to determine ovulation (more correctly to determine an increase in LH);
- measurement of basal (rectal) temperature;
- determination of progesterone in the second phase of the cycle;
- Ultrasound - folliculometry.
Using test strips to determine ovulation (more correctly, to determine an increase in LH levels)
The action of modern home ovulation test strips is based on determining the moment of a sharp increase in the level of LH (luteinizing hormone) in the urine. The start day of testing should be determined depending on the length of the menstrual cycle.
We remind you that the first day of the cycle is the day when menstruation began. Cycle length is the number of days that have passed from the first day of the last menstruation to the first day of the next. If a woman has a regular cycle (always the same length), then you need to start doing tests about 17 days before the start of the next menstruation, since the corpus luteum phase (after ovulation) lasts 12-16 days (on average, usually 14) . The arithmetic is simple, you need to subtract 17 days from the length of the cycle, the resulting number will be the day from which you need to start determining ovulation. For example, if the usual cycle length is 28 days, then testing should begin on the 11th day, and if 35, then on the 18th day.
If the cycle length is not constant, then you need to select the shortest cycle in the last 6 months and use its duration to calculate the day to start testing.
In the absence of regularity and the presence of large delays, the use of tests, without additional monitoring of ovulation and follicles, is not reasonable, both due to the high cost of the tests and their low reliability (when using tests every few days, ovulation can be missed, and the use these tests every day are not worth it).
When used daily (or even 2 times a day - morning and evening), home tests give good results, especially in combination with ultrasound.
When using ultrasound guidance, you can avoid wasting tests and wait until the follicle reaches the required size, approximately 18-20 mm, when it is able to ovulate. Then you can start doing tests every day. Tests can be taken at any time of the day, but if possible you should stick to the same test time. At the same time, in order for the concentration of the hormone in the urine to be as high as possible, it is advisable to refrain from urinating for at least 4 hours and avoid excess fluid intake before testing, because this may lead to a decrease in the concentration of LH in the urine and reduce the reliability of the result. The best time to test is in the morning.
Evaluation of results.
When evaluating test results, it is necessary to compare the result line with the control line. The control line is used for comparison with the result line. The control line always appears in the window if the test was carried out correctly. If the result line is significantly paler than the control line, then the LH surge has not yet occurred and testing should be continued. If the result line is the same or darker than the control line, it means that the hormone has already been released and ovulation will occur within 24-36 hours. The most suitable time for conception is considered to be 2 days from the moment it was determined that the LH surge had already occurred.
If sexual intercourse occurs within the next 2 days, the chance of getting pregnant will be maximum. Once it has been determined that a release has occurred, there is no need to continue testing.
However, this method cannot provide 100% reliability. Since ovulation tests do not show ovulation itself, but a change in the level of luteinizing hormone (LH) over time. A significant rise in LH is very characteristic of the ovulation phase, however, the rise in LH itself does not provide a 100% guarantee that the rise in the hormone is associated specifically with ovulation and ovulation has taken place. An increase in LH levels can also occur in other situations, in particular, with hormonal dysfunction and fluctuations in other hormones (FSH, TSH). In such conditions, an increase in the hormone may occur, but ovulation does not occur. Therefore, you should not completely rely on a positive test result.
Measuring basal (rectal) temperature to determine ovulation
Basal or rectal temperature (BT) is the body temperature at rest after at least 3-6 hours of sleep. The temperature is taken in the mouth, rectum or vagina. The temperature measured at this moment is practically not affected by environmental factors. It is necessary to measure the basal temperature, and not the body temperature under the armpit. A general increase in temperature as a result of illness, overheating, physical activity, eating, stress, naturally affects the basal temperature readings and makes them unreliable.
The method of measuring basal body temperature was developed in 1953 by the English professor Marshall and refers to research techniques that are based on the biological effect of sex hormones, namely on the hyperthermic (i.e., responsible for increasing temperature) effect of progesterone on the thermoregulation center in the brain.
Measuring basal body temperature is one of the main tests for the functional diagnosis of ovarian function. Based on the BT measurement results, a graph is constructed. You need to measure your basal temperature for at least 3 menstrual cycles. A basal temperature chart compiled according to all measurement rules can show the presence of ovulation in a cycle or its absence.
For measurement, a conventional medical thermometer is used: mercury or electronic. The basal temperature is measured with a mercury thermometer for 5 minutes, and the electronic thermometer must be removed after the signal about the end of the measurement, while waiting a few seconds, because The temperature after the signal will continue to rise for some time.
Basic rules for measuring basal temperature.
- You should measure your basal temperature every day if possible, including on your period.
- Measurements can be taken in the mouth, vagina or rectum. The main thing is that the measurement location does not change throughout the entire cycle. Measuring armpit temperature does not provide accurate results. With the oral method of measuring basal temperature, you place the thermometer under your tongue and measure for 5 minutes with your mouth closed. When using the vaginal or rectal method of measurement, insert the narrow part of the thermometer into the anus or vagina, the measurement duration is 3 minutes. Measuring temperature in the rectum is the most common.
- Measure your basal temperature in the morning, immediately after waking up and before getting out of bed.
- It is necessary to measure basal temperature at the same time (a difference of half an hour to an hour (maximum one and a half hours) is acceptable). Keep in mind that every extra hour of sleep raises your basal temperature by about 0.1 degrees.
- Continuous sleep before measuring basal temperature in the morning should last at least three hours. Therefore, if you measure your temperature at 8 am, but got up at 7 am to go, for example, to the toilet, it is better to measure your BBT before that, otherwise, at your usual 8 o’clock it will no longer be informative.
- You can use either a digital or a mercury thermometer to take measurements. It is important not to change the thermometer during one cycle. If you use a mercury thermometer, shake it before going to sleep. The amount of force you use to shake the thermometer immediately before taking your basal temperature can affect your temperature.
- Basal temperature is measured while lying still. Do not make unnecessary movements, do not turn, activity should be minimal. Do not under any circumstances get up to take a thermometer! Therefore, it is better to prepare it in the evening and place it near the bed so that you can reach the thermometer with your hand. Some experts advise taking the measurement without even opening your eyes, since daylight can increase the release of certain hormones.
- Readings from the thermometer are taken immediately after it is removed.
- It is best to immediately record your basal temperature after measurement. Otherwise you will forget or get confused. The basal temperature is approximately the same every day, differing by tenths of degrees. Relying on your memory, you can get confused in the readings. If the thermometer readings are between two numbers, record the lower reading.
- The schedule must indicate the reasons that could lead to an increase in basal temperature (acute respiratory infections, inflammatory diseases, etc.).
- Business trips, travel and flights, sexual intercourse the night before or early in the morning can significantly affect your basal temperature.
- In case of illnesses accompanied by elevated body temperature, your basal temperature will be uninformative and you can stop taking measurements for the duration of your illness.
- Basal temperature can be affected by various medications, such as sleeping pills, sedatives or hormonal drugs. Measuring basal temperature and simultaneous use of oral (hormonal) contraceptives does not make any sense, because basal temperature depends on the concentration of hormones in the tablets.
- After drinking a large amount of alcohol, the basal temperature will be uninformative.
- When working at night, basal temperature is measured during the day after at least 3-4 hours of sleep.
Rationale for the basal body temperature method
Basal body temperature changes throughout the menstrual cycle under the influence of sex hormones.
During the maturation of the egg against the background of relatively high levels of estrogen and low progesterone (the first phase of the menstrual cycle, the proliferation phase), the basal temperature is low; on the eve of ovulation it drops to its minimum, and then rises again, reaching a maximum - at this time ovulation takes place.
After ovulation, a high temperature phase begins (the second phase of the menstrual cycle, the secretory phase), which is caused by low levels of estrogen and high levels of progesterone. Pregnancy under the influence of progesterone also occurs entirely in a high temperature phase. The difference between the “low” (hypothermic) and “high” (hyperthermic) phases is 0.4-0.8 °C. Only with an accurate measurement of basal body temperature, it is possible to record the level of “low” temperature in the first half of the menstrual cycle, the transition from “low” to “high” on the day of ovulation, and the level of temperature in the second phase of the cycle.
Usually during menstruation the temperature remains at 37°C. During the period of follicle maturation (the first phase of the cycle), the temperature does not exceed 37°C. Just before ovulation, it decreases, and after it, the basal temperature rises to 37.1 ° C and higher, due to the influence of progesterone. Until the next menstruation, the basal temperature remains elevated and decreases slightly by the first day of menstruation. If the basal temperature in the first phase, relative to the second, is high, then this may indicate a low amount of estrogens in the body and requires correction with medications containing female sex hormones. On the contrary, if in the second phase, relative to the first, a low basal temperature is observed, then this is an indicator of low progesterone levels and here, drugs are also prescribed to correct hormonal levels. You should take the appropriate medications only after passing the necessary hormone tests and as prescribed by your doctor.
How to interpret the results?
The thermogenic effect of progesterone leads to an increase in body temperature by at least 0.33 ° C and this effect lasts until the end of the luteal, that is, the second phase of the menstrual cycle.
- A persistent two-phase cycle indicates that ovulation has occurred and a functionally active corpus luteum has formed (the correct rhythm of the ovaries).
- If there is no rise in temperature in the second phase of the cycle (monotonic curve) or there are significant temperature swings in both the first and second half of the cycle with the absence of a stable rise, this indicates anovulation (lack of release of the egg from the ovaries).
- If the rise in temperature is delayed or is short-lived (hypothermic phase for 2-7, or 10 days), this indicates a shortening of the luteal phase.
- A slight rise in temperature by 0.2-0.3 °C indicates insufficient function of the corpus luteum.
Normal two-phase cycle according to the basal temperature chart
Such graphs indicate an increase in temperature in the second phase of the cycle by at least 0.4 degrees; noticeably “preovulatory” and
"premenstrual" drop in temperature. The duration of the temperature increase after ovulation is 12-14 days. This curve is typical for a normal two-phase menstrual cycle.
The example graph shows a pre-ovulatory drop on the 12th day of the cycle (the temperature drops significantly two days before ovulation), as well as a premenstrual drop starting from the 26th day of the cycle.
Estrogen deficiency
In the first phase of the cycle, the hormone estrogen dominates in the female body. Under the influence of this hormone, the basal temperature before ovulation averages between 36.2 and 36.5 degrees. If the temperature in the first phase rises and remains above this level, then estrogen deficiency can be assumed. In this case, the average temperature of the first phase rises to 36.5 - 36.8 degrees and is maintained at this level. In such cases, estrogen deficiency also leads to elevated temperature in the second phase of the cycle (above 37.1 degrees), while the rise in temperature is slow and takes more than 3 days.
Using the example graph, the temperature in the first phase is above 37.0 degrees, in the second phase it rises to 37.5, the temperature rises by 0.2 degrees by 17 and
The 18th day of the cycle is insignificant. Fertilization in a cycle with such a schedule is very problematic.
Low temperature in the second phase of the menstrual cycle In the second phase of the cycle, the basal temperature should differ significantly (by about 0.4 degrees) from the first phase and be at 37.0 degrees or higher if you measure the temperature rectally. If the temperature difference is less than 0.4 degrees and the average temperature of the second phase
does not reach 36.8 degrees, this may indicate problems.
Corpus luteum deficiency
In the second phase of the cycle, the female body begins to produce the corpus luteum hormone - progesterone. This hormone is responsible for raising the temperature in the second phase of the cycle and preventing the onset of menstruation. If this hormone is not enough, the temperature rises slowly and the resulting pregnancy may be in jeopardy.
The temperature with corpus luteum deficiency rises shortly before menstruation, and there is no “premenstrual” drop. This may indicate hormonal deficiency.
Particular attention should be paid to charts with a short second phase. If the second phase is shorter than 10 days, then one can also judge that the second phase is insufficient.
Situations when the basal temperature remains elevated for more than 14 days occur during pregnancy, the formation of an ovarian corpus luteum cyst, as well as during an acute inflammatory process of the pelvic organs.
Estrogen-progesterone deficiency
If, in combination with low temperature in the second phase, the graph shows a slight rise in temperature (0.2-0.3 C) after ovulation, then such a curve may indicate not only a lack of progesterone, but also a lack of the hormone estrogen.
Anovulatory cycle.
In a cycle without ovulation, the corpus luteum, which produces the hormone progesterone and affects the increase in basal body temperature, does not form. In this case, the temperature rise line is not visible on the basal temperature graph, which indicates the absence of ovulation and, accordingly, we are talking about an anovulatory cycle.
Since every woman can have 1-2 anovulatory cycles per year, one anovulatory cycle is not a reason for concern. This is a normal option and does not require medical intervention. But if this situation repeats in 2-3 cycles, then you should contact a gynecologist. Without ovulation, pregnancy is impossible!
A monotonous curve occurs when there is no pronounced rise throughout the entire cycle. This schedule is observed during an anovulatory (no ovulation) cycle.
Menstrual cycle length
Normally, the total length of the cycle should not be shorter than 21 days and should not exceed 35 days. If the cycles are shorter or longer, then there may be ovarian dysfunction, which is often the cause of infertility and requires treatment by a gynecologist.
The basal temperature chart is divided into the first and second phases. The division takes place where the ovulation line (vertical) is marked. Accordingly, the first phase of the cycle is the segment of the graph before ovulation, and the second phase of the cycle is after ovulation.
Normally, the length of the second phase of the cycle is from 12 to 16 days, most often 14 days. In contrast, the length of the first phase can vary greatly, and these variations are the individual norm. At the same time, in a healthy woman in different cycles there should be no significant differences in the length of the first phase and the second phase. The total length of the cycle normally changes only due to the length of the first phase.
One of the problems identified on the graphs and confirmed by subsequent hormonal studies is the failure of the second phase. If, over the course of several cycles, measuring basal temperature, according to all the rules, the second phase is shorter than 10 days, this is a reason to contact a gynecologist.
Temperature difference
Normally, the difference in average temperatures of the first and second phases should be more than 0.4 degrees. If it is lower, this may indicate hormonal problems.
An increase in basal temperature occurs when serum progesterone levels exceed 2.5-4.0 ng/ml (7.6-12.7 nmol/l). However, monophasic basal temperature has been identified in a number of patients with normal progesterone levels in the second phase of the cycle. In addition, monophasic basal temperature is observed in approximately 20% of ovulatory cycles.
You need to know that the presence of a two-phase basal temperature does not guarantee the occurrence of ovulation, since even with the luteinization of a non-ovulated follicle, a two-phase basal temperature is observed . However, the duration of the luteal phase in accordance with basal temperature data and the low rate of rise in basal temperature after ovulation are accepted by many authors as criteria for diagnosing luteinization syndrome of a non-ovulating follicle.
Individual features of the basal temperature chart
Low or high temperature in both phases, provided that the temperature difference is at least 0.4 degrees, is not a pathology. This is an individual feature of the body. The measurement method can also affect the temperature values. Typically, with an oral measurement, the basal temperature is 0.2 degrees lower than with a rectal or vaginal measurement.
Determination of progesterone to determine ovulation.
The diagnosis is made based on a blood test for progesterone in the second phase of the cycle. With a regular menstrual cycle and suspected anovulation, it is necessary to measure progesterone in the blood serum on days 20-24 of the cycle. When progesterone levels decrease below 3-4 ng/ml, the cycle is considered anovulatory. But we must remember that a blood test will have to be taken over 2-3 menstrual cycles, since the presence of chronic ovulatory dysfunction is indicated by the absence of ovulation in 2 out of 3 cycles. It should also be noted that normally women have 1-2 cycles per year that can be anovulatory. Therefore, taking a blood test for progesterone once does not make sense.
Ultrasound folliculometry to determine ovulation.
Today, folliculometry is considered one of the most accurate methods for determining the day of ovulation and, accordingly, increasing the chance of fertilization of the egg. In fact, folliculometry is ultrasound monitoring that allows you to monitor the development and maturation of the follicle from the beginning to the end of the menstrual cycle. The study must be repeated 3 to 5 times in one menstrual cycle.
For women with a normal menstrual cycle that lasts 28 days, as a rule, the first ultrasound is scheduled on the 8th or 10th day of the menstrual cycle. Naturally, during this period it is difficult to isolate the desired follicle - however, it is possible to determine the presence of pathology of the uterus and ovaries, therefore, the first ultrasound is basic. Data obtained from each ultrasound in one cycle must be compared with ultrasound data in subsequent cycles.
For patients who have an unstable menstrual cycle lasting more or less than 28 days (but within the normal menstrual cycle length of 21 to 35 days), the first examination is scheduled six days before the expected day of ovulation, relying on the length of the shortest cycle in the last 6 months .
Let's look at this with a specific example.
It is believed that the second phase of the menstrual cycle is stable and lasts on average 14 (12-16) days . To determine the expected day of ovulation, subtract 14 days from the last day of the cycle. If the duration of the menstrual cycle is 30 days, then 30-14=16, which means that ovulation is expected on the 16th day of the cycle (14-18), then you need to subtract 6 from 16, you get the number 10 (8-12) - this will be the day of the cycle when to start folliculometry. Repeated studies are carried out at intervals of 2-3 days before and after the ovulation period. For longer menstrual cycles, the decision on the need for folliculometry is made by the gynecologist for each patient individually.
During the first examination, the doctor may notice one, rarely several, enlarged follicles. In most cases, only one dominant follicle matures; its dominance is determined after a few days. On average, the diameter of the follicle is 12-15 mm. But its dimensions are constantly increasing - at the time of ovulation they are most often 20-25 mm . It is these details that the doctor pays attention to. Moreover, immediately after the mature follicle ruptures and the egg is released, a corpus luteum forms in its place, which can be examined during an ultrasound for a few more days. After ovulation, a small amount of free fluid is present in the retrouterine space - this is the follicular fluid of the ruptured follicle. The doctor also evaluates the thickness of the endometrium over time.
Ideally, a blood test for progesterone can also be performed on days 20-24 of the menstrual cycle. An increased level of progesterone in the blood, together with signs of ovulation according to ultrasound, reliably indicates that ovulation has occurred.
The following are the options identified when performing folliculometry.
- Normal ovulation.
It is characterized by such signs as:
- before ovulation there are 1-2 dominant follicles (their size is at least 15 mm, but not more than 24 mm);
- the dominant follicle disappears after ovulation;
- after ovulation, signs of the corpus luteum are visualized in the ovary;
- after the release of the egg, a certain amount of free fluid is visualized behind the uterus;
- a week after ovulation, a high level of progesterone is noted in the blood (this is due to the fact that the corpus luteum has begun to work).
Persistent follicle.
Despite the fact that the dominant follicle was fully mature, ovulation did not occur, and the follicle continued to persist. This situation may persist after menstruation.
Signs of this condition are:
- long-existing follicle measuring 18-24 mm;
- lack of free fluid in the space behind the uterus;
- the corpus luteum does not form;
- high levels of estrogen and low levels of progesterone are determined in the blood.
Follicular cyst.
This is a condition when the follicle not only did not ovulate, but also grew in size more than 25 mm.
Signs of such a cyst are:
- follicle diameter 25 mm or more;
- no free fluid behind the uterus;
- the corpus luteum did not form
- the level of hormones in the blood: progesterone - low, estrogen - high.
Luteinization of the follicle.
The follicle formed, did not ovulate, but, despite the fact that ovulation did not occur, a corpus luteum formed in its place.
Signs of this follicle:
- the follicle can be of any size;
- the follicle gradually shrinks;
- no free fluid behind the uterus;
- hormone levels in the blood: progesterone – increased, as in the second phase of the cycle.
No follicular development.
Signs:
— there are follicles, but they do not grow;
- no corpus luteum;
- no dominant follicle;
- progesterone levels are low.
Treatment of endocrine infertility
Treatment of endocrine infertility usually consists of two stages.
At the first stage, the doctor treats the patient, aimed at correcting hormonal imbalances .
At the second stage, it stimulates ovulation , in which the maturation of one or more dominant follicles is achieved with the help of hormonal drugs.
Correction of the endocrine system
If the cause of endocrine disorders is obesity or weight loss , which causes secondary amenorrhea, treatment should include mandatory weight adjustment. This is achieved through proper diet and exercise, as well as the use of certain medications (weight loss medications are prescribed by a doctor according to strict indications).
hyperprolactinemia , a condition in which the level of the hormone prolactin in the blood increases, is relatively easy to treat dopamine receptor agonist drugs are used in treatment : bromocriptine and cabergoline.
With polycystic ovary syndrome (PCOS), some women successfully undergo conservative treatment of hormonal infertility, but some women have to resort to surgical intervention: wedge resection of the ovaries or cauterization (electro- or thermocoagulation of the ovaries). Both operations lead to the restoration of a normal menstrual cycle and ovulation in 60-70% of women. However, unfortunately, pregnancy in women after wedge resection of the ovaries is possible only in 40-55%. This is due, among other things, to the fact that after such an operation, adhesions usually form in the small pelvis, making the fallopian tubes impassable. In this case, endocrine infertility turns into tubal-peritoneal, which is much less treatable.
In case of hyperadrogenism, treatment of amenorrhea and anovulation is also carried out - through medicinal hormonal correction of adrenal or ovarian function.
Ovulation stimulation
When treating endocrine infertility, it is often necessary to stimulate ovulation. In this case, the drug clomiphene citrate (Clomid) is used, which stimulates the release of follicle-stimulating hormone (FSH) in the body. With this type of stimulation, about 10% of pregnancies may be multiple. However, about 30% of women are clomiphene-resistant, i.e. do not respond to clomiphene.
If treatment with clomiphene is ineffective during 4-6 ovulatory cycles, gonadotropins (HMG, r-FSH, hCG) or laparoscopy (cautery or wedge resection of the ovaries) are used to stimulate ovulation. If there is no effect, the issue of IVF is considered.
It must be remembered that for a number of reasons, the effectiveness of IVF after 35 years sharply decreases.
Section: Ovulation
So, you armed yourself with a thermometer and the willingness to wake up every morning at the same time, look at the mercury column with bated breath and torment your girlfriends with questions about whether ovulation occurred)
To make life easier for your beloved girlfriends, let's figure out what basal temperature is and how to prepare it correctly)))
Rules for measuring basal temperature:
- You can start measuring your basal temperature on any day of your cycle, but it is better if you start measuring at the beginning of your cycle (on the first day of your period).
- Always measure the temperature in the same place. You can choose the oral, vaginal or rectal method. Measuring under the armpit does not give accurate results. It doesn't matter which measurement method you choose: it is important not to change it during one cycle.
- With the oral method, you place the thermometer under your tongue and measure for 5 minutes with your mouth closed.
- With the vaginal or rectal method, the measurement time is reduced to at least 3 minutes.
- Take your temperature in the morning, immediately after waking up and before getting out of bed.
- Continuous sleep before measurement should last at least 6 hours.
- The temperature is measured strictly at the same time. If the measurement time differs from the usual one by more than 30 minutes, then this temperature is considered not indicative.
- You can use either a digital or a mercury thermometer to measure. It is important not to change the thermometer during one cycle.
- If you use a mercury thermometer, shake it off before you go to sleep. The effort you use to shake off the thermometer just before taking a measurement can affect the temperature.
- Write down your basal temperature values every day in a notepad or use our website to keep charts.
- Business trips, travel and flights can significantly affect your basal temperature.
- In case of illnesses accompanied by elevated body temperature, your basal temperature will not be indicative and you can stop taking measurements for the duration of your illness.
- Various medications, such as sleeping pills, sedatives and hormonal drugs, can affect basal temperature.
- Measuring basal temperature and simultaneous use of contraception does not make any sense.
- After drinking a large amount of alcohol, the temperature will not be indicative.
We have studied the rules, now we move directly to studying the chart itself.
Ovulation line on the basal temperature chart
To determine the onset of ovulation, the rules established by the World Health Organization (WHO) are used:
Three temperature values in a row must be above the level of the line drawn over the previous 6 temperature values. The difference between the center line and the three temperature values must be at least 0.1°C on two out of three days and at least 0.2°C on one of those days. If your temperature curve meets these requirements, then an ovulation line will appear on your basal temperature chart 1-2 days after ovulation.
A little boring, but useful...
Cycle length
Smart doctors say that in general, the length of the cycle should be from 21 to 35 days. In any other case, they are afraid of the possibility of ovarian dysfunction. So put your feet up and see a doctor if there are differences.
Length of the second phase on the basal temperature chart
The basal temperature chart is divided into two phases by the vertical ovulation line. The first phase is the period before ovulation and the length of the first phase can vary greatly and these variations are the individual norm. But the period after is precisely the time when each of us begins to wonder: “Is there life after ovulation?” - and is called the second phase of the cycle. It can last from 12 to 18 days. The total length of the cycle normally changes only due to the length of the first phase.