Cholecystitis
Which doctors should I contact?
After detecting symptoms indicating cholecystitis, you should immediately consult a doctor.
Usually in such cases they turn to a surgeon, therapist, gastroenterologist, and in acute cases call an ambulance. All patients with acute cholecystitis and suspected of having this disease are subject to referral to a surgical hospital with a team of qualified surgeons and anesthesiologist on duty around the clock. In severe cases, the participation of a resuscitator is required. Treatment of cholecystitis
The main goals of treatment of chronic acalculous cholecystitis are relief of pain and inflammation in the gallbladder, correction of digestive and metabolic disorders, treatment of complications and concomitant diseases.
- During the period of exacerbation, patients with chronic cholecystitis are recommended bed rest, fasting for 1-3 days, then diet therapy - limiting fatty foods and their calorie content (diet No. 5, 5A), eating 4-6 times a day.
- Antispasmodics and analgesics are the main drugs for the treatment of exacerbation of cholecystitis, allowing to alleviate biliary colic.
- Analgesics are used to relieve pain.
- To stop the infectious inflammatory process, broad-spectrum antibiotics are prescribed.
- When helminthiasis is confirmed, anthelmintic drugs are used.
- Relief of dyspeptic disorders is carried out with the help of enzymatic, antiemetic drugs that suppress gastric secretion, etc.
- Violation of the outflow of bile is corrected with choleretic agents.
- If the stones are cholesterol, then there is a possibility of dissolving them with the help of drugs based on ursodeoxycholic acid.
Lithotripsy is a shock wave method that is used to crush stones, which are subsequently safely removed from the body or dissolved.
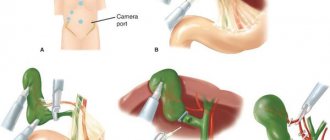
The selection criterion for patients for this procedure is limited by the size of the stones - single stones no more than 2 cm, a few up to 1 cm. The standard solution for the treatment of chronic calculous cholecystitis is surgical intervention, which eliminates new exacerbations and possible complications. Laparoscopic cholecystectomy is the main surgical method for treating chronic calculous cholecystitis. Removal of the gallbladder is performed with special instruments through one or more small incisions in the abdominal wall. Complications
Cholecystitis can lead to a number of serious complications.
- Due to inflammation, the gallbladder can stretch and increase in size (dropsy), which increases the risk of its rupture (perforation) and the development of peritonitis.
- Stagnation of bile in the gallbladder is a risk factor for infection of bile by bacteria, as a result of which the infection can enter the bloodstream with the development of sepsis.
- Violation of blood microcirculation in the wall of the gallbladder with the further development of ischemia and focal or total necrosis of the wall is the cause of gangrene of the gallbladder.
The following complications of cholecystitis require emergency surgical care:
- empyema of the gallbladder - accumulation of pus in the cavity of the gallbladder;
- peri-vesical infiltrate and abscess - an inflammatory process that spreads beyond the gallbladder;
- perforation is a rupture of the wall of the gallbladder with the release of its contents into the abdominal cavity.
Intraoperative complications include bleeding and bile duct injury.
Postoperative complications include pneumonia, myocardial infarction, thromboembolic complications, and pulmonary embolism. Prevention of cholecystitis
Primary prevention consists of eliminating risk factors leading to the development of chronic cholecystitis - timely sanitation of the biliary tract, elimination of dyskinesia, early detection of stones in the gallbladder and timely adequate treatment, including surgery.
Secondary prevention involves reducing the frequency of relapses, preventing the progression of the disease and the development of complications. Active identification of patients with clinically pronounced forms of chronic cholecystitis, frequent exacerbations and their adequate non-drug and drug therapy.
Diet plays a significant preventive role - low-calorie, predominantly plant-based food is useful, the use of vegetable fats containing polyunsaturated fatty acids, phospholipids, vitamin E, which help normalize cholesterol metabolism, participate in the synthesis of prostaglandins that dilute bile, and increase the contractile function of the gallbladder. Vegetable fats are especially important for bile stagnation. Vegetables, fruits, and bran promote the discharge of bile, reduce the cholesterol content in bile, thereby reducing the likelihood of stone formation.
Sources:
- National clinical guidelines “Acute cholecystitis”. Russian Society of Surgeons, 2015.
- Beburishvili A.G., Panin S.I., Zyubina E.N., Bykov A.V. Optimal timing of surgical treatment of acute cholecystitis according to evidence-based studies. Annals of surgical hepatology. 2020;25(3):12-19.
- Vorotyntsev A.S. Modern ideas about the diagnosis and treatment of cholelithiasis and chronic calculous cholecystitis. "Attending doctor". No. 02, 2012.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
Publications in the media
Acute cholecystitis is an acute inflammation of the gallbladder. Frequency . Women over 40 years of age who are obese are more often affected. Acalculous cholecystitis most often develops in men.
Classification • Acute catarrhal cholecystitis. Inflammation is limited to the mucous and submucous membranes • Phlegmonous cholecystitis - purulent inflammation with infiltration of all layers of the gallbladder. Possible ulceration of the mucous membrane with subsequent exudation of inflammatory fluid into the paravesical space • Gangrenous cholecystitis - partial or total necrosis of the gallbladder wall. When the bladder wall is perforated, bile leaks into the abdominal cavity (gangrenous-perforative cholecystitis). Empyema of the gallbladder is purulent inflammation of the gallbladder.
Etiology • In 95% of cases, it develops due to obstruction of the cystic duct by a stone • Intestinal microflora is most often cultured from the wall of the gallbladder • Acalculous cholecystitis (5–10% of cases of acute cholecystitis in adults, up to 30% in children) can be associated with major surgical interventions, multiple injuries, extensive burns, recent childbirth, sepsis, salmonellosis, prolonged fasting, parenteral nutrition.
Pathogenesis • Stone obstruction leads to stagnation of bile and irritation of the gallbladder wall • Increased pressure in the gallbladder can lead to compression of the vessels of the gallbladder wall and its necrosis • Bacteria deconjugate bile salts with the formation of toxic bile acids that damage the mucous membrane of the gallbladder • In the pathogenesis of acalculous cholecystitis The significance of bile stagnation against the background of gallbladder paresis, an increase in its viscosity and lithogenicity have been established.
Pathomorphology • The gallbladder is distended, dull, contains turbid fluid or pus • Histologically, swelling of the wall and hemorrhages in the submucosa are revealed • As inflammation subsides, fibrosis develops.
Clinical manifestations
• Pain (hepatic colic) •• Localized in the epigastric or right hypochondrium •• Radiates to the back below the angle of the right shoulder blade, right shoulder, less often to the left half of the body •• Occurs at night or early in the morning, increases to a certain level and lasts 30–60 min without decreasing •• The occurrence of pain may be preceded by the consumption of fatty, hot, spicy foods, alcohol, emotional experiences •• Accompanied by increased sweating, a grimace of pain on the face and a forced posture - on the side with legs tucked to the stomach • Fever • Nausea, vomiting, sometimes with an admixture of bile • Shallow breathing, the stomach is weakly involved in the act of breathing • Murphy's symptom - involuntary holding of breath during inspiration with pressure on the right hypochondrium • Pain when inhaling during palpation of the right hypochondrium (Keur's symptom) • Pain when tapping along the edge of the right costal arch (Ortner's symptom) • Geno de Mussy-Georgievsky's symptom (phrenicus symptom) - pain when pressing with a finger between the legs of the right sternocleidomastoid muscle • Shchetkin-Blumberg's symptom becomes positive when the peritoneum is involved in the inflammatory process (peritonitis) • Jaundice (in 15% of patients) - caused by obstruction of the common bile duct with stones • On percussion of the abdomen - tympanitis (reflex intestinal paresis).
Laboratory tests • Blood test - leukocytosis, moderate shift of the leukocyte formula to the left • In 10-15% of patients (with concomitant choledocholithiasis, with acalculous cholecystitis), the concentrations of alkaline phosphatase and bilirubin are increased in the serum, bilirubin appears in the urine, with complete stone obstruction - urobilin disappears • Patients with fever may have positive blood cultures.
Instrumental studies • General radiography is performed for abdominal pain of unknown etiology • Ultrasound of the gallbladder reveals stones, thickening of the gallbladder wall, accumulation of fluid around it, with acalculous cholecystitis - gas in the bladder wall and detachment of the mucous membrane • Radioisotope scanning visualizes the common bile duct and intestines without filling the gallbladder indicates obstruction of the cystic duct (with acalculous cholecystitis, the method gives a large number of false positive results).
Differential diagnosis • Perforated or penetrating ulcer of the stomach and/or duodenum • MI • Pancreatitis • Hiatal hernia • Right lower lobe pneumonia • Acute appendicitis • Hepatitis • Infectious diseases.
TREATMENT
Diet . At the beginning of an attack of acute cholecystitis - a water-tea break • After 5-10 days, diet No. 5a is prescribed • If all acute phenomena disappear after 3-4 weeks - switch to diet No. 5.
Conservative treatment • Bed rest • Antispasmodics • Painkillers • Intravenous fluids • Antibacterial therapy •• If the patient is in a stable condition with pain and mild fever - ampicillin (4-6 g/day) •• For severe septicemia - a combination of gentamicin (3-5 mg /kg/day) with clinadmicin (1.8–2.7 g/day) or metronidazole with third generation cephalosporins, or imipenem + cilastatin.
Surgical treatment • The method of choice is early (within the first 72 hours) laparoscopic cholecystectomy, because with such an operation, mortality and the incidence of complications are lower than with a planned operation performed after 6-8 weeks of conservative treatment • Patients with acute cholecystitis, complicated peritonitis, gangrenous cholecystitis, perforation of the gallbladder wall are subject to • Percutaneous cholecystostomy in combination with antibacterial therapy - method of choice in the treatment of seriously ill patients, elderly patients with complications of acute cholecystitis • Emergency cholecystectomy is indicated for patients with acalculous cholecystitis; in case of critical condition of the patient, percutaneous cholecytostomy is performed under ultrasound control.
Complications • Empyema - acute purulent inflammation of the gallbladder • Perforation (15% of cases) •• Into the free abdominal cavity, the course is acute, mortality 30% •• Local - leads to the development of a peri-vesical abscess, the course is subacute •• Into the adjacent organ (duodenum, jejunum , colon or stomach), chronic course with the formation of a vesico-intestinal fistula • Sepsis • Pancreatitis.
Course and prognosis of the disease • In 85% of cases - spontaneous recovery, in 1/3 of patients a new attack develops within 3 months • Rapid progression of cholecystitis to gangrene or empyema of the gallbladder, formation of fistulas, intrahepatic abscesses, development of peritonitis is possible • Mortality in complicated cholecystitis reaches 50–60% • Mortality with acalculous cholecystitis is 2 times higher than with calculous cholecystitis, gangrene and perforation develop more often.
ICD-10 • K81 Cholecystitis
Popular questions about calculous cholecystitis
What is calculous?
The term means that the cause of an acute or chronic inflammatory process lies in stones formed inside the gallbladder.
How much water should you drink if you have cholecystitis?
During an attack, it is recommended to drink as much mineral water as possible without carbon. Water is especially useful after a bout of vomiting.
What can you eat with acute cholecystitis?
Doctors recommend limiting food intake and eating foods that do not cause increased bile secretion.
Causes of the disease
The cause of the disease is a violation of the natural outflow of bile. The secretion stagnates, corrodes the walls of the gallbladder, blood supply to tissues deteriorates, pathogenic microflora is activated. When the bile ducts become clogged with a stone, the patient becomes inflamed.
Factors that increase the likelihood of disease:
- obesity;
- sudden weight loss;
- starvation;
- long-term parenteral nutrition;
- taking medications belonging to the category of synthetic hormones, antibiotics (contraceptives, estrogen- and progesterone-containing drugs, ceftriaxone).
The likelihood of occurrence and exacerbation of the disease is observed during pregnancy and childbirth. Risk factors also include advanced and middle age, hereditary predisposition, a history of diabetes mellitus, liver cirrhosis, Crohn's disease, etc.
Causes of acute phlegmonous calculous cholecystitis
The formation of stones in the gall bladder provokes acute phlegmonous calculous cholecystitis
The causes of this condition can be divided into two groups: those that provoke the appearance of stones and those that promote the accumulation of pus.
There are also factors that equally influence both of these processes. In general, stones play a dominant role in the formation of phlegmonous cholecystitis.
Reasons for their formation:
Chronic cholecystitis - symptoms and treatment
Treatment of chronic cholecystitis can be either conservative or surgical.
Due to the fact that 85-95% of patients with chronic cholecystitis have a calculous (stone form) of the disease, which is associated with the development of serious complications, removal of the gallbladder is the only possible and most effective way to prevent the latter.
Surgery for cholecystitis
Surgical treatment of chronic cholecystitis (cholecystectomy) is a planned operation, and in case of severe exacerbation - an emergency or even a “life-saving” operation. Depending on the severity of the disease, its duration, the number of relapses, their intensity and the patient’s condition, removal of the gallbladder can be carried out using several methods:
- classic cholecystotomy (through an incision of the anterior abdominal wall about 15 cm long in the right hypochondrium);
- mini-cholecystectomy (incision in the right hypochondrium 4-6 cm long);
- laparoscopic cholecystectomy (using laparoscopic instruments, i.e. through “punctures” - four incisions 5-10 mm in size);
- mini-laparoscopic cholecystectomy (three punctures 3-5 mm in size) - used in rare cases when it is absolutely necessary to achieve maximum cosmetic effect.
Rehabilitation after cholecystectomy
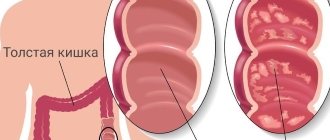
After removal of the gallbladder, the patient must regularly visit the doctor over the next three months; at 3–6–12 months, he must undergo blood tests and undergo an ultrasound of the abdominal organs. You should also take choleretic drugs, eat small portions 3-5 times a day and avoid fatty foods. If you do not adjust your diet, aggressive bile that flows into the intestines increases the risk of colorectal cancer.
Ultrasound lithotripsy
If there are contraindications to surgery or if the patient does not want to undergo surgery, you can use a non-surgical method of crushing stones - ultrasonic lithotripsy. However, crushing and removing stones is not a cure, and in 95-100% of cases the stones form again after some time.
Drug therapy
During an exacerbation, painkillers (non-steroidal anti-inflammatory drugs - NSAIDs) and antispasmodics are used to relieve spasm of the muscles of the gallbladder and its ducts.
Prevention of infection and sanitation of the lesion is carried out with antibiotic therapy (cephalosporins). Detoxification is carried out using solutions of glucose and sodium chloride. Treatment of dyspeptic syndrome is also necessary: enzyme preparations are usually used for this.[10]
Diet
When the disease is in remission, it is necessary to strictly follow a diet: avoid spicy, fatty and fried foods.
Physiotherapy and traditional methods of treatment
Patients suffering from chronic acalculous cholecystitis are treated by a gastroenterologist. It is possible to carry out physiotherapy (electrophoresis, mud therapy, reflexology, stay at balneological resorts) and herbal medicine (taking decoctions of yarrow, tansy, buckthorn).
Therapeutic exercises for cholecystitis
There is no convincing evidence about the benefits of special exercises in the treatment or prevention of cholecystitis. Moreover, the use of therapeutic exercises can be dangerous. More often, the disease occurs in the form of chronic calculous cholecystitis; physical activity in this case can lead to complications, such as obstructive jaundice. It is quite enough for the patient to lose weight and engage in regular physical therapy.
Treatment methods
Prevention of the development of cholecystitis involves maintaining a healthy lifestyle, eliminating bad habits and abuse, normalizing the diet, monitoring the quality and composition of food consumed.
It is very important to promptly treat infectious diseases, strengthen the immune system and prevent serious inflammatory processes in internal organs. It is especially important to prevent liver diseases and effectively treat them, since the relationship between liver pathologies and cholecystitis is very close.
Prevention of obesity, combating excess weight and normal physical activity are factors that prevent not only the occurrence of cholecystitis, but also a large number of other diseases.
Inpatient treatment of cholecystitis consists of surgical or conservative therapy. In mild cases, drug treatment, diet and physiotherapy are used, sometimes treatment outside the hospital, on an outpatient basis, is possible. During periods of remission, patients with chronic cholecystitis are advised to undergo courses of physiotherapeutic and sanatorium-resort treatment.
The most commonly used drug treatments for exacerbations are:
• non-steroidal anti-inflammatory drugs; • antibacterial drugs; • sulfonamides; • antispasmodics; • choleretic agents; • stimulants of bile duct peristalsis; • enzymes; • homeopathic remedies, herbal medicine.
Diet for cholecystitis plays a central role and is selected strictly individually, depending on the patient’s digestive characteristics, metabolic processes, causes of the disease, the presence of chronic pathologies and many other factors.
The following requirements are common to all therapeutic nutrition systems for cholecystitis:
• categorical exclusion of fried, spicy, fatty foods, pickles, marinades, canned and smoked foods; • refusal of alcoholic beverages; • strict adherence to food intake; • avoiding overeating and irregular meals;
Meals should be fractional, you need to eat in small portions several times a day. You should not eat either too hot or too cold food. A nutritious and healthy diet greatly increases the effectiveness of the treatment measures taken, allows you to achieve the best results in treatment and consolidate them for a long time. Following a diet and strictly following medical recommendations can help completely avoid exacerbations or reduce them to a minimum.
Surgical treatment of cholecystitis (cholecystectomy) is a last resort in the treatment of gallbladder inflammation.
The operation can be emergency - in case of complications of cholecystitis (peritonitis, necrosis, empyema) or so-called “early cholecystectomy”, that is, planned, if indicated. Planned operations for cholecystitis are performed to prevent the development of complications and remove stones from the gallbladder and ducts.
Modern surgery uses two options for performing cholecystectomy: the conventional method and the closed (endoscopic) method. Endoscopic operations are less traumatic and do not require large incisions, however, open operations are still safer and more effective interventions for cholecystitis, especially in emergency cases.
Surgery for cholecystitis often saves the patient’s life, but does not prevent further development of the negative consequences of the disease.
That is why it is very important to consult a doctor in a timely manner at the first signs of disruption of the gallbladder and liver. Regular visits to a gastroenterologist for chronic cholecystitis will help you properly organize the necessary lifestyle and avoid many complications and irreversible consequences.