Antibiotics of the macrolide group are extremely often prescribed in therapeutic practice. This is quite justified - in the modern world, with such a variety of antibacterial drugs, preference should be given to those that have a minimum of side effects undesirable for the patient, and macrolide antibiotics are usually well tolerated by patients.
In order to improve the safety profile, antibiotics of the macrolide group with an additional prebiotic component were developed - Ecoantibiotics. These drugs have an additional beneficial effect on the state of the intestinal microflora, thereby improving the tolerability of antibacterial therapy. The group of macrolides includes ecoantibiotics Ecomed (azithromycin) and Ecositrin (clarithromycin).
Antibiotics from the macrolide group
Macrolides are drugs, antibiotics, the chemical composition of which is complex: to be more precise, these are solid substances similar in their properties to lactones; their structure contains a macrocyclic lactone ring
Depending on the number of carbon atoms in the ring, macrolides are divided into 14-membered ones, which include erythromycin, roxithromine and clarithromycin; 15-membered - azithromycin and 16-membered - midecamycin, spiramycin, josamycin.
The main purpose of macrolides is activity against intracellular pathogens, such as chlamydia, mycoplasma, legionella and campylobacter; macrolides also show activity against gram-positive cocci (streptococci and staphylococci).
Publications
Modern medicine is unthinkable without antibacterial drugs, which are successfully used in patients with various diseases.
The huge role of antibiotics in the treatment of diseases caused by bacteria is indisputable, but it should be said that in almost 50% of cases, according to leading world experts, this group of drugs is used unjustifiably [1,2]. Unfortunately, pediatricians in outpatient clinics are often forced to prescribe initial antibiotic therapy empirically, without identifying the pathogen, guided by information about the most common pathogens for a particular pathology. This tactic is justified if the patient has signs of a bacterial disease, but there are often cases when antibiotics are prescribed to patients with ARI and diarrhea, which most often have a viral etiology [3,4].
In recent years, many new antibiotics of different pharmacological groups have been introduced into medical practice. The group of macrolides attracts the greatest attention from pediatricians. This is facilitated by the increasing frequency of drug allergies to penicillins and cephalosporins in the pediatric population (up to 10% of cases), as well as the ineffectiveness of b-lactams for infections caused by intracellular pathogens [5]. Among the antibacterial groups, macrolides, created more than half a century ago, continue to be one of the most commonly used classes of antimicrobial agents. According to the results of a study by the European Society of Antimicrobial Chemotherapy (ESAC), conducted in 2001–2002, in most European countries, macrolides rank second among antibiotics in terms of consumption in outpatient practice, second only to penicillins [6,7]. Macrolides are a relatively small group of antibacterial drugs. To date, slightly more than 10 antibiotics of this group are known [8].
The basis of the chemical structure of macrolides is a macrocyclic lactone ring with one or more carbohydrate residues. Depending on the number of carbon atoms in the macrocyclic ring, they are divided into 14-, 15- and 16-membered (Table 1). [9]. A representative of the first generation of so-called “old” macrolides is erythromycin. Features of pharmacokinetics, a significant percentage of adverse events and an increase in microbial resistance created the prerequisites at the end of the 20th century for the development and implementation of the second generation of macrolides. “New” macrolides have a wider spectrum of antimicrobial activity, including intracellular pathogens, while maintaining a low level of microbial resistance. Many of them have unique additional anti-inflammatory and immunomodulatory effects. [6,10].
Table 1. Classification of macrolides [9,11].
| 14-member | 15-membered (azalides) | 16-member |
| Natural | ||
| Erythromycin Oleandomycin | Spiramycin Josamycin Midecamycin | |
| Semi-synthetic | ||
| Roxithromycin Clarithromycin | Azithromycin | Midecamycin acetate |
The antimicrobial effect of macrolides is due to disruption of protein synthesis at the stage of translation in the cells of microorganisms sensitive to them. The nature of the antimicrobial action of macrolides is usually bacteriostatic, although under certain conditions, depending on the type of microorganisms and the concentration of the drugs, a bactericidal effect is possible (for example, against S. pyogenes, S. pneumoniae, N. meningitides, pathogens of diphtheria, whooping cough). [8,11-13].
Macrolides have approximately the same spectrum of antibacterial activity, including gram-positive (S. agalactiae, penicillin-sensitive
strains S. pneumoniae, S. pyogenes, S. viridans, S. aureus MS), a number of gram-negative (B. burgadorferi, G. vaginalis, H. pilory, B. pertusis, M. catarrhalis, H. influenzae, N. gonorrheeae, T. gondii, etc.), as well as intracellular pathogens (C. jejuni, C. pneumoniae, C. trachomatis, Legionella spp., M. pneumoniae). However, there are also differences. Thus, clarithromycin and midecamycin are most active against methicillin-sensitive strains of S. aureus [8,10-13]. Azithromycin is superior to other macrolides in activity against H. influenzae, M. catarrhalis and C. jejuni, rickettsia, which causes atypical pneumonia, and the causative agents of Lyme disease. In addition, azithromycin is the only macrolide capable of acting on Enterobacteriaceae, such as Escherichia coli, Shigella and, to a lesser extent, Salmonella. Clarithromycin is superior to other macrolides in its action on L. pneumophila and H. pylori. Against the whooping cough bacillus, clarithromycin and erythromycin show the highest activity, and roxithromycin and josamycin have the weakest effect [8].
The attractiveness of using macrolides in outpatient pediatric practice is explained by the following points.
Features of drug pharmacokinetics. Macrolides are characterized by the presence of such pharmacological characteristics as rapid absorption in the gastrointestinal tract, with the exception of erythromycin, excellent penetration into tissue, good clinical and biological tolerability, which distinguish them favorably from antibiotics of other groups. Penetrating into various tissues, they accumulate especially well in lung tissue, bronchial mucosa, bronchial secretions, saliva, tonsils, middle ear, and sinuses [8]. In addition, they have the inherent ability to accumulate not just in tissues, but intracellularly in concentrations several times higher than their content in the blood. Thus, the only 15-membered macrolide, azithromycin (Azalide), is characterized by the most pronounced ability among all macrolides to accumulate in the cells of the reticulohistiocytic system of the body, as well as in other cells and tissues. Its concentration in alveolar macrophages exceeds the concentration in blood plasma by 240 times (!), and in neutrophils by approximately 40 times [2–6,8,11–14]. This explains the high efficiency and prolonged action of the drug. As a result of the ability of macrolides to accumulate intracellularly, a bactericidal effect of drugs is achieved against a group of intracellular pathogens, such as chlamydia, mycoplasma, legionella, borreliosis pathogens, etc. Moreover, very few antibiotic groups, in particular tetracyclines and fluoroquinolones, have a similar effect. The use of these antibiotics in pediatrics is limited. Tetracyclines are only approved for use in children over 8 years of age, and fluoroquinolones are not approved at all.
Many macrolides have a post-antibiotic effect, which means inhibition of bacterial activity after their short-term contact with a macrolide drug. This effect is based on irreversible changes in the ribosomes of microorganisms, resulting in a persistent block of translocation, due to which the antibacterial effect of the drug is enhanced and prolonged, which makes it possible to prescribe some of them (azithromycin) for a short course [14].
In addition, macrolides have a distinct anti-inflammatory activity that is not related to their antibacterial effect: they increase the sensitivity of bacteria to phagocytosis, enhancing it. This reduces the aggressiveness of microbes towards the tissues of the macroorganism and helps free it from infection [8,14].
Ease of use combined with a prolonged action effect. The vast majority of macrolide drugs are prescribed orally, and in children under 12 years of age, all macrolides are prescribed only orally.
Azithromycin and clarithromycin have the most optimal organoleptic properties, which also have special children's dosage forms (suspensions) that allow them to be widely used in early childhood.
Azithromycin, in addition, has unique pharmacokinetics even for the group of macrolides with minimal antibiotic content in the blood and significant intracellular accumulation of the drug, as well as its gradual elimination from the body. [8,15]. This feature of the drug allows you to take it, firstly, once a day. Secondly, on the first day a maximum dose of 10 mg/kg is administered, and then only a maintenance dose of 5 mg/kg. Thirdly, this same unique pharmacokinetic feature of azithromycin allows the use of short 3- or 5-day courses of therapy. Moreover, 5-day courses of antibiotics in children are indicated in cases of mild or moderate pneumonic process and sinusitis, since azithromycin exhibits the most distinct and long-lasting post-antibiotic effect against S. pneumoniae. For bronchitis, otitis, nasopharyngitis and tonsillopharyngitis, a 3-day course of therapy is usually sufficient. [8,16-18]
Efficacy of macrolides against diseases of the ENT organs and upper respiratory tract in children. Macrolides act on a fairly wide range of pathogens encountered in outpatient pediatric practice (nasopharynx and respiratory organs). They are included in the list of drugs recommended for the treatment of streptococcal and staphylococcal tonsillitis, mycoplasma and chlamydial tonsillopharyngitis, acute otitis media, sinusitis, bronchitis and pneumonia [11-13, 16-18]. In the treatment of paratonsillitis, epiglottitis, and retropharyngeal abscess, drugs are usually not used [12].
Azithromycin is particularly attractive in the treatment of upper respiratory tract pathology. In our republic, a number of studies have been conducted on the clinical effectiveness of various forms of azithromycin ( Azikar , production) for mild to moderate upper and lower respiratory tract infections at the outpatient stage.
One of the studies was conducted by us on the basis of the 10th children's clinical clinic in Minsk, which showed good treatment results in 16 patients using the suspension form of azicar [16]; another - I.E. Bovbel et al. [17] on the basis of the 17th children's clinic in Minsk, which showed good effectiveness and tolerability of the tablet form of azicar in children from 8 to 17 years old with mild and moderate forms of community-acquired pneumonia.
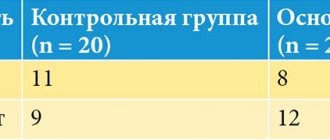
The third study [18] included 45 patients with respiratory tract infections of presumably streptococcal (pneumococcal) etiology (acute tonsillopharyngitis, acute bacterial rhinosinusitis, acute otitis media, infectious exacerbation of chronic obstructive pulmonary disease). The patients were randomized into two groups. The first group (25 people) received Azicar 500 mg orally once a day for 3 days. The second group (20 people) received amoxicillin 500 mg three times a day for 7-10 days, depending on the pathology. Patients with viral respiratory tract infections were not included in the study. The clinical effectiveness of treatment (normalization of body temperature, disappearance of leukocytosis and subjective improvement) in both study groups was comparable and amounted to 88% and 85%, respectively. During treatment, patients taking Azicar noted a more rapid disappearance of symptoms of the disease.
Efficacy of macrolides against the most common pathogens of community-acquired pneumonia. S. pneumoniae remains one of the leading pathogens of pneumonia, with chlamydia and mycoplasma taking second place. And if S. pneumoniae, according to recent studies, demonstrates only 4.3% of strains resistant to macrolides [19,20], then in relation to chlamydia and M. pneumoniae, macrolide antibiotics are practically the only active group of antibacterial drugs approved in pediatrics drugs. It should also be noted that in infants and preschool children, in 7–10% of cases, pneumonia is caused by H. influenzae, in which only azithromycin is active. Therefore, it is no coincidence that it is the drug of choice for mild and moderate pneumonia in this age group [19, 20].
The problem of chlamydial and mycoplasma infections. In recent years, chlamydial infection has become particularly relevant not only among the adult population, but also among children. In the course of analyzing the results of treatment of chlamydial vulvitis and urinary tract infections in children with azithromycin in comparison with erythromycin, it was found that in the group of children receiving azithromycin, a sanitizing effect was achieved in 94% of children, while therapy with erythromycin made it possible to achieve the effect of eliminating the pathogen only in 73% of cases [24]. A study of the effectiveness of treatment with azithromycin for juvenile chronic arthritis associated with chlamydial infection showed a certain effectiveness of long-term and repeated courses of this drug [25]. Azithromycin is also used to treat chlamydial and mycoplasma infections in newborns [26].
But the most important problem for pediatricians is the problem of respiratory chlamydia, the true prevalence of which has not yet been fully established. In a study by M.S. Savenkova (2005) [27], the use of a modern complex of clinical, laboratory and functional research methods made it possible to verify with a high degree of reliability the chlamydial etiology of respiratory diseases and determine their real frequency in the examined groups of children, which amounted to 18 for acute respiratory infections .5%, croup 15.4%, bronchitis 17.3%, bronchial asthma 27.4% and pneumonia 31.7%. Young children were infected predominantly with C. trachomatis, older children - with C. pneumoniae. 39% of children in the first 6 years of life were primarily infected with an acute form of the disease in the form of acute respiratory infections, croup and acute bronchitis. With age, the number of chronic forms of the disease increased in children, which occurred as an exacerbation of the underlying disease and required longer and repeated courses of treatment.
Macrolides are considered in children as first-choice drugs in cases where chlamydial etiology of respiratory disease is initially suspected. [8].
In a fairly large (262 patients) study conducted by M.S. Savenkova, M.P. Savenkov (2007), a positive clinical effect of the treatment of respiratory chlamydia was noted with the use of all groups of macrolides. Clinical efficacy was equally high (more than 90%) when using second-generation macrolides, and when using azithromycin it was 93.4%.
Macrolides are also the first choice drugs for mycoplasma etiology of respiratory diseases, which are characterized by prolonged (for 6 days or more) severe febrile fever, persistent obsessive, often nocturnal cough, and mycoplasma pneumonia is not uncommon. And in this case, almost all macrolides turned out to be effective, especially azithromycin and spiramycin (as second-line therapy) [8, 28].
Increasing incidence of allergic diseases in children. It should be noted that macrolides are generally recognized to be the least toxic of all groups of antibiotics and are well tolerated. They extremely rarely cause allergic reactions, which are so common when using β-lactam drugs. This, in fact, makes them an alternative group of antibiotics to β-lactams for respiratory pathologies. This same feature makes macrolides the drugs of choice in patients with allergies, primarily in children with atopic dermatitis, which is the most common allergic pathology in infants and preschool children. [8].
The problem of overcoming microbial resistance. To macrolides, a slower development of microbial resistance is recorded. In a number of European countries, such as France, Spain, and Hungary, the resistance of pneumococcus, the main causative agent of respiratory pathology, to penicillin has increased significantly and reached 40–58% of all strains isolated from patients [8, 20–22]. At the same time, such a significant change in resistance to macrolides over the same period of time was not noted. For example, for Russia, the problem of resistance of respiratory pathogens to macrolides, and, in particular, to azithromycin, is not yet significant. According to antibiotic resistance monitoring data, the frequency of isolation of azithromycin-resistant strains does not exceed 6.2% for S. pneumoniae and 7% for S. pyogenes, and no azithromycin-resistant H. influenzae strains have been identified. No clinically significant resistance to macrolides has been registered for atypical microbes: mycoplasmas, chlamydia, legionella [29].
It should be said that antibiotics of this group do not affect representatives of the family of intestinal bacteria, Pseudomonas aeruginosa and similar pathogens, as well as a number of anaerobic pathogens that cause severe purulent-inflammatory processes. The entry of antibiotics of this group into the cerebrospinal fluid and brain cells is extremely low. Therefore, macrolides are not used in the treatment of meningitis [8,11-13].
Low probability of developing dysbacteriosis during the use of macrolides. The lack of antibacterial activity of macrolides against gram-negative bacteria of the intestinal group, enterococci and a number of anaerobic bacteria makes them intact in relation to the aerobic and anaerobic components of the normal intestinal biocenosis. In other words, macrolides are not able to have any noticeable effect on the child’s intestinal microflora or disrupt its colonization resistance, i.e. are not capable of causing intestinal dysbiosis [8,11-13].
The problem of hemophilus influenzae infection in pediatrics. Haemophilus influenzae (especially Haemophilus influenzae type β) is a highly relevant causative agent of respiratory tract infection in children aged 6 months to 7 years. It accounts for at least 7–10% of diseases of the lower respiratory tract - pneumonia and bronchitis. In addition, Haemophilus influenzae plays a significant role as a causative agent of rhinopharyngitis and otitis media. In most cases, hemophilus influenzae infection is severe, with severe fever, intoxication and a large number of complications, including the development of a retropharyngeal abscess, epiglottitis, and purulent meningitis. The high sensitivity of the child's body in the first years of life to hemophilus influenzae infection and the large number of serious complications were the basis for the introduction of vaccination against this pathogen. However, at present, a layer of vaccinated children is just beginning to form, and this is a strong argument for the careful choice of macrolide antibiotics in children, primarily preschool and early age. The vast majority of 14- and 16-membered drugs do not have antibacterial activity against Haemophilus influenzae. The exception is the only 15-membered macrolide, azithromycin. Therefore, this drug has clear advantages when choosing a drug for the treatment of respiratory diseases in infants and preschool children. Especially in cases of severe intoxication and febrile reaction [8,11-13].
Treatment of helicobacteriosis and campylobacteriosis. There are other features of the antimicrobial spectrum of macrolides. Thus, clarithromycin is characterized by the greatest activity against Helicobacter and pronounced acid resistance, which was the basis for its inclusion in first-line treatment regimens for Helicobacter in both adults and children [21,23]. In addition, the Russian group for the study of Helicobacter pylori infection in children included azithromycin and roxithromycin in H. pylori eradication regimens. These same drugs have maximum activity against C.jejuni [8,22,23].
Additional immunomodulatory effect. A unique feature of macrolides, including azithromycin, is the ability to provide anti-inflammatory, immunomodulatory and mucoregulatory effects, complementing the antibacterial effect, which is of practical importance for the treatment of infectious processes in children, in most cases occurring against the background of changes in the immune system. The immunomodulatory effect of macrolides is realized by influencing phagocytosis, chemotaxis, killing and apoptosis of neutrophils in two phases. In the first phase, neutrophil degranulation and oxidative burst are stimulated, activating the body’s defense mechanisms. When using azithromycin, this phase develops quickly and also quickly subsides, so the resulting highly active free oxygen radicals do not have a damaging effect on the tissue. In the absence of infection, azithromycin is able to immediately suppress the oxidative burst, i.e. the early phase occurs only in the presence of a pathogen [6, 33]. Upon achieving eradication of pathogens, azithromycin inhibits the synthesis and secretion of pro-inflammatory cytokines (interleukins-1, -6 and -8, TNF-alpha) and, on the contrary, enhances the secretion of anti-inflammatory cytokines (interleukins-2, -4 and 10), which helps to minimize the severity of the inflammatory reaction (second phase of immunomodulation). [30-33].
Positive in some cases effect on cough. The high effectiveness of macrolide antibiotics for respiratory tract infections has another basis. It has been shown that under the influence of macrolides there is a suppression of mucus secretion due to a decrease in the secretion of chloride ions and water by bronchial epithelial cells. This mucoregulatory effect increases the clinical effectiveness of antibiotics in those respiratory diseases where mucus hypersecretion occurs. On the other hand, the “drying” effect of macrolides should be taken into account when prescribing them. The presence of a non-productive dry cough requires the simultaneous use of mucolytics that can quickly and effectively thin bronchial mucus (for example, acetylcysteine, ambroxol), and limit or eliminate drugs that have a “drying” effect (first generation antihistamines, for example). It should be noted that infants and young children are especially prone to hypersecretion of bronchial mucus in response to an acute respiratory infection. The mechanism of development of bronchial obstruction in the first years of life is associated with this. Therefore, the “drying” mucoregulatory effect of macrolides may be useful in certain clinical situations [8]. Thus, the main approaches to prescribing modern macrolides are as follows (Table 3).
Table 2. Indications for the use of macrolides in modern conditions.
| Pathology in which macrolides are the first choice drugs | Preferred Use | "Alternative or reserve antibiotic" |
| Chlamydial etiology of the disease | In children with symptoms of intestinal dysbiosis | Ineffectiveness of β-lactam antibiotics within 72 hours of use |
| Mycoplasma etiology of the disease | Atopic dermatitis (allergy) | |
| Intolerance to β-lactam antibiotics |
Side effects. In conclusion, we should dwell on the side effects of macrolide antibiotics. They are the least toxic of all groups of antibiotics and are well tolerated. However, the frequency of side effects, mainly from the gastrointestinal tract, when using them can reach from 5 to 26%. [8, 11-13, 23]. Most often, intestinal dysfunction due to the prokinetic effect is observed with the use of erythromycin. The so-called new macrolides, i.e. drugs of a later generation demonstrate this side effect relatively rarely (usually with a frequency in the range of 2–4%). Intestinal dysfunction is mainly observed in 14-membered drugs (clarithromycin, roxithromycin); in 16-membered drugs (spiramycin, midecamycin, josamycin) it is much less common. With azithromycin, this manifestation occurs in no more than 2.5% of cases [8,23]. Macrolides extremely rarely cause allergic reactions, which are so common when using β-lactam drugs. This, in fact, makes them an alternative group of antibiotics to β-lactams for respiratory pathologies. This same feature makes macrolides the drugs of choice in patients with allergies, primarily in children with atopic dermatitis, which is the most common allergic pathology in infants and preschool children. [8, 23, 34]. Serious side effects of macrolide antibiotics include cholestatic hepatitis, which is characterized by an increase in liver size and an increase in the level of transaminases in the blood. They develop with the use of josamycin, clarithromycin, spiramycin and large doses of erythromycin. High doses of erythromycin and spiramycin may prolong the QT interval and cause ventricular tachycardia, i.e. may affect myocardial conductivity. These side effects require discontinuation of macrolide therapy. [34]. Fortunately, such side effects are extremely rare, mainly when using large doses of erythromycin and are described as exclusive observations. But nevertheless, you should know and remember about them [8, 34].
References.
- Talashova S.V. Some aspects of the use of antibacterial drugs in pediatrics using the example of macrolides. // RMJ, 2009. – No. 7. – P. 464 – 468.
- Antibacterial therapy.//Practical guide, ed. L.S. Stravinsky, Yu.B. Belousov, S.N. Kozlov./ M., 2000, – 200 p.
- Namazova L.S., Tatochenko V.K., Bakradze M.D., Volkov K.S., Nisevich L.L. The use of modern macrolide antibiotics in pediatric practice.//Medical Council. – 2007. – No. 1. – From 34 – 37.
- Possibilities of using modern macrolides in pediatric practice. MA. Mamaeva. Terra medica nova. Magazine for doctors of all specialties.
- Beloborodova N.V. and others. Methodological recommendations No. 49 of the Moscow Department of Health. - M, 2005. - 30 p.
- Mazankova L.N., Ilyina N.O. The place of azalides in pediatric practice.//Breast cancer. - 2008. - No. 3. – P.121 – 124.
- Keshishyan E.S., Semina G.Yu. Evaluation of the clinical effectiveness of the drug “Zitrocin” in the treatment of various infectious and inflammatory diseases in children. // Bulletin of pediatric pharmacology and nutrition. – 2007. – vol. 4. – No. 5. – pp. 35–39.
- Samsygina G.A. The place and role of macrolide antibiotics in pediatrics. // Consilium medicum (Pediatrics appendix). – 2007. – No. 2. — P.96-100.
- Bryskier A, Agouridans C, Gasc JC. Classification of macrolide antibiotic. In Bryskier AJ, Butzler JP, Neu HC, Tulkens PM, eds., Macrolides, Chemistry, Pharmacology and Clinical Uses. Paris: Arnette-Blackwell, 1993. - R 5 - 66.
- Zaprudnov A.M., Mazankova L.N., Grigoriev K.I. New macrolides in pediatrics. // Library of a practicing physician (Current issues of modern medicine). – M., 1998. – 48 p.
- Strachunsky L.S., Kozlov S.N. Macrolides in modern clinical practice. — ISBN 5-88590-837-0.
- Strachunsky L.S., Kozlov S.N. Modern antimicrobial chemotherapy. Guide for doctors. - M.: Borges, 2002. - 432 p.
- Rational antimicrobial pharmacotherapy. Ed. V.P. Yakovlev and S.V. Yakovlev. M.: Litera, 2003. – C102 – 111.
- Hand V.N., Hand D.L. Mechanisms of accumulation and release of azithromycin in human polymorphonuclear leukocytes. Antibiotics and chemotherapy. – 2002. – T. 47. – No. 7. – P. 6 – 12.
- Antibacterial therapy. Practical guide. Ed. L.S.Strachunsky, Yu.B.Belousov, S.N.Kozlov. M., 2000. – 215 p.
- Ermakova O.E., Bomberova L.A., Nazarenko O.N. Experience in the use of azikar in the treatment of children with diseases of the respiratory tract and ENT organs in a day hospital. //Recipe. – 2004. – No. 6. – P. 24 – 26.
- Bovbel I.E., Malyugin V.Yu., Efimenko S.E., Voronovich E.L. Clinical effectiveness of azithromycin (Azicar) in the treatment of community-acquired pneumonia in children and adolescents. //Medical panorama. – 2008. – No. 12. – P. 31 – 33.
- Kachanko E.F. Macrolides: drugs of choice or alternative in the treatment of pneumococcal infections? //Medical panorama. – 2008. – No. 1. – P. 6-8.
- Strachunsky L.S., Krechikova O.I., Reshedko G.K. and others // Klin. microbiology and antimicrobial chemotherapy. – 1999. – No. 1. — P. 31 – 40.
- Tatochenko V.K. For every day pediatrician – 2002. Reference book on drug therapy. /M., 2002. – P. 132 – 137.
- Geslin P, Buu-Hoi A, Flemaux A et al. Antimicrobial resistance in Streptococcus pneumoniae: an epidemiological survey in France 1970–1990. Clin Infect Dis 1992; 15:95–98.
- Linares J, Pallares R, Alonso T et al. Trends in antimicrobial resistant of clinical isolates of Streptococcus pneumoniae in Bellivitge hospital, Barselona, Spain (1979–1990). Clin Infect Dis 1992:15:99–105.
- Marton A. Pneumococcal antimicrobial resistance: the problem of Hungary. Clin Infect Dis 1992:15:106–11.
- Zaprudnov A.M., Mazankova L.N., Grigoriev K.I. New macrolides in pediatrics. // Library of a practicing physician (Current issues of modern medicine). – M., 1998. – 48 p.
- Hercogava J. et al. Roxytromycin in the treatment.// 5th Eur. Congr. Clin. Microbiol. and Infect. Dis. – Oslo, 1991. – Abstr.80.
- Evsyukova I.I. Current problems of intrauterine chlamydial infection in newborns. // Materials of V Ross. National Congress "Man and Medicine". – M., 1998. – P. 270.
- Savenkova M.S. Chlamydial and mycoplasma infections in pediatric practice. Pediatrics. – 2005. – T.7. — No. 1. P. 439 – 442.
- Savenkova M.S., Savenkov M.P. Antibacterial therapy of respiratory chlamydia in children. Pediatrics. 2007. - No. 2. - P. 30 - 35.
- Kozlov R.S., Sivaya O.V., Shpynev K.V. Antibiotic resistance of Streptococcus pneumoniae in Russia in 1999–2005: results of multicenter prospective studies of PeGAS-I and PeGAS-II // KMAH. – 2006. – No. 8. – P.33–47.
- Labro MT. Interaction of macrolides and quinolones with the host defense system. Eur Bull Drug Res 1993; 2 (suppl 1): 7–13.
- Kadota J., Mizunoe S., Kishi K., et al. Antibiotic–induced apoptosis in human activated peripheral lymphocytes.// Inf. J. Antimicrob. Agents. – 2005. – No. 25 (3). – P. 216–220.
- Kolling UK, Hansen F, Braun J, et al. Leucocyte respons and anti-inflammatory cytokines in community-acquired pneumonia. // Thorax. – 2001. – No. 56. – P. 121–125.
- Karpov O.I. Macrolides: a new paradigm - pharmacodynamics/immunomodulation. // Clinical pharmacology and therapy. – 2005. – T.14. - No. 5. – P. 564 – 566.
- Comparative analysis of the tolerability of macrolide antibiotics used in pediatric practice. Ex press information. Bulletin. – 1999. No. 3. pp. 3–5.
Nazarenko O.N., Zagorsky S.E., Ermakova O.E., Bomberova L.A.
Spectrum of activity of macrolide antibiotics
Macrolides are broad-spectrum antibiotics. They show high activity against gram-positive cocci (S.pyogenes, S.pneumoniae, S.aureus), only MRSA is not included in this group. Also, macrolide antibiotics are used to eradicate the pathogens of whooping cough and diphtheria, Legionella, Moraxella, Campylobacter and Listeria. Macrolides are often indispensable for diseases caused by spirochetes, ureaplasmas, chlamydia and mycoplasmas. The use of macrolides is also effective for anaerobic infections (except for cases of infection with B.fragilis).
It is important to note that azithromycin (belonging to semi-synthetic drugs) has a stronger effect on Pseudomonas aeruginosa than others in the group of macrolides. In turn, clarithromycin is superior to other drugs in its effect on Helicobacter pylori and atypical mycobacteria.
Some macrolide antibiotics (azithromycin, spiramycin and roxithromycin) are active against protozoa such as Toxoplasma gondii and Cryptosporidium spp..
It is important to remember that a number of microorganisms are not sensitive to macrolide antibiotics. These include bacteria of the Enterobacteriaceae, Pseudomonas and Acinetobacter families.
Pharmacokinetics of macrolides
Macrolides, after oral administration, behave differently: it all depends on the type of drug and the presence of food at the time of taking the antibiotic, which can reduce the bioavailability of, for example, erythromycin, and to a lesser extent affect the absorption of antibiotics such as azithromycin and roxithromycin. At the same time, among macrolides there are antibiotics whose pharmacokinetics are not related to food intake - clarithromycin, spiramycin and josamycin.
Plasma protein binding among macrolides also varies. The highest concentrations of the antibiotic in the blood serum are observed after taking roxithromycin, since more than 90% of the drug is bound to blood proteins. For spiramycin this figure is minimal - 20%.
The distribution of macrolide antibiotics in the body occurs by creating high concentrations in the tissues of the body. These drugs are able to accumulate at the site of inflammation and quickly suppress the infection. In this case, the most active macrolides should be considered azithromycin and clarithromycin, which are capable of suppressing inflammation in the early stages, even long-term, since they create high tissue concentrations of the active substance. At the same time, it should be noted that drugs from the macrolide group have a positive effect on inflammatory factors, ensuring their direct anti-inflammatory effect of these antibiotics.
An important advantage of macrolide antibiotics is their ability to penetrate the cell wall, which ensures their activity against intracellular pathogens, which is especially important in the treatment of infections caused by atypical pathogens and STDs.
The process of macrolide metabolism occurs, in turn, mainly through the liver with the participation of cytochrome P-450. Metabolites are excreted mostly through bile; 5 to 10 percent is excreted through the kidneys; T1/2 varies for different molecules and ranges from 1 hour for medicamicin to 55 hours for azithromycin. In liver cirrhosis, the half-life of drugs such as erythromycin and josamycin can significantly increase; the prescription of these macrolides for this pathology requires special precautions. However, renal failure has virtually no effect on the half-life of macrolide antibiotics. The only exceptions are clarithromycin and roxithromycin.
Antibiotics of the macrolide group are practically unable to overcome the blood-brain and blood-ophthalmic barriers. The hematoplacental barrier is passable for macrolides, and they are also able to penetrate into breast milk, which imposes some restrictions on their use during pregnancy and breastfeeding, despite the lack of a teratogenic effect.
The use of macrolides in children in modern conditions
Through chemical and microbiological transformation, so-called semi-synthetic antibiotics have been created that have new, medically valuable properties: acid and enzyme resistance, an expanded spectrum of antimicrobial action, better distribution in tissues and body fluids, and fewer side effects. Based on the type of antimicrobial action, antibiotics are divided into bacteriostatic and bactericidal, which is of practical importance when choosing the most effective therapy. A comparative analysis of antibiotics is based on indicators of their effectiveness and safety, determined by the severity of the antimicrobial effect in the body, the rate of development of resistance of microorganisms during treatment, the absence of cross-resistance in relation to other chemotherapy drugs, the degree of penetration into lesions, the creation of therapeutic concentrations in the patient’s tissues and fluids, and the duration of their maintenance, the preservation of action in various environmental conditions. Important properties are also stability during storage, ease of use with different methods of administration, high chemotherapeutic index, absence or mild toxic side effects, as well as allergization of the patient. A discussion of the place of antibiotics in the treatment of bacterial infections in childhood cannot be complete without addressing the problem of antimicrobial resistance. Due to the repeated and often unjustified prescription of antibiotics, the incidence of infections caused by microorganisms that have become resistant to the antibiotics used is increasing throughout the world. The growth in the number of patients with immunodeficiency, the introduction of new invasive medical techniques, mutations of the microorganisms themselves, and some others also play a role in the formation of resistance. Antibiotic resistance is currently leading to increased morbidity, mortality and healthcare costs worldwide. Due to the rapid increase in resistance, problems arise especially acutely in the treatment of bacterial infections in childhood. Of particular importance is the resistance to penicillin and cephalosporin of Streptococcus pneumoniae, the multidrug resistance of Haemophilus influenzae (insensitive to ampicillin, chloramphenicol, tetracycline and trimethoprim), the rapid spread of penicillin-resistant Neisseria meningitidis. Methicycline-resistant strains of Staphylococcus aureus are increasingly being discovered; All over the world, doctors are faced with multidrug resistance in Enterobacteriaceae (thus, the number of isolated cultures of Klebsiella and Enterobacter species that are insensitive to third-generation cephalosporins is increasing). Resistance of Salmonella and Shigella species is developing, in particular, to trimethoprim and cephalosporins, enterococci to vancomycin, and group A streptococci to erythromycin. Although the emergence of antibiotic resistance may be an inevitable result of widespread use, the problem of resistance can certainly be reduced in practice. For example, in Holland the use of systemic antibiotics is limited by the state program and the problem of resistance is not so acute. In recent years, many new antibiotics of different pharmacological groups have been introduced into medical practice. However, the group of macrolides currently attracting the greatest attention from clinicians. This is facilitated by the increasing frequency of drug allergies to penicillins and cephalosporins in the pediatric population, as well as the ineffectiveness of b-lactams for infections caused by intracellular pathogens. Macrolides are now one of the most rapidly developing classes of antibiotics due to their high efficiency and relative safety. They have a wide spectrum of antimicrobial activity and favorable pharmacokinetic properties, combine high efficiency in the treatment of infections and good tolerance by patients. The first macrolide antibiotic synthesized in 1952 was erythromycin, obtained by Waksman from the soil fungus Streptomyces erythreus. Three years later, two more macrolide drugs appeared - spiramycin and oleandomycin. For a long time, erythromycin remained the only alternative in the treatment of many bacterial infections in children allergic to b-lactams. In recent years, a real scientific breakthrough has occurred: several, in a certain sense, unique in their qualities, drugs have been created that hold a “high bar” to this day: azithromycin (Zithrocin, etc.), roxithromycin, clarithromycin, spiramycin, etc. Macrolides got their name due to the presence of a macrocyclic lactone core. Depending on the number of carbon atoms in the lactone ring, macrolides are divided into 3 subgroups: • 14-membered (erythromycin, oleandomycin, roxithromycin, clarithromycin); • 15-membered (azithromycin); • 16-membered (spiramycin, josamycin, midecamycin). One of the general properties of macrolides is a bacteriostatic effect, which is caused by disruption of protein synthesis in the microbial cell through reversible binding to the 50S ribosomal subunit. The bacteriostatic effect in this case has its own characteristics. On the one hand, the microbial agent is not completely destroyed, but on the other hand, there is no effect of additional intoxication of the body due to the action of toxins released from the destroyed microbial cell. When high concentrations of the antibiotic accumulate at the site of infection, macrolides have a so-called post-antibiotic effect, which means suppression of bacterial activity when the effect of the drug has theoretically ceased. The mechanism of this effect is not fully understood. Macrolides are weak bases, their antimicrobial activity increases in an alkaline environment. At pH 5.5–8.5, they penetrate more easily into the microbial cell and are less ionized. Macrolides are metabolized in the liver, and, as a rule, more active metabolites are formed. The main route of elimination is through the gastrointestinal tract (about 2/3 of the drug), the remaining amount is excreted through the kidneys and lungs, so dose adjustment of macrolides is required only in cases of severe liver failure. 14-member macrolides have an important additional property: they exhibit an anti-inflammatory effect by increasing the production of endogenous glucocorticoids and changing the cytokine profile due to activation of the hypothalamic-pituitary-adrenal system. In addition, the stimulating effect of macrolides on neutrophil phagocytosis and killing has been established. Food has a multidirectional effect on the bioavailability of macrolides: it does not affect the absorption of telithromycin, clarithromycin, josamycin and midecamycin acetate; slightly reduces the bioavailability of midecamycin, azithromycin and significantly reduces the bioavailability of erythromycin and spiramycin. Concomitant use with lipid-rich food increases the bioavailability of the tablet form of azithromycin. The pharmacokinetics of macrolides is characterized by a pronounced dependence on the pH of the environment, when it decreases, ionization at the site of inflammation increases and part of the drug is converted into inactive forms. The optimal effect of erythromycin, clarithromycin and especially azithromycin occurs at pH>7.5. Macrolides penetrate well into the cells of the human body, where they create high concentrations, which is fundamentally important for the treatment of infectious diseases caused by intracellular pathogens (Mycoplasma spp., Chlamydia spp., Legionella spp., Campylobacter spp.). With the exception of roxithromycin, the content of macrolides in monocytes, macrophages, fibroblasts and polymorphonuclear leukocytes is tens, and for azithromycin hundreds of times higher than their serum concentration. An important feature of macrolides is their ability to accumulate in phagocytes with subsequent release at the site of infection under the influence of bacterial stimuli and the active recapture of the drug “not utilized” by microorganisms. The maximum accumulation of macrolides is observed in lung tissue, fluid lining the mucous membranes of the bronchi and alveoli, bronchial secretions, saliva, tonsils, middle ear, sinuses, gastrointestinal mucosa, prostate gland, conjunctiva and eye tissues, skin, bile, urethra, uterus, appendages and placenta. Metabolism of macrolides is carried out in the liver by enzymes of the cytochrome P450 system. According to the degree of affinity for enzymes, all macrolides can be divided into three groups: a) oleandomycin and erythromycin have the greatest affinity; b) clarithromycin, midecamycin, josamycin and roxithromycin are characterized by weak affinity; c) when using azithromycin, dirithromycin and spiramycin, competitive binding with enzymes does not occur. The half-life (T1/2) differs for different macrolides and may depend on the dose: azithromycin has the longest T1/2 - up to 96 hours, the shortest - erythromycin and josamycin - 1.5 hours (Table 1). Macrolides are excreted from the body mainly with bile, undergoing enterohepatic recirculation. In addition to the direct antimicrobial effect on the cell, some macrolides are distinguished by properties that enhance their effectiveness in the conditions of the macroorganism. Among them: •? post-antibiotic effect, which manifests itself in the absence of the effect of resumption of bacterial growth, despite the removal of the antibiotic from the body. •? subinhibitory effect, but it is difficult to use in therapeutic regimens, since the use of antibiotics in subinhibitory concentrations may cause an increase in resistance to it. It is used as a test to assess the distribution of a bacterial population according to the degree of antibiotic sensitivity and the proportion of resistant individuals in it, a high number of which may indicate signs of the formation of resistance. Macrolides are an undisputed alternative in case of allergy to b-lactams in the treatment of tonsillitis, sinusitis, otitis, bronchitis, pneumonia, skin and soft tissue infections (Table 1). Considering that macrolides have an equally good effect on both extracellular and intracellular pathogens, they have become first-line antibiotics in the treatment of many urogenital infections and so-called atypical bronchopulmonary infections caused by chlamydia, mycoplasma, etc. Macrolides are also used in gastroenterology and are increasingly included in treatment regimens for chronic gastroduodenitis associated with H. pylori (for example, clarithromycin). Macrolides are first-line antibiotics in the treatment of whooping cough in children (moderate and severe forms), and are included in the complex of therapeutic measures for diphtheria of the pharynx. Resistance to macrolides does not yet pose serious problems in most regions of Russia, as evidenced by the results of the multicenter study PeGAS-I. According to the data presented, the prevalence of resistant clinical strains of S. pneumoniae is within 4%. Modern macrolides have convenient release forms: from tablets with different dosages to suspensions and syrups, which can be prescribed to children even at an early age. Some macrolides are available in the form of ointments for external use (erythromycin), and also have forms for parenteral administration (erythromycin, clarithromycin, azithromycin), which makes their use possible in emergency situations. All new macrolides are significantly superior in their pharmacological properties to both erythromycin and midecamycin, have a more prolonged effect, are designed to be taken 1-2 times a day, and have significantly fewer side effects. But in other qualities these drugs have differences, sometimes significant. The absorption of azithromycin depends on the timing of meals. Bioavailability is considered to be greatest for roxithromycin (72–85%) and clarithromycin (52–55%) compared to azithromycin (37%), spiramycin (35%), etc. From the 50s of the last century to the present day, macrolides have been used with high efficiency, especially for pathologies of the upper respiratory tract. In terms of frequency of use, macrolides occupy third place among all classes of antibiotics, and in the treatment of tonsillitis they compete with penicillins. According to T.I. Garashchenko and M.R. Bogomilsky [3], this is due to a number of reasons: 1. High degree of accumulation of macrolides in lymphoid tissue. 2. Efficiency (up to 90%) in patients with tonsillopharyngitis. 3. Increased frequency of isolation from the tonsils (especially with recurrent tonsillopharyngitis) of microorganisms producing b-lactamases capable of destroying penicillins, first generation cephalosporins (M. catarrhalis, St. aureus) and high activity of macrolides against these pathogens. 4. An increase in the frequency of atypical pathogens (M. pneumoniae, CI. pneumoniae) in the etiology of acute and recurrent tonsillopharyngitis, adenoids (up to 43%), inaccessible to penicillins (including protected ones), cephalosporins, aminoglycosides, lincosamides. 5. Few side effects compared to other antibiotics. 6. No effect on the microflora of the intestines and pharynx, moderate antifungal effect. 7. High safety range, allowing the dose of macrolide (azithromycin) to be doubled to achieve a bactericidal effect. 8. High compliance due to short courses of treatment (3–5 days for azithromycin) and ease of administration of the drug (once a day for azithromycin). 9. Activity of some macrolides against H. influenzae (azithromycin). 10. The absence of competitive interaction between azalides and antifungal and antihistamine drugs, which allows for combination therapy in children with allergic manifestations and mycoses. 11. High activity of macrolides not only against nonspecific pathogens of pharyngeal diseases (GABHS, St. aureus, Str. pneumonia), but also specific ones - N. meningitides, N. gonorrhoeas, Treponema pallidum, Legionella pneumonia, Lisferia monocytogenes, Coryne-bacterium diphtheriae, activity against anaerobes - causative agents of paratonsillitis. 12. Immunomodulatory effect. Despite the large number of positive criteria, in the last few years there has been some caution regarding the use of macrolide antibiotics due to reports of an increase in resistance to them in vitro in a number of countries (France, Italy, Spain), which, however, is not accompanied by reports of corresponding this increase in clinical ineffectiveness of macrolide antibiotics. Moreover, the high safety of macrolide antibiotics, and primarily azithromycin, allows the use of new dosage regimens (treatment of acute otitis media with a single dose) and their improvement to achieve a better bactericidal effect in patients with a burdened premorbid background. Thus, R. Cohen [cit. according to 4], analyzing the clinical and bacteriological effectiveness of treatment of chronic tonsillitis with azithromycin at a course dose of 30 and 60 mg/kg, taken for 3 days, notes that bacteriological effectiveness at a dose of 30 mg/kg was registered only in 58% of cases, whereas with 60 mg/kg – achieved 100% bacteriological eradication of the pathogen, comparable to a 10-day course of penicillin (95%). The cost of macrolides in the modern pharmaceutical market varies widely: from expensive original drugs, undoubtedly of higher quality, to more affordable generics, some of which are also of good quality (zitrocin, clerimed, roxihexal, etc.), which ensures accessibility drugs of this group to all segments of the population. But the doctor should not only be guided by the price of the drug when prescribing treatment for a child. An analysis of the clinical effectiveness of various representatives of macrolides shows that the unreasonable and frequent prescription of a popular drug in one region throughout the year can negate the antimicrobial effect, since under these conditions protoplasts and L-forms are quickly formed. Macrolides are well tolerated and can be successfully used in children from birth. However, this does not apply to clarithromycin and azithromycin suspension, the safety and effectiveness of which have not been studied in children under 6 months of age. Doses of macrolides used in children are presented in Table 2. Adverse reactions requiring discontinuation of the drug: allergic reactions - anaphylaxis and Quincke's edema (extremely rare); acute cholestatic hepatitis; cardiotoxic effect (prolongation of the QT interval, arrhythmias); pseudomembranous colitis; acute interstitial nephritis; reversible hearing loss. Adverse reactions that require attention if they persist for a long time and/or are poorly tolerated: allergic reactions (urticaria, itchy skin); pain at the injection site; reactions from the gastrointestinal tract (nausea, vomiting, changes in taste, pain and discomfort in the abdomen, diarrhea); dizziness and headache (extremely rare). The most typical adverse reactions are observed in the gastrointestinal tract. In the case of azithromycin and clarithromycin, their frequency rarely reaches 12%, but when using erythromycin base it can increase to 32%. With the use of josamycin, clarithromycin, spiramycin and high doses of erythromycin (? 4 mg/day), acute cholestatic hepatitis is possible. When prescribing high doses of erythromycin in terms of 36 hours to 8 days, a reversible hearing loss is possible. High doses of erythromycin, teelithromycin and spiramycin can cause extension of the QT interval and the occurrence of ventricular tachycardia such as “Torsades de Pointes”. Cross allergic reactions to all macrolides are extremely rare. Although macrolides can contribute to a change in the intestinal biocenosis, this acquires clinical value in very rare cases with the development of Clostridium dificille - ascified pseudo -dummy colitis, diarrhea, vaginal or oral candidiasis. Among the macrolide drugs, a special place is occupied by azithromycin, obtained and implemented in clinical practice in the early 90s of the XX century. This is the first representative of the new subgroup of antibiotics - azalids, in the structure of the lacton ring of which a nitrogen atom is contained. Such a restructuring of the erythromycin molecule gave the obtained compound new properties, including the expansion of the antimicrobial spectrum, the creation of high levels in tissues and cells significantly exceeding the concentration in the blood (tissue orientation of pharmacokinetics), and other properties that significantly distinguish it from the antibiotics of the macrolides group. Along with maintaining activity against gram -positive cocci of azithromycin (zyspin and others), it exceeds erythromycin against Haemophilus influenzae, Moraxella Catarrhalis, Neisseria spp., Campylobacler jejuni, Helicobacter pylori, Borrelia Burgdorferi. It is also active in relation to some enterobacteria: its value of the MPK90 in relation to Salmonella, SHIGELLA, E.Coli ranges from 4–16 mg/l. Azithromycin (zysprine and others) is active in relation to some “atypical” microorganisms, as well as intracellularly located pathogens - Chlamydia spp., Mycoplasma spp. and others. Azithromycin at various pH values is more stable than erythromycin. After taking a single dose in the stomach, more than 37% of azithromycin is absorbed compared to 25% of erythromycin. Food or simultaneous use of antacids reduces the bioavailability of azithromycin, and therefore it should be taken at least 1 hour before or 2 hours after eating. The concentration of azithromycin in tissues and cells exceeds 10-100 times detected in the blood; The intracellularly concentrates in the lysosomes. The average value of T1/2 of azithromycin is 2-4 days. In the recommended treatment conditions (3 and 5 days), the drug in effective concentrations is maintained within 7 or more days. When resolving the issue of repeated courses of antibacterial therapy, it is necessary to take into account the properties of azithromycin into the body's tissues, which allows reducing the duration of the course of treatment with azithromycin and provides a stagiotic effect. Azithromycin quickly includes in white blood cells (polynuclear, monocytes, lymphocytes), in high concentrations and is detected for a long time in alveolar macrophages, fibroblasts. During migration into the focus of infection, polynuclera plays a transport role, providing a high and long -lasting antibiotic level in tissues and cells. Even with the introduction of azithromycin in maximum doses, it creates low concentrations in the blood, but has high penetration into polynuclear (phagocytes), responsible for the clearance of pathogens from the focus of infection and blood channel. The drug is not metabolized in the patient’s body, does not inhibit the isoenzymes of the p450 cytochrome system. From the patient’s body is excreted mainly with feces and partially (~ 20%) in urine. Thus, modern synthetic macrolides (azithromycin, clarithromycin, roxytromycin) are characterized by a wide range of action: they are active against most gram -positive microorganisms, many gram -negative bacteria, “atypical” intracellular pathogens of respiratory infections; The spectrum of their actions also includes atypical mycobacteria, pathogens of a number of dangerous infectious diseases (rickests, brucelli, borrelia, etc.) and some simplest. They surpass natural macrolides not only in terms of breadth of the spectrum and degree of antibacterial activity, but also in the bactericidal effect on many pathogens. New macrolides (especially azithromycin) have improved pharmacokinetic properties: prolonged with pharmacokinetics (T1/2 of azithromycin, depending on the dose, is 48–60 hours), the ability to accumulate and linger for a long time in immunocompetent cells for 8-12 days after the completion of 3-5 —The day internship courses in a standard dose. The interest of pediatricians in azithromycin is due to its high degree of accumulation in the lymphoid tissue and long -term preserved concentrations of the drug, providing the bactericality of the effect, as well as rare side effects, the lack of effect on the normal microflora of the oral cavity and intestines, and a low probability of drug interaction. The tissue and cell orientation of kinetics, the prolonged effect of new macrolides, the possibility of their effective use in short courses without the risk of developing serious adverse reactions determine the low frequency of antibiotic resistance.
Literature 1. Strachunsky L.S., Kozlov S.N. Macrolides in modern clinical practice. Smolensk: Rusich, 1998. 2. Samsygina G.A., Bogomilsky M.R., Garashchenko T.I. Antibacterial therapy of acute respiratory diseases in children. Lectures on Pediatrics Volume 2. Ed. V.F. Demina, S.O. Klyuchnikova, G.A Samsygina. RGMU. Moscow, 2002 3. Garashenko T.I., Bogomilsky M.R. New approaches to the treatment of exacerbations of chronic tonsillitis in children. // Children's infections, No. 1 - 2004. 4. Lukyanov S.V. Clinical pharmacology of macrolides. Consilium medicum 2004; No. 6, p. 769–73. 5. Mizernitsky Yu.L., Sorokina E.V. Macrolides for respiratory tract infections: modern ideas about the mechanisms of action. Consilium medicum, Pediatrics, 2006; No. 2, c. 23–26.
Adverse reactions of macrolide antibiotics
Unlike other classes of antimicrobial drugs, adverse reactions during the period of taking antibiotics belonging to the macrolide group are quite rare. These drugs are generally easily tolerated by patients, including children, pregnant women and the elderly.
Below is a list of possible reactions during a course of antibacterial therapy with drugs from the macrolide group:
- From the gastrointestinal tract: abdominal discomfort, pain, nausea, vomiting, diarrhea, which can be caused by erythromycin, as it can have a prokinetic effect, stimulating intestinal motility. Less commonly, similar phenomena are observed when spiramycin and josamycin are prescribed.
- Adverse events from the liver are most typical for erythromycin. According to research, liver damage during macrolide therapy is 3.6 cases per 100 thousand, so in general, the course of antibacterial therapy is considered favorable. General malaise, weakness, abdominal pain, rarely fever, signs of jaundice are a consequence of cholestatic hepatitis. In this case, ALT and AST are observed. It is important to note that the risk of developing hepatotoxic reactions most often occurs due to the interaction of macrolides with other drugs; a very important indicator in this case is the presence of liver diseases.
- From the central nervous system, dizziness, headache, and very rarely hearing loss (with intravenous administration of macrolides in extremely high doses) are possible.
- From the cardiovascular system, changes may appear on the ECG - prolongation of the QT interval.
- Local reactions caused by intravenous use of macrolide antibiotics include the following: phlebitis and thrombophlebitis. It is important to take into account here that these drugs can only be administered dropwise; jet administration is contraindicated.
Allergic reactions, skin rash, and urticaria are not typical for macrolides and occur in very rare cases.
Popular drugs
In the list of macrolide antibiotics, there are two substances that are most commonly used at the moment:
- clarithromycin;
- azithromycin.
These are representatives of two different generations of macrolide drugs. From these, azithromycin was later obtained. Despite the fact that they are united by the mechanism of action on microbes and belonging to the same group, there are significant differences:
| Comparison parameter | Azithromycin | Clarithromycin |
| Microbial spectrum of action |
| |
|
| |
| Effect speed | Within 2-3 hours. A stable concentration of the drug in the blood appears after 5-7 days of regular use. | Within 2-3 hours. A stable concentration of the drug in the blood occurs after 2-3 days of regular use. |
| Efficiency | Equally effective in the treatment of Helicobacter gastritis. Azithromycin distributes better throughout the lung tissue when treating a pulmonary infection, however, the effectiveness of the drug is similar to clarithromycin in a similar case of administration. Azithromycin is more effective against legionellosis. | |
| Adverse reactions |
| |
|
| |
| Safety for pregnant and lactating patients |
| |
Thus, the advantages of azithromycin include fewer adverse reactions in the form of severe life-threatening conditions.
For clarithromycin, the advantages of use are a wider spectrum of action and rapid achievement of stable levels in the patient’s blood.
The main disadvantage for both macrolide antibiotics is their undesirable use in pregnant women, which complicates the choice of drug in this population group.
Indications for prescribing macrolide antibiotics
A course of antibacterial therapy with macrolide drugs is prescribed to patients with various infectious diseases:
- For upper respiratory tract infections: acute sinusitis, streptococcal tonsillitis, acute otitis media in children (the highest activity is observed with azithromycin, which is also prescribed for allergic reactions to penicillin). Separately, we should dwell on such a disease as streptococcal tonsillopharyngitis - drugs of the macrolide group in this case act as an alternative to penicillin, not being inferior to it in the effectiveness of suppressing the source of inflammation, so they can be prescribed to patients to prevent serious complications of tonsillopharyngitis (rheumatism and glomerulonephritis).
- For lower respiratory tract infections: chronic bronchitis in the acute stage, community-acquired pneumonia, including those caused by atypical pathogens.
- For “childhood infections”: whooping cough and diphtheria. In the latter case, erythromycin is prescribed, which is combined with anti-diphtheria serum.
- For infectious diseases of the skin and soft tissues: furunculosis, moderate and severe forms of skin acne (erythromycin or azithromycin is used), etc.
- For sexually transmitted infections, both in women and men: syphilis, chlamydia, ureaplasmosis, mycoplasmosis, chancroid, lymphogranuloma venereum.
- For infections of the oral cavity that affect the tissues surrounding the roots of the teeth - periodontitis, periostitis.
- Erythromycin is indicated for the treatment of campylobacter gastroenteritis, manifested by diarrhea, nausea, fever and abdominal pain.
- In the treatment of gastric and duodenal ulcers for the eradication of Helicobacter pylori, the administration of clarithromycin as part of a three- or four-component regimen is indicated.
- In the treatment of parasitic diseases of humans and animals: spiramycin, a natural antibiotic of the macrolide group, is most often used for the treatment of toxoplasmosis. For cryptosporidiosis, preference is given to spiramycin and roxithromycin.
- For the prevention and treatment of diseases such as mycobacteriosis caused by mycobacteria M.avium in patients with acquired immunodeficiency syndrome. The most effective drugs in this case should be clarithromycin and azithromycin.
- For the purpose of prophylactic use, drugs from the macrolide group are prescribed:
- people who have had contact with patients with whooping cough are prescribed erythromycin;
- for patients suffering from rheumatism who have an allergic reaction to penicillin, erythromycin is recommended as an alternative;
- for meningococcal carriage, spiramycin is recommended;
- in dentistry - azithromycin and clarithromycin;
- When performing intestinal decontamination in patients who are being prepared for colon surgery, erythromycin is prescribed in combination with kanamycin.
Macrolides and their importance in the treatment of community-acquired pneumonia of various etiologies
I.V. LESCHENKO
, Doctor of Medical Sciences, Professor,
Z.D.
BOBYLEVA , Doctor of Medical Sciences,
Ural State Medical University of the Ministry of Health of Russia, Yekaterinburg
The success of antibiotic therapy depends on the correctly chosen antibiotic, the timeliness of its administration, the state of the macroorganism (patient) and microorganism (resistance of the bacterial pathogen to the drug), bioavailability and bioequivalence . The latter applies to generic drugs, which are so widely represented on the domestic pharmacological market.
Macrolide antibiotics occupy one of the leading places in the antibacterial therapy of community-acquired pneumonia (CAP) of various etiologies. According to their pharmacokinetic characteristics, macrolides are classified as tissue antibiotics. Features of the pharmacokinetics of the antibiotics most often prescribed in the treatment of CAP (beta-lactams and macrolides) include the ability of macrolides to be more concentrated at the site of infection than in the blood plasma ( Table 1
) [1].
| Table 1. Pharmacokinetics of beta-lactams and macrolides | |
| Beta-lactams | Macrolides |
| Serum concentration = concentrations at the site of infection | The concentration at the site of infection is greater than the concentration in the blood plasma |
| Ability to extrapolate in vivo MIC results obtained in vitro | Difficult to extrapolate in vivo MIC results obtained in vitro |
One of the macrolide antibiotics widely represented on the pharmacological market is azithromycin.
It has been proven that azithromycin can act not only bacteriostatically, like other macrolides, but also, unlike antibiotics of this class, bactericidal. The bactericidal effect is achieved due to the ability of azithromycin to create very large intracellular concentrations against many pathogens located inside cells [2]. Already on the first day of administration, azithromycin creates concentrations at the site of infection, mainly in alveolar macrophages, many times higher than the minimum inhibitory concentration (MIC) ( Fig. 1, 2
) [3].
A feature of azithromycin is the ability to create not only high concentrations at the site of infection, but also to provide a drug concentration several times higher than the MIC after a 3-day dose for 7 days, which practically corresponds to 10 days of antibacterial therapy [4].
Azithromycin exhibits a post-antibiotic effect and post-antibiotic sub-MIC, i.e., an effect on microorganisms after exposure to subinhibitory concentrations of the antibiotic not only against Streptococcus pneumoniae, but also against Streptococcus pyogenes, Haemophilus influenzae, Legionella pneumophila. Azithromycin is the only macrolide with natural activity against Haemophilus Influenzae, and it is superior to clarithromycin in the duration of post-antibiotic effect in Haemophilus Influenzae and Legionella pneumophila [5].
Azithromycin and other macrolides are known to have immunomodulatory and anti-inflammatory effects [6]. The uniqueness of azithromycin not only as an antibiotic with antibacterial but also immunomodulatory properties may be associated with the special structure of the molecule. According to its chemical structure, azithromycin is a 15-membered macrolide and its fundamental difference from the “classical” 14-membered macrolides is that its molecule contains a nitrogen atom. In an experiment on healthy volunteers who took azithromycin at a dose of 500 mg per day for 3 days, a biphasic immunomodulatory effect of the drug was demonstrated [7]. The early immunomodulatory effect of azithromycin manifests itself in enhancing the body's natural immune response to infection, while the late (delayed) anti-inflammatory effect of the antibiotic helps resolve inflammation. Macrolides, and in particular azithromycin, increase the activity of T-killers. They accumulate in neutrophils, monocytes and macrophages, enhance their migration to the site of inflammation, increase phagocytic activity, and stimulate the secretion of interleukins IL-1, IL-2, IL-4. In addition, azithromycin accelerates neutrophil apoptosis after pathogen eradication. The anti-inflammatory effect of macrolides is associated with a decrease in airway hyperreactivity, which usually accompanies bronchopulmonary infections [6, 8]. The mechanisms of the immunomodulatory action of azithromycin are shown in Figure 3
.
An important condition when choosing an antibiotic is the expected frequency and severity of adverse events. Azithromycin, like macrolides in general, is one of the least toxic antibiotics [9]. More often than other adverse events when using it, adverse reactions from the gastrointestinal tract are observed (<12%). They are usually mild and, as a rule, do not require discontinuation of the drug. With parenteral use of azithromycin, pain at the site of venipuncture and post-infusion phlebitis are observed, which are recorded in 6.5 and 3% of cases, respectively [10]. Adverse events requiring discontinuation of the drug are significantly less common (<3%): rash, persistent diarrhea, nausea and vomiting, laboratory signs of cytolysis and cholestasis, abdominal pain and drowsiness. Allergic reactions are also extremely rare [9]. A characteristic feature of allergic manifestations when using azithromycin is the resumption of allergic reactions in the long term after the cessation of symptomatic therapy, which requires 3-4 weeks of observation of the patient. Slightly more common macrolide intolerance
observed when antibiotics are prescribed in high doses. However, even with intravenous administration of 4.0 g of azithromycin solution, the incidence of abdominal pain and nausea does not exceed 0.5%.
One of the important aspects of the safety of antibiotics is the determination of their cardiotoxicity associated with the effect on the conduction system of the heart. The results of the studies convincingly indicate the cardiovascular safety of macrolides. The incidence of life-threatening arrhythmias with their use is extremely low and does not exceed 1 case per 100 thousand prescriptions [11]. In an experiment (Poluzzi E. et al.) and in a study by H. Svanstrom et al. It was found that among macrolides, azithromycin has the least arrhythmogenic potential [12, 13].
As for hepatotoxicity, compared to many antibiotics, azithromycin has the lowest frequency of hepatotoxic reactions, including compared to other macrolides ( Fig. 4
) [14, 15].
In this regard, the widespread myths about the hepato- and cardiotoxicity of macrolides (azithromycin) are unacceptable, since this can lead to excessive consumption of the remaining classes of antibiotics and an increase in the resistance of microorganisms [16].
According to national and international recommendations for CAP, azithromycin is used for the treatment of non-severe CAP both as monotherapy (group 1 of patients with CAP) and as combination antibacterial therapy (ABT) (group 2) [17, 18].
Indications for prescribing macrolides for mild cases of CAP are:
• suspicion of an “atypical” etiology of the disease (Mycoplasma pneumoniae, Chlamydia pneumoniae, Legionella spp.); • allergy to β-lactams; • lack of effect when treated with β-lactams. Based on national recommendations for community-acquired pneumonia in adults, we have developed an algorithm for the management of patients with CAP in an outpatient setting, presented in Tables 2 and 3
[19].
| Table 2. Patients with non-severe pneumonia without concomitant diseases who have not taken any medication in the last 3 months. antibacterial drugs (group 1) | ||
| Frequency of visits to the local doctor | Name of studies (frequency) | Name of antibiotic (all antibiotics are prescribed orally) |
| 4 times 1st - when visiting a doctor - making a diagnosis (clinically), determining the severity of the patient’s condition and indications for outpatient treatment, ordering a blood test and an x-ray examination of the chest organs. 2nd - after 3-4 days of antibacterial therapy: clinical assessment of the effectiveness of treatment (improvement of well-being, reduction or normalization of temperature), assessment of x-ray data and blood tests. 3rd - after 7-10 days of antibacterial therapy to decide whether to discontinue antibiotics or continue treatment (antibiotics are continued for 3 days after body temperature normalizes). 4th - 14-16 days from the start of treatment to resolve the issue of the patient’s ability to work | 1. General blood test 2 times. 2. X-ray (large-frame FG*) of the chest in 2 projections, 2 times. Studies are carried out on the 1st-3rd and 14-16th days of illness from the day the patient contacts the doctor | Drugs of choice (one antibiotic is prescribed): • Amoxicillin 500-1,000 mg 3 times a day; • Azithromycin 500 mg 1 time/day (course dose 1.5 g); • Clarithromycin SR 1000 mg 1 time/day; • Clarithromycin 500 mg 2 times/day * FG here and in Table 3 fluorography. |
| Table 3. Patients with non-severe pneumonia with concomitant diseases and/or who have taken over the past 3 months. antibacterial drugs? 2 days (2nd group) | ||
| Frequency of visits to the local doctor | Name of studies (frequency) | Name of medications (all drugs are prescribed orally) |
| 4-5 times 1st - when visiting a doctor - making a diagnosis (clinically), determining the severity of the patient’s condition and indications for outpatient treatment, ordering a blood test and x-ray examination of the chest organs. 2nd - after 3-4 days of antibacterial therapy. 3rd - after 7-10 days of antibacterial therapy to decide whether to discontinue antibiotics or continue treatment. 4th - 14-16 days from the start of treatment to resolve the issue of the patient’s ability to work. 5th - according to indications (if the patient has not completed treatment): 17-20 days from the start of treatment to resolve the issue of the patient’s ability to work | 1. General blood test 2 times. 2. X-ray (large-frame FG) of the chest in 2 projections, 2 times. Studies are carried out on the 1st-3rd and 14-18th days of illness from the day the patient contacts the doctor | • Amoxicillin/clavulanate 625 mg 3 times/day or 1,000 mg 2 times/day ± macrolide orally; • Amoxicillin/sulbactam 1,000 mg 3 times/day or 2000 mg 2 times/day ± macrolide orally; • Levofloxacin 500 mg/day; • Moxifloxacin 400 mg/day; • Gemifloxacin 400 mg/day |
Combined antibacterial therapy for CAP, including macrolides, is used for non-severe CAP in patients with concomitant pathologies or when patients indicate an appointment within the last 3 months. antibacterial drugs? 2 days. Macrolides are most often used in patients with CAP who require hospitalization, including in the intensive care unit [17, 18]. In this aspect, macrolides should be considered not only as a means of “covering” against intracellular pathogens, but also as an antibiotic with potentiation of the effect against pneumococcus [20]. Table 4
Antibacterial treatment regimens for CAP in hospitalized patients of varying severity are presented [17, 18].
| Table 4. Antibacterial therapy for community-acquired pneumonia in hospitalized patients | ||
| Group | Most common pathogens | Recommended treatment regimens |
| Mild pneumonia1 | S. pneumoniae H. influenzae C. pneumoniae S. aureus Enterobacteriaceae | Ampicillin IV, IM ± macrolide orally2 Amoxicillin/clavulanate IV ± macrolide orally2 Amoxicillin/sulbactam IV, IM ± macrolide orally2 Cefotaxime IV, IM ± macrolide orally2 Ceftriaxone IV, IM /m ± macrolide orally2 Ertapenem IV, IM ± macrolide orally2 or Respiratory fluoroquinolone (levofloxacin, moxifloxacin) IV or orally |
| Severe pneumonia 3 | S. pneumoniae Legionella spp. S. aureus Enterobacteriaceae | Amoxicillin/clavulanate IV + macrolide IV Cefotaxime IV + macrolide IV Ceftriaxone IV + macrolide IV Ertapenem IV + macrolide IV or Respiratory fluoroquinolone (levofloxacin, moxifloxacin) IV + cefotaxime, ceftriaxone IV |
| Note. 1 Stepped therapy is preferred. If the patient’s condition is stable, oral administration of drugs is allowed immediately. 2 Preference should be given to the most studied macrolides for CAP with improved pharmacokinetic properties (azithromycin, clarithromycin). 3 In the presence of risk factors for P. aeruginosa infection (bronchiectasis, use of systemic glucocorticoids, therapy with broad-spectrum antibiotics for more than 7 days during the last month, exhaustion of the body), the drugs of choice are ceftazidime, cefepime, cefoperazone/sulbactam, ticarcillin/clavulanate, piperacillin/ tazobactam, carbapenems (meropenem, imipenem) + ciprofloxacin or + aminoglycosides of the II-III generation (gentamicin, tobramycin, amikacin). If aspiration is suspected, it is advisable to use amoxicillin/clavulanate or cefoperazone/sulbactam, or ticarcillin/clavulanate, or piperacillin/tazobactam, or moxifloxacin as monotherapy or as combination therapy with third-generation cephalosporins (ceftriaxone, cefotaxime) + metronidazole. | ||
In practice, the most common combination antibacterial therapy for severe pneumonia is a combination of third-generation cephalosporins and macrolides, and the prescription of a combination of these 2 classes of antibiotics should be used as initial therapy, only in this case the duration of hospitalization is significantly reduced [21]. Answering the question: “Which macrolide should be preferred when combined with third-generation cephalosporins?”, we present the results of a prospective comparative study that shows the advantage of combined therapy with ceftriaxone and azithromycin compared with treatment with ceftriaxone and clarithromycin (Fig. 5) [22].
The importance of macrolides in the treatment of patients with severe pneumonia is evidenced by the results of a systematic review of 28 observational studies of about 10 thousand patients with severe CAP, which showed that the use of macrolides in combination therapy with beta-lactam antibiotics compared with monotherapy led to a decrease in mortality (p = 0.02) [23]. A comparative assessment of mortality rates in patients with severe CAP who received beta-lactams in combination with macrolides and beta-lactams in combination with respiratory fluoroquinolones (RFQs) is noteworthy. It turned out that there was no significant difference between these antibacterial drug regimens (20% beta-lactam + macrolide and 23% beta-lactam + RPC; odds ratio (OR) 0.83, 95% confidence interval (CI) 0.67-1.03, p = 0.09).
Emphasizing the importance of macrolides, and in particular azithromycin, in the treatment of patients with pneumonia, it is necessary to note the importance of this antibiotic in legionella pneumonia (Legionnaires' disease). An epidemic outbreak of legionellosis was registered in the city of Verkhnyaya Pyshma, Sverdlovsk region in July–August 2007 [24]. The etiological diagnosis of legionella pneumonia was established in 61 people, of which in 15 patients (9.1%) the course of the disease was defined as mild (without systemic inflammatory response syndrome) and in 46 (90.9%) - severe, in accordance with the recommendations of the American Society Infectious Diseases Society of America / American Thoracic Society - IDSA / ATS [25]. The mortality rate was 6.6%.
Azithromycin is one of the drugs of choice for Legionnaires' disease. The antibiotic was prescribed as monotherapy for 10 days, 500 mg once, for mild manifestations of Legionella infection orally in 10 cases out of 15 (66.7%) and in 17 patients out of 46 (37.0%) with severe Legionella pneumonia according to the principle of step-down therapy .
As a result of treatment with azithromycin, positive clinical, laboratory and radiological dynamics were achieved in patients with severe Legionella pneumonia. There were no deaths among those treated with azithromycin.
A significant increase in the level of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) in the peripheral blood after antibiotic therapy with an unusually long course of azithromycin in patients with severe Legionella CAP without concomitant liver diseases was noted [26]. The results obtained correspond with literature data indicating a transient increase in transaminases as a side effect of antibiotics [27-29]. Hepatocyte cytolysis syndrome was transient in nature without signs of liver failure, which was confirmed by normalization of transaminase levels after 12 months. after patients are discharged from the hospital. A comparative assessment of AST and ALT indicators over time in patients with severe Legionella pneumonia treated with azithromycin is presented in Table 5
.
| Table 5. Comparative assessment of AST and ALT indicators over time in patients with severe Legionella pneumonia treated with azithromycin, M (95% CI)1 | |||||
| Index | During hospitalization (1); n = 28 | After treatment (2) n = 22 | After 12 months (3) n = 17 | R1-2 | R2-3 |
| AST2, IU/l | 26,5 (17,3-35,6) | 79,0 (53,2-104,7) | 22,8 (18,93—26,71) | 0,0007 | 0,0000 |
| ALT3, IU/l | 36,6 (22,0-51,2) | 75,8 (48,2-103,5) | 26,4 (20,0?32,9) | 0,01 | 0,0001 |
| Note: 1 M (95% CI) - M - mean value (95% confidence interval); 2 AST - aspartate aminotransferase; 3 ALT - alanine aminotransferase. | |||||
Another confirmation of the need for azithromycin is the results we obtained in the treatment of patients with severe pneumonia during an epidemic outbreak of influenza A (H1N1) pdm09. Of the 250 patients under observation, 104 (41.6%) were treated with a simultaneously prescribed combination of third-generation cephalosporins and azithromycin [30]. Most of them (64 patients) were diagnosed with severe pneumonia due to influenza A (H1N1) pdm09. Parenteral use of third generation cephalosporins and azithromycin at a dose of 500 mg for 3-5 days followed by the administration of inhibitor-protected penicillins provided regression of clinical symptoms and radiological changes in the respiratory system after 16.3 days 95% CI [15.2-17.3] .
Thus, at present, macrolides have one of the leading places in the antibacterial therapy of community-acquired pneumonia, regardless of their etiology and severity of the disease, and azithromycin is one of the main representatives of this class of antibiotics.
References 1. Gordon EM, Blumer JL. Pharmacokinetics and pharmacodynamics: azithromycin concentrates in tissues. Pediatr. Infect. Dis. J., 2004. 23(suppl 2): S102-S107. 2. Odenholt-Tornqvist I, Lowdin E, Cars 0. Postantibiotic effects and postantibiotic sub-MIC effects of roxithromycin, clarithromycin, and azithromycin on respiratory tract pathogens. Antimicrob. Agents. Chemother., 1995. 39: 221-226. 3. Baldwin DR, Wise R, Andrews JM et al. Azithoromycin concentrations at the sites of pulmonary infection. Eur. Respira. J., 1990. 3: 886-890. 4. Lode H. Azithromycin in the Treatment of Community-Acquired Pneumonia in Adults. Cambrige Medical Publications, 2002. 24. 5. Fang GD, Stout JE, Yu VL. Comparison of intracellular postantibiotic effect of azithromycin and clarithromycin vs. erythromycin against Legionella pneumophila serogroup 1. In: The 36th International Conference on Antimicrobial Agents and Chemotherapy, New Orleans, 1996. abstr. A91. 6. Lukyanov S.V. Clinical pharmacology of macrolides. Consilium medicum, 2004. 10: 769–773. 7. Culi O, Erakovi V, Cepelak I et al. Azithromycin modulates neutrophil function and circulatig inflammatory mediators in healthy human subjects. Eur. J. Pharmacol., 2002. 450 (3): 277-89. 8. Strachunsky L.S., Kozlov S.N. Macrolides in modern clinical practice. 9. Stetsyuk O.U., Andreeva I.V., Kolosov A.V., Kozlov R.S. Safety and acceptability of antibiotics in outpatient practice. KMAH, 2011. 13. 1: 67-84. 10. Plouffe J, Schwartz D, Kolokathis A et al. Clinical efficacy of intravenous followed by oral azithromycin monotherapy in hospitalized patients with community-acquired pneumonia. The Azithromycin Intravenous Clinical Trials Group. Antimicrob. Agents Chemother., 2000. 44 (7): 1796-802. 11. Mosholder AD, Alexander JJ, Smith H et al Cardiovascular risks with azithromycin and other antibacterial drugs. N.Engl. J. Med., 2013. 368: 1665-1668. 12. Poluzzi E, Raschi E, Motola D et al. Antimicrobials and the risk of torsades de pointes: the contribution from data mining of the US FDA Adverse Event Reporting System. Drug. Saf., 2010. 33(4): 303-314. 13. Svanstrom H, Pasternak B, Hviid A. Use of Azithromycin and Death from Cardiovascular Causes. N.Engl. J. Med., 2013. 368: 1704-1712. 14. Sinopalnikov A.I., Andreeva I.V., Stetsyuk O.U. Safety of macrolide antibiotics: a critical review. Clinical Medicine, 2012. 3: 23-30. 15. Andrade RJ, Tulkens PM. Hepatic safety of antibiotics used in primary care. J. Antimicrob. Chemother., 2011. 66(7): 1431-1446. 16. Kozlov R.S. et al. Antimicrobial Therapeutics Summit Resolution. Consilium Medicum, 2014. 16 (11): 33-36. 17. Chuchalin A.G., Sinopalnikov A.I., Kozlov R.S., Tyurin I.E. Rachina S.A. Community-acquired pneumonia in adults: practical recommendations for diagnosis, treatment and prevention. A manual for doctors. M., 2010: 82 p. 18. Guidelines for the management of adult lower respiratory tract infections/Guest Editor: Didier Raoult. The official publication of the European Respiratory Society and European Society for Clinical Microbiology and Infectious Diseases. Clin Microbiol Infect, 2011. 17(Suppl. 6): 1-24. 19. Leshchenko I.V., Bobyleva Z.D., Trifanova N.M. and others. Clinical and organizational algorithm for the management of patients with community-acquired pneumonia. Guidelines. Under the general editorship. A.G. Chuchalina. 2nd ed., revised. and additional, Moscow, LLC "Elikon-Design" 2012. 70 p. 20. Girard D, Finegan SM, Dunne MW et al. Enhanced efficacy of single-dose versus multi-dose azithromycin regimens in preclinical infection models. J. Antimicrob. Chemoter, 2005. 56 (2): 65-71. 21. Stahl JE, Barza M, DesJardin J et al. Effects of macrolides as part of initial emperic therapy on length of stay in patients hospitalized with CAP. Arch. Intern. Med., 1999. 159: 2576-2580. 22. Sanchez F, Mensa J, Martinez JA et al. Is azithromycin the first-choice macrolide for treatment of community-acquired pneumonia? Clin. Infect. Dis., 2003. 36: 1239–1245. 23. Sligl WI, Asadi L, Eurich DT et al. Macrolides and Mortality in Critically Ill Patients With Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis. Critical Care Medicine, 2014. 42 (2): 420–432. 24. Mikhailova D.O., Leshchenko I.V., Bobyleva Z.D. et al. The first outbreak of legionella infection in the Sverdlovsk region. Algorithm for diagnosis and treatment. Ural Medical Journal, 2007. 8: 4-10. 25. Bobyleva Z.D., Leshchenko I.V., Vinokurova A.N. Comparative analysis of clinical, laboratory and radiological data in patients with legionellosis and non-legionella pneumonia during the epidemic outbreak of legionellosis in the Sverdlovsk region. Pulmonology, 2009. 6: 45-52. 26. Bobyleva Z.D., Leshchenko I.V. Features of the clinical course and long-term results of legionella pneumonia during the epidemic outbreak of legionellosis in the Sverdlovsk region. Clinical Medicine, 2010. 4: 72-77. 27. Sherlock S. Diseases of the liver and biliary tract (translated from English). M., 1999: 386–423. 28. DeLeve LD. Mechanisms of drug-induced liver disease. N. Clin. N. Amer., 1995. 24: 787–810. 29. Schiano TD Drug-induced and toxic liver disease. Schiano TD, Black M. In: Friedman LS, Keefe EB, Maddrey WC (ed.). Handbook of Liver Disease. Churcill. Livingstone, 1998: 103-123. 30. Leshchenko I.V., Krivonogov A.V. Features of the course of pneumonia during pandemic influenza A/H1N1/09. Pulmonology, 2011. 6: 62-68.
Contraindications to the use of macrolides
Allergy to the corresponding drug should be considered a contraindication when prescribing macrolide antibiotics; pregnancy (this contraindication is relevant to clarithromycin, midecamycin or roxithromycin); During breastfeeding, the above antibiotics, as well as spiramycin and josamycin, are contraindicated.
Warnings
- During pregnancy, the use of clarithromycin should be avoided, as there is evidence of its negative effects on fetal development. At the moment, there is no information that could confirm the absence of negative effects of roxithromycin and midecamycin, as a result of which their use during pregnancy should be avoided.
- Macrolide antibiotics such as josamycin, spiramycin and erythromycin do not cause negative effects on the fetus. Therefore, a course of antibacterial therapy with these drugs is not contraindicated for pregnant women.
- Azithromycin can be recommended with caution during pregnancy.
- During breastfeeding, antibiotics pass into breast milk, so only erythromycin is safe for a nursing woman. These data are not available for azithromycin, and all other macrolide antibiotics are contraindicated for nursing women. During treatment with macrolides, breastfeeding should be suspended.
- For children, macrolides are prescribed from 6 months in a special children's form. For example, Ecomed (azithromycin) is available in powder form for the preparation of a suspension, which makes its use in children convenient.
- Prescribing antibacterial therapy with macrolides to older people does not pose any danger. However, when prescribing erythromycin, it is necessary to take into account its possible negative effect on hearing.
- If renal function is impaired, T1/2 of clarithromycin can be increased to 20 hours (if creatine clearance decreases to less than 30 ml/min), and the half-life of its active metabolite is extended to 40 hours.
- T1/2 of roxithromycin when creatine clearance decreases to 10 ml/min increases to 13-15 hours. In this regard, in case of renal failure, titration of the dose of these macrolide antibiotics is required.
- in case of severe liver dysfunction, treatment with antibiotics of this group should be avoided, since the elimination time of the drug increases, which can lead to an increased risk of hepatoxicity. Of particular note is the occurrence of such adverse events when using josamycin and erythromycin.
- Given the possible effect on prolongation of the QT interval, caution should be exercised when treating macrolide antibiotics in patients suffering from heart disease. An electrocardiogram allows you to see changes in the functioning of the heart.
Use in childhood
The use of macrolides for children is a separate section: drugs in this group are not always approved for use without restrictions. In addition, recommended dosages of medications are lower than those for the adult population, and are almost always calculated based on the baby’s body weight.
Erythromycin solution for intravenous administration can rarely cause acute toxic hepatitis in a child. The substance is prescribed at a dose of 30-40 mg per kilogram of body weight, this daily dose is divided into 2-4 doses. The duration of the course is unchanged (7-10 days).
Drugs containing the macrolide clarithromycin are limited to newborns and infants up to 6 months. For children over 12 years of age, they are prescribed 250 mg twice a day.
Roxithromycin is not recommended for babies under 2 months, while others are prescribed 5-8 mg per 1 kg of body weight. The dose is divided into 2 doses.
Azithromycin is not used in children:
- up to 16 years (for infusion forms);
- up to 12 years with a weight of less than 45 kg (for tablet and capsule form);
- up to six months (for suspension).
In this case, the dosage for children over 12 years of age with a body weight of more than 45 kg is the same as the adult dose. And for a child 3-12 years old and weighing less than 45 kg, an antibiotic is prescribed at 10 mg per kilogram once a day.
The dose of josamycin is 40-50 mc/kg. It is evenly divided into 2-3 doses per day. It is recommended to prescribe 1-2 grams. Spiramycin tablets of 1.5 million IU are not given to children under 3 years of age, and 3 million IU tablets are not given to children under 18 years of age. The maximum dose is 300 IU per kilogram per day.
Information for patients taking macrolide antibiotics
Instructions for the use of antibacterial drugs belonging to the group of macrolides serve as the main guideline in prescribing a course of treatment. This or that drug should be taken as prescribed by the attending physician, taking into account factors such as the presence of chronic diseases, general malaise, reduced immunity, age, pregnancy, breastfeeding and individual characteristics of the body.
The general rules for the use of macrolide antibiotics are as follows:
- Macrolides should be taken orally 1 hour before meals or 2 hours after meals. Exceptions are clarithromycin, spiramycin and josamycin; they can be taken without taking into account meal times; Erythromycin should be taken with plenty of water (at least 1 full glass);
- when preparing suspensions for children, it is recommended to follow the attached instructions;
- You cannot, without a doctor’s recommendation, change the time interval between taking antibiotics, skip or change the dosage (increase or decrease);
- if for some reason the required dose was missed, you should take it as quickly as possible, but if it is already time to take the next one, you should not do this;
- it is necessary to adhere to the prescribed course of therapy and not increase it on your own, do not stop taking the drug prematurely (this is especially important to consider in case of streptococcal infections);
- when treating with erythromycin, it is necessary to abstain from alcohol-containing drinks and medications during treatment;
- You cannot combine the use of macrolides with antacids.
Main characteristics and features of the use of various macrolides
- Erythromycin - used 2 to 4 times a day. The peculiarities of erythromycin include the fact that when taking the drug orally, it is important to take into account the presence of food - it reduces the bioavailability of the drug. With simultaneous use of erythromycin with theophylline, cisapride, carbamazepine, disopyramide and cyclosparine, an increase in the concentration of the drug in plasma may be observed. When taking erythromycin, adverse events from the gastrointestinal tract often occur. The drug can be used in pregnant and lactating women.
- Clarithromycin - recommended oral administration 2 times a day; A feature of clarithromycin should be considered its high activity against H. pylori, as well as atypical mycobacteria. Clarithromycin is characterized by higher bioavailability and tissue penetration compared to erythromycin. This macrolide is prescribed with caution for renal failure and is not recommended for use in pregnant and lactating women. In pediatric practice, clarithromycin is used from 6 months. An eco-analogue of clarithromycin is available in tablets under the trade name Ecositrin.
- Azithromycin is used once a day, as it has a very long half-life. It can accumulate in tissues in significant concentrations, which makes it possible to use azithromycin in short courses (3-5 days). Single use is possible in children with acute otitis media and in adults with acute urogenital chlamydia. Take azithromycin 1 hour before a meal or 2 hours after a meal, since it is advisable to take it on an empty stomach. Azithromycin is more active than other macrolides against Pseudomonas aeruginosa and enterobacteria. An eco-analogue of azithromycin, Ecomed, is available in capsules, tablets and powder for the preparation of a suspension (children's form).
- Roxithromycin - prescribed 1-2 times a day, regardless of meals. If the patient has renal failure, the standard therapeutic dose should be reduced. Therapy with roxithromycin is easier to tolerate than treatment with erythromycin and is less likely to interact with other drugs. This antibiotic should not be used during pregnancy and breastfeeding.
- Spiramycin - used 2-3 times a day. Women should interrupt breastfeeding while taking the drug. This macrolide antibiotic has high bioavailability regardless of food intake, and creates higher concentrations of the active substance in tissues than erythromycin. The drug is usually well tolerated by patients, and no interactions with other drugs have been established to date. Spiramycin is active against some streptococci that exhibit resistance to 14- and 15-membered macrolides. Unlike other macrolides, spiramycin can be prescribed for toxoplasmosis and cryptosporidiosis.
- Josamycin - taken orally 3 times a day; unlike erythromycin, josamycin is rapidly absorbed from the gastrointestinal tract regardless of the presence of food; this macrolide is active against some staphylococci and streptococci resistant to erythromycin; The drug is not prescribed for breastfeeding women.
- Midecamycin - take 3 times a day, preferably an hour before meals. Therapy with this macrolide antibiotic is well tolerated by patients; no interactions with other drugs have been identified; Contraindicated for lactating and pregnant women.
- Midecamycin acetate is a derivative of midecamycin, which has higher antibacterial activity and bioavailability; taken 3 times a day, contraindications are similar to midecamycin.
Macrolides
| Macrolides are characterized by the presence of a 14-, 15-, or 16-membered lactone ring in their structure; exception is tacrolimus with a 23-atom ring |
| Clarithromycin is the most commonly used macrolide in gastroenterology (in particular, in the eradication of Helicobacter pylori ). Has a 14-membered lactone ring (top left) |
| Erythromycin is historically the first macrolide drug. A widely used antibiotic. Has a 14-membered lactone ring |
| Azithromycin is a macrolide-azalide. It has a 15-membered lactone ring, which differs from the 14-membered one by the nitrogen atom included in it (N), in the figure - top left. Antibiotic |
| Josamycin is a macrolide with a 16-membered lactone ring (bottom right). Antibiotic |
| Alemcinal is a macrolide with a 14-membered lactone ring (top) and is not an antibiotic. Considered as a promising prokineticist |
| Tacrolimus is a macrolide and immunosuppressant with a 23-membered ring (middle) |
Macrolides
(eng.
macrolides
) are drugs whose molecular structure contains a 14-, 15- or 16-membered lactone ring. Most macrolides are antibiotics. Macrolides are agonists of motilin receptors and therefore, to varying degrees, stimulate the motility of the gastrointestinal tract, exhibiting prokinetic properties.
General characteristics of the group of macrolides
Macrolide antibiotics occupy one of the leading positions in antibacterial therapy for a wide range of diseases. They are the least toxic among antimicrobial agents and are well tolerated by patients. According to their pharmacokinetic characteristics, macrolides are classified as tissue antibiotics. Features of the pharmacokinetics of the most commonly prescribed antibiotics include the ability of macrolides to reach higher concentrations at the site of infection than in the blood plasma. Historically, the first macrolide is the natural antibiotic erythromycin, discovered in 1952, isolated from the streptomycete species Streptomyces erythreus
(later reclassified as the species
Saccharopolyspora erythraea
).
The first semisynthetic macrolide is roxithromycin. The most commonly used macrolide currently used in clinics is clarithromycin. Both erythormycin, roxithromycin, and clarithromycin are antibiotics and have a 14-membered lactone ring in their molecules.
In the group of macrolides, a subgroup of azalides is distinguished, in which a nitrogen atom is additionally included in the lactone ring between the 9th and 10th carbon atoms (the ring thus becomes 15-membered). The most famous azalide is the semisynthetic antibiotic azithromycin.
Of the 16-membered antibiotics, the best known is the naturally occurring antibiotic josamycin.
14-membered macrolides, in which a keto group is attached to the lactone ring at the 3rd carbon atom, are classified as ketolides. Ketolides were developed to combat macrolide-resistant pathogens of respiratory tract infections and have not become widespread in gastroenterology.
Natural macrolide with a 23-membered ring, tacrolimus, first obtained from streptomycetes of the species Streptomyces tsukubaensis
, is an immunosuppressive drug that is not an antibiotic. Due to the inherent quality of macrolides to stimulate the motor-evacuation function of the gastrointestinal tract, tacrolimus is the most effective drug among immunosuppressants in the treatment of gastroparesis that occurs after allogeneic bone marrow transplantation and in other similar situations (Galstyan G.M. et al.).
Macrolide antibiotics are characterized by high bioavailability (30-65%), long half-life (T½), and the ability to easily penetrate tissue (especially azithromycin). Characterized by a direct anti-inflammatory effect. They have a predominantly bacteriostatic effect on gram-positive cocci (streptococci, staphylococci) and intracellular microorganisms (legionella, mycoplasma, chlamydia). Clarithromycin is highly active against Helicobacter pylori
, acid resistance, high concentration in tissues, long half-life (3-7 hours) and good tolerability.
Dose: 500 mg 2 times a day; course of treatment is 7-10 days. Azithromycin is characterized by high bioavailability (40%), high content in tissues, long half-life (up to 55 hours), which allows it to be prescribed once a day and use short courses of treatment (1-5 days); characterized by a long-lasting post-antibiotic effect (5-7 days after discontinuation), good tolerability; active against Helicobacter pylori
. Dose: 500 mg 1 time per day for 3 days (Zimmerman Y.S.).
The use of macrolides in the eradication of Helicobacter pylori
The effectiveness of the use of regimens including macrolides for the eradication of Helicobacter pylori
has been shown in numerous studies.
Macrolides provide the maximum bactericidal effect against Helicobacter pylori
among all antibiotics used in the regimen. This effect is dose-dependent and occurs when using, for example, clarithromycin at a dose of 1000 mg per day. Macrolides also have a significant, pronounced anti-inflammatory effect, which is very important for the correction of nonspecific secondary chronic duodenitis in patients with duodenal ulcer, which usually persists even after scarring of the ulcer.
Macrolides have a high ability to penetrate cells and accumulate in the mucous membrane of the stomach and duodenum, which increases their effectiveness against Helicobacter pylori
. In addition, macrolides have fewer contraindications and side effects and a higher eradication rate than tetracyclines, which can also accumulate in cells.
The most common side effects are caused by antibiotics such as tetracycline and furazolidone. Macrolides are well tolerated, and the need to discontinue therapy is noted no more than in 3% of cases (Maev I.V., Samsonov A.A.).
Of all macrolides, the greatest activity against Helicobacter pylori
has clarithromycin. This makes it the main drug from this group recommended for the treatment of Helicobacter pylori infection. Comparative results of the effectiveness of azithromycin and clarithromycin on the eradication rate indicate the greatest effectiveness of the latter by almost 30% (Maev I.V. et al.).
At the same time, the widespread use of macrolides (as well as other antibiotics) when implementing the “screen and treat” strategy can lead to the emergence of resistant pathogens other than Helicobacter pylori
.
Use of a macrolide at a single dose and duration of the shortest regimen for eradication of Helicobacter pylori
(clarithromycin 500 mg twice daily for 7 days) increased the resistance of macrolide-resistant pharyngeal
Streptococcus pneumoniae
in a placebo-controlled study in healthy volunteers.
This difference was statistically significant throughout the study over 180 days. The use of macrolides has been associated with increased resistance of Streptococcus pyogenes
and
Staphylococcus aureus
, which are common causes of community-acquired infections (Starostin B.D.).
There is information that macrolides lead to the development of cholestatic phenomena in the liver, which may be reflected in an increase in the concentration of secondary toxic bile salts in bile, impaired motility of the gastroduodenal zone and alkalization of the pyloric region. The consequence of this may be either an increase in the frequency of biliary reflux or compensatory hypergastrinemia with acidification of the antrum. Considering that the “mixed” version of reflux has a more pronounced damaging effect on the esophageal mucosa, it can be assumed that there is a relationship and the formation of a cascade of disorders in the acid-producing and acid-neutralizing functions of the upper gastrointestinal tract (Karimov M.M., Akhmatkhodzhaev A.A.).
Publications for healthcare professionals addressing the use of macrolides in the eradication of Helicobacter pylori
- Maev I.V., Samsonov A.A., Andreev N.G., Kochetov S.A. Clarithromycin as the main element of eradication therapy for diseases associated with Helicobacter pylori infection // Gastroenterology. 2011. No. 1.
- Maev I.V., Samsonov A.A. Duodenal ulcer: various approaches to modern conservative therapy // CONSILIUM MEDICUM. – 2004. – T. 1. – p. 6–11.
- Kornienko E.A., Parolova N.I. Antibiotic resistance of Helicobacter pylori in children and choice of therapy // Issues of modern pediatrics. – 2006. – Volume 5. – No. 5. – p. 46–50.
- Parolova N.I. Comparative assessment of the effectiveness of eradication therapy for H. pylori infection in children. Abstract of dissertation. PhD, 14.00.09 – pediatrics. SPbGPMA, St. Petersburg, 2008.
- Tsvetkova L.N., Goryacheva O.A., Gureev A.N., Nechaeva L.V. Rational pharmacotherapeutic approach to the treatment of duodenal ulcer in children // Materials of the XVIII Congress of Pediatric Gastroenterologists. – M. – 2011. – P. 303–310.
On the GastroScan.ru website in the “Literature” section there is a subsection “Antibiotics used in the treatment of gastrointestinal diseases,” containing articles on the use of antimicrobial agents in the treatment of diseases of the digestive tract.
Macrolides as prokinetics
Erythromycin and other macrolides interact with motilin receptors, imitating the action of the physiological regulator of the gastroduodenal migratory motor complex.
Erythromycin is capable of causing powerful peristaltic contractions, similar to those of the migratory motor complex, accelerating gastric emptying of liquid and solid food, however, erythromycin has not found widespread use in the treatment of patients with gastroesophageal reflux disease (GERD), since its effect on esophageal motility is practically absent. In addition, a significant decrease in the effectiveness of erythromycin was found against the background of gastric atony with long-term use, which creates obstacles to the use of this drug for GERD (Maev I.V. et al.). Erythromycin activates motilin receptors of smooth muscle cells of the gastrointestinal tract and cholinergic neurons of the intermuscular nerve plexus. In patients with GERD, erythromycin increases the basal pressure of the lower esophageal sphincter (LES). Its effect on transient relaxation of the LES (TRNS) has not been proven. Erythromycin does not affect the amplitude of primary peristaltic contractions of the esophagus, but reduces the number of episodes of “incomplete” contractions. It improves esophageal and gastric emptying in patients with gastroparesis, but this effect is absent in patients with GERD. In high doses, erythromycin is poorly tolerated; it has not found widespread use in gastroenterological practice (Ivashkin V.T., Trukhmanov A.S.).
Azithromycin at a dose of 250 mg per day in patients with GERD can shift the postprandial acid pocket distally, which reduces acid reflux without affecting the total number of refluxes. However, azithromycin has not found widespread use as a prokinetic agent due to side effects (Avdeev V.G.).
A number of macrolide drugs (alemcinal, mitemcinal), due to the fact that they are agonists of motilin receptors and are not antibiotics, are considered promising drugs for the treatment of functional dyspepsia and as such are mentioned in the Recommendations of the Russian Gastroenterological Association for the diagnosis and treatment of functional dyspepsia and 2011 ( Ivashkin V.T., Sheptulin A.A. et al.), and 2022. (Ivashkin V.T., Maev I.V., etc.). They are also offered for the treatment of other gastrointestinal diseases (GERD, reflux esophagitis, IBS-d, diabetic gastroparesis and others). However, none of the macrolides, based on the results of clinical trials of the second stage, could receive a positive conclusion, and today there is skepticism regarding the clinical use of both macrolide antibiotics and non-antibiotic macrolides as prokinetics: “as for such prokinetics as erythromycin, azithromycin, alemcinal , then their use for functional dyspepsia is not indicated due to the “non-physiological acceleration of gastric emptying”” (Sheptulin A.A., Kurbatova A.A.).
Publications for healthcare professionals addressing the use of macrolides as prokinetic agents
- Alekseeva E.V., Popova T.S., Baranov G.A. and others. Prokinetics in the treatment of intestinal failure syndrome // Kremlin Medicine. Clinical Bulletin. 2011. No. 4. pp. 125–129.
- Alekseeva E.V. Prokinetics in the treatment of intestinal failure syndrome in critically ill surgical patients. Abstract of dissertation. PhD, 01/14/20 - anesthesiology and resuscitation, 03/14/03 - pat. physiology. UC UDPRF, Moscow, 2010.
- Rosen R, Vandenplas Y, Singendonk M, et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of NASPGHAN and ESPGHAN. // J Pediatr Gastroenterol Nutr. 2022 Mar;66(3):516-554.
- Rakitin B.V. Main recommendations in the article: Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of NASPGHAN and ESPGHAN. J Pediatr Gastroenterol Nutr. 2022.
On the website GastroScan.ru in the “Literature” section there is a subsection “Prokinetics”, containing publications for medical workers and medical students on the use of prokinetics in the treatment of diseases of the gastrointestinal tract.
Appendix 1. Macrolides in ATC
In the Anatomical Therapeutic Chemical Classification (ATC), in section “J Antimicrobial drugs for systemic use”, subsection “J01 Antibacterial drugs for systemic use” there is a group “J01FA Macrolides”, which includes the following codes: J01FA01 Erythromycin J01FA02 Spiramycin J01FA03
Midecamycin J01FA05 Oleandomycin J01FA06 Roxithromycin J01FA07 Josamycin J01FA08 Troleandomycin J01FA09 Clarithromycin J01FA10 Azithromycin J01FA11 Myocamycin J01FA12 Rokitamycin J01FA13 Dirithromycin J01FA14 Flurithromycin J01FA15 Telithromycin J01 FA16 Solithromycin
In the ATC section “A Drugs affecting the digestive tract and metabolism” there is a group “A02BD Combinations of drugs for the eradication of Helicobacter pylori
", which separately identifies combinations of drugs for the treatment of
Helicobacter pylori
diseases, including the macrolide clarithromycin:
A02BD04 Pantoprazole in combination with amoxicillin and clarithromycin A02BD05 Omeprazole, amoxicillin and clarithromycin A02BD06 Esomeprazole, amoxicillin and clarithromycin A02BD07 Lansoprazole, amoxicillin and clarithromycin A02BD09 Lansoprazole, clarithromycin and tinidazole A02 BD11 Pantoprazole, amoxicillin, clarithromycin and metronidazole
Tacrolimus has two ATC codes:
In section “L Antineoplastic drugs and immunomodulators”, group “L04A Immunosuppressants”, “L04AC Interleukin inhibitors”:
L04AD02 Tacrolimus
and in section “D Drugs for the treatment of skin diseases”:
D11AH01 Tacrolimus
Appendix 2. Trade names of drugs with active ingredients - macrolides
The State Register of Medicines of Russia contains (including those with expired registration) macrolide medicines with the following trade names*:
- international nonproprietary name (INN) clarithromycin
(semi-synthetic antibiotic, 14-members): Arvicin, Bacticap, Biotericin, Zimbaktar, Kispar, Klabaks, Klabaks OD, Klarbakt, Clarithromycin-Akrikhin, Clarithromycin-Verte, Clarithromycin-J, Clarithromycin Zentiva, Clarithromycin Protech, Clarithromycin Pfizer, Clarithromycin Retard-OBL, Clarithromycin Sanofi, Clarithromycin SR, Clarithromycin-Teva, Clarithromycin Ecositrin, Clarithromycin-OBL, Clarithrosin, Claricin, Claricit, Claromin, Klasine, Klacid, Klacid SR, Clerimed, Coater, Lekoklar, Mycetinum, Romiclar, Seydon-Sanovel, SR-Klaren, Fromilid, Fromilid Uno, Ecositrin - INN erythromycin
(natural antibiotic, 14-members): Erythromycin, Erythromycin-AKOS, Erythromycin-LekT, Erythromycin-Ferein; complex active ingredient: - erythromycin + zinc acetate
: Zinerit - erythromycin + isotretinoin
: Isotrexin
(semi-synthetic antibiotic, 14-members): Xitrocin, Remora, Roxeptin, RoxyHexal, Roxithromycin, Roxithromycin DS, Roxithromycin Sandoz, Roxolit, Romik, Rulid, Rulitsin, Elrox, Esparoxi
(semi-synthetic antibiotic, 15-members): Azibiot, Azivok, Azidrop, Azimicin, Azitral, Azithromycin-BI, Azitrox, Azithromycin, Azithromycin-Bi, Azithromycin-Vetex, Azithromycin-J, Azithromycin Zentiva, Azithromycin-Leksvm, Azithromycin McLeodz, Azithromycin Sandoz, Azithromycin Forte, Azithromycin Forte-OBL, Azithromycin-OBL, Azithromycin Ecomed, AzitRus, AzitRus forte, Azicide, Zetamax retard, Z-factor, Ziromin, Zitnob, Zitrolide, Zitrolide forte, Zitrocin, Sweetrox, Sumacli d, Sumaclid 1000, Sumamed, Sumamed forte, Sumametcin, Sumamox, Sumatrolide solutab, Sumatrolide Solution Tablets, Tremak-Sanovel, Ecomed, Hemomitsin;
complex active ingredient: azithromysine + fluconosal + secnidazole
: Safotsid
(natural antibiotic, 16-members): Vilprafen, Vilprafen Solutab
(natural antibiotic, 16-members): Rovamycin, Spiramisar, Spiramycin-vero
(natural antibiotic, 16-members): Macropen
(natural antibiotic, 14-members) - no;
complex active ingredient oleandomycin + tetracycline
: Oletetrin
(semi-synthetic antibiotic, 14-member ketoid): Ketek
(natural 23-member immunosuppressant): Advagraf, Grastiva, Pangraf, Priluxid, Prograf, Protopic, Redinesp, Tacrolimus, Tacrolimus-Acri, Tacrolimus-Richter, Tacrolimus-Teva, Tacrolimus STADA, Tacropic, Tacrosel**
* as of the beginning of October 2022 ** as of the beginning of February 2022
Macrolide medications have contraindications, side effects and application features; consultation with a specialist is required.
Back to section