Levofloxacin is a prescription antimicrobial agent that is prescribed to patients in the older age group for infectious pathologies of the body. Used in dermatology, pulmonology, otolaryngology, ophthalmology. Before starting the course, it is recommended to carefully study the restrictions, since ignoring this condition will lead to irreversible negative consequences.
If for some reason the drug is not suitable, then it is recommended that you familiarize yourself with one of the analogues of Levofloxacin 500 mg presented in the article.
pharmachologic effect
Manufacturer: Vertex, Russia
Release form: eye drops, tablets, solution for infusion
Active ingredient: levofloxacin
Levofloxacin contains the main component of the same name, which has an antimicrobial and bactericidal effect on pathogenic cells. It is characterized by rapid absorption and absorption from the gastrointestinal tract, while food intake has virtually no effect on this fact. Penetrates well into lung tissue, the mucous surface of the bronchi, organs of the urinary and reproductive systems, and is excreted along with urine.
Indications for use of Levofloxacin
According to the instructions for use, Levofloxacin is prescribed for the following indications:
- bronchitis in the chronic stage;
- pneumonia;
- sinusitis;
- otitis media;
- acute pyelonephritis and other infections of the urinary system and kidneys;
- festering atheromas;
- abscess;
- boils;
- urogenital chlamydia and other infectious disorders of the reproductive system.
Helpful information! If a patient is diagnosed with bacterial ophthalmic infections, then in most cases Levofloxacin eye drops are prescribed.
Carefully
- In patients predisposed to the development of seizures [in patients with previous lesions of the central nervous system (CNS); in patients simultaneously taking drugs that lower the threshold of convulsive activity of the brain, such as fenbufen, theophylline] (see section “Interaction with other drugs”);
- In patients with latent or manifest deficiency of glucose-6-phosphate dehydrogenase (increased risk of hemolytic reactions during treatment with quinolones);
- In patients with impaired renal function (mandatory monitoring of renal function is required, as well as correction of the dosage regimen, see section “Dosage and Administration”);
- In patients with known risk factors for QT interval prolongation: in elderly patients; in female patients; in patients with uncorrected electrolyte disturbances (with hypokalemia, hypomagnesemia); with congenital long QT syndrome; with heart disease (heart failure, myocardial infarction, bradycardia); while taking medications that can prolong the QT interval (class IA and III antiarrhythmic drugs, tricyclic antidepressants, macrolides, antipsychotics) (see sections “Overdose”, “Interaction with other drugs”, “Special instructions”);
- In patients with diabetes mellitus receiving oral hypoglycemic drugs (for example, glibenclamide) or insulin drugs (the risk of hypoglycemia increases);
- In patients with severe adverse reactions to other fluoroquinolones, such as severe neurological reactions (increased risk of developing similar adverse reactions when using levofloxacin);
- In patients with psychosis or in patients with a history of mental illness (see section "Special instructions");
- In elderly patients, in patients after transplantation, as well as with concomitant use of glucocorticosteroids (increased risk of tendinitis and tendon rupture) (see section "Special instructions").
Levofloxacin - instructions for use
Levofloxacin tablets are intended for oral administration. It is recommended to drink a significant amount of liquid. The dosage and duration of therapy are adjusted by the attending physician depending on the diagnosis, general condition and concomitant pathologies.
| Indications | Dosage | Course duration |
| Sinusitis | 500 mg once daily | 7–10 days, but no more than two weeks after preliminary consultation with a specialist |
| Chronical bronchitis | 250–500 mg once daily | |
| Pneumonia | 250–500 mg no more than twice daily | |
| Infectious pathologies of the urinary tract | 250 mg once daily | |
| Infectious pathologies of the skin or soft tissues | 250–500 mg no more than twice daily |
Helpful information! If the patient is unable to swallow the tablet on his own, then Levofloxacin for injection is prescribed.
For eye infectious pathologies, drops are prescribed for adults and children from one year of age, 1-2 drops. every two hours, but more than 8 times a day. This dosage must be adhered to for the first two days during an exacerbation. Starting from days 3 to 7, Levofloxacin drops are used 4 times a day. The duration of the course is no more than a week.
How to take Levofloxacin: before or after meals
It is recommended to take Levofloxacin tablets 30–45 minutes before meals. It is also allowed to take the drug between meals. During therapy, the patient also needs to supplement the course with agents that restore intestinal microflora and maintain normal kidney function.
Levofloxacin 250 mg 5 pcs. film-coated tablets
pharmachologic effect
Levofloxacin is a synthetic broad-spectrum antibacterial drug from the group of fluoroquinolones, containing levofloxacin, a levorotatory isomer of ofloxacin, as an active substance.
Levofloxacin blocks DNA gyrase, disrupts supercoiling and cross-linking of DNA breaks, inhibits DNA synthesis, and causes profound morphological changes in the cytoplasm, cell wall and membranes. Levofloxacin is active against most strains of microorganisms both in vitro and in vivo.
Aerobic gram-positive microorganisms: Corynebacterium diphtheriae, Enterococcus faecalis, Enterococcus spp, Listeria monocytogenes, Staphylococcus coagulase-negative methi-S(I), Staphylococcus aureus methi-S, Staphylococcus epidermidis methi-S, Staphylococcus spp(CNS), Streptococci group C and G, Streptococcus agalactiae, Streptococcus pneumoniae peni I/S/R, Streptococcus pyogenes, Viridans streptococci peni-S/R.
Aerobic gram-negative microorganisms: Acinetobacter baumannil, Acinetobacter spp, Actinobacillus actinomycetemcomitans, Citrobacter freundii, Eikenella corrodens, Enterobacter aerogenes, Enterobacter agglomerans, Enterobacter cloacae, Enterobacter spp, Escherichia coli, Gardnerella vaginalis, Haemophilus ducreyi, Haemophilus influenzae ampi-S/R, Haemophilus parainfluenzae, Helicobacter pylori, Klebsiella oxytoca, Klebsiella pneumoniae, Klebsiella spp, Moraxela catarrhalis (3+/p-, Morganella morganii, Neisseria gonorrhoeae non PPNG/PPNG, Neisseria meningitidis, Pasteurella conis, Pasteurella dagmatis, Pasteurella multocida, Pasteurella spp, Proteus mirabilis, Proteus vulgaris, Providencia rettgeri, Providencia stuartii, Providencia spp, Pseudomonas aeruginosa, Pseudomonas spp, Salmonella spp, Serratia marcescens, Serratia spp.
Anaerobic microorganisms: Bacteroides fragilis, Bifidobacterium spp, Clostridium perfringens, Fusobacterium spp, Peptostreptococcus, Propionibacterum spp, Veilonella spp.
Other microorganisms: Bartonella spp, Chlamydia pneumoniae, Chlamydia psittaci, Chlamydia trachomatis, Legionella pneumophila, Legionella spp, Mycobacterium spp, Mycobacterium leprae, Micobacterium tuberculosis, Mycoplasma hominis, Mycoplasma pneumoniae, Ricketsia spp, Ureaplasma urealyticum.
Composition and release form Levofloxacin 250 mg 5 pcs. film-coated tablets
Tablets - 1 tablet:
- Active ingredients: levofloxacin hemihydrate - 256.23 mg. 9 corresponds to the content of levofloxacin - 250 mg);
- Excipients: microcrystalline cellulose, hypromellose (hydroxypropyl methylcellulose), primellose (croscarmellose sodium), calcium stearate.
- Shell composition: hypromellose, macrogol 4000, talc, titanium dioxide, yellow iron oxide dye.
5/10 pcs. — polymer cans/blister packaging, cardboard packs.
Description of the dosage form
Yellow film-coated tablets, round, biconvex; On a cross section, two layers are visible.
Directions for use and doses
The drug is taken orally 1 or 2 times a day. Do not chew the tablets and take a sufficient amount of liquid (from 0.5 to 1 glass); you can take them before meals or between meals. Doses are determined by the nature and severity of the infection, as well as the sensitivity of the suspected pathogen.
For patients with normal or moderately reduced renal function (creatinine clearance > 50 ml/min.), the following dosage regimen is recommended: sinusitis: 500 mg 1 time per day - 10-14 days; exacerbation of chronic bronchitis: 250 mg or 500 mg 1 time per day - 7-10 days; community-acquired pneumonia: 500 mg 1-2 times a day - 7-14 days. uncomplicated urinary tract infections: 250 mg 1 time per day for 3 days; prostatitis: 500 mg - 1 time per day - 28 days; complicated urinary tract infections, including pyelonephritis: 250 mg 1 time per day - 7-10 days; infections of the skin and soft tissues: 250 mg 1 time a day or 500 mg 1-2 times a day - 7-14 days; septicemia/bacteremia: 250 mg or 500 mg 1-2 times a day for 10-14 days; intra-abdominal infection: 250 mg or 500 mg 1 time per day - 7-14 days (in combination with antibacterial drugs acting on anaerobic flora).
Patients undergoing hemodialysis or continuous ambulatory peritoneal dialysis do not require additional doses.
Patients with impaired liver function do not require special dosing, since levofloxacin is metabolized in the liver only to an extremely small extent.
As with the use of other antibiotics, treatment with Levofloxacin is recommended to be continued for at least 48-78 hours after normalization of body temperature or after laboratory confirmed recovery.
Pharmacokinetics
Levofloxacin is rapidly and almost completely absorbed after oral administration. Food intake has little effect on the speed and completeness of absorption. The bioavailability of 500 mg levofloxacin after oral administration is almost 100%. After taking a single dose of 500 mg of levofloxacin, Cmax is 5.2-6.9 mcg/ml, the time to reach Cmax is 1.3 hours, T1/2 is 6-8 hours.
Bonding with plasma proteins is 30-40%. Penetrates well into organs and tissues: lungs, bronchial mucosa, sputum, genitourinary organs, bone tissue, cerebrospinal fluid, prostate gland, polymorphonuclear leukocytes, alveolar macrophages.
In the liver, a small portion is oxidized and/or deacetylated. It is excreted from the body primarily by the kidneys by glomerular filtration and tubular secretion. After oral administration, approximately 87% of the dose taken is excreted unchanged in the urine within 48 hours, less than 4% in the feces within 72 hours.
Indications for use Levofloxacin 250 mg 5 pcs. film-coated tablets
Infectious and inflammatory diseases caused by sensitive microorganisms:
- acute sinusitis;
- exacerbation of chronic bronchitis;
- community-acquired pneumonia;
- complicated urinary tract infections (including pyelonephritis);
- uncomplicated urinary tract infections;
- prostatitis;
- infections of the skin and soft tissues;
- septicemia/bacteremia associated with the above indications;
- intra-abdominal infection.
Contraindications
- hypersensitivity to levofloxacin or other quinolones;
- renal failure (with creatinine clearance less than 20 ml/min. - due to the impossibility of dosing this dosage form);
- epilepsy;
- tendon lesions due to previous treatment with quinolones;
- childhood and adolescence (up to 18 years);
- pregnancy and lactation period.
It should be used with caution in the elderly due to the high likelihood of a concomitant decrease in renal function, as well as in cases of glucose-6-phosphate dehydrogenase deficiency.
Application Levofloxacin 250 mg 5 pcs. film-coated tablets during pregnancy and breastfeeding
Contraindicated during pregnancy and lactation. Levofloxacin should not be used to treat children and adolescents (under 18 years of age) due to the likelihood of damage to articular cartilage.
special instructions
Levofloxacin should not be used to treat children and adolescents due to the likelihood of damage to articular cartilage.
When treating elderly patients, it should be borne in mind that patients in this group often suffer from impaired renal function.
In severe pneumonia caused by pneumococci, levofloxacin may not provide an optimal therapeutic effect. Hospital-acquired infections caused by certain pathogens (P. aeruginosa) may require combination treatment.
During treatment with Levofloxacin, seizures may develop in patients with previous brain damage caused, for example, by stroke or severe trauma.
Despite the fact that photosensitivity is observed very rarely with the use of levofloxacin, in order to avoid it, patients are not recommended to be exposed to strong solar or artificial ultraviolet irradiation unnecessarily.
If pseudomembranous colitis is suspected, levofloxacin should be discontinued immediately and appropriate treatment should be initiated. In such cases, drugs that inhibit intestinal motility should not be used.
Rarely observed with the use of the drug Levofloxacin, tendonitis (primarily inflammation of the Achilles tendon) can lead to tendon rupture. Elderly patients are more prone to tendinitis. Treatment with glucocorticosteroids appears to increase the risk of tendon rupture. If tendonitis is suspected, treatment with Levofloxacin should be stopped immediately and appropriate treatment of the affected tendon should be initiated.
Patients with glucose-6-phosphate dehydrogenase deficiency (an inherited metabolic disorder) may respond to fluoroquinolones by destroying red blood cells (hemolysis). In this regard, treatment of such patients with levofloxacin should be carried out with great caution.
Impact on the ability to drive vehicles and operate machinery
Side effects of Levofloxacin, such as dizziness or drowsiness, drowsiness and visual disturbances, may impair reactivity and ability to concentrate. This may pose a risk in situations where these abilities are of particular importance (for example, when driving a car, when servicing machinery, when performing work in an unstable position).
Overdose
Symptoms of an overdose of Levofloxacin appear at the level of the central nervous system (confusion, dizziness, disturbances of consciousness and seizures of the epileptic type). In addition, gastrointestinal disorders (for example, nausea) and erosive lesions of the mucous membranes, prolongation of the QT interval may occur.
Treatment should be symptomatic. Levofloxacin is not eliminated by dialysis (hemodialysis, peritoneal dialysis and continuous peritoneal dialysis). There is no specific antidote.
Side effects Levofloxacin 250 mg 5 pcs. film-coated tablets
Allergic reactions: sometimes – itching and redness of the skin; rarely - general hypersensitivity reactions (anaphylactic and anaphylactoid reactions) with symptoms such as urticaria, constriction of the bronchi and possibly severe suffocation; very rarely - swelling of the skin and mucous membranes (for example, in the face and throat), sudden drop in blood pressure and shock, increased sensitivity to solar and ultraviolet radiation, allergic pneumonitis, vasculitis; in some cases - severe skin rashes with blistering, for example, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell's syndrome) and exudative erythema multiforme. General hypersensitivity reactions may sometimes be preceded by milder skin reactions. The above reactions can develop after the first dose, a few minutes or hours after administration of the drug.
From the digestive system: often - nausea, diarrhea, increased activity of liver enzymes (for example, alanine aminotransferase and aspartate aminotransferase); sometimes - loss of appetite, vomiting, abdominal pain, digestive disorders; rarely - diarrhea mixed with blood, which in very rare cases can be a sign of intestinal inflammation and even pseudomembranous colitis.
On the metabolic side: very rarely - a decrease in the concentration of glucose in the blood, which is of particular importance for patients with diabetes (possible signs of hypoglycemia: increased appetite, nervousness, perspiration, trembling). Experience with the use of other quinolones suggests that they can cause exacerbation of porphyria in patients already suffering from this disease. A similar effect cannot be excluded when using the drug levofloxacin.
From the nervous system: sometimes - headache, dizziness and/or stupor, drowsiness, sleep disturbances; rarely - anxiety, paresthesia in the hands, trembling, psychotic reactions such as hallucinations and depression, agitation, convulsions and confusion; very rarely - impaired vision and hearing, impaired taste and smell, decreased tactile sensitivity.
From the cardiovascular system: rarely - increased heartbeat, decreased blood pressure; very rarely - vascular (shock-like) collapse; in some cases - prolongation of the QT interval.
From the musculoskeletal system: rarely - tendon damage (including tendinitis), joint and muscle pain; very rarely - tendon rupture (for example, Achilles tendon); this side effect can be observed within 48 hours after the start of treatment and can be bilateral in nature, muscle weakness, which is of particular importance for patients with bulbar syndrome; in some cases - muscle damage (rhabdomyolysis).
From the urinary system: rarely - increased levels of bilirubin and creatinine in the blood serum; very rarely - deterioration of kidney function up to acute renal failure, interstitial nephritis.
From the hematopoietic organs: sometimes - an increase in the number of eosinophils, a decrease in the number of leukocytes; rarely - neutropenia, thrombocytopenia, which may be accompanied by increased bleeding; very rarely - agranulocytosis and the development of severe infections (persistent or recurrent increase in body temperature, deterioration in health); in some cases - hemolytic anemia; pancytopenia.
Other: sometimes - general weakness; very rarely - fever.
Any antibiotic therapy can cause changes in the microflora that is normally present in humans. For this reason, increased proliferation of bacteria and fungi resistant to the antibiotic used may occur, which in rare cases may require additional treatment.
Drug interactions
There are reports of a pronounced decrease in the threshold of convulsive readiness with the simultaneous use of quinolones and substances that can, in turn, reduce the cerebral threshold of convulsive readiness. This also applies equally to the simultaneous use of quinolones and theophylline.
The effect of Levofloxacin is significantly weakened when used simultaneously with sucralfate. The same thing happens with the simultaneous use of magnesium or aluminum containing antacids, as well as iron salts. Levofloxacin should be taken at least 2 hours before or 2 hours after taking these medications. No interaction was detected with calcium carbonate.
When using vitamin K antagonists simultaneously, monitoring of the blood coagulation system is necessary.
The elimination (renal clearance) of levofloxacin is slightly slowed down by the action of cimetidine and probenecid. It should be noted that this interaction has virtually no clinical significance. However, with the simultaneous use of drugs such as probenecid and cimetidine, which block a certain excretion pathway (tubular secretion), treatment with levofloxacin should be carried out with caution. This applies primarily to patients with limited renal function.
Levofloxacin slightly increases the half-life of cyclosporine.
Taking glucocorticosteroids increases the risk of tendon rupture.
Levofloxacin analogs
On pharmacy shelves there is an assortment of foreign and Russian analogues of Levofloxacin in ampoules, tablets, and also in the form of eye drops. When choosing an identical substitute, you should pay attention to products that are similar in composition (active ingredient). The main differences between the products are the manufacturer, price category and pharmacological action. Most drugs are available by prescription, so it is recommended that you first seek additional advice from a specialist to make an accurate diagnosis and eliminate restrictions.
List of Levofloxacin analogues with prices
| Drug name | price, rub. | Manufacturer country |
| Levofloxacin | 140-890 | Russia |
| Popular substitutes | ||
| Amoxiclav | 120-450 | Slovenia |
| Tavanik | 500-1150 | France |
| Azithromycin | 100-310 | Russia |
| Norfloxacin | 200-340 | |
| Ceftriaxone | 30-200 | |
| Glevo | 40-200 | India |
| Ofloxacin | 40-200 | Russia, Hungary |
| Ciprofloxacin | 40-130 | |
| Sumamed | 230-610 | Croatia |
| Other analogues | ||
| Moxifloxacin | 160-550 | Russia, Hungary |
| Clarithromycin | 150-580 | Russia, Croatia |
| Suprax | 550-1100 | Jordan, Italy |
| Klacid | 520-890 | Italy, UK |
| Augmentin | 140-460 | UK, France |
| Biseptol | 40-150 | Poland |
| Flemoklav Solutab | 300-420 | Netherlands |
| Vilprafen | 300-1300 | France, Germany, Italy |
| Avelox | 630-680 | Germany |
| Tsifran | 40-340 | India |
| Eleflox | 850-920 | |
| Hyleflox | 420-480 | |
| Tsiprolet | 50-230 | |
| Levolet | 400-590 | |
| Leflobakt | 250-510 | Russia |
| Doxycycline | 300-340 | |
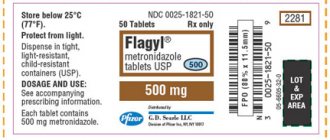
| Metronidazole | 70-190 | |
| Flexid | 250-310 | Slovenia |
| Nolitsin | 230-450 | |
Levofloxacin or Amoxiclav - which is better for pneumonia
Manufacturer: SANDOS, Slovenia
Release form: powder for suspensions, tablets
Active ingredient: amoxicillin + clavulanic acid
Amoxiclav is an analogue cheaper than Levofloxacin. This is an antimicrobial agent with a wide spectrum of action, which is prescribed to patients for various infectious diseases in gynecology, otolaryngology, urology, and pulmonology. It is prescribed to children from birth, but depending on the form of release. The antibiotic contains a penicillin series of substances. Has a detrimental effect on organisms and strains that are not resistant to amoxicillin.
Indications for taking the imported analogue do not depend on the patient’s age group. This substitute for Levofloxacin 500 mg is prescribed for the following infectious diseases and disorders:
- Upper respiratory tract and ENT organs.
- Lower respiratory tract.
- Urinary tract and genital organs.
- Skin, soft tissues.
- Bone and connective tissue.
- Biliary tract.
- For odontogenic infections.
For pneumonia, it is recommended to use one of the drugs presented, since they are effective for this disorder and can stabilize the patient’s condition within several days.
Antibacterial chemotherapy
When making a diagnosis of pneumonia, the practitioner must immediately determine the ABT program, which means choosing a first-line antibiotic, its daily dose, method of administration and frequency of administration of the drug. In the following days, questions about the advisability of ABT correction and the optimal timing of its use are resolved. It is important that our country allows the medical use of numerous generics. For example, in the United States, the use of a brand name ciprofloxacin and three generics is permitted. In the Russian Federation (RF), in addition to the brand, the medical use of more than 60 generics of ciprofloxacin is permitted. A brand is a patent-protected drug developed and manufactured by a company. Brands undergo thorough clinical testing, their use is permitted only after successful proof of the drug’s high effectiveness and good tolerability. Brands are naturally more expensive than generics, which are approved for medical use without clinical testing. Generics cost significantly less, sometimes due to the use of cheaper excipients. Some scientific studies comparing brand and generic drugs have shown that brand-name antibiotics are superior in efficacy and tolerability.
In our country, the majority of patients with pneumonia are hospitalized. Domestic formularies for the treatment of pneumonia largely correspond to international ones, which provide for the treatment of pneumonia both at home and in a hospital setting. Optimal antibacterial treatment involves the correct choice of antibiotic, its dosage and duration of treatment. The federal standard for the treatment of pneumonia requires treatment for 7 days. This is acceptable for uncomplicated pneumonia of mild to moderate severity. It is important that therapy should be prolonged not only in case of abscess formation or development of pleural empyema, but also depending on the etiological agents. Thus, for mycoplasma and chlamydial pneumonia, the duration of antibacterial therapy is 14 days, and for legionella pneumonia – up to 21 days. In all formularies for the treatment of pneumonia, the so-called so-called antibacterial agent is given as an important antibacterial agent. respiratory fluoroquinolones: levofloxacin (Tavanic) and moxifloxacin.
Tavanic (levofloxacin brand) well suppresses gram-positive microorganisms: streptococci, pneumococci, staphylococci, listeria, corynebacteria and, to a lesser extent, enterococci. It has high activity against most gram-negative bacteria - Haemophilus influenzae, Moraxella, Acinetobacter, Enterobacter, Citrobacter and somewhat less activity against Pseudomonas aeruginosa, Escherichia coli, Klebsiella. Levofloxacin is highly active against legionella, mycoplasma and chlamydia; it also inhibits mycobacterium tuberculosis and some anaerobes.
Levofloxacin is well absorbed and characterized by high bioavailability (up to 99%). This creates high concentrations of the drug in the bronchial mucosa, alveolar macrophages, and pulmonary parenchyma, exceeding those in the blood serum. It is important that the pharmacokinetics allow the use of levofloxacin once a day (which ensures good adherence to therapy) at a dose of 500 mg. Levofloxacin is generally well tolerated [1–4]. The drug, to a lesser extent than other fluoroquinolones, is characterized by hepatotoxicity and phototoxicity, and prolongation of the QT interval on the electrocardiogram. The drug should not be prescribed to persons allergic to any quinolones, as well as to children, pregnant and nursing mothers.
A wide spectrum of antibacterial activity, high bioavailability, pharmacokinetics and distribution in the respiratory system, and good tolerability determine the possibility of using levofloxacin as a first-line drug in the treatment of community-acquired pneumonia (evidence level A) [6, 7]. Its high effectiveness has been proven for respiratory tract infections, community-acquired and hospital-acquired pneumonia, and urinary tract infections. Tavanic is approved for medical use in the Russian Federation in two dosage forms: tablets of 500 and 250 mg for oral administration and a solution for intravenous administration in 100 ml bottles containing 500 mg of the drug. Tavanik is taken orally before meals or in the interval between meals. The intravenous infusion of the drug should be long (at least 60 minutes). During treatment with Tavanik, insolation and ultraviolet irradiation should be avoided. If tendonitis develops, levofloxacin is immediately discontinued. In the hospital, for the treatment of community-acquired pneumonia, especially severe ones and when the possibility of infection by intracellular agents is suspected, β-lactam antibiotics are prescribed in combination with macrolides [1–4]. Also, instead of a combination of two antibacterial agents, monotherapy with respiratory fluoroquinolones (levofloxacin, moxifloxacin) is possible.
In cases of severe pneumonia, antibiotics should be used intravenously as early as possible (immediate ABT implies the first administration of an antibiotic within two hours of diagnosis).
In the Department of Pulmonology of the Federal State Institution “Central Clinical Hospital with Polyclinic” of the Presidential Administration of the Russian Federation, among the respiratory fluoroquinolones, Tavanik is widely used, which in recent years has been used to treat more than 400 patients with pneumonia.
The main criteria for the decision to prescribe Tavanik to patients diagnosed with community-acquired pneumonia of moderate and severe course: • late diagnosis of pneumonia (on the 5-10th day from the onset of the disease) without pre-hospital antibiotic therapy; • unsuccessful use of β-lactam antibiotics (in effective doses) in the prehospital stage.
Other reasons for prescribing Tavanik were: • lobar and multilobar pneumonia in patients with allergies to β-lactam antibiotics; • pneumonia in epidemiological outbreaks (outbreaks of respiratory infections in a family or community). • in the absence of effect from the initial ABT with 3rd generation cephalosporins in combination with macrolides.
Naturally, in the conditions of the pulmonology department, the use of Tavanik began with intravenous infusions of 500 mg once a day. For lobar and multilobar pneumonia, on the first day of treatment the daily dose was 1000 mg, which made it possible to obtain a clear clinical effect within 24 hours. In the following days, the usual dosages of the drug were used - 500 mg every 24 hours intravenously. In severe cases or in persons with a resected stomach, the drug was used only intravenously. The average duration of treatment was 10–12 days. The desire to ensure high efficiency of treatment while reducing its cost and reducing the number of injections justified the widespread use of stepdown therapy programs in the department, which have been introduced into the practice of the department since 1994. When using this technique, treatment begins with parenteral administration of an antibiotic. When a clinical effect is achieved, 2–3 days from the start of therapy, intravenous use of the drug is replaced by oral administration of the antibiotic. The average duration of treatment for stepwise therapy was 10 days. This therapy is easier to tolerate by patients and is less likely to be accompanied by side effects.
The analysis showed that the most widely used regimen of stepwise monotherapy with levofloxacin 500 mg intravenously every 24 hours for 2–3 days, followed by switching to oral administration of 500 mg every 24 hours, was effective in the treatment of community-acquired pneumonia of moderate severity in the majority of patients. The initial daily dosage of 1000 mg was used to a limited extent in approximately 10% of the most severely ill patients. Side effects from the gastrointestinal tract, noted in several subjects (previously treated for chronic colitis), were short-lived and regressed after the use of eubiotics, antispasmodics and completion of therapy with a respiratory fluoroquinolone.
Over the past four years, there have been an unusually large number of patients with multilobar pneumonia with extremely severe septic conditions requiring intensive care using artificial ventilation (ALV). In almost all such clinical situations, we used combined ABT, consisting of Tavanic 500 mg intravenously every 24 hours and meropenem 1000 mg intravenously every 8 hours. This therapy was quite effective, as evidenced by the recovery of elderly patients who were on mechanical ventilation for 52 and 74 days.
Several years ago, a multicenter international study was conducted in which Tavanic was used for the treatment of hospital-acquired pneumonia at a dosage of 750 mg intravenously once daily. According to the results of this study, high doses of Tavanic are also effective in the treatment of nosocomial pneumonia.
Levofloxacin or Tavanic - which is better, what is the difference
Manufacturer: SANOFI, France
Release form: tablets
Active ingredient: levofloxacin hemihydrate
Tavanic is an analogue of Levofloxacin tablets to the active substance. This is a synthetic antibacterial drug from the group of fluoroquinolones. The composition includes the same active ingredient, which has a detrimental effect on microorganisms and their cell structures. The antibiotic is prescribed to patients for infectious and inflammatory pathologies of the lower respiratory tract, reproductive system and urinary tract, skin and soft tissues.
Tavanik tablets are prescribed for drug-resistant forms of tuberculosis, for the prevention of anthrax. For pneumonia, one of the drugs presented is prescribed. The drugs show positive results for these disorders and are able to normalize the patient’s condition in the shortest possible time. This eliminates relapse and transition of the pathology to the chronic stage. Reviews from both doctors and patients are positive.
The value of levofloxacin for respiratory and urogenital infections in outpatient practice
The first fluoroquinolone drugs appeared in clinical practice in the early 1980s. They were characterized by a wide spectrum of antimicrobial activity and favorable tissue pharmacokinetics (concentrations in most tissues exceeded serum levels). The unique mechanism of action of fluoroquinolones on microbial cells (inhibition of DNA gyrase or topoisomerase IV) explained the lack of cross-resistance with other classes of antimicrobial agents.
The most well-studied early fluoroquinolones are ciprofloxacin and ofloxacin. Fluoroquinolones have taken leading positions in the treatment of various bacterial infections, primarily nosocomial ones, the main pathogens of which are gram-negative bacteria.
The disadvantage of early fluoroquinolones is their low natural activity against gram-positive microorganisms, primarily Streptococcus pneumoniae, which did not allow these drugs to be recommended for the treatment of community-acquired respiratory infections.
At the end of the 1990s. drugs of the fluoroquinolone group appeared, fundamentally different in antimicrobial properties from earlier drugs. These differences are, first of all, characterized by significantly higher natural activity against gram-positive bacteria (pneumococci, staphylococci) and atypical microorganisms (chlamydia, mycoplasmas). These drugs were called "new fluoroquinolones" or "respiratory fluoroquinolones." The first of the respiratory fluoroquinolones was levofloxacin, later other drugs appeared (gemifloxacin, moxifloxacin).
Due to the high activity of the new fluoroquinolones against Gram-positive microbes, including S. pneumoniae, resistant to other antibiotics, they were mainly marketed for the treatment of community-acquired respiratory tract infections, and therefore they are sometimes called “respiratory fluoroquinolones.” Also, new fluoroquinolones, along with increased activity against gram-positive bacteria, retain, and in some cases exceed, the high activity of earlier fluoroquinolones against gram-negative bacteria.
Levofloxacin is characterized by high natural activity against all pathogens of community-acquired respiratory infections. In addition, levofloxacin is characterized by good tissue pharmacokinetics, in particular, high tissue and intracellular concentrations of the drug are maintained at therapeutic levels for 24 hours.
A large number of controlled clinical studies have shown:
- Levofloxacin is not inferior in effectiveness to β -lactam antibiotics for community-acquired respiratory infections;
- Levofloxacin in monotherapy is not inferior in effectiveness to combined regimens ( β -lactam + macrolide) for pneumonia of any severity;
- Levofloxacin is characterized by higher efficacy in monotherapy compared to the ceftriaxone/macrolide combination in severe community-acquired pneumonia;
- Higher effectiveness of levofloxacin compared to macrolide antibiotics for community-acquired legionella pneumonia;
- The advantage of levofloxacin compared to macrolide antibiotics in exacerbation of COPD both in eradication of Haemophilus influenzae and in the duration of the relapse-free period.
The most common causative agents of urinary tract infections are Escherichia coli and other enterobacteriaceae; gram-positive microorganisms are less common. Levofloxacin is characterized by high natural activity against these pathogens, comparable to the activity of ciprofloxacin, and superior to it against staphylococci and enterococci.
In recent years, in almost all regions of the world, there has been an increase in the resistance of urogenital strains of Escherichia coli and other enterobacteria to almost all antimicrobial drugs, including fluoroquinolones. The decrease in the sensitivity of enterobacteria to levofloxacin is compensated by high concentrations of the drug in the urine (250-300 μg/ml), which is many times higher than the MIC90 values. It is also characterized by good penetration into the tissues of the genitourinary system, where its concentrations are 2-5 times higher than serum concentrations. This explains the fact that, despite some reduction in the sensitivity of uropathogens, levofloxacin continues to demonstrate high efficacy against urogenital infections in controlled clinical trials.
Levofloxacin also has good penetration into the secretions and tissue of the prostate gland, which are difficult to reach for most antibiotics. An hour after a single dose of 250 mg, the concentration of levofloxacin in the prostate secretion averaged 0.89 mcg/ml, in the seminal fluid -3.25 mcg/ml, with an average concentration in the blood of -1.7 mcg/ml. The clinical effectiveness of levofloxacin has been confirmed in controlled clinical studies.
Levofloxacin has advantages over earlier fluoroquinolones in the treatment of chronic bacterial prostate and urogenital chlamydia, both in tissue pharmacokinetics and higher natural activity against some actual pathogens, primarily Enterococcus faecalis, Ureaplasma urealyticum, Chlamydia trachomatis.
Thus, along with community-acquired respiratory infections, levofloxacin can be positioned as a drug of choice in the treatment of complicated urinary infections, bacterial prostatitis and some other sexually transmitted diseases.
Recommendations for wider use of levofloxacin for respiratory and urinary infections in outpatient practice are supported by data on the good tolerability and safety of the drug.
Levofloxacin or Azithromycin - which is better and stronger
Manufacturer: Vertex, Russia
Release form: capsules
Active ingredient: azithromycin
What else can replace Levofloxacin for pneumonia? Azithromycin is an antibacterial agent that has a broad spectrum of action. It has bacteriostatic and bactericidal properties.
This analogue of the antibiotic Levofloxacin is prescribed to adults and children over 12 years of age for infectious disorders and pathologies:
- Upper, lower respiratory tract and ENT organs (including pneumonia, bronchitis).
- Skin and soft tissues.
- Genitourinary system.
- With borreliosis.
Azithromycin is also included in the combination therapy of gastrointestinal pathologies caused by Helicobacter pylori.
Levofloxacin or Ciprofloxacin – which is better and more effective?
Manufacturer: RAFARMA, Russia
Release form: tablets, eye drops
Active ingredient: ciprofloxacin
Ciprofloxacin is a prescription analogue of Levofloxacin with the same active ingredient in the composition. This is an antimicrobial drug with a broad spectrum of action that has a bactericidal effect.
It has a detrimental effect on most pathogens that provoke infectious and inflammatory pathologies of the respiratory tract, abdominal cavity, pelvic organs, bone and joint tissue.
It is also prescribed for patients of the older age group for septicemia and diseases in otolaryngology. Ciprofloxacin can be used as a prophylactic against infections in immunocompromised patients, as well as for prostatitis in men.
To achieve maximum results from therapy, you must adhere to the prescribed dosage and course duration.
Contraindications
Hypersensitivity to levofloxacin, other fluoroquinolones or components of the drug, epilepsy, tendon damage during previous treatment with quinolones, pregnancy, lactation, childhood and adolescence (up to 18 years), myasthenia gravis.
Lactose intolerance or lactase deficiency, as well as glucose-galactose malabsorption.
Due to the inability to split the tablet in two, the use of the drug is contraindicated in patients with impaired renal function:
- in patients with creatinine clearance less than 50 ml/min, it is impossible to use a dosage regimen with an initial dosage of 250 mg/24 hours;
- in patients with creatinine clearance less than 20 ml/min, it is impossible to use the dosage regimen with an initial dosage of 500 mg/24 hours and 500 mg/12 hours;
- when creatinine clearance is less than 10 ml/min (including during hemodialysis and continuous ambulatory peritoneal dialysis), it is impossible to use it for all dosage regimens.
Levofloxacin or Norfloxacin – which is better?
Manufacturer: OBOLENSKOE FP, Russia
Release form: tablets
Active ingredient: norfloxacin
Norfloxacin is a prescription analogue of Levofloxacin 100 mg, which contains the active ingredient of the same name. Refers to antimicrobial synthetic drugs. Has a bactericidal effect. The substitute is active against most gram-negative bacteria.
It is worth noting that the substance norfloxacin penetrates the placental barrier. It is excreted along with urine. Prescribed to patients of the older age group for urinary tract infections, prostatitis, uncomplicated gonorrhea.
Before starting the course, it is recommended to pay attention to existing restrictions, as well as drug interactions.
Oftadek
Oftadek eye drops are antimicrobial drugs. They produce antiseptic and antimicrobial effects against gram-positive and gram-negative bacteria. Used for complex treatment of eye diseases.
Indications for use:
- acute and chronic conjunctivitis;
- damage to the mucous membrane of the eyes by chlamydia;
- prevention of blenorrhea in newborns;
- prevention of complications in the postoperative period;
- processing of contact lenses.
Adverse reactions are rare. Price - 100-115 rubles.
Levofloxacin or Ceftriaxone – which is better and more effective for pneumonia
Manufacturer: PHARMSTANDARD+, Russia
Release form: powder for the preparation of solution for injection
Active ingredient: ceftriaxone
Ceftriaxone is an analogue of Levofloxacin infusion solution, which is even prescribed to women during pregnancy, but only in the second and third trimester. The drug is classified as a third generation cephalosporin antibiotic. The drug has bactericidal properties.
A new generation analogue of Levofloxacin injections is prescribed to patients with infectious pathologies of the respiratory tract, skin, genitourinary system, bone, joint and connective tissue. Used in otolaryngology. The drug is also prescribed as a prophylaxis after surgery.
Levofloxacin or Glevo – which is better?
Manufacturer: GLENMARK FAMACEUTICS, India
Release form: tablets
Active ingredient: levofloxacin
Glevo is a prescription analogue of Levofloxacin, which contains the same active ingredient. Refers to antibacterial drugs with a wide spectrum of action. The drug is active against most pathogenic microorganisms that provoke infectious and inflammatory pathologies.
Prescribed for sinusitis, chronic bronchitis, community-acquired pneumonia, urinary tract and abdominal infections, bacterial prostatitis, pathologies of the skin and soft tissues, and bacteremia.
The main difference between these antibiotics is that the Glevo analogue is recommended for patients even with drug-resistant forms of tuberculosis.
Description
Capsule-shaped biconvex tablets, film-coated, white or almost white; on the cross section two layers are visible, the inner layer is light yellow to yellow in color, white inclusions are allowed.
Pharmacotherapeutic group:
antimicrobial agent, fluoroquinolone.
ATX code:
J01MA12.
Pharmacological properties
Pharmacodynamics
Levofloxacin is a synthetic broad-spectrum antibacterial drug from the group of fluoroquinolones, containing the levorotatory isomer of ofloxacin as an active substance.
Levofloxacin blocks DNA gyrase, disrupts supercoiling and cross-linking of DNA breaks, inhibits DNA synthesis, and causes profound morphological changes in the cytoplasm, cell wall and membranes of bacteria.
Levofloxacin has a bactericidal effect and is active against a large number of pathogens of bacterial infections both in vitro
, and
in vivo
.
Sensitive microorganisms (minimum inhibitory concentration (MIC) ≤ 2 mg/l):
- aerobic gram-positive microorganisms: Bacillus anthracis , Corynebacterium diphtheriae , Corynebacterium jeikeium , Enterococcus spp
., including
Enterococcus faecalis, Listeria monocytogenes, Staphylococcus spp.
( coagulase-negative, methicillin-sensitive/leukotoxin-containing/moderately sensitive strains), including
Staphylococcus aureus (
methicillin-sensitive strains
), Staphylococcus epidermidis (
methicillin-sensitive strains
), Streptococcus spp.
groups C and G, Streptococcus agalactiae, Streptococcus pneumoniae ( penicillin-sensitive / moderately sensitive / resistant strains
), Streptococcus pyogenes, Streptococcus spp.
Viridans group ( penicillin-sensitive/resistant strains
); - aerobic gram-negative microorganisms: Acinetobacter spp .
, including
Acinetobacter baumannii , Acinetobacillus actinomycetemcomitans , Citrobacter freundii , Eikenella corrodens , Enterobacter spp
., including
Enterobacter aerogenes , Enterobacter cloacae , Escherichia coli , Gardnerella vaginalis , Haemophilus ducreyi , Haemophilus influenzae
(ampicillin-sensitive/ resistant strains),
Haemophilus parainfluenzae , Helicobacter pylori , Klebsiella spp
., including
Klebsiella oxytoca , Klebsiella pneumoniae , Moraxella catarrhalis
(beta-lactamase producing and non-producing strains),
Morganella morganii , Neisseria gonorrhoeae
(penicillinase producing and non-producing strains),
Neisseria meningitidis , Pasteurella spp .
, including
Pasteurella canis , Pasteurella dagmatis , Pasteurella multocida , Proteus mirabilis , Proteus vulgaris , Providencia spp
., including
Providencia rettgeri , Providencia stuartii , Pseudomonas spp .
, including
Pseudomonas aeruginosa
(hospital infections caused by
Pseudomonas aeruginosa
may require combination treatment),
Serratia spp
., including
Serratia marcescens , Salmonella spp
.; - anaerobic microorganisms: Bacteroides fragilis , Bifidobacterium spp ., Clostridium perfringens , Fusobacterium spp ., Peptostreptococcus spp ., Propionibacterium spp ., Veillonella spp
.; - other microorganisms: Bartonella spp ., Chlamydia pneumoniae , Chlamydia psittaci , Chlamydia trachomatis , Legionella pneumophila , Legionella spp ., Mycobacterium spp .
, including
Mycobacterium leprae , Mycobacterium tuberculosis , Mycoplasma hominis , Mycoplasma pneumoniae , Rickettsia spp ., Ureaplasma urealyticum
.
Moderately sensitive microorganisms (MIC = 4 mg/l):
- aerobic gram-positive microorganisms: Corynebacterium urealyticum , Corynebacterium xerosis , Enterococcus faecium , Staphylococcus epidermidis
(methicillin-resistant strains),
Staphylococcus haemolyticus
(methicillin-resistant strains); - aerobic gram-negative microorganisms: Campylobacter jejuni , Campylobacter coli
; - anaerobic microorganisms: Prevotella spp ., Porphyromonas spp
.
Resistant microorganisms (MIC more than 8 mg/l):
- aerobic gram-positive microorganisms: Staphylococcus aureus
(methicillin-resistant strains), other
Staphylococcus spp
. (coagulase-negative methicillin-resistant strains); - aerobic gram-negative microorganisms: Alcaligenes xylosoxidans
; - anaerobic microorganisms: Bacteroides thetaiotaomicron
- other microorganisms: Mycobacterium avium
.
Clinical efficacy (effectiveness in clinical studies against infections caused by the following microorganisms):
- aerobic gram-positive microorganisms: Enterococcus faecalis , Staphylococcus aureus , Streptococcus pneumoniae , Streptococcus pyogenes
; - aerobic gram-negative microorganisms: Citrobacter freundii , Enterobacter cloacae , Escherichia coli , Haemophilus influenzae , Haemophilus parainfluenzae , Klebsiella pneumoniae , Moraxella catarrhalis , Morganella morganii , Proteus mirabilis , Pseudomonas aeruginosa , Serratia marcescens
; - other microorganisms: Chlamydia pneumoniae , Legionella pneumophila , Mycoplasma pneumoniae
.
Resistance to levofloxacin develops as a result of a stepwise process of mutations in the genes encoding both type II topoisomerases: DNA gyrase and topoisomerase IV. Other resistance mechanisms, such as the mechanism of influencing the penetration barriers of the microbial cell (a mechanism characteristic of Pseudomonas
aeruginosa
) and the mechanism of efflux (active removal of the antimicrobial agent from the microbial cell), may also reduce the sensitivity of microorganisms to levofloxacin.
Due to the peculiarities of the mechanism of action of levofloxacin, cross-resistance between levofloxacin and other antimicrobial agents is not usually observed.
Pharmacokinetics
Absorption
Levofloxacin is rapidly and almost completely absorbed after oral administration; food intake has little effect on its absorption. Absolute bioavailability when taken orally is 99-100%. After a single dose of 500 mg of levofloxacin, the maximum concentration in blood plasma (Cmax) is reached within 1-2 hours and is 5.2 ± 1.2 μg/ml. The pharmacokinetics of levofloxacin is linear in the dose range from 50 to 1000 mg. The equilibrium state of levofloxacin concentration in blood plasma when taking 500 mg of levofloxacin 1 or 2 times a day is achieved within 48 hours.
On the 10th day of oral administration of the drug Levofloxacin Ecolevid® 500 mg 1 time per day, the Cmax of levofloxacin was 5.7 ± 1.4 mcg/ml, and the minimum concentration of levofloxacin (concentration before taking the next dose) (Cmin) in the blood plasma was 0.5 ±0.2 µg/ml.
On the 10th day of oral administration of the drug Levofloxacin Ecolevid® 500 mg 2 times a day, Cmax was 7.8 ± 1.1 μg/ml, and C min was 3.0 ± 0.9 μg/ml.
Distribution
The connection with serum proteins is 30-40%. After a single and repeated dose of 500 mg of levofloxacin, the volume of distribution of levofloxacin is, on average, 100 l, which indicates good penetration of levofloxacin into organs and tissues of the human body.
Penetration into the bronchial mucosa, epithelial lining fluid, alveolar macrophages
After a single oral dose of 500 mg of levofloxacin, the maximum concentrations of levofloxacin in the bronchial mucosa and epithelial lining fluid were reached within 1 hour or 4 hours and were 8.3 μg/g and 10.8 μg/ml, respectively, with penetration coefficients into the mucosa bronchi and epithelial lining fluid, compared with plasma concentrations of 1.1-1.8 and 0.8-3, respectively.
After 5 days of oral administration of 500 mg levofloxacin, the mean concentrations of levofloxacin 4 hours after the last dose in the epithelial lining fluid were 9.94 μg/ml and in alveolar macrophages - 97.9 μg/ml.
Penetration into lung tissue
Maximum concentrations in lung tissue after oral administration of 500 mg of levofloxacin were approximately 11.3 mcg/g and were achieved 4-6 hours after dosing with penetration coefficients of 2-5, compared with plasma concentrations.
Penetration into alveolar fluid
After 3 days of taking 500 mg of levofloxacin 1 or 2 times a day, the maximum concentrations of levofloxacin in the alveolar fluid were reached 2-4 hours after taking the drug and were 4.0 and 6.7 μg/ml, respectively, with a penetration coefficient of 1. compared to plasma concentrations.
Penetration into bone tissue
Levofloxacin penetrates well into cortical and cancellous bone tissue in both the proximal and distal parts of the femur, with a penetration coefficient (bone tissue/blood plasma) of 0.1-3. The maximum concentrations of levofloxacin in the cancellous bone tissue of the proximal femur after oral administration of 500 mg of the drug were approximately 15.1 mcg/g (2 hours after dosing).
Penetration into the cerebrospinal fluid
Levofloxacin penetrates poorly into the cerebrospinal fluid.
Penetration into prostate tissue
After oral administration of 500 mg of levofloxacin once daily for 3 days, the average concentration of levofloxacin in prostate tissue was 8.7 mcg/g, the average prostate/blood plasma concentration ratio was 1.84.
Concentrations in urine
Mean urinary concentrations 8 to 12 hours after oral doses of 150, 300, and 600 mg of levofloxacin were 44 mcg/mL, 91 mcg/mL, and 162 mcg/mL, respectively.
Metabolism
Levofloxacin is metabolized to a small extent (5% of the dose taken). Its metabolites are demethyllevofloxacin and levofloxacin N-oxide, which are excreted by the kidneys. Levofloxacin is stereochemically stable and does not undergo chiral transformations.
Removal
After oral administration, levofloxacin is relatively slowly eliminated from the blood plasma (half-life (T1/2) - 6-8 hours). Excretion is mainly through the kidneys (more than 85% of the dose taken). The total clearance of levofloxacin after a single dose of 500 mg was 175±29.2 ml/min.
There are no significant differences in the pharmacokinetics of levofloxacin when administered intravenously and orally, which confirms that oral and intravenous administration are interchangeable.
Pharmacokinetics in selected patient groups
The pharmacokinetics of levofloxacin do not differ between men and women.
Pharmacokinetics in elderly patients do not differ from those in younger patients, with the exception of differences in pharmacokinetics associated with differences in creatinine clearance (CC).
In renal failure, the pharmacokinetics of levofloxacin changes. As renal function deteriorates, renal excretion and renal clearance (CIR) decrease and T1/2 increases.
Pharmacokinetics in renal failure after a single oral dose of 500 mg of Levofloxacin Ecolevid®.
| CC (ml/min) | <20 | 20-49 | 50-80 |
| CIR (ml/min) | 13 | 26 | 57 |
| T1/2 (h) | 35 | 27 | 9 |
Ofloxacin or Levofloxacin – which is better?
Manufacturer: TEVA, Hungary
Release form: tablets
Active ingredient: ofloxacin
Ofloxacin is a foreign prescription analogue of Levofloxacin, which is classified as an antimicrobial agent. The composition includes the active ingredient of the same name. The drug has a bactericidal effect.
Prescribed to patients of the older age group for infectious and inflammatory pathologies of the lower respiratory tract, kidneys and urinary tract, genital and pelvic organs, as well as the skin and soft tissues.
The main difference between the drugs is the price category.
Sumamed or Levofloxacin – which is better?
Manufacturer: TEVA, Croatia
Release form: capsules, tablets, powder for suspension
Active ingredient: azithromycin
Sumamed is a foreign prescription analogue of Levofloxacin. It is a broad-spectrum bacteriostatic antibiotic. The drug has a detrimental effect on the cell membrane of the pathogenic microorganism.
The Sumamed analogue is recommended to be taken for infectious diseases of the upper and lower respiratory tract, including pneumonia, as well as for pathologies of the stomach and duodenum, erythema migrans, borreliosis, infections of the genitourinary tract, skin and soft tissues.
Levofloxacin-solofarm drops hl. 0.5% 5ml 1 piece
Pharmacological group:
Antimicrobial agent – fluoroquinolone.
Pharmacodynamics:
Levofloxacin is the L-isomer of the racemic drug substance ofloxacin. The antibacterial activity of ofloxacin relates mainly to the L-isomer. As an antibacterial drug of the fluoroquinolone class, levofloxacin blocks DNA gyrase (topoisomerase II) and topoisomerase IV, disrupts supercoiling and cross-linking of DNA breaks (deoxyribonucleic acid), suppresses DNA synthesis, causes profound morphological changes in the cytoplasm, cell wall and membranes. Mechanism of resistance development Resistance to levofloxacin can develop primarily through two main mechanisms, namely: a decrease in the intracellular concentration of the drug or changes in the targets of the drug. Changes in the targets of the two bacterial enzymes DNA gyrase and topoisomerase IV are the result of mutations in the chromosomal genes encoding DNA gyrase (gyrA and gyrB) and topoisomerase IV (parC and parE; grlA and grlB in Staphylococcus aureus). Drug resistance due to low intracellular concentration develops as a result of changes in the porin channel system of the outer cell membrane, which leads to a decrease in fluoroquinolone entry into gram-negative bacteria, or from efflux pumps. Efflux-mediated resistance has been described for pneumococci (PmrA), staphylococci (NorA), anaerobic and gram-negative bacteria. Plasmid-mediated quinolone resistance (defined by the qnr gene) has been detected against Klebsiella pneumoniae and Escherichia coli. The development of cross-resistance between fluoroquinolones is possible. Single mutations may not lead to clinical resistance, but multiple mutations cause clinical resistance to all drugs in the fluoroquinolone class. Alterable outer membrane porins and efflux systems can have broad substrate specificity, affecting multiple classes of antibacterial agents and leading to multiple resistance. Its effectiveness against gram-positive aerobes - Enterococcus faecalis - has been established in vitro and confirmed in clinical studies. Staphylococcus aureus (methicillin-sensitive strains), Staphylococcus epidermidis (methicillin-sensitive strains), Staphylococcus saprophyticus, Streptococcus pneumoniae (including multi-resistant strains - MDRSP), Streptococcus pyogenes; gram-negative aerobes - Enterobacter cloacae, Escherichia coli, Haemophilus influenzae, Haemophilus paraintluenzae, Klebsiella pneumoniae, Legionella pneumophila, Moraxella catarrhalis, Proteus mirabilis, Pseudomonas aeruginosa, Serratia marcescens and other microorganisms - Chlamydia pneumoniae, Mycoplasma pneumoniae. For most (>90%) strains of the following microorganisms, minimum inhibitory concentrations of levofloxacin (2 μg/ml or less) have been established in vitro, however, the effectiveness and safety of the clinical use of levofloxacin in the treatment of infections caused by these pathogens has not been established in adequate and well-controlled studies : gram-positive aerobes - Staphylococcus haemolyticus, Streptococcus (group C/F), Streptococcus (group G), Streptococcus agalactiae, Streptococcus milleri. Streptococcus viridans; gram-negative aerobes - Acinetobacter lwoffii, Acinetobacter baumannii, Bordetella pertussis, Citrobacter (diversus) koseri, Citrobacter freundii, Enterobacter aerogenes, Enterobacter sakazakii, Klebsiella oxytoca, Morganella morganii, Pantoea (Enterobacter) agglomerans, Proteus vulgaris, Providencia rettgeri, Providencia s tuartii, Pseudomonas fluorescens ; gram-positive anaerobes - Clostridium perfringens. Sensitive microorganisms: aerobic gram-positive microorganisms - Corynebacterium diphtheriae, Enterococcus spp., including Enterococcus faecalis, Listeria monocytogenes, Staphylococcus spp. (coagulase-negative methicillin-sensitive/leukotoxin-containing/moderately sensitive strains), including Staphylococcus aureus (methicillin-sensitive strains), Staphylococcus epidermidis (methicillin-sensitive strains), Streptococcus spp. groups C and G, Streptococcus agalactiae, Streptococcus pneumoniae (penicillin-sensitive/moderately sensitive/resistant strains), Streptococcus pyogenes, Streptococcus spp. viridans group (penicillin-sensitive/resistant strains); aerobic gram-negative microorganisms - Acinetobacter spp., including Acinetobacter baumannii, Acinetobacillus actinomycetecomitans, Citrobacter freundii, Eikenella corrodens, Enterobacter spp., including Enterobacter aerogenes, Enterobacter agglomerans, Enterobacter cloacae, Escherichia coli, Gardnerella vaginalis, Haemophilus ducreyi, Haemophilus in fluenzae (ampicillin-sensitive/resistant strains), Haemophilus parainfluenzae, Helicobacter pylori, Klebsiella spp., including Klebsiella oxytoca, Klebsiella pneumoniae, Moraxella catarrhalis (beta-lactamase producing and non-producing strains), Morganella morganii, Neisseria gonorrhoeae (penicillinase producing and non-producing strains) strains), Neisseria meningitidis, Pasteurella spp., including Pasteurella canis, Pasteurella dagmatis, Pasteurella multocida, Proteus vulgaris, Providencia spp., including Providencia rettgeri, Providencia stuartii, Pseudomonas spp., including Pseudomonas aeruginosa, Serratia spp. ., including Serratia marcescens, Salmonella spp.; anaerobic microorganisms - Bacteroides fragilis, Bifidobacterium spp., Clostridium perfringens, Fusobacterium spp., Peptostreptococcus spp., Propionibacterium spp., Veilonella spp.; other microorganisms - Bartonella spp., Chlamydia pneumoniae, Chlamydia psittaci, Chlamydia trachomatis, Legionella pneumophila, Legionella spp., Mycobacterium leprae, Mycobacterium tuberculosis, Mycoplasma hominis, Mycoplasma pneumoniae. Rickettsia spp., Ureaplasma urealyticum. Moderately sensitive microorganisms (MIC more than 4 mg/l): aerobic gram-positive microorganisms - Corynebacterium urealyticum, Corynebacterium xerosis, Enterococcus faecium. Staphylococcus epidermidis (methicillin-resistant strains), Staphylococcus haemolyticus (methicillin-resistant strains); aerobic gram-negative microorganisms - Burkhoideria cepacia, Campylobacter jejuni, Campylobacter coli; anaerobic microorganisms - Bacteroides thetaiotaomicron, Bacteroides vulgatus, Bacteroides ovatus, Prevotella spp., Porphyromonas spp. Resistant microorganisms (MIC more than 8 mg/ml): aerobic gram-positive microorganisms - Corynebacterium jeikeium, Staphylococcus aureus (methicillin-resistant strains), other Staphylococcus spp. (coagulase-negative methicillin-resistant strains); aerobic gram-negative microorganisms - Alcaligenes xylosoxidane; other microorganisms - Mycobacterium avium. The in vitro activity of levofloxacin is approximately 2 times higher than that of ofloxacin against representatives of Enterobacteriaceae, Pseudomonas aeruginosa and gram-positive microorganisms. In the case of using levofloxacin in the treatment of chlamydial diseases of the organs of vision, concomitant therapy is required. The degree of sensitivity of microorganisms to levofloxacin may have significant geographical differences. The maximum concentration of levofloxacin achieved using 0.5% eye drops is more than 100 times the minimum inhibitory concentration (MIC) of levofloxacin for sensitive microorganisms.
Pharmacokinetics:
After instillation into the eye, levofloxacin is well preserved in the tear film.
The concentration of levofloxacin in tear fluid after a single dose (1 drop) quickly reaches high values and is maintained at a level above the minimum inhibitory concentration for most sensitive ocular pathogens (less than or equal to 2 mcg/ml) for at least 6 hours. In studies in healthy volunteers, mean tear film concentrations of levofloxacin measured 4 and 6 hours after topical application were 17.0 mcg/mL and 6.6 mcg/mL, respectively. In five of six volunteers, levofloxacin concentrations were 2 μg/ml or higher 4 hours after instillation. In four out of six volunteers, this concentration remained 6 hours after instillation. The average concentration of levofloxacin in blood plasma 1 hour after use is from 0.86 ng/ml on the 1st day to 2.05 ng/ml. The maximum concentration of levofloxacin in plasma, equal to 2.25 ng/ml, was detected on the 4th day after two days of using the drug every 2 hours up to 8 times a day. The maximum concentrations of levofloxacin achieved on day 15 were more than 1000 times lower than those observed after oral administration of standard doses of levofloxacin.
Answers on questions
Is Levofloxacin an antibiotic or not?
It is an antibacterial and antimicrobial drug. Therefore, during the course it is necessary to take probiotics to restore intestinal microflora.
Can I take levofloxacin with alcohol or not?
Levofloxacin is incompatible with alcoholic beverages.
Is Levofloxacin an antibiotic or an antiviral?
The medication is not an antiviral drug, it is an antibiotic.