You can fight harmful rats and other rodents in different ways. Sometimes, after their destruction, the room needs disinfection, which you can do yourself - it is important to choose only the appropriate method. Behind the unpleasant odor after controlling rodent pests are hidden more serious problems that can cause a number of unpleasant diseases. Once you have cleaned the rooms, be sure to thoroughly disinfect every corner. For these purposes, you can use Medifox Super, which is proportionally diluted with water and is suitable for contact treatment of surfaces.
Product description
You can treat wall and floor surfaces, clothing, bed linen, door handles, chairs and other objects with this disinfectant. The product is suitable for disinfestation at different times of the year. It can be used to treat absorbent and non-absorbent surfaces.
Medifox Super can be used to irrigate areas where small insects accumulate and cause harm to humans. The special product is effective regardless of the type of surface being treated. The working emulsion is valid for 8 hours after its preparation, so it is necessary to start treating the room immediately.
Mode of application
Depending on which surface needs to be treated, the special product is diluted with clean boiled water. The concentration is prepared taking into account the purposes for which it will be used. During the treatment of the room, you need to remove or carefully hide dishes, food, and animals. It is required to wear gloves when carrying out disinfestation work, and it is also advisable to use other protective equipment. After all the required areas have been treated, the perimeter must be left to ventilate for at least 30 minutes. The drug has a residual acaricidal effect, so even with its single use, the area after treatment should be well ventilated.
The amount of Medifox Super required for the preparation of working emulsions:
| Insect type | Concentration (%) in the Far East | Concentration (%) by drug | Ratio (concentrate: water, ml.) for preparing n liters of working aqueous emulsion | ||
| 1 l | 5 l | 10 l | |||
| Cockroaches | 0,5 | 2,5 | 25 : 975 | 125 : 4875 | 250 : 9750 |
| 5,0 | 1,0 | 50 : 950 | 250 : 4750 | 500 : 9500 | |
| 2,0 | 10,0 | 100 : 900 | 500 : 4500 | 1000 : 9000 | |
| Bedbugs | 0,5 | 2,5 | 25 : 975 | 125 : 4875 | 250 : 9750 |
| Fleas | 0,1 | 0,5 | 5 : 995 | 25 : 4975 | 50 : 9950 |
| Ants | 0,5 | 2,5 | 25 : 975 | 125 : 4875 | 250 : 9750 |
| Rat ticks | 0,5 | 2,5 | 25 : 975 | 125 : 4875 | 250 : 9750 |
| Scabies mites | 0,2 | 1,0 | 10 : 990 | 50 : 4950 | 100 : 9900 |
| Lice | 0,1 | 0,5 | 5 : 995 | 25 : 4975 | 50 : 9950 |
| 1,0 | 0,2 | 10 : 990 | 50 : 4950 | 100 : 9900 | |
| Flies imago | 0,5 | 2,5 | 25 : 975 | 125 : 4875 | 250 : 9750 |
| 5,0 | 1,0 | 50 : 950 | 250 : 4750 | 500 : 9500 | |
| Flies larvae | 1,0 | 5,0 | 50 : 950 | 250 : 4750 | 500 : 9500 |
| Mosquito imago | 0,2 | 1,0 | 10 : 990 | 50 : 4950 | 100 : 9900 |
| Mosquito larvae | 0,01 | 0,05 | 0,5 : 999,5 | 2,5 : 4997,5 | 5 : 9995 |
Modern approaches to the diagnosis and treatment of scabies
Scabies is a contagious parasitic skin disease caused by the scabies mite Sarcoptes scabiei, accompanied by itching, worse in the evening and at night, and papular-vesicular rashes.
Currently, scabies remains one of the most common parasitic dermatoses in our country.
An increase in the number of patients with scabies usually accompanies wars, natural disasters, and social upheavals, which is caused by population migration, economic recession, and deterioration of social and living conditions.
As mentioned above, the causative agent of scabies is the scabies mite - Sarcoptes scabiei. This species belongs to the family Sarcoptidae, group Acaridiae, suborder Sarcoptiphormes, order Acariphormes. Members of the genus Sarcoptes are currently known as parasites of more than 40 species of animal hosts belonging to 17 families of 7 orders of mammals.
The morphological appearance of scabies mites of the Sarcoptidae family is extremely unique and is due to profound adaptations to intradermal parasitism. The structure of scabies, like most mites, is characterized by strict constancy of the microstructures of the exoskeleton, which is associated with their microscopic size.
The female scabies mite resembles a turtle in appearance. Its size is 0.25–0.35 mm. Adaptations for intradermal parasitism are represented by multiple setae, triangular outgrowths of the cuticle on the dorsal surface, spines on all tarsi that serve as stops when gnawing, gnawing-type chelicerae, long elastic bristles on the tarsi of the hind pairs of legs to maintain the direction of the gait only forward. Adaptations for ectoparasitism are sticky pneumatic suckers on the front legs, waxy bristles on the body and limbs, which create an extensive mechanoreceptive sphere around the tick and allow it to navigate by touch without eyes. The speed of movement of the female during the course is 0.5–2.5 mm/day, and on the surface of the skin 2–3 cm/min. Scabies mites are characterized by sexual dimorphism. The main function of males is fertilization. They are much smaller in size - 0.15–0.2 mm, have dense bristles on the body for protection from mechanical stress and suckers also on the fourth pair of legs for attachment to the female during mating. The ratio of females to males in scabies mites is 2:1.
The life cycle of the scabies mite is clearly divided into two parts: short-term cutaneous and long-term intradermal. Intradermal is represented by two topically separated periods: reproductive and metamorphic. Reproduction is carried out by the female in the itch she gnaws, where she lays eggs. The hatching larvae emerge from the passages onto the surface of the skin through holes made by the female above the site of each clutch, settle on it and penetrate into the hair follicles and under the scales of the epidermis. Here their metamorphosis (molting) occurs: through the proto- and teleonymph stage, new individuals (females and males) are formed. Females and males of the new generation come to the surface of the skin, where they mate. Daughter females migrate to the hands, wrists, feet, penetrate the skin and immediately begin to make passages and lay eggs. In rare cases, the introduction of females is possible in other areas of the skin (buttocks, axillary areas, abdomen, etc.) due to mechanical pressure. Clinically, this corresponds to scabious lymphoplasia of the skin. Only females and larvae are infective stages and participate in infection. At room temperature and relative humidity, at least 60% of females retain mobility for 1–6 days. Even at 100% humidity, females survive on average up to 3 days, larvae - up to 2 days.
Scabies mites are characterized by a strict daily rhythm of activity. During the day, the female is at rest. In the evening and in the first half of the night, she gnaws one or two egg knees at an angle to the main direction of the stroke, in each of which she lays an egg. Before laying eggs, she deepens the bottom of the passage, and makes an exit hole in the roof for the larvae. During the second half of the night, the female gnaws the passage in a straight line, feeding intensively; during the day, she stops and freezes. The daily program is carried out by all females synchronously. As a result, the itch on the patient's skin has a convoluted shape and consists of segments of the course, called the daily element of the course. The posterior part of the tract gradually peels off, and during a clinical examination of the patient, it simultaneously consists of 4–7 daily elements and has a constant length of 5–7 mm. During her life, the female travels 3–6 cm in the epidermis; the revealed daily rhythm of activity is of great practical importance. It explains the intensification of itching in the evening, the predominance of the direct route of infection through contact in bed in the evening and at night, and the effectiveness of prescribing anti-scabies at night.
Clinical picture
The clinical picture of scabies is determined by the characteristics of the pathogen and the reaction of the host body to its introduction.
The incubation period for scabies varies in length and depends on whether the skin is an adult female or a larva. In the first case it is extremely short, and in the second it is 2 weeks. Itching, as the main symptom of scabies, appears in a period that ranges from 14 days to 6 weeks during primary infection and can be extremely short, limited to a few days during reinfection. It has also been shown that reinfection, however, may be more difficult in already sensitized individuals, and the number of detectable scabies mites in such patients is often minimal [7, 9].
The typical form of scabies is characterized by the presence of itchy skin, which is most pronounced in the evening and during sleep. However, the itching can also be constant. It can be localized to individual areas of the skin or spread throughout the body, with the exception of the facial skin and scalp. An extremely important sign is the presence of itching among family or team members.
During the examination, specific rashes are revealed. The main clinical symptoms of scabies are scabies, polymorphic rashes outside the tracts, characteristic sites of rashes, as well as symptoms named after the authors Ardi (presence of pustules and purulent crusts on the elbows and in their circumference), Gorchakov (presence of bloody crusts there), Michaelis (presence of bloody crusts and impetiginous rashes in the intergluteal fold with transition to the sacrum), Sezari (detection of scabies in the form of a slight elevation on palpation).
Typical localization sites for rashes are predominantly the flexor surface of the joints (wrist and elbow), as well as the anterolateral surface of the abdomen, lower back, buttocks, and genital area, while they are absent on the upper half of the back. Scabies and rashes are well expressed in the interdigital and axillary folds, on the areola of the breast of women, in the navel area. The rashes are represented by paired papules and vesicles, scabies, eczematous pseudovesicles (pearly vesicles) on the skin of the lateral surfaces of the fingers and palms; scabious ulcers, with crusts on the surface; as well as scabious nodules.
It seems to us advisable to classify and present atypical forms of scabies
- scabies without skin lesions;
- urticarial scabies;
- scabies during corticosteroid therapy;
- nodular (with postscabiosis nodules) scabies;
- eczematized scabies;
- scabies complicated by pyoderma;
- Norwegian scabies;
- infant and childhood scabies.
The first two forms are caused primarily by allergic reactions.
Scabies without skin lesions can represent the beginning forms of the disease in people who observe standards of body hygiene, but more often it manifests itself as an allergic reaction to mite antigens during the period of the disease or after its treatment. This form of the disease is more often detected during an active examination of persons who have been in contact with a patient with scabies.
Urticarial scabies is represented by small blisters caused by sensitization to both mites and their metabolic products. They occur more often on the front of the torso, thighs, buttocks and forearms.
Scabies with local corticosteroid therapy, also called latent scabies, as a result of suppression of the immune reactions of the skin, leads to the loss of specific symptoms of scabies. The disease acquires papulosquamous, papulovesicular, and sometimes even hyperkeratotic rashes.
Nodular scabies (scabious lymphoplasia) is characterized by the appearance of itchy nodules that are red, pink or brown. Scabies can be found on the surface of new nodules. Typical localization: penis, scrotum, axillary and intergluteal folds, areola. The nodules are usually few in number. Sometimes they are the only diagnostic sign of scabies [2, 4].
Eczematized scabies usually occurs in people with an allergic predisposition. Foci of lichenification may appear at the sites of scratching. However, eczematous lesions usually come to the fore and the diagnosis of scabies may not always be suspected. Rashes appear on the hands, armpits, legs, and hands. In advanced cases, the rash can become disseminated, leading to the development of erythroderma.
In persons with reduced body resistance, eczematized lesions at the sites of scratching may be accompanied by a secondary bacterial infection in the form of impetigo or ecthyma; staphylococcal folliculitis, boils and abscesses may occur.
Norwegian scabies (crustic, crusted) in the initial stages is presented as ordinary scabies or disguised as atopic dermatitis, psoriasis, seborrheic dermatitis. Characterized by keratinization, the formation of scales or thick crusts. In case of severe immunodeficiency, the process can be generalized; in case of neurological diseases, it can manifest itself in a limited area of sensory impairment.
Infant and childhood scabies are characterized by rashes resembling urticaria or infant pruritus in the form of a large number of scratched and crusty blisters with a predominant localization in the perineum on the scrotum, in the axillary folds. Characteristic scabies can be found on the soles.
Diagnostics
Diagnosis of scabies, in addition to clinical data, is based on microscopic confirmation of the diagnosis. However, this procedure requires considerable skill, an experienced microbiologist, and is not feasible in some clinical forms. The minimal clinical manifestations of scabies also make it difficult to obtain sufficient biological material for research. The technique has advantages in specialized institutions. There are several methods for laboratory diagnosis of scabies: removing the mite with a needle, the method of thin sections, scrapings, alkaline skin preparation.
Treatment
For the treatment of scabies, various preparations of sulfur, benzyl benzoate, Peruvian balsam, etc. were previously proposed. In recent years, new drugs have begun to be used, such as Spregal, crotamiton, lindane, malathion, permethrin, Prioderm, Tetmosol, thiobendazole, prescribed in the form of ointments, creams, solutions , shampoos, emulsions and aerosols. The main requirements for anti-scabies are the speed and reliability of the therapeutic effect, the absence of irritating effects on the skin and contraindications for use, ease of preparation and use, stability during long-term storage, availability for mass use, hygiene and low cost [8, 9] . In addition, various forms of scabies, such as postscabiosis, eczematized or urticarial, require the addition of pathogenetic therapy.
General principles: rubbing anti-scab preparations into the skin, especially carefully into the mite’s favorite localization areas. After each forced hand washing, it is necessary to re-treat them with an anti-scabies agent. In the presence of complications (primarily pustular skin lesions), lubrication rather than rubbing is performed. Before starting treatment, it is advisable to take a hot shower or bath, using a washcloth and soap to mechanically remove mites from the surface of the skin, as well as to loosen the surface layer of the epidermis, which simplifies the penetration of antiscabiotic drugs. In the presence of secondary pyoderma, water procedures are contraindicated. Regardless of the method of therapy, the entire skin is treated with an anti-scabies drug. Avoid contact of the drug with the eyes and mucous membranes. The dosage of the acaricidal agent should not be too large, and other skin preparations should not be used at the same time. The patient should be given clear and precise recommendations.
Medicines used to treat scabies:
1. Preparations containing sulfur
It has long been used to treat scabies. Examples of such products are: 10–33% sulfur ointment, 10% sulfur vaseline, Demyanovich’s method, Wilkinson ointment, 5–10% polysulfide liniment, Sulfodecortem, Helmerica ointment, Milian paste.
Currently, the use of such drugs is limited, since the therapeutic effect of some of them is questioned. In addition, they have a number of undesirable properties: medications have an unpleasant odor, stain clothes and underwear, and have an adverse effect on the skin (dermatitis, eczematization).
Sulfur ointment - a 33% concentration is used to treat adults, and 10–15% to treat children. The ointment is rubbed daily, preferably at night, over the entire skin for 5–7 days. On the 6th or 8th day, the patient washes, changes his underwear and bed linen.
Sulfodecortem is a drug containing 10% precipitated sulfur and hydrocortisone acetate. Apply after washing for 5–7 days. Repeated washing and change of linen are carried out after the end of the course of treatment.
The Demyanovich method was widely used in our country. It is based on the acaricidal effect of sulfur and sulfur dioxide, released during the interaction of sodium thiosulfate and hydrochloric acid.
A 60% solution of sodium thiosulfate (solution No. 1) and a 6% solution of concentrated hydrochloric acid (solution No. 2) are successively rubbed into the skin of the torso and limbs; for children, the concentration is 40% (No. 1) and 4% (No. 2). Apply solutions for 3 days. Before use, solution No. 1 is slightly warmed up and rubbed into the skin with your hands in a certain sequence: starting with simultaneous rubbing of the drug into the skin of both hands, then the limbs, then the skin of the torso (chest, abdomen, back, gluteal region, genitals) and finally skin of the lower extremities to the toes and soles. Rubbing into each area lasts 2 minutes, the entire procedure should take at least 10 minutes. The second rubbing is carried out with the same solution in the same way as the first. After a 10-minute break, they begin to rub in solution No. 2 in the same sequence, 1 minute for each area 3-4 times with 5-minute breaks for drying. At the end of rubbing and after the skin has dried, the patient puts on clean underwear and does not wash for 3 days, but rubs it into the hands again after each wash. After 3 days, the patient washes and changes his underwear again.
Solution No. 1 Rp.: Natrii thiosulfatis 120.0 Aq. Destil. Rub 80.0 M.DS into the skin Solution No. 2 Rp.: Ac.hidrochlorici puri 12.0 Aq. Destil. 200.0 MDS rub into skin
Today, the use of this drug is limited due to the ever-decreasing number of pharmacies that have production departments. In addition, this method is very labor-intensive and is accompanied by the release of an unpleasant odor of sulfur and sulfur dioxide.
2. Peruvian balsam
This balm is made from an extract of one of the plants of the legume family (Miroxylon Periferum). One of the active ingredients is cinnamein, which contains benzyl benzoate, which apparently gives the drug an antiparasitic effect. Side effects include local allergic reactions and eczema. When applying the drug to a large surface area of the body, resorptive effects with symptoms of renal intoxication are possible.
3. Benzyl benzoate preparations
Benzyl benzoate. It is used in the form of a 20% water-soap suspension; children under 3 years of age are prescribed a 10% suspension. The suspension is rubbed into the skin of the entire body, except the head, and for children under 3 years old and into the skin of the face. Rubbing is carried out in a certain sequence (see Demyanovich's method). The course requires two treatments with an interval of 3 days to affect the mobile forms of the mite and larvae. Linen is changed twice after each treatment. The cost of the drug is 100 ml for treatment and 200 ml for the course. Treatment with benzyl benzoate is contraindicated in pregnant women and during lactation. The freshly prepared drug is most effective. When stored, benzyl benzoate loses its effectiveness, which explains the failures in its use.
It is also possible to use benzyl benzoate in the form of a 10–20% ointment. In this case, the consumption of the drug is 30–40 g per application and 60–80 g per course.
Askabiol is a drug containing equal amounts of benzyl benzoate, solid soap and ethyl alcohol.
Benzoseptol is a preparation containing equal amounts of benzyl benzoate, mild soap and isopropyl alcohol.
Novoscabiol is a drug containing benzyl benzoate - 30.0, methyl ester - 1.0, paraffin oil - 69.0.
Nbin is a preparation containing benzyl benzoate - 68 parts, Tween-80-14 parts, anesthesin - 12 parts, DDT (insecticide - trichloromethyldi(p-chlorophenyl)methane)) - 6 parts.
4. Lindane or gammabenzenehexachlorane
This organochlorine insecticide is used in the form of a 1% lotion, which is applied once to the entire surface of the body and left for 6 hours, then washed off. In hot climates, it is possible to use lindane in powder form. The drug can also be used in the form of cream, shampoo and ointment. The drug is not used during pregnancy and lactation, in infancy, as well as in patients with eczema and atopic dermatitis, as it can cause exacerbation (Latin exacerbo - irritate, aggravate) the process.
5. Crotamiton (Yurax)
Apply as 10% cream, lotion or ointment. The active ingredient crotamiton, in addition to its acaricidal effect, has the ability to relieve itching, which is very important for patients with scabies. Apply the drug after washing 2 times a day at daily intervals or four times every 12 hours for 2 days. The drug is interesting because it does not cause side effects and can be used to treat children, pregnant women and patients with allergic dermatoses. At the same time, its effectiveness is not absolute.
6. Permethrin preparations
The mechanism of action is based on disruption of the permeability of membranes of insect nerve cells to cations, which has an acaricidal effect. Affects adult larvae and eggs.
Medifox is a 5% concentrate of the synthetic pyrethroid permethrin in alcohol and castor oil. Available in ampoules of 2 ml, glass bottles of 24 ml, polymer containers from 0.1 to 5.0 l. It is applied externally in the form of a freshly prepared 0.4% emulsion. To do this, 8 ml of a factory-packaged 5% solution should be added to 100 ml of water. Rubbing is done once a day at night for 3 days. Shelf life of the working emulsion is 8 hours.
Nittifor is a solution for external use in a 60 ml bottle, containing permethrin and cytylperidinium bromide.
Rubbing the drug is carried out once a day at night for 3 days. On the fourth day, the remnants of the drug are washed off with cold water and bed and underwear are changed.
7. Pyrethrin group
Aerosol Spregal (esdepalletrin) is a synthetic pyrethrin (neurotoxin for small arthropod parasites), enhanced with piperonyl butoxide (an enzyme inhibitor that helps remove pyrethrin from the parasite), used as the active principle of the aerosol anti-scabies Spregal. An excipient (auxiliary substance) specially developed for it allows the solution to be applied to the entire surface of the skin and ensures the penetration of the active substances into the skin and scabies tracts with the subsequent destruction of the female mite and her eggs.
However, when using Spregal, some caution is sometimes required, for example, in the presence of a large number of excoriations, since in this case there may be a slight increase in skin itching and the appearance of dermatitis in patients who have an individual intolerance to one of the components.
The question of choosing a drug for the treatment of scabies is the main one for the practitioner.
The choice of therapeutic method for atypical forms of scabies is based on modern knowledge of its immunopathogenesis. Adding differentiated pathogenetic therapy to basic etiotropic therapy increases the effectiveness of treatment of these forms of scabies that are difficult to treat.
A special problem in the treatment of scabies is severe itching that does not disappear after treatment. The reasons for this phenomenon can be varied:
- allergy to the used medicinal drug, especially in suspicious patients who use it too often;
- a state of physiological hypersensitivity, which manifests itself in the fact that severe itching does not disappear within 8–10 days after treatment;
- incorrect diagnosis;
- improper treatment or secondary invasion;
- psychiatric problems: acarophobia (fear of scabies) or mania for parasitosis.
Thus, persistent itching can be due to various reasons and requires medical supervision; the patient should not self-medicate.
Prevention of scabies
The most important link in the prevention of scabies is early diagnosis and active identification of patients. They are carried out during preventive examinations of designated groups of patients. It is very important to identify foci of scabies and work to eliminate them. Identification and simultaneous treatment of all contact persons. Timely and thorough disinfection of clothing, underwear and bed linen. Control of cure is carried out 3 days after the end of treatment, and then every 10 days for 1.5 months. Linen is boiled, dresses and other clothes (if it is impossible to process in a disinfection chamber) are thoroughly ironed or ventilated in the air for 5 days, and in the cold for 1 day. Conducts wet cleaning with a 5% chloramine solution. Upholstered furniture is treated with the same solution. For the purpose of disinfecting an epidemiological outbreak, an aerosol agent A-PAR is recommended, which allows for high-quality disinfection at home.
A-PAR is an anti-itch preparation, the excipient of which, safe for humans, allows you to disinfect clothing and bedding without leaving stains on clothing and, in addition, is intended for treating furniture, hard surfaces, door handles, children's toys, and shoes.
Final disinfection is carried out after the end of treatment, in children's groups twice: after identifying a patient in the group and at the end of treatment. In large, long-term, intensively operating teams, it is advisable to carry out final treatment of premises using the preparations Medifox (0.2% aqueous emulsion), Medifox-super (0.2% aqueous emulsion), Tsifox (0.5% aqueous emulsion).
Literature
- Gebra F. Guide to the study of skin diseases: trans. with him. Ed. A. A. Polotebny. St. Petersburg: O. I. Bakst, 1876. T. 1.
- Daria J. Fundamentals of dermatology: trans. from French Ed. A. A. Sakhnovskaya. M.–L.: State. publishing house, 1930.
- Demyanovich M. P. Scabies. M.: Medgiz, 1947.
- Korotky N. G. Modern external therapy of dermatoses. Tver: Provincial Medicine, 2001.
- Savchak V., Galnikina S. Practical dermatology. K.: Ukrmedkniga, 1998. pp. 14–22.
- Samtsov A.V. Contagious dermatoses and venereal diseases (modern methods of treatment). St. Petersburg: Special literature, 1997. pp. 30–33.
- Sergeev Yu. V. Modern clinical and immunological features of scabies and new approaches to its diagnosis and therapy // Immunopathology, allergology, infectology. 2000, No. 4, p. 102–107.
- Sokolova T.V., Fedorovskaya R.F., Lange A.B. Scabies. M.: Medicine, 1989.
- Sokolova T.V., Lopatina Yu.V. Parasitic dermatoses: scabies and mite-borne dermatitis. M.: Binom, 2003.
- Fedorov S. M., Selissky T. D. Scabies. In the book: Skin diseases. M.: Medicine, 1998. pp. 164–172.
- Belyab P., Jean-Pastor M. J. Scabies. SCAT. 1996, Marseille. R. 22–26.
- Ackerman B. Histopathology of human scabies. Ed. Lippincott Compagny, 1997, Philadelphia. R. 88–95.
- Saurat JA Risques systemiques des medicaments topiques chez l'enfant // Sem. Hop. Paris. 1982, 58, 26–27, 1643–1649.
- Shakter B. Treatment of scabies and pediculosis with linden preparation: an evalution // J. Am. Acad. Dermatol. 1981, 5, 517–527.
- Van Neste D. Immuno — allergological aspects of scabies: a comparative study of spontaneous blastogenesis in the dermal infiltrates of common and hyperkeratotic scabies? Allergic contact dermatitis and irritant dermatitis // Arh. Dermatol. Res. 1982, 274, 159–167.
I. V. Verkhoglyad, Doctor of Medical Sciences, Associate Professor I. Ya. Pinson, Doctor of Medical Sciences
GBOU DPO RMAPO Ministry of Health and Social Development of Russia, Moscow
Contact information for authors for correspondence
Safety
The insecticide contains several components of different nature, so when using it you should definitely follow safety precautions. The main active ingredients are insecticide derivatives that allow you to fight different types of parasites. To avoid negative effects, you should adhere to the correct procedure for using the disinfectant and follow the dosage. The toxic composition, when used correctly, does not cause side effects, but it is recommended to treat surrounding objects with it without the presence of people. Avoid contact with mucous membranes and the digestive tract.
This product requires special preparation when used. You must carefully read the instructions for use and follow safety precautions.
Currently, four drugs are used to treat scabies in the Russian Federation and CIS countries: benzyl benzoate emulsion/ointment, Medifox, Spregal and sulfur ointment. When choosing a drug to treat patients with scabies, the doctor must take into account the positive aspects and disadvantages of each remedy.
Benzyl benzoate.
Approved for use in children over 3 years of age due to the possibility of developing Gasping syndrome (sudden death syndrome), , , . Not recommended for use in pregnant women. Patients note a burning sensation when the drug is first applied. It is not the drug of choice for the treatment of complicated scabies, especially in hot climates. Relatively high cost of emulsion.
Sulfuric ointment.
A 5% concentration is allowed from 5 years of age. Not for use in pregnant women. Often contributes to the development of dermatitis, especially when using a 33% concentration. It has an unpleasant odor and stains laundry. The course of treatment is long (5-7 days). Poorly tolerated in the hot season.
Spregal
. It is allowed to be used in children from the neonatal period. May be used with caution in pregnant women. It is the drug of choice for the treatment of complicated scabies, including in hot climates. However, the high price of the drug limits its use in large families with low incomes.
Medifox.
It is allowed to be used in children starting from one year of age. Can be used with caution in pregnant women. It is the drug of choice for the treatment of complicated scabies, including in hot climates. The main disadvantage is the short shelf life of the working solution (8 hours). However, in conditions of large irradiating foci, the prepared solution can be used both for the treatment of patients and for the preventive treatment of contact persons. The cost of the drug allows it to be used even in economically disadvantaged families.
The active ingredient in Medifox is permethrin. The mechanism of its action is based on disruption of the microcirculation of sodium channels in ticks, which leads to a delay in repolarization, causing paralysis and death of the parasite at all stages of development. Permethrin belongs to the group of low-toxic scabicides. It is widely used both in our country and abroad. According to Russian specialists, the effectiveness of treatment with Medifox reaches 100%, , . Considering that the drug does not have a 100% ovicidal effect, a treatment regimen has been developed taking into account the effect on females and eggs of scabies mites. It is recommended to rub the drug on the 1st and 4th days of the course. Medifox is widely used for the treatment of scabies in the Armed Forces of the Russian Federation.
It should be noted that abroad permethrin is used in the form of a cream of 5% concentration. Permethrin cream is often used to treat scabies in the US, UK and Australia. In the first two countries, 5% permethrin cream is included in national protocols for the treatment of patients with scabies as a first-line drug. More often, permethrin is used once at night, , , , , , , , , , less often - twice with an interval of one week, , , , . The effectiveness of therapy ranges from 89 to 98%, , ,, , . Exposure of 5% permethrin cream to the skin is usually 8-14 hours. It is then washed off with soap and water.
A comparative analysis of the effectiveness of four scabicides approved for use in the Russian Federation in terms of the dynamics of clinical manifestations and the effect on the pathogen in a hospital setting, where patients with complicated scabies were mainly hospitalized, showed that recovery when using 0.4% Medifox emulsion was 80.7%. American dermatologists believe that 5% permethrin cream is superior in effectiveness and safety to lindane and crotamiton, and ivermectin. It has been established that the toxicity of 5% permethrin cream is 40-400 times less than 1% lindane lotion. In 1996, side effects from permethrin use were only 2.5 per 1,000 scabies patients treated with the drug.
In the United States, permethrin has no age restrictions. The American Academy of Pediatrics considers permethrin 5% cream to be a safe and effective scabicide. It can be used to treat even infants. In Canada it is used in children older than 2 months. It is applied overnight (from 8 to 12 hours), then washed off and the course is repeated a week later. In infants, the entire skin, including the head, is treated.
An interesting study examined the effectiveness and safety of 4% permethrin cream in 196 pregnant women. The majority of women were in the second (42.2%) and third trimesters (46.9%) of pregnancy and only 10.9% were in the first. It has been proven that 4% permethrin, even when rubbed in twice, does not cause intrauterine abnormalities in fetal development and can be recommended for treatment during pregnancy.
In the literature of the last two decades, publications have appeared on the formation of resistance of scabies mites to permethrin, , , , . However, all studies involved people living in settlements where scabies persisted, for example, in Australia and El Salvador. Permethrin has been used for the treatment of patients and prophylactic treatment of contact persons for several years. There are no officially confirmed data on tick resistance to permethrin in vivo in the literature.
Purpose
This study was a comparative study of the effectiveness of treating scabies with 0.4% and 0.8% Medifox emulsion.
Materials and methods of research.
The work was carried out in the Republic of Tajikistan on the basis of city clinical hospital No. 1 in 2011-2012. 42 family centers of scabies, totaling 252 people, were examined. The diagnosis of scabies was confirmed in the laboratory by scraping the epidermis using 40% lactic acid and by dermatoscopy. The incidence of scabies in foci was 75.4%. 194 patients with scabies were treated with Medifox.
The control group (CG) consisted of 92 patients who received treatment with a 0.4% Medifox emulsion. In the experimental group (OG), there were 102 patients, and the drug concentration was 2 times higher (0.8%). Rubbing in the freshly prepared emulsion was carried out in the evening on days 1 and 4 of the course. To treat complications of scabies, days 2, 3, 5 and subsequent days were used until the clinical manifestations completely resolved. Treatment of secondary superficial pyoderma was carried out with topical antibacterial agents (fucorcin, potassium permanganate, canadex, celestoderm with garamycin). To treat allergic dermatitis, as a complication of scabies, creams/ointments with topical corticosteroids (celestoderm, dermovate) were used. Creams/ointments with topical corticosteroids (celestoderm, sinaflan) were rubbed into lenticular papules with scabious lymphoplasia of the skin (SLK) twice a day. Treatment of scabies complicated by dermatitis, pyoderma, as well as when they were combined with SLC in the CG and OG was carried out in the same way. The effectiveness of treatment was assessed after 5 days (at the end of the course of therapy) and after 2 weeks (during follow-up). In the presence of LSK, the observation period was extended until the rashes completely resolved. Efficacy was assessed according to the following criteria: recovery, significant improvement, reinvasion. No drug complications were recorded during therapy.
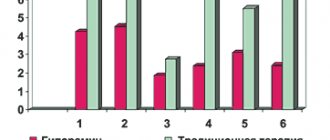
The distribution of patients with scabies in the CG and MG by gender and age is presented in Fig. 1 and 2.
Data in Fig. 1 and 2 indicate that the distribution of patients by gender and age in the CG and MG was representative.
An analysis of numerous literary sources shows that when assessing the effectiveness of treatment for scabies, there is no differentiated approach to the duration of resolution of specific clinical manifestations of the disease and its complications, which regress much later. In this case, the effectiveness of a particular drug is assessed based on the dynamics of clinical manifestations without taking into account the effect on the pathogen. A distinctive feature of this study was a differentiated approach to assessing the rate of resolution of clinical manifestations of scabies (disappearance of scabies ducts, vesicles and follicular papules), its complications and LS. If after a course of specific therapy the patient still had clinical manifestations of scabies, then they were given an additional single application of 0.8% Medifox emulsion. To prevent possible reinvasion in family foci of scabies, all healthy family members (81 people) received 100% preventive treatment with 0.8% Medifox. No cases of illness among contact persons were registered in these cases.
Results of our own research.
The distribution of patients with scabies in the CG and OG, taking into account the clinical form of the disease, is presented in Table. 1.
Table 1
Distribution of patients with scabies treated with Medifox, taking into account the clinical type of scabies
| Clinical type of scabies | Number of patients | |||
| KG (0.4%) N=92 | OG (0.8%) N=102 | |||
| Abs. | % | Abs. | % | |
| Typical scabies without complications and scabies | 33 | 35,9 | 42 | 41,2 |
| Scabies in combination with SLK | 30 | 21,7 | 28 | 27,5 |
| Scabies complicated by secondary pyoderma in combination with LSK | 19 | 20,6 | 22 | 21,5 |
| Scabies complicated by allergic dermatitis, secondary pyoderma in combination with LSK | 10 | 10,9 | 10 | 9,8 |
| TOTAL | 92 | 100 | 102 | 100 |
In the CG and OG, patients with typical scabies without complications and LS were predominant. In both groups they were recorded almost equally often (35.9% and 41.2%) (p>0.05). Scabies in combination with LSK was observed in 21.7% and 27.5% of patients, respectively (p>0.05). A fifth of the sample from the CG (20.6%) and OG (21.5%) consisted of patients with scabies complicated by secondary pyoderma in the presence of LS (p>0.05). Scabies complicated by allergic dermatitis was recorded in both groups equally often (10.9% and 9.8%), but always in combination with secondary pyoderma and LS. In other words, the distribution of patients taking into account the clinical form of scabies in the CG and OG was also representative.
A comparative assessment of the effectiveness of 0.4% and 0.8% Medifox emulsion was carried out for the entire sample and for the treatment of each type of scabies noted in Table 1. Data in Fig. 3 indicate that recovery of patients with typical scabies without complications and LSK, when using a 0.8% concentration of Medifox after 2 weeks, was achieved significantly 1.3 times more often than with a 0.4% concentration of the drug (95.2% versus 75 .7%) (p<0.05). It should be borne in mind that the effectiveness of a scabicide is considered good if, after a course of specific therapy according to the chosen regimen, recovery occurs in 80% of patients or more. In the CG this figure was slightly lower (75.7%). Reinvasion was observed in 1 (2.4%) patient with OG and 2 (6.1%) patients with CG. The sources of reinfestation were family members infected with scabies who were absent from the outbreaks during the period of treatment of patients and preventive treatment of contact persons. The data obtained clearly demonstrate the higher effectiveness of 0.8% medifox emulsion in the treatment of typical scabies, which predominated in both the CG and OG.
There were 30 patients with typical manifestations of scabies in combination with scabies in the control group and 28 in the group. It is important to note that after 2 weeks there were significant differences in the resolution of typical clinical manifestations of scabies (initial variants of scabies burrows, follicular papules on the trunk and non-inflammatory vesicles on the hands and feet) was not detected when using different concentrations of Medifox (p>0.05) (Fig. 4). Recovery of 83.3% (CG) and 96.4% (OG) of patients indicates the effectiveness of the drug. At the same time, it was noted that when using a 0.8% concentration of Medifox, typical manifestations of scabies disappeared after 5 days in a larger number of patients (by 13.1%). The itching that accompanies SLS was the cause of the appearance of fresh scratches and small papules, which is often regarded by dermatologists as the persistence of typical scabies.
There were 41 patients with typical scabies complicated by superficial pyoderma in combination with LSK, including 19 in the CG and 22 in the OG. It was found that when using a higher concentration of Medifox (0.8%), the percentage of resolution of typical clinical manifestations of scabies was 1 .3 higher (90.9% vs. 68.4%) (p<0.05). This is quite natural, because secondary pyoderma is often associated with scabies. In this case, staphylococcal impetigo appears on the hands, wrists and feet in place of scabies, and in place of follicular papules - ostiofolliculitis and folliculitis. Opening of pustules during itching is accompanied by the formation of purulent crusts, limiting the access of the drug to the pathogen. It is well known that in the presence of pyoderma, the itching is less intense. T.V. Sokolova (1989) experimentally proved that in passages with pustules, mites are often absent and, therefore, the production of allergens is sharply reduced. Due to this, the intensity of itching is also reduced in the area of the LM, which is essentially a marker of the immunoallergic process in the patient’s body.
Scabies complicated by allergic dermatitis, secondary pyoderma in combination with LSK was registered in 20 patients, 10 in the CG and MG. In this case, the rate of resolution of typical manifestations of the disease did not significantly depend on the concentration of the drug (p>0.05). With such a clinical picture of the disease, it was impossible to distinguish a specific process from a nonspecific one. The recovery rate in the control group was 80%, in the experimental group – 90%, i.e. only 10% higher (p>0.05) (Fig. 6). However, it should be taken into account that the sample of patients in these groups was minimal and, perhaps, therefore no significant differences were identified.
Generalized data on the rate of resolution of typical manifestations of scabies in all its clinical variants for patients with CG (92) and OG (102) are presented in Fig. 7. The effectiveness of treatment when using 0.8% medifox emulsion was 17.4% higher than 0.4% (94.1% versus 77.2%). At the same time, a differentiated approach to assessing the resolution of typical manifestations of scabies showed that a 0.8% concentration of Medifox was 1.3 times more effective in the treatment of patients with typical scabies without complications and LSK, as well as with typical scabies complicated by secondary pyoderma in combination with SLC. These patients made up 2/3 (116 people) of the sample. The results obtained clearly indicate that the effectiveness of treatment directly depends on the clinical form of the disease.
The dynamics of resolution of superficial pyoderma in patients with scabies was monitored (Fig. 8). In 2/3 (67.2%) of cases, superficial pyoderma (single ostiofolliculitis, impetigo) resolved after 5 days. In a third (32.8%) of cases, pyoderma (folliculitis, multiple impetigo, tourniol) resolved by the end of the second week.
The dynamics of resolution of SLK were monitored in 194 patients treated with 0.4% and 0.8% Medifox emulsion (Fig. 9). After 5 days, SLK regressed in 15.1% of patients, after 2 weeks – in another 22.7%, after 3 weeks – in another 27.7%, after a month – in another 31.1%. Thus, in 96.6% of cases, LSK resolved within a month.
No side effects or drug complications were registered.
Discussion of the results obtained.
Evaluation of the effectiveness of scabies treatment should be carried out taking into account the clinical form of the disease (typical, complicated by pyoderma, dermatitis, in combination with LS), which allows obtaining reliable information. Using the example of 0.4% and 0.8% concentrations of Medifox, it was shown that in the whole sample, when using twice the concentration of the drug, there were no significant differences (94.6% versus 77.2%, p>0.05). They were identified taking into account the clinical form of the disease for patients with typical scabies, as well as when it is combined with scabies against the background of complications of secondary pyoderma. This group of patients made up 2/3 of the sample. An increase in the concentration of Medifox led to the recovery of a significantly larger number of patients: 90.9% versus 68.4% (p<0.05), and LSK resolved in 96.6% of patients within a month. A single treatment of healthy family members with a 0.8% Medifox emulsion prevented intrafamilial reinvasion and the possibility of a “ping-pong” infection. At the same time, an increase in the effectiveness of treating scabies with a 2-fold increase in the concentration of Medifox indicates the absence of resistance of the scabies mite to this scabicide. A promising direction is the development by domestic enterprises of stable dosage forms of Medifox (gel, cream) with a higher concentration of the drug (2-5%).
Persistence of SLC is often regarded by doctors as ineffective treatment of scabies, although there is no live pathogen in scrapings of the epidermis. However, laboratory confirmation of the effectiveness of therapy is not used in medical institutions. We have shown that in the whole group, LSK resolved in 96.6% of patients within a month.
Thus, assessing the effectiveness of scabies treatment with one or another scabicide without taking into account the clinical form of the disease (typical, complicated by pyoderma, dermatitis, in combination with LSK) does not allow obtaining reliable results.