Since the problem of bone fragility is predominantly female (men's bones are usually stronger), the main consumers of calcium and vitamin D products are women. And now it turns out that while strengthening the bones, they harm their blood vessels. American scientists from West Virginia University came to this conclusion. They conducted a large study in which they assessed how different vitamins, macro- and microelements affect health. Calcium and Vitamin D were of concern to them.
Article on the topic Calcium: absorb and not lose
Smoke is not without fire
What can you say about this? There is no smoke without fire. Back in 2008, a study by Australian scientists was published in the influential British Medical Journal (BMJ). They found that in women who took one gram of calcium citrate daily to prevent osteoporosis for many years, the risk of heart attacks doubled.
In 2010, the same journal published a meta-analysis (combining a number of studies and re-evaluating them), which assessed the use of calcium supplements (without vitamin D) used to prevent osteoporosis. As a result, it turned out that calcium increases the likelihood of developing myocardial infarction by 31%. At the same time, it was noted that the risk of strokes was still increasing, but not statistically significant.
Scientists then stated that the indications for the use of calcium supplements to prevent osteoporosis should be reconsidered. Moreover, many experts then began to speak out not only against drugs with calcium, but also against complex products containing vitamin D. Although, strictly speaking, such drugs were not included in this meta-analysis. But they had a reason to say so. And that's why.
Article on the topic
Test yourself. Are you getting enough calcium?
Description of the drug
Calcium citrate with vitamin D3 is a dietary supplement from the American pharmaceutical company Solgar, a well-known manufacturer of highly effective drugs of natural origin. Available in the form of white tablets weighing 1540 mg. You can buy the drug in a dark glass jar, the package contains 60 pieces.
The main active ingredients are:
- calcium in the form of citrate in the amount of 250 mg;
- vitamin D3 in the amount of 150 IU.
Additionally, each tablet contains magnesium salt of stearic acid, glycerin, titanium and silicon dioxides, microcrystalline cellulose, vegetable cellulose and croscarmellose.
When is calcium bad for you?
Strokes and heart attacks are associated with excess calcium in the blood. Firstly, when there is a lot of it, it increases blood clotting, and this can lead to the formation of blood clots. Blood clots are the cause of heart attack and ischemic stroke. They block blood flow in the vessels supplying the heart or brain. In the first case, a heart attack occurs, in the second, a stroke.
But there is a second mechanism for the negative effect of calcium on blood vessels. Its excess can be deposited on the inner wall of the arteries, making them stiffer. Moreover, when calcium is fixed on cholesterol plaques, blood clots form on them more easily. In addition, calcium and plaque can erode the artery wall, leading to an aneurysm or even rupture. Ruptures of an aortic aneurysm are usually associated with destruction of its wall, in which calcium deposits play a major role. And this leads to sudden death. By the way, the frequency of such deaths in the 2010 study was also increased, but not statistically significant.
Where to get calcium from if dairy products are poorly digested? More details
Why vitamin D is also dangerous
Vitamin D can also play a significant role in this. It increases the absorption of calcium from the digestive tract, and thereby ensures that its concentration in the blood will be higher. And this means that it enhances all the effects of the drug described above.
Question answer
Which vitamins are compatible with each other and which are not?
The negative role of vitamin D was confirmed a year later. In 2011, again in the same British Medical Journal, an article was published describing how two types of drugs (with calcium alone and with calcium and vitamin D in combination) increase the risk of cardiovascular diseases, and especially myocardial infarction.
That is, the current study of an increase in strokes in those who took calcium and vitamin D at the same time echoes scientific papers published in 2010 and 2011. But that's not all.
The role of diet in preventing osteoporosis
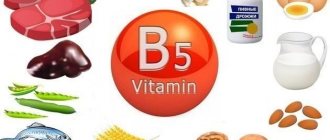
Because osteoporosis usually progresses to a clinically advanced stage before its effects become apparent, preventing bone loss is the single best way to avoid the possibility of fractures and resulting disability. Although increasing calcium in the diet is one of the strategies most often proposed, many studies have failed to show a clear relationship between dietary absorption of this mineral and bone density. Consumption of calcium and vitamin D-rich foods is likely more important during the bone-growing years before peak mass is reached rather than later in adulthood.
Dairy products contain more than 70% of the calcium in the diet of the “average” resident of our country. The calcium found in these foods is quickly absorbed because these foods contain lactose and some are fortified with vitamin D.
Vegetarians who avoid animal foods can get calcium from soy milk, tofu (soy curd) processed with calcium sulfate, grains (especially unrefined or slightly refined grains), some green leafy vegetables (cabbage, turnips), beans and nuts. Some types of currently popular mineral drinks and tap water also contain calcium, the amount of calcium varies depending on the source.
Supplement Efficacy
Due to widespread and questionable advertising linking dietary calcium to osteoporosis, this mineral has been added to many products, including orange juice, soda, and bread products.
Calcium supplements have also become popular, but their value as a source of calcium remains controversial. Supplements vary in absorption capacity, and many people take them incorrectly. For example, until recently, calcium supplements came in the form of large, difficult-to-take pills. Supplement manufacturers have reduced the size of the pills to make them easier to swallow, but they may have compressed the pills so much that they do not dissolve in the stomach and pass intact through the gastrointestinal tract.
Calcium supplements vary in the percentage of the mineral in each dose and their effect on the body. Among the most commonly used compounds are calcium carbonate (Kalmagin, Calcium D3 Nycomed, etc.) and calcium citrate (Citrical, etc.). Calcium carbonate contains up to 40% pure calcium. It reacts with hydrochloric acid in the stomach to form calcium chloride, a highly soluble and available compound.
Undesirable effects of large amounts of calcium carbonate include flatulence, nausea and constipation. Excessive use of supplements may also cause excess hydrochloric acid due to stimulation of gastric secretion; The possibility of developing kidney stones has also been reported. Calcium carbonate may reduce the absorption of medications such as aspirin, tetracycline, atenolol, and ferrous sulfate if the supplement and these medications are taken together. Antacids containing both calcium carbonate and aluminum actually block calcium absorption.
Calcium citrate contains less calcium, approximately 24%. This compound does not require hydrochloric acid to dissolve, making it more suitable for those who are deficient in this component of gastric juice. This condition, known as achlorhydria, is quite common in old age.
In addition to the evidence regarding the potential of calcium supplements to cause gastrointestinal problems, there is other evidence that casts doubt on their value. Calcium supplements alone have little beneficial effect on postmenopausal bone mineral loss. They may slow compact bone loss but are not very effective in preventing trabecular bone loss.
Additionally, medications that also contain vitamin D may cause toxic accumulation of this fat-soluble vitamin if taken in excess amounts. Bone meal and dolomite contain calcium and are relatively inexpensive, but they also contain toxins such as lead and should be avoided.
Typical mistakes in the diet of patients with osteoporosis:
- insufficient calcium in the diet;
- excessive amounts of dietary fiber, phytic and oxalic acid, which impair the absorption of calcium;
- protein deficiency in the diet, leading to a negative nitrogen balance and a decrease in reparative processes;
- too much protein in the diet, which contributes to increased excretion of calcium in the urine (for every 50 g of protein in excess of the norm, 60 mg of calcium is lost in the urine);
- excess carbohydrates in the diet, which also leads to increased loss of calcium in the urine;
- excess phosphorus in the diet, which impairs calcium absorption;
- abuse of alcohol and drinks with a high caffeine content (coffee, strong tea, cola, chocolate), which increases the loss of calcium in urine and feces;
- too much sodium, leading to loss of calcium in the urine;
- excessive (less often - insufficient) energy value of the diet;
- deficiency of vitamin D in the diet and insufficient insolation necessary for endogenous synthesis of the vitamin;
- lack of fat in the diet, which leads to impaired absorption of all fat-soluble vitamins, including vitamin D;
- underestimation of the role of dietary supplements and preparations containing calcium and vitamin D for the prevention and treatment of osteoporosis.
Additional Arguments
Over the years, there have been several studies confirming the negative effects of calcium and vitamin D. For example, in 2016, two studies were published at once: one tried to rehabilitate calcium supplements, and the other confirmed their ability to increase the risk of heart disease. This study, published in the Journal of the American Heart Association and conducted by American scientists from several universities, found that calcium supplement users had a 22% increased risk of calcium plaque in the heart vessels. This was proven using computed tomography. The first time it was done at the beginning of the study, selecting volunteers without plaques in the vessels of the heart, and the second time after 10 years. And tomography revealed the negative effect of calcium supplements.
Question answer
Does calcium intake affect the development of heart disease?
The Council for Responsible Nutrition, which represents manufacturers of dietary supplements (including calcium), did not agree with the doctors' conclusions - and stated that there are studies showing the opposite.
Best lists
Of the listed drugs, we will highlight the best in the following categories:
- the best product in the price/quality category;
- best dietary supplement.
The best product in the price/quality category
This drug is perfect if you have bone problems. Effectively heals fractures, relieves joint pain, improves heart and eye function. Chewable tablets have a lemon flavor (unlike other analogues, which taste like chalk). The manufacturer is located in Norway, which means that you can rest assured about the quality of the components, because their products undergo strict testing.
Best Dietary Supplement
This Russian supplement will be a great help for the body if you want to help your bones. The composition is enriched with a number of other useful vitamins, such as vitamin A, C, E and group B, and the price will be lower than if you had to buy all these vitamins separately. It has shown itself to be effective in healing fractures and strengthening nails and teeth.
Food instead of drugs
Today, most researchers agree that to prevent osteoporosis, it is better not to take drugs with calcium or with calcium and vitamin D, but to consume foods that contain a lot of calcium. They, unlike drugs, do not sharply increase the concentration of calcium in the blood, and thus do not contribute to its deposition in the vessels.
Until the age of 24, while bones continue to grow, we need 1200 mg of calcium every day. This is important because during these years we build up a supply of calcium for the rest of our lives. Then it is enough to consume 1000 mg of this element daily. Women need higher doses during pregnancy and breastfeeding (1200-1600 mg per day), as well as after menopause (1500 mg/day). The best sources of calcium are milk and dairy products, as well as cabbage and greens (see table).
Calcium and vitamin D3 - basic pharmacotherapy for somatic polymorbidity
It is well known that insufficient intake of vitamin D and calcium in the body at any age has a negative effect on bone tissue, since it leads to the development of rickets in young children, slows down bone mass gain during the formation of the skeleton in adolescents, and also causes accelerated bone loss in adults of both sexes, which is accompanied by the development of osteoporosis.
It is important to note that there is evidence from epidemiological and clinical intervention studies, as well as animal models of human disease, that low vitamin D levels and insufficient dietary calcium intake increase the likelihood of developing a variety of other diseases, including various types of malignancies, chronic infections , inflammatory and autoimmune diseases, metabolic disorders, as well as arterial hypertension and cardiovascular diseases.
These circumstances require a reconsideration and understanding of the role of calcium and vitamin D in the treatment of patients with somatic polymorbidity. As evidence of the relationship between calcium and vitamin D deficiency and somatic polymorbidity, it is first of all worth citing known facts in accordance with the level of evidence, which was done in the work of M. Peterlik et al. [1] (table).
Pathogenetic understanding of the role of calcium and vitamin D in the genesis of somatic polymorbidity
Many cell types express calcium-sensing receptors (CaRs) that are capable of responding to changes in calcium concentration lasting several minutes; As a result, calcium ions serve as the “primary messenger” for various cellular reactions [2].
Strengthening signals from extracellular calcium, in turn, through the connection of receptors with activating or inhibitory G-proteins, is transmitted through various intracellular signaling pathways. Expression of functional CaRs mediates cell-specific responses to physiological changes in blood calcium concentrations.
CaR receptors not only regulate the secretion of parathyroid hormone in the parathyroid glands, but also play a key role in the formation of normal cartilage and bone tissue, and also limit the growth of normal and tumor cells.
On the other hand, low dietary calcium intake is accompanied by the development of hyperparathyroidism due to decreased CaR activity; this mechanism can lead to the development of not only osteoporosis and various malignant tumors, but also other chronic diseases.
In humans, vitamin D comes from two sources: it can be synthesized as vitamin D3 (cholecalciferol) in the epidermis upon exposure to ultraviolet radiation from the sun, and it can be absorbed from foods and dietary supplements, which in some countries may contain vitamin D2 (ergocalciferol). Both of these forms of vitamin D enter the liver, where they are converted into 25-hydroxyvitamin D, or 25(OH)D (it is possible to test the concentration in the patient in a laboratory). The term 25(OH)D is used to refer to the sum of 25(OH)D3 and 25(OH)D2. Thus, the plasma concentration of this metabolite reflects the total amount of vitamin D synthesized in the body and taken from food, being a reliable indicator of the level of vitamin D in a particular person.
The conversion of 25(OH)D3 to its most active metabolite, 1,25-dihydroxyvitamin D3(1,25(OH)2D3), is catalyzed by the enzyme 25(OH)D-1-alpha-hydroxylase, which is encoded by the CYP27B1 gene and is found primarily in the kidneys , but also in many other organs and tissues [3], including normal and tumor cells of the epithelium of the skin, gastrointestinal tract, male and female genital organs, as well as osteoblasts and osteoclasts, cells of the vascular, central nervous and immune systems.
The most active metabolite of vitamin D (1,25(OH)2D3) binds to the high-affinity nuclear vitamin D receptor (VDR), which regulates gene expression.
The intensity of intracellular synthesis of this metabolite in cells depends primarily on the level of 25(OH)D3 in surrounding tissues and is not related to the concentration of 1,25(OH)2D3 in the systemic circulation [4].
Therefore, at low serum 25(OH)D concentrations, 25(OH)D-1 alpha-hydroxylase activity may be insufficient to maintain tissue levels of 1,25(OH)2D3 sufficient for the effective regulation of autocrine and paracrine functions, as well as for cell growth and functioning. This explains the negative association with serum 25(OH)D concentration in a variety of chronic diseases [5]. Low serum 25(OH)D concentrations have also been demonstrated to be an important predictor of all-cause mortality [6].
In understanding how vitamin D and calcium levels influence the pathogenesis of chronic diseases, the fact that most cell types synthesize 25(OH)D-1-alpha-hydroxylase and cellular CaR is important.
Therefore, vitamin D and calcium deficiency impair cell-specific signaling pathways mediated by 1,25(OH)2D3/VDR and CaR, which are essential for normal cell function.
In particular, this mechanism has been demonstrated for osteoporosis and many malignant tumors such as colorectal and breast cancer.
Low serum 25(OH)D concentrations and insufficient calcium intake have been described as risk factors for diseases such as hypertension, obesity, metabolic syndrome and type 2 diabetes mellitus.
In addition, vitamin D and calcium deficiency have been correlated with the development of cardiovascular symptoms such as angina, coronary insufficiency, myocardial infarction, transient ischemic attack and stroke, as well as with increased mortality from chronic cardiovascular diseases [7–17]. .
According to many studies, deficiency of vitamin D and its metabolites plays a key role in the pathogenesis of a wide range of clinically important extraskeletal dysfunctions or diseases, especially muscle, cardiovascular, autoimmune pathologies and some malignancies.
Interestingly, a meta-analysis of 18 randomized clinical trials including 57,311 patients concluded that vitamin D supplementation reduced all-cause mortality (hazard ratio (RR) 0.93; 95% confidence interval (CI) 0.77–0 .96, compared to the control group). This may be due to the effects of vitamin D on the musculoskeletal system or various extraskeletal disorders [18].
Groups of people requiring mandatory examination of calcium and vitamin D levels
In accordance with the recommendations of M. Peterlik et al. (2009) [1], special diagnostic attention to calcium and vitamin D deficiency should be paid to the following categories of patients [19]:
- children, teenagers, young and old;
- patients with somatic polymorbidity;
- immobilization for more than 2 weeks or decreased physical activity;
- certain ethnic groups.
Calcium reduces the risk of cardiovascular complications
Observational studies suggest an inverse association between calcium intake and the development of vascular disease.
In the Iowa Women's Health Study of 34,486 postmenopausal women (55–69 years), RM Bostick et al. found that calcium intake in the top quartile (>1425 mg/day) compared with the bottom quartile (<696 mg calcium/day) reduced coronary heart disease mortality by 33% (RR 0.67, 95% CI 0 .47–0.94). According to the analysis, risk reduction depends on overall calcium intake and can be achieved by diet, supplementation, or both [20].
Likewise, EG Knox found a strong negative association between dietary calcium intake and mortality from coronary heart disease [21].
The Nurses' Health Study followed a group of 85,764 women aged 39 to 59 years over a 14-year period. Women taking total calcium intake in the top quintile (median 1145 mg/day) were found to have a lower risk of stroke (RR 0.69, 95% CI 0.50–0.95) compared with the bottom quintile ( median 395 mg/day) [22].
To explain the observed protective effect on blood vessels, it can be assumed that calcium has a beneficial effect on a large number of vascular risk factors. These, in particular, include a decrease in the following parameters in the patient [23]:
- blood pressure;
- serum lipid concentration;
- body weight, although in some cases the data are ambiguous.
In some trials, an inverse relationship between calcium levels and blood pressure levels was observed. In controlled randomized trials, a meta-analysis found that blood pressure decreases both when taking calcium with food and when it is taken in the form of supplements.
Consistent with these findings, the present study found that women over 45 years of age who consumed at least 679 mg of dietary calcium/day had a significantly reduced risk of hypertension. In women with dietary calcium intake in the top quintile (1000–2560 mg calcium/day), the risk was reduced by 13% (RR 0.87, 95% CI 0.81–0.93) [24].
Another potential cardioprotective mechanism may be a decrease in serum lipid concentrations. This is observed due to the binding of calcium to fatty and bile acids in the intestine, resulting in fat malabsorption. In addition, there is a direct effect of calcium on adipocytes in the form of increased lipolysis [25].
In a controlled, randomized trial, men treated with a calcium-rich diet significantly reduced total cholesterol, low-density lipoprotein (LDL) cholesterol, and apolipoprotein B [26].
Similarly, in a randomized placebo-controlled trial in postmenopausal women taking a dietary supplement containing 1000 mg calcium for 12 months, high-density lipoprotein (HDL) levels and their ratio to LDL levels increased [27].
With regard to weight loss, various large epidemiological studies suggest that dietary calcium intake and calcium supplementation may reduce patient weight [28], an effect mediated by the same mechanism as the effect on lipid profiles [29].
Safety of combined calcium and vitamin D3 preparations
Recently, a number of researchers have been discussing a slight increase in cardiovascular risk when taking calcium supplements. However, special attention should be paid to the fact that an increase in cardiovascular risk has been established only in relation to calcium monotherapy.
A meta-analysis of 15 double-blind, placebo-controlled studies was published in 2010 in the British Medical Journal (MJ Bolland et al.) and included data on more than 12,000 subjects. An increased risk of myocardial infarction of approximately 30% was observed in individuals taking calcium supplements (≥ 500 mg/day) compared to those receiving placebo [30].
However, there was no significant increase in the incidence of vascular endpoints. These included stroke (RR 1.20, 95% CI 0.96–1.50), death (RR 1.09, 95% CI 0.96–1.23) and composite endpoints of myocardial infarction, stroke and sudden death (RR 1.18, 95% CI 1.00–1.39).
Although the meta-analysis data should be interpreted as significant evidence that calcium supplementation (without vitamin D) may potentially increase the risk of myocardial infarction, some limitations and even controversies must be taken into account.
First, the statistical significance of the difference was only borderline (RR 1.31, 95% CI 1.02–1.67; p = 0.035), with the 95% confidence level approaching 1, so evaluation of these results should be done with caution. In addition, the studies included in the analysis were designed to evaluate the effect of calcium on bone density and fracture risk. None of the studies presented included cardiovascular complications as a primary or secondary endpoint. As a result, they were not counted in a standardized way, which could lead to over- or under-reporting.
Third, although the meta-analysis data show a clear increase in the risk of myocardial infarction, this relationship is not consistent with the risk of stroke, death, or the composite endpoint of myocardial infarction, stroke, and sudden death. It may be added that the studies excluded data on calcium supplementation with vitamin D, which is the recommended strategy for preventing fractures in most older people. In this regard, it should be noted that a large number of large-scale studies of calcium supplementation in combination with vitamin D did not reveal an increase in cardiovascular risk [31].
It is possible, although not certain, that correction of vitamin D deficiency may prevent the potentially harmful vascular effects of calcium supplementation [18, 32].
Finally, with the exception of a relatively small group of subjects [30], individual studies of calcium supplements have not found a significant increase in cardiovascular risk.
In fact, data from the present randomized placebo-controlled trial by JR Lewis et al., without a meta-analysis, do not indicate a high risk of death or primary hospitalization related to atherosclerosis in patients taking calcium supplements [33]. Moreover, sub-analysis even suggests a cardioprotective effect in patients with pre-existing cardiovascular disease.
Selection of correction methods and doses of calcium and vitamin D in the basic strategy for managing patients with multimorbidity
An international study of vitamin D intake [34] clearly showed that in many countries dietary vitamin D levels were too low to maintain 25(OH)D levels in the general population in the range of 40–100 nmol/L, which is considered adequate for optimal health [35].
KD Cashman et al. [36] calculated that individuals aged 20–40 years needed daily vitamin D intake of 300 to 1600 IU to maintain vitamin D balance in winter, depending on the amount of sun exposure in the previous summer.
M. L. Nelson et al. [37] reported that vitamin D3 at a daily dose of 800 IU provided a sustained “optimal” serum 25(OH)D concentration (≥ 75 nmol/L) in 80% of premenopausal women.
Taking a similar daily dose of vitamin D3 maintained serum 25(OH)D concentrations at 50 nmol/L in 97.5% of elderly people with insufficient sun exposure [38].
There is reliable documentation of the beneficial effects of vitamin D at a dose of 800 IU on various health indicators. Taking vitamin D3 at a dose of 700–800 IU/day ensures a normal level of bone tissue remodeling in healthy men in winter [39], and also reduces the risk of colorectal and breast cancer by 50% [40, 41].
An average calcium intake of 1000–1200 mg/day is based not only on physiological considerations, but also on health studies.
For example, a daily dose of calcium of 1200 mg provides effective prevention of bone loss and fractures due to osteoporosis in people aged 50 years and older [42], and also leads to a 40–50% reduction in the risk of colorectal cancer in men and breast cancer in premenopausal women [43, 44].
In order to prevent or improve the course of many chronic diseases, simultaneous correction of insufficiency of vitamin D and calcium consumed in food is necessary, which is explained by two reasons.
First, dietary intakes of vitamin D and calcium are closely related [45], and vitamin D deficiency is often associated with low calcium intake.
Second, because vitamin D and calcium have joint effects on cell proliferation, differentiation, and function, it can be hypothesized that adequate vitamin D would be required to achieve the beneficial effects of increasing calcium intake and vice versa.
Based on a meta-analysis of 10 randomized controlled trials of the effect of oral vitamin D with or without calcium on the risk of hip fracture in older adults compared with placebo or no treatment, Boonen et al. [46] concluded that vitamin D supplementation appears to reduce the risk of hip fracture only when supplemented with calcium.
JM Lappe et al. [47] presented the results of a randomized, placebo-controlled study, according to which in postmenopausal women, combined intake of calcium and vitamin D3, that is, 1400–1500 mg of calcium along with 1100 IU of vitamin D3, reduces the cumulative risk of malignant tumors of the breast, lungs, and colon. , uterus and hematopoietic system to 0.232 after 4 years of therapy.
E. Cho et al. [48], based on an analysis of pooled primary data from 10 cohort studies that included follow-up results in more than 500 thousand people over 6–16 years, concluded that the greatest reduction in the risk of colorectal cancer was achieved with simultaneous intake of high doses of vitamin D and calcium.
Supplementation with a combination of vitamin D and calcium is a safe and cost-effective strategy for the prevention of osteoporosis, colorectal and breast cancer, and quite possibly many other components of medical multimorbidity.
It should be emphasized that the daily intake of 800 IU of vitamin D and 1000–1200 mg of calcium is much lower than the currently accepted maximum permissible doses, which are 2000 IU (= 50 μg) of vitamin D3 and 3000 mg of calcium [49].
A relatively inexpensive way to prevent osteoporotic fractures is a combination of 1200 mg/day calcium and 800 IU/day vitamin D3. However, a pronounced effect from taking this combination is observed only in groups of patients who comply with the dosage regimen by at least 80% [42].
Poor adherence, which occurs with long-term use of any drug, limits the effectiveness of the combination of vitamin D and calcium in correcting related deficiencies in the general population. As a result, the combination of vitamin D and calcium should only be recommended for the purpose of disease prevention in high-risk groups, i.e., among individuals who cannot achieve adequate intake of vitamin D and calcium by other means; this may be due to specific living conditions (immobilization, disability, old age, chronic diseases), traditional or personal food preferences, lifestyle (lack of physical activity, constant stay indoors), etc.
Literature
- Peterlik M., Cross HS Vitamin D and calcium insufficiency-related chronic diseases: molecular and cellular pathophysiology // Eur. J. Clin. Nutr. 2009.
- Tfelt-Hansen J., Brown EM The calcium-sensing receptor in normal physiology and pathophysiology: a review // Crit. Rev. Clin. Lab. Sci. 2005, 42, 35–70.
- Zehnder D., Bland R., Williams MC, McNinch RW, Howie AJ, Stewart PM, Hewison M. Extrarenal expression of 25-hydroxyvitamin D3–1 alpha-hydroxylase // J. Clin. Endocrinol. Metab. 2001, 86, 888–894.
- Anderson PH, O'Loughlin PD, May BK, Morris HA Modulation of CYP27 B1 and CYP24 mRNA expression in bone is independent of circulating 1,25(OH)2D3 levels // Bone. 2005, 36, 654–662.
- Cross, HS, Kallay E. Regulation of the colonic vitamin D system for prevention of tumor progression: an update // Future Oncol. 2009, 5, 493–507.
- Dobnig H., Pilz S., Scharnagl H., Renner W., Seelhorst U., Wellnitz B., Kinkeldei J., Boehm BO, Weihrauch G., Maerz W. Independent association of low serum 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality // Arch. Intern. Med. 2008, 168, 1340–1349.
- McCarron DA, Reusser ME Finding consensus in the dietary calcium-blood pressure debate // J. Am. Coll. Nutr. 1999, 18, 398 S-405 S.
- Hintzpeter B., Mensink GB, Thierfelder W., Muller MJ, Scheidt-Nave C. Vitamin D status and health correlates among German adults // Eur. J. Clin. Nutr. 2008, 62, 1079–1089. Int. J. Environ. Res. Public Health 2009, 62601.
- Judd SE, Nanes MS, Ziegler TR Wilson PW, Tangpricha V. Optimal vitamin D status attenuates the age-associated increase in systolic blood pressure in white Americans: results from the third National Health and Nutrition Examination Survey // Am. J. Clin. Nutr. 2008, 87, 136–141.
- Davies KM, Heaney RP, Recker RR, Lappe JM, Barger-Lux MJ, Rafferty K., Hinders S. Calcium intake and body weight // J. Clin. Endocrinol. Metab. 2000, 85, 4635–4638.
- Arunabh S., Pollack S., Yeh J., Aloia JF Body fat content and 25-hydroxyvitamin D levels in healthy women // J. Clin. Endocrinol. Metab. 2003, 88, 157–161.
- Alemzadeh R., Kichler J., Babar G., Calhoun M. Hypovitaminosis D in obese children and adolescents: relationship with adiposity, insulin sensitivity, ethnicity, and season // Metabolism. 2008, 57, 183–191.
- Pittas AG, Lau J., Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis // J. Clin. Endocrinol. Metab. 2007, 92, 2017–2029.
- Reis JP, von Muhlen D., Kritz-Silverstein D., Wingard DL, Barrett-Connor E. Vitamin D, parathyroid hormone levels, and the prevalence of metabolic syndrome in community-dwelling older adults // Diabetes Care. 2007, 30, 1549–1555.
- Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E., Lanier K., Benjamin EJ, D'Agostino RB, Wolf M., Vasan RS Vitamin D deficiency and risk of cardiovascular disease // Circulation. 2008, 117, 503–511.
- Bostick RM, Kushi LH, Wu Y., Meyer KA, Sellers TA, Folsom AR Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women // Am. J. Epidemiol. 1999, 149, 151–161.
- Hagstrom E., Hellman P., Larsson TE, Ingelsson E., Berglund L., Sundstrom, J., Melhus H., Held C., Lind L., Michaelsson K., Arnlov J. Plasma parathyroid hormone and the risk of cardiovascular mortality in the community. Circulation. 2009, 119, 2765–2771.
- Autier P., Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials // Arch Intern Med. 2007, 167: 1730–1737.
- Peterlik. M., Boonen S., Cross HS, Lamberg-Allardt C. Vitamin D and Calcium Insufficiency-Related Chronic Diseases: an Emerging World-Wide Public Health Problem // Int. J. Environ. Res. Public Health. 2009, 6, 2585–2607.
- Bostick RM, Kushi LH, Wu Y., Meyer KA, Sellers TA, Folsom AR Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women // Am J Epidemiol. 1999, 149: 151–161.
- Knox EG Ischemic-heart-disease mortality and dietary intake of calcium // Lancet. 1973, 1:1465–1467.
- Iso H., Stampfer MJ, Manson JE, Rexrode K., Hennekens CH, Colditz GA, Speizer FE, Willett WC Prospective study of calcium, potassium, and magnesium intake and risk of stroke in women // Stroke. 1999, 30: 1772–1779.
- Chung M., Balk E.M., Brendel M. et al. Vitamin D and calcium: a systematic review of health outcomes // Evid Rep Technol Assess (Full Rep). 2009, 1–420.
- Wang L., Manson JE, Buring JE, Lee IM, Sesso HD Dietary intake of dairy products, calcium, and vitamin D and the risk of hypertension in middle-aged and older women // Hypertension. 2008, 51: 1073–1079.
- Zemel MB, Shi H., Greer B., Dirienzo D., Zemel PC Regulation of adiposity by dietary calcium // FASEB J. 2000, 14: 1132–1138.
- Denke MA, Fox MM, Schulte MC Short-term dietary calcium fortification increases fecal saturated fat content and reduces serum lipids in men // J Nutr. 1993. 123:1047–1053.
- Reid IR, Mason B., Horne A., Ames R., Clearwater J., Bava U., Orr-Walker B., Wu F., Evans MC, Gamble GD Effects of calcium supplementation on serum lipid concentrations in normal older women : a randomized controlled trial // Am J Med. 2002, 112: 343–347.
- Heaney RP Normalizing calcium intake: projected population effects for body weight // J Nutr. 2003, 133: 268 S–270 S.
- Parikh SJ, Yanovski JA Calcium intake and adiposity // Am J Clin Nutr. 2003, 77: 281–287.
- Bolland MJ, Avenell A., Baron JA, Gray A., MacLennan GS, Gamble GD, Reid IR Effect of calcium supplements on the risk of myocardial infarction and cardiovascular events: metaanalysis // BMJ. 2010, 341: c3691.
- Hsia J., Heiss G., Ren H. et al. Calcium/vitamin D supplementation and cardiovascular events // Circulation. 2007, 115: 846–854.
- Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E., Lanier K., Benjamin EJ, D'Agostino RB, Wolf M., Vasan RS Vitamin D deficiency and risk of cardiovascular disease // Circulation. 2008, 117: 503–511.
- Lewis JR, Calver J., Zhu K., Flicker L., Prince RL Calcium supplementation and the risks of atherosclerotic vascular disease in older women: results of a 5-year RCTand a 4. 5-year follow-up // J Bone Miner Res. 2011, 26: 35–41.
- Calvo MS, Whiting SJ, Barton CN Vitamin D intake: a global perspective of current status // J. Nutr. 2005, 135, 310–316.
- Yetley EA, Brule D., Cheney MC, Davis CD, Esslinger KA, Fischer, PW, Friedl KE, Greene-Finestone LS, Guenther PM, Klurfeld DM, L'Abbe MR, McMurry KY, Starke-Reed PE, Trumbo PR Dietary reference intakes for vitamin D: justification for a review of the 1997 values // Am. J. Clin. Nutr. 2009, 89, 719–727.
- Cashman KD, Hill TR, Lucey AJ, Taylor N., Seamans KM, Muldowney S., Fitzgerald AP, Flynn A., Barnes MS, Horigan G., Bonham MP, Duffy EM, Strain JJ, Wallace JM, Kiely M. Estimation of the dietary requirement for vitamin D in healthy adults // Am. J. Clin. Nutr. 2008, 88, 1535–1542.
- Nelson ML, Blum JM, Hollis BW, Rosen C., Sullivan SS Supplements of 20 microg/d cholecalciferol optimized serum 25-hydroxyvitamin D concentrations in 80% of premenopausal women in winter // J. Nutr. 2009, 139, 540–546.
- Cashman KD, Wallace JM, Horigan G., Hill TR, Barnes MS, Lucey, AJ, Bonham MP, Taylor N., Duffy EM, Seamans K., Muldowney S., Fitzgerald AP, Flynn A., Strain JJ, Kiely M Estimation of the dietary requirement for vitamin D in free-living adults > 64 years of age // Am. J. Clin. Nutr. 2009, 89, 1366–1374.
- Viljakainen HT, Vaisanen M., Kemi V., Rikkonen T., Kroger H., Laitinen E., Rita H., Lamberg-Allardt C. Wintertime vitamin D supplementation inhibits seasonal variation of calcitropic hormones and maintains bone turnover in healthy men / / J. Bone Miner. Res. 2009, 24, 346–352.
- Gorham ED, Garland CF, Garland FC, Grant WB, Mohr SB, Lipkin, M., Newmark HL, Giovannucci E., Wei M., Holick MF Vitamin D and prevention of colorectal cancer // J. Steroid Biochem. Mol. Biol. 2005, 97, 179–194.,
- Garland CF, Gorham ED, Mohr SB, Grant WB, Giovannucci EL, Lipkin M., Newmark H., Holick MF, Garland FC Vitamin D and prevention of breast cancer: Pooled analysis // J. Steroid Biochem. Mol. Biol. 2007, 103, 708–711.
- Tang BM, Eslick GD, Nowson C., Smith C., Bensoussan A. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis // Lancet. 2007, 370, 657–666.
- Shin MH, Holmes MD, Hankinson SE, Wu K., Colditz GA, Willett WC Intake of dairy products, calcium, and vitamin D and risk of breast cancer // J. Natl. Cancer Inst. 2002, 94, 1301–1311.
- Slattery ML, Sorenson AW, Ford MH Dietary calcium intake as a mitigating factor in colon cancer // Am. J. Epidemiol. 1988, 128, 504–514.
- Berube S., Diorio C., Verhoek-Oftedahl W., Brisson J. Vitamin D, calcium, and mammographic breast densities // Cancer Epidemiol. Biomarkers Prev. 2004, 13, 1466–1472.
- Boonen S., Lips P., Bouillon R., Bischoff-Ferrari HA, Vanderschueren D., Haentjens P. Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials / / J. Clin. Endocrinol. Metab. 2007, 92, 1415–1423.
- Lappe JM, Travers-Gustafson D., Davies KM, Recker RR, Heaney RP Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial // Am. J. Clin. Nutr. 2007, 85, 1586–1591.
- Cho E., Smith-Warner SA, Spiegelman D., Beeson WL, van den Brandt PA, Colditz GA, Folsom AR, Fraser GE, Freudenheim JL, Giovannucci E., Goldbohm RA, Graham S., Miller AB, Pietinen P. , Potter JD, Rohan TE, Terry P., Toniolo P., Virtanen MJ, Willett WC, Wolk A., Wu K., Yaun SS, Zeleniuch-Jacquotte A., Hunter DJ Dairy foods, calcium, and colorectal cancer: a pooled analysis of 10 cohort studies // J. Natl. Cancer Inst. 2004, 96, 1015–1022.
- Human vitamin and mineral requirements. Report of a Joint FAO/WHO Expert Consultation. Food and Agriculture Organization, Rome, Italy, 2002.
A. V. Naumov, Doctor of Medical Sciences, Professor A. L. Vertkin, Doctor of Medical Sciences, Professor
GBOU VPO MGMSU im. A. I. Evdokimova Ministry of Health of the Russian Federation, Moscow
Contact information for authors for correspondence