- Morphine
- Ketamine
- Fentanyl
- Promedol
- Tramadol
- Common effects for all opioid agonists
Attention!
Drug use causes irreparable harm to health and poses a danger to life!
Methadone is a powerful pain reliever that is used medically. In the USA and European countries, methadone is used for substitution therapy for opiate addiction. The essence of these programs is that addicts are given small doses of methadone every few days. As a result, opioid receptors are blocked and withdrawal does not occur. In addition, cravings for heroin or other street drugs are reduced.
The effectiveness of the program has not been fully studied. What is clear for now is that without a desire to quit and professional psychological help, no types of replacement therapy will help.
Methadone substitution therapy is not carried out in the CIS countries. This is argued by the fact that the technique is more harmful than useful. Given the peculiarities of our medicine, such programs may lead to an increase in the amount of street methadone.
Methadone lasts longer than all known opiates. It is because of this property that the drug is chosen for replacement therapy. It is believed that the use of methadone in recommended pharmacological doses does not lead to a toxic effect and does not cause addiction.
If we analyze methadone analogues, then it is more correct to compare it with medications that are used for pain relief in anesthesiology and palliative medicine. Such means include:
- Morphine;
- Ketamine;
- Fentanyl;
- Promedol;
- Tramadol.
There is no point in comparing methadone with street drugs, as they have a more pronounced toxic and narcotic effect. But the closest action to methadone is heroin.
Morphine
It is the most widely used opioid in the world. It is used in medicine in cases where pain relief is needed in urgent conditions. Most often prescribed for open fractures, myocardial infarction, damage to internal organs, after severe operations with severe tissue damage.
Morphine is an alkaloid from the sleeping poppy. There have been attempts to synthesize morphine, but all of them are not economically viable, so morphine is still extracted from biological raw materials.
Morphine is rarely used as a drug because it is not available without a prescription. Addicted people use morphine if there are no other options (heroin or hanka).
Detoxification
3 000 ₽
Calling a narcologist to your home
3 000 ₽
Overdose
Persons over 14 years of age are usually prescribed 50 mg of the drug at a time (1 tablet). Repeated administration of the tablet form is allowed after 30-60 minutes if the desired effect does not occur.
The permissible single dose for injection is 50-100 mg (1-2 ampoules). Repeated administration should be carried out no earlier than after 4 hours.
The maximum dose of the drug per day for persons over 14 years of age is 400 mg, sometimes the dosage is increased to 600 mg. Elderly people should not take more than 300 mg of the drug per day.
Usually, for children under 14 years of age, the doctor prescribes Tramadol in the form of injections or drops. A single dosage depends on the patient’s weight (1-2 mg/kg), the maximum dosage per day should not exceed 8 mg/kg.
Increasing these dosages can lead to coma and death. If symptoms of overdose occur, it is important to provide fresh air to the patient and urgently call an ambulance.
Ketamine
Ketamine is an anesthetic that helps put a patient into medicated sleep and numb the patient for surgery. The mechanism of action of ketamine is through stimulation of NMDA receptors. The subsequent effect is so similar to the effect of opiates that this drug can be considered an analogue of morphine or methadone: both in its analgesic effect and in its narcotic effect.
A special feature of ketamine is that it blocks the transmission of nerve impulses from the spinal cord to the brain. Normally, pain impulses from peripheral receptors go to the dorsal ganglion, then to the spinal cord, and only then through the brain stem to the postcentral gyrus. When ketamine works, it breaks the neural connection at the level of the brain stem, and as a result, the person does not feel pain or other sensory sensations.
The same goes for movements. The impulse to the muscles goes from the precentral gyrus to the brain stem, then to the spinal cord and then to the muscles. Communication is also interrupted at the level of the brain stem. As a result, a person can open his eyes, move them to the sides and even express emotions, but at this moment he is completely “cut off” from sensory sensations.
Ketamine is very toxic, so they try not to use it unnecessarily, and pharmaceutical companies are looking for safer analogues.
Fentanyl
Unlike the previous drug, fentanyl is an opioid agonist and is therefore used as a pain reliever. Fentanyl acts quickly, 1-2 minutes after administration, but the effects last only 15-25 minutes.
The properties of fentanyl and its selective stimulation of opioid receptors have led to the fact that this analgesic is used for the relief of acute pain, for anesthesia, or for combined neuroleptanalgesia (when the patient is put to sleep and given substances to block pain impulses).
Fentanyl can be used as a drug to obtain drug intoxication. But this often ends tragically, since this drug does not give a strong effect in small doses. And in large doses, it causes respiratory arrest, slowing of the heartbeat, disruption of the regulation of sweating and, accordingly, heat exchange. The substance is metabolized in the liver and therefore can cause destruction of hepatocytes.
Ketamine quickly becomes addictive. If you stop using ketamine after using it several times, withdrawal symptoms may begin, similar to heroin withdrawal symptoms.
All types of drug addiction
Drug addiction treatment
More details
Female, age, beer
Treatment of alcoholism
More details
Compatibility in oncology
The rules for taking medications do not indicate that it is unacceptable to combine them, but it clearly states what will happen if you combine them. When used correctly and prescribed by a doctor, this combination is permissible, and phenazepam and tramadol can be used together where there is a need for simultaneous use.
According to WHO regulations, there is a pain scale for oncology. In the second degree, when the pain intensity is 4–6 points, the above-mentioned analgesic is used.
If pain prevents the patient from sleeping, or there are indications for prescribing tranquilizers, then the doctor may prescribe tramadol and phenazepam in a therapeutic dosage. The compatibility of these drugs in cancer is completely justified and has a beneficial effect. Expert opinion. If the treatment of cancer patients requires the simultaneous use of psychotropic and painkillers, then it is permissible to combine these medications without exceeding the dosages prescribed by the doctor.
Promedol
Its structure is very similar to fentanyl, and its action resembles morphine. The drug is used to relieve pain in injuries, gastric and duodenal ulcers, myocardial infarction, and after operations. In Russia, the drug is sold by prescription. It is rarely used on the drug market; it is mainly used by young guys without drug “experience”. They think that this drug is not as toxic and dangerous as other opioids that need to be injected into a vein. But this is a misconception, since opioid receptor agonists, such as promedol, cause physical and mental dependence.
Even in pharmacological doses, promedol can cause jaundice, urinary retention, severe vomiting, constipation, and breathing problems. When this drug is used for recreational purposes, all these phenomena are aggravated. Liver cells are destroyed, impulse transmission through neurons to the central nervous system is slowed down and disrupted, endogenous opiate reserves are depleted, respiratory depression occurs, and death from overdose is possible.
Dependence on such drugs should be treated in special rehabilitation and recovery centers for addicts. Without outside help, promedol addicts switch to heroin or desomorphine.
Drug effect and side effects
Drug addicts taking Tramadol experience:
- A feeling of bliss that lasts almost the entire period of intoxication
- Duration of the trip is about 10 hours
- Excitement due to the duality of the mechanism of action
- Slowness, lethargy, drowsiness
- Getting a "high" from ordinary things that caught their attention (watching a tree)
Symptomatic therapy with the drug often goes well. But exceeding the dose and using it for non-medical purposes is accompanied by the following symptoms:
- Increased heart rate
- Headache
- Excessive sweating
- Muscle weakness
- Nausea and vomiting
- Insomnia
- Impaired coordination of movements
- Severe lethargy
- Stomach ache
- Allergy
- Dyspnea
- Swallowing disorder
- Urinary retention
Tramadol
Tramadol is a pain reliever whose mechanism of action is to stimulate opioid receptors with subsequent disruption of the transmission of pain impulses through synapses in the central nervous system. Tramadol is included in military first aid kits as a means for emergency pain relief from combat wounds.
In Russia, tramadol is not sold in pharmacies without a prescription, since the drug is considered potent. There are few cases of tramadol addiction. Basically, drug addicts use this drug as a reserve in the absence of other opiates.
To get the desired high from tramadol, you need to take a lot of it, and this can cause an overdose or respiratory arrest. Experienced drug addicts have tolerance to opiates, therefore, to obtain narcotic intoxication from tramadol, its dose must exceed the permissible dose several times.
If heroin or other hard drugs run out, withdrawal begins after 10-14 hours. At this point, drug addicts use tramadol as replacement therapy, just like with methadone. But the problem remains unresolved: tramadol, like other opiates, causes withdrawal and without a new dose, withdrawal will still begin.
Efficiency of using analogues
Since Tramadol is an analgesic drug available only with a doctor’s prescription, analogues can be used with its permission. If a patient tries to make a choice on his own, the pharmacy will not sell him the medicine. They are especially careful about drug therapy if injections are needed. The active substance directly enters the systemic bloodstream, bypassing physiological barriers. Therefore, the risk of side effects increases.
The doctor will take into account the difference, the presence of other active ingredients in addition to the analgesic. If a person has only pain, it is recommended to use painkillers. If there is fever or inflammation, complex medications are selected. For example, in combination with a non-steroidal anti-inflammatory drug or antipyretic component. The effectiveness of using analogues is achieved if all data on laboratory and instrumental examination methods are taken into account. During the treatment process, tests are repeated, revealing a positive or negative result.
Common effects for all opioid agonists
Main effects after taking opioid agonists:
- constriction of the pupils;
- vomit;
- loss of sensation;
- impaired reaction, slowed thinking, suppressed reflexes;
- disturbance of intestinal motility;
- the appearance of arrhythmia, bradycardia;
- decreased respiratory rate, respiratory arrest;
- toxic damage to the liver and kidneys;
- the formation of a persistent dominant in the brain that the new dose is above all else;
- disruption of impulse transmission in the brain;
- depression of cognitive functions and the ability to think analytically.
All drugs that stimulate opioid receptors are toxic, they cause addiction and cause personality destruction. The changes that occur after drug addiction to pharmaceutical opiates are irreversible.
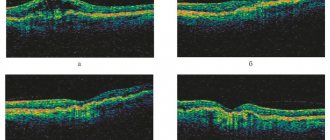
Initiation of pain therapy
First of all, if there is severe pain, you need to make sure that it is in no way related to serious complications of the underlying pathology. Such complications can be metastatic lesions of the brain, infection, etc. To understand the cause of severe pain, you need to undergo ultrasound, CT and MRI. If concerns are confirmed, appropriate action is taken. If there are no serious complications, the principle of taking an analgesic is based on the severity of discomfort and the effectiveness of previous medical treatment. facilities.
The fundamental basis of pain therapy is the World Health Organization's Ladder. This ladder determines the following types of pain discomfort: • burning; • piercing; • cutting; • pulsating; • drilling. The intensity of the pain syndrome can be: • weak; • average; • strong. The duration of discomfort can be: • acute; • chronic. According to the nature of the localization of pain, there are: • abdominal (present in the abdominal cavity); • muscular-articular (everything is clear here by the name).