Roza Ismailovna Yagudina , Ph.D. Sc., prof., head. Department of Organization of Drug Supply and Pharmacoeconomics and Head. laboratory of pharmacoeconomic research of the First Moscow State Medical University named after. I. M. Sechenov.
Evgenia Evgenievna Arinina , Ph.D., leading researcher at the laboratory of pharmacoeconomic studies of the First Moscow State Medical University named after. I. M. Sechenova
Cardiovascular diseases (CVDs) are the leading cause of death worldwide. WHO estimates that 17.3 million people died from CVDs in 2008, accounting for 30% of all deaths worldwide. Of this number, 7.3 million died from coronary heart disease. According to WHO forecasts, by 2030, approximately 23.3 million people will die from CVDs annually.
The group of cardiovascular diseases includes several nosological units:
- coronary heart disease - a disease of the blood vessels that supply blood to the heart muscle;
- disease of the blood vessels in the brain that supply it with blood;
- disease of the peripheral arteries that supply blood to the arms and legs;
- rheumatic carditis - damage to the heart muscle and heart valves as a result of a rheumatic attack caused by streptococcal bacteria;
- congenital heart disease - deformations of the structure of the heart existing from birth;
- Deep vein thrombosis and pulmonary embolism - the formation of blood clots in the leg veins that can dislodge and move towards the heart and lungs.
One of the most common pathologies in the structure of CVD is coronary heart disease (CHD), to which we will devote a number of articles. IHD, as defined by WHO, is acute or chronic cardiac dysfunction resulting from an absolute or relative decrease in the supply of arterial blood to the myocardium.
In more than 90% of cases, the anatomical basis for the development of coronary artery disease is damage to the coronary arteries of the heart, leading to a decrease in coronary blood flow and an imbalance between the need of the heart muscle for oxygen and nutrients and the blood supply capabilities of the heart. Often this effect is caused by dyslipidemias, leading to the development of atherosclerosis, therefore, in the first article devoted to the problem of pharmacotherapy of IHD, we will dwell in detail on dyslipidemias (hyperlipidemias).
Currently, the following forms of IHD are distinguished:
- Sudden cardiac arrest
- Angina pectoris
- Silent cardiac ischemia
- Syndrome X (microvascular angina)
- Myocardial infarction
- Cardiosclerosis (atherosclerosis)
- Heart failure
- Heart rhythm disturbances
Causes
- Heredity.
- Hypothyroidism is a dysfunction of the thyroid gland.
- Diabetes.
- Obstructive liver diseases.
- Taking diuretics, immunosuppressants and other medications.
- Increased content of animal fats in food.
Provoking factors include a sedentary lifestyle, cholesterol abuse, alcohol intake, smoking, and a stressful personality type. The sooner a patient at risk contacts a lipidologist, the higher his chances of avoiding complications.
Tests and diagnostics
- Blood chemistry. Lipoproteins are studied fractionally (6 indicators). Traditionally, blood sampling is recommended on an empty stomach. However, studies have shown that the differences in blood parameters taken on an empty stomach and after a meal are very small. The result of the biochemical study is a statement of increased levels of lipids and protein. The analysis includes determining the atherogenicity coefficient, which reflects the ratio of atherogenic to antiatherogenic lipoproteins. This coefficient accurately reflects the favorable/unfavorable combination of lipoproteins to determine the risk of developing coronary artery disease. Sometimes the levels of apolipoproteins are additionally determined: apolipoprotein A1 , which is included in high-density lipoproteins and apolipoprotein B , which is included in low-density lipoproteins. ApoB is a marker of atherogenic lipoproteins and its increase indicates a high risk of cardiovascular diseases.
- Depending on the underlying disease, additional examinations are prescribed, which may include a blood test for sugar, insulin levels, Noma index, coagulogram, ECG, MRI of the brain, ultrasound of the vessels of the lower extremities, etc.
Principles of treatment of secondary dyslipidemia
If the disease develops against the background of another disease, it is very important to determine the original source and eliminate it. Complex therapy includes non-drug and drug methods.
Non-drug treatment
It is important for the patient to normalize body weight. For this purpose, he is prescribed dosed physical activity and a diet with limited animal fats. The diet must be enriched with vitamins and dietary fiber, and preference should be given to vegetables and fruits. It is mandatory to give up alcohol and smoking, otherwise other actions will be meaningless.
Drug treatment includes the following drugs:
- statins - to reduce cholesterol synthesis in the liver, to relieve inflammation;
- inhibitors of cholesterol absorption in the intestine;
- bile acid sequestrants;
- fibrates – to reduce triglyceride levels and increase high-density lipoprotein levels;
- Omega-3 polyunsaturated fatty acids.
Progressive lipidology specialists also practice extracorporeal methods indicated for severe forms of the disease. Genetic engineering methods have been developed for patients with a hereditary form.
Dyslipidemia (DLP) is a violation of the normal (physiological) ratio of blood lipids (fats). If it persists for a long time, it leads to the development of atherosclerosis and diseases of the cardiovascular system, increasing the risk of developing such serious diseases as heart attack and stroke.
Synonyms Russian
“Bad” cholesterol, hypercholesterolemia, poor lipid profile.
English synonyms
Dyslipidemia, “bad” cholesterol, hypercholesterolemia, abnormal lipid profile.
Symptoms
Dyslipidemia does not manifest itself for a long time and can be discovered accidentally. Although it refers more to laboratory terms, some people may also have external manifestations associated with the deposition of cholesterol in various parts of the body:
- xanthomas are dense nodules over tendons (dense structures that attach muscles to bones), and they are also found on the hands, less often on the soles of the feet, palms;
- xanthelasmas - flat yellow nodules or nodules that do not differ in color from other areas of the skin, under the skin of the eyelids;
- lipoid arc of the cornea - a white or grayish-white rim along the edges of the cornea of the eye; the appearance of this symptom before the age of 50 indicates the presence of hereditary dyslipidemia.
Most often, external signs are observed in individuals with hereditary disorders of lipid metabolism.
There may also be various symptoms of organ damage that appear with the development of atherosclerosis due to DLP, for example, pain in the heart, pain in the legs when walking, memory impairment, and dizziness. With hereditary dyslipidemia, the first manifestations may be a stroke or heart attack without any chronic diseases.
Who is at risk?
- Persons in whom one or both parents have been diagnosed with dyslipidemia or early development of atherosclerosis;
- people with diseases such as diabetes, hypertension, hypothyroidism, chronic kidney disease, metabolic syndrome, Cushing's syndrome;
- obese people (BMI 30 and above) leading a sedentary lifestyle;
- people with bad habits such as smoking, alcohol abuse (increases TG);
- women after menopause;
- men over 45 years old;
- people taking medications that may negatively affect the lipid profile (for example, glucocorticoids, beta blockers, some diuretics, retinoids, anabolic steroids, antidepressants).
General information about the disease
Cholesterol (C) is a waxy substance found in all cells of your body. It is synthesized mainly in the liver and in smaller quantities in many other organs. 20-30% of cholesterol enters the body with food. It has several different functions, including energy storage, signal transduction, building cellular structures, producing hormones and steroids, activating enzymes, supporting brain function, and absorbing fat-soluble vitamins. Cholesterol and triglycerides (TG) are transported in the bloodstream in complex with proteins and in this form they are called lipoproteins. Depending on the density, the following main types of lipoproteins are distinguished: chylomicrons (CM), very low density lipoproteins (VLDL), low density lipoproteins (LDL), intermediate density lipoproteins (IDL), high density lipoproteins (HDL).
LDL contains 65-75% of total plasma cholesterol. TG are included in almost all drugs, but predominate in cholesterol and VLDL. After eating fatty foods, their concentration in the blood quickly increases, but normally returns to its original level after 10-12 hours.
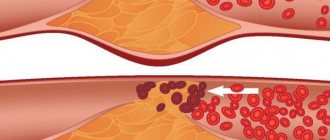
Dyslipidemia usually means that LDL or TG levels are too high. It may also mean that your HDL levels are too low. LDL is considered the “bad” type of cholesterol because it can accumulate and form plaque on the walls of the arteries, thereby narrowing the lumen. This condition is called atherosclerosis. Atherosclerosis, for example in the coronary vessels, can cause coronary heart disease (CHD) and cause a heart attack.
It is also known that very high triglyceride levels significantly increase the risk of developing pancreatitis and hepatosplenomegaly. HDL is the “good” cholesterol because it helps remove LDL from the blood.
Triglycerides are stored in fat cells - sources of energy in reserve. If a person consumes more calories than he expends, then all the excess can turn into triglycerides.
High triglyceride levels, like LDL, increase your risk of heart attack and/or stroke. Low HDL levels are also associated with a higher risk of "vascular accidents."
According to the mechanism of occurrence, dyslipidemia can be primary or secondary. Primary dyslipidemia is inherited, while secondary dyslipidemia is an acquired condition. In the hereditary form of the disease, certain gene mutations can cause overproduction or defective elimination of triglycerides, high levels of LDL, or underproduction/excessive elimination of HDL.
Among primary dyslipidemias, the following diseases are distinguished:
- familial combined hyperlipidemia is the most common inherited cause of high LDL and triglycerides; as a rule, the first symptoms indicating this pathology appear in adolescence or at the age of 20 years; individuals with this condition are at higher risk of early-onset CAD, which can lead to a heart attack;
- familial hypercholesterolemia and polygenic hypercholesterolemia - both diseases are characterized by high levels of total cholesterol (TC);
- familial hyperapobetalipoproteinemia - this disease is associated with high levels of apolipoprotein B, a protein that is part of LDL.
Depending on the type of fats, the level of which is increased, pure or isolated hypercholesterolemia (increased blood cholesterol as part of lipoproteins), pure hypertriglyceridemia (increased TG only) and mixed or combined hyperlipidemia (increased blood cholesterol and triglycerides) are distinguished. ).
Dyslipidemias are also classified according to Fredrickson:
- Type 1 – hereditary hyperchylomicronemia: only chylomicrons are elevated in the blood, TG is normal or elevated; the only type of dyslipidemia, the ability of which to cause atherosclerosis has not been proven;
- Type 2a – hereditary, polygenic (caused by hereditary factors and environmental influences) hypercholesterolemia: LDL is elevated in the blood, TG is normal;
- type 2b – combined hyperlipidemia: TC, LDL, VLDL and TG are increased in the blood;
- Type 3 – hereditary dysbetalipoproteinemia: increased DILP, TG, and total cholesterol in the blood;
- Type 4 – endogenous hyperlipidemia: VLDL is increased in the blood, TC is often normal, TG is increased; often this condition is accompanied by insulin resistance (IR), central obesity and high blood pressure;
- Type 5 – hereditary hypertriglyceridemia: VLDL and CM, TC and TG are increased in the blood; characterized by low atherogenicity; is rare.
In addition, there is also HDL cholesterol (hypoalphalipoproteinemia). This type is more often observed in men and is accompanied by damage to the coronary and cerebral vessels with the risk of developing a heart attack or stroke.
Also separately distinguished is nutritional dyslipidemia, which develops with excessive consumption of animal fats.
It is generally accepted that the most common cause of secondary dyslipidemia in men is alcohol abuse (secondary DLP type V), and in women it is hypothyroidism (usually DLP types IIa and IIb).
Very often the term hyperlipidemia is used interchangeably with dyslipidemia. But this is not entirely accurate. Hyperlipidemia is characterized by high levels of total cholesterol due to elevated LDL or triglycerides. And with dyslipidemia, the level of total cholesterol may be normal, but the levels of its fractions will be altered.
Diagnostics
Dyslipidemia is an exclusively laboratory indicator detected by a special blood test - lipid profile:
- elevated LDL;
- elevated TG;
- HDL levels are reduced;
- high coefficient of atherogenicity (development of atherosclerosis);
- total cholesterol is most often elevated, but can also be normal.
Depending on whether there are symptoms suggestive of other disorders, other tests may be needed, such as fasting glucose, insulin resistance, liver enzymes, creatinine, thyroid-stimulating hormone, and urine protein.
For anyone over 20 years of age who does not have cardiovascular disease (CVD), the American Heart Association recommends having your total cholesterol and TG levels checked every four to six years. If you have risk factors for heart disease (eg, obesity, diabetes, low HDL, high blood pressure), you may need to get tested more often. If hypercholesterolemia was previously diagnosed, then after normalizing the level of total cholesterol, it is still necessary to do a lipid profile to track the level of individual lipid fractions.
Children usually do not need to be tested for LDL levels. But for those at greater risk (eg, obesity, diabetes, hypertension), a lipid profile should be performed for the first time between the ages of 2 and 10 years.
Treatment
With a slight increase in “bad” cholesterol or TG, you can achieve normalization of their levels by changing your lifestyle, giving up bad habits, losing excess weight, proper nutrition, and dosed regular physical activity. Thus, according to the conclusion of the American Heart Association, comprehensive non-drug measures can lead to a decrease in LDL levels by 15-25 mg/dL (0.4 - 0.65 mmol/L). If within 8-12 weeks these methods are ineffective, then medications are added. Persons with the highest risk of developing CVD (coronary artery disease, atherosclerosis of the cerebral and peripheral arteries, abdominal aortic aneurysm, diabetes) require immediate lipid-lowering therapy.
Currently, HMG-CoA reductase inhibitors (statins), fibric acid derivatives (fibrates), nicotinic acid and its modern dosage forms, bile acid sequencers or anion exchange resins, polyunsaturated fatty acids (fish oil, omacor), inhibitor are used to correct DLP. absorption of cholesterol in the intestine (ezetimibe).
The most commonly recommended drugs are statins (eg, atorvastatin, simvastatin, fluvastatin, cerivastatin, rosuvastatin). They help lower LDL levels by inhibiting the production of cholesterol in the liver and improve endothelial function. During therapy, it is necessary to monitor lipid parameters, liver and muscle enzymes (ALT, AST, CPK) once every 3 months during the first year of therapy, and subsequently at least once every 6 months. In some cases, other drugs, such as fibrates and omega-3 fatty acids, are prescribed instead or in addition to them.
Treatment of dyslipidemia should always include correction of underlying health problems that increase the risk of developing serious diseases, such as high blood pressure, diabetes.
If lipid-lowering drug therapy is insufficiently effective, invasive methods for correcting lipid metabolism disorders can be used: plasmapheresis and LDL-phapheresis.
Prevention
It is necessary to lead a healthy lifestyle, give up bad habits if possible, maintain your weight at an optimal level, eat a balanced diet and do not forget about regular physical activity.
Also recommended
- [40-039] Lipidogram
- [18-072] Apolipoprotein E (ApoE). Detection of polymorphism e2-e3-e4
- [06-009] Apolipoprotein A1
- [06-008] Apolipoprotein B
- [06-178] Lipoprotein (a)
- [06-015] Plasma glucose
- [06-014] Glycated hemoglobin (HbA1c)
- [06-071] Glucose tolerance test (advanced)
- [08-118] Thyroid-stimulating hormone (TSH)
- [08-116] Free thyroxine (free T4)
- [40-492] Advanced laboratory examination of the heart and blood vessels
- [40-135] Laboratory testing for metabolic syndrome
Prevention
If left untreated, dyslipidemia leads to atherosclerosis with chronic and acute complications. In the first case, chronic ischemia develops in the area of the blood supply where an atherosclerotic plaque has formed. In the second - acute vascular insufficiency due to the closure of the lumen of blood vessels, and then infarction of various organs.
The prognosis depends on the localization of atherosclerosis, the rate of development of changes and provoking factors that can be influenced. It is very important to normalize body weight and adjust your diet, give up bad habits and emotional overload, and switch to a physical activity program on an individual schedule.
Specialists from Professor Gorbakov’s Clinic will talk about these and other preventive methods with which you can maintain your health and prevent serious consequences.
Pathogenesis
Lipoproteins whose diameter is less than 70 nm pass through the vascular endothelium. ApoB-containing lipoproteins in the arterial wall become trapped and trigger a process whereby lipids are deposited in the wall. Low-density lipoproteins are oxidized and, together with monocytes, form the core of an atherosclerotic plaque. The active substances released during this process are involved in the proliferation of smooth muscle cells in blood vessels and the breakdown of collagen. In patients with high levels of apoB-containing lipoproteins, more particles are deposited, and the atherosclerotic plaque progresses faster. Over time, other particles are deposited in the vessel wall, and the atherosclerotic plaque, reaching a critical point, ruptures with the formation of a blood clot on the surface. It becomes the cause of blockage of the vessel with the development of angina or myocardial infarction .
Dyslipidemia develops with
insulin resistance .
Under conditions of increased insulin secretion with decreased tissue sensitivity to insulin, increased breakdown of fats into fatty acids occurs. The latter are delivered to the liver, where they produce low-density lipoprotein cholesterol. Dyslipidemia causes increased blood pressure. The role of very low-density and low-density lipoproteins in the development of vascular endothelial dysfunction has been proven, which causes disruption of the synthesis of nitric oxide and an increase in the production of the vasoconstrictor peptide endothelin-1. As a result, vasoconstriction occurs and systemic blood pressure increases. Primary hyperlipidemia type 1 is associated with a mutation in the lipoprotein lipase gene. A defect in this enzyme blocks the metabolism of chylomicrons and they accumulate in large quantities in the plasma. With reduced lipoprotein lipase activity, triglycerides are not broken down and severe triglyceridemia .
List of sources
- ESC/EAS 2022 recommendations for the treatment of dyslipidemia: modification of lipids to reduce cardiovascular risk/Russian Journal of Cardiology 2020; 25 (5), pp. 121-193.
- Ershova A.I., Al Rashi D.O., Ivanova A.A., Aksenova Yu.O., Meshkov A.N. Secondary hyperlipidemia: etiology and pathogenesis. Russian Journal of Cardiology. 2019; (5): 74-81.
- Diagnosis and correction of lipid metabolism disorders for the prevention and treatment of atherosclerosis. Russian recommendations VI revision. Atherosclerosis and dyslipidemia. 2017; 3 (28): 5-22.
- Cronenberg G. M. et al. Obesity and lipid metabolism disorders / Trans. from English edited by I. I. Dedova, G. F. Melnichenko. M.: Read Elsiver LLC, 2010. 264 p.
- Vizir V.A., Berezin A.E. Modern approaches to the treatment of hyperlipidemia/Zaporozhye Medical Journal. - 2011. - volume 13, no. 1, pp. 108-117.
Risk group
People at risk for developing hyperlipidemia include:
- suffering from abnormalities of the endocrine system (diabetes or obesity);
- who have a history of close relatives with the development of atherosclerosis;
- abusing alcohol and tobacco products;
- those who do not follow proper nutrition (the predominance of fatty and fried foods in the diet);
- over the age of 50;
- leading a sedentary lifestyle.